Abstract
Trauma of the cervical spine is one of the most harrowing injuries seen in athletics. Although such injuries are not common, their impact can be devastating. Based on a thorough review of the literature, this article explains the identification of cervical spine trauma and the importance of stability therein. Multiple examples are given highlighting these findings and the way that multiple modalities can be used to asses such injuries. The article concludes with a brief review of the current recommendations as they relate to imaging in the initial assessment of cervical spine trauma.
Keywords: cervical spine trauma, computed tomography, magnetic resonance imaging
Injuries of the cervical spine are conservatively estimated to occur in over 1 million blunt trauma patients per year.2,5 As of the mid-1990s, more than $3.4 billion per year was being spent in the evaluation and treatment of cervical spine injuries.1 The major causes of cervical spine injury are as follows: motor vehicle accident, acts of violence, falls, and sporting injuries.18 Although sporting injuries are not the most common cause of cervical spine injury, the potential harrowing consequences of these injuries and their litigious implications have made imaging a strong component in their clinical treatment.15 This review covers the common and potentially most dangerous injuries that the sports-related clinician may encounter. Given the lack of clarity regarding whom to image and how to do so, a brief review of the literature with recommendations is also presented.
There are many ways to approach cervical spine trauma; unfortunately, none of them is easy. One helpful way is to think of the injury patterns based on mechanism—namely, flexion, extension, compression/axial load, and shearing/rotation. This classification allows one to predict what trauma may occur in a given athletic injury and what injuries to be alert for. The drawback of this classification is that, given the speed of athletics, it may always be a question of exactly what the injury mechanism was. A detailed discussion of all such injuries would be too vast for this article; however, the mechanisms are thoroughly described (see figures).
Injuries to the cervical spine are grave, given the potential injury to the spinal cord and other neural elements. The injury to the neural elements may occur at the time of the initial athletic trauma, or the trauma may leave the person predisposed to future injury. Studies have shown that delayed onset of paralysis occurs in up to 15% of missed fractures,6 which underscores the importance of recognizing spine instability and its potential to lead to neurological complication. White and Panjabi33 define clinical instability as “the loss of the ability of the spine under physiologic loads to maintain its pattern of displacement so that there is no initial or additional neurological deficit, no major deformity, and no incapacitating pain.”33 Given that much of the decision making that relates to patient treatment is based on this concept of stability, much of this article deals with a further examination of this concept.
Cervical Spine Anatomy and Injury
Within the cervical spine, the multiple ligaments supporting the cervical spine are of the utmost importance. These include the anterior longitudinal ligament, posterior longitudinal ligament, and the posterior ligament complex of Holdsworth, which is composed of the ligamentum flavum, apophyseal joint capsules, interspinous ligament, and the supraspinous ligament / ligamentum nuchae.16 The greater the degree of injury to these structures, the greater the risk for translation in the cervical spine and neurological injury.11 Ligaments themselves are now exquisitely visualized on magnetic resonance imaging (MRI) (Figures 1 and 2). These ligaments, when disrupted, render the spine unstable. However, if the ligaments remain intact or partially intact, it does not imply stability, because a stretched, sprained, or partially disrupted ligament may not be able to sustain physiologic loads and so lead to further osseous or neurological injury.4 As described in cadaveric examinations by Stabler, multiple soft tissue injuries were seen in ligaments and facet capsules in the setting of no associated clinical symptomatology.28 Therefore, the degree of injury necessary to produce instability or significance is still in question.5
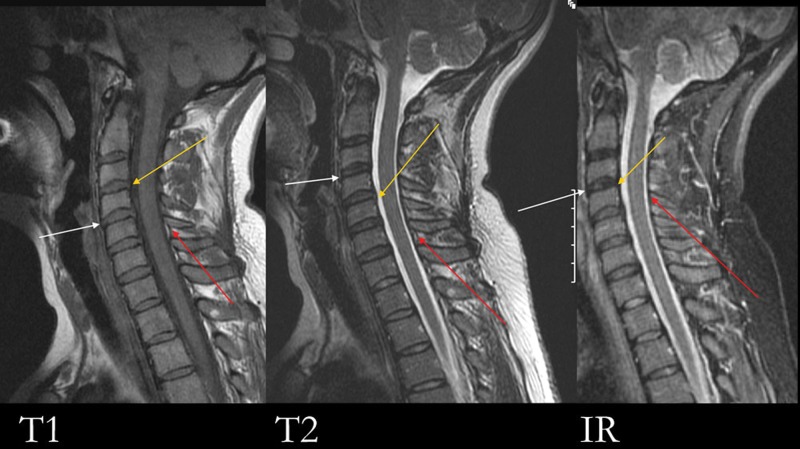
Figure 1.
T1, T2, and IR (inversion recovery) sagittal sequences of the cervical spine demonstrate normal anterior longitudinal ligament (white arrow), posterior longitudinal ligament (yellow arrow), and ligamentum flavum (red arrow).
Figure 2.

Yellow arrow (on the left) demonstrates a focal disruption of the posterior longitudinal ligament. White arrows (on the right) show a thickened, sprained ligamentum flavum with a partial intrasubtance disruption.
Atlantoaxial Articulation
The ligaments mentioned thus far are seen throughout the cervical spine, but the atlantoaxial articulation is unique in its ligamentous architecture. The key ligament in maintaining stability at the atlantoaxial articulation is the transverse atlantal ligament, which extends between the lateral masses of C1 to support the dens. Disruption of this ligament may be seen in the setting of an axial load injury yielding a comminuted fracture of the anterior and posterior arches of C1, or a Jefferson fracture. On MRI, the transverse atlantal ligament disruption may be seen (Figure 3), but on radiographs or computed tomography (CT), the ligament is presumed to have been disrupted in a Jefferson fracture with an atalantoaxial distance measuring greater than 3 mm or with a lateral mass offset of C1 on C2 measuring more than 7 mm (Figures 4 and 5).24,25
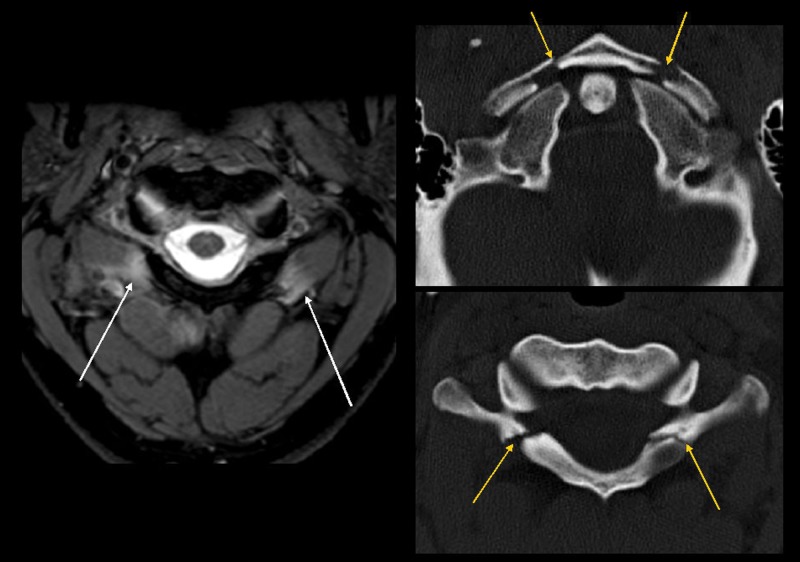
Figure 3.
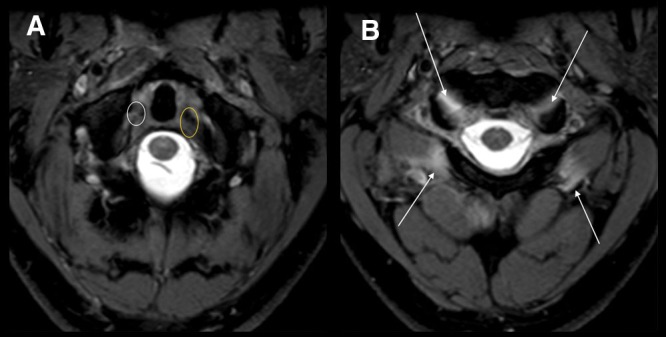
Transverse atlantal ligament disruption: A, white circle shows disruption of the transverse ligament of the atlas, or transverse atlantal ligament, in the setting of an axial load injury. Yellow circle demonstrates thickening of the ligament without clear disruption. B, axial images of the same patient, demonstrating edema pattern about the anterior and posterior arches of C1 (white arrows).
Figure 4.
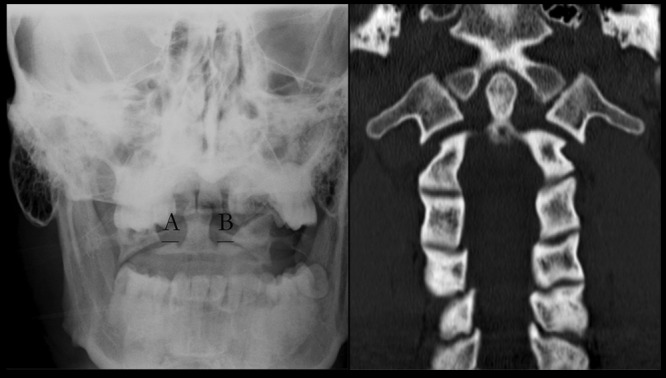
Same patient as in Figure 3, who sustained an axial load injury with an unstable Jefferson fracture. Open mouth, or odontoid, radiograph and coronal CT reformation shows the offset of the lateral masses greater than 7 mm (ie, A + B is greater than 7 mm).
Figure 5.
Jefferson fracture much more easily seen on CT study (yellow arrows) as compared to the MRI, where only an edema pattern (white arrows) can be seen.
Hyperextension Injuries
Hyperextension injuries can be seen in addition to the axial load mechanism for injury in the upper cervical spine. Hyperextension injuries frequently lead to so-called hangman fractures, or bilateral C2 pars fractures. As described by Effendi, the hangman fracture is actually a constellation of fractures, which he classified as types I, II, and III.9 The fractures are classified by degree of angulation at the fracture site, fracture fragment displacement, abnormalities at the C2-C3 disk space, and C2-C3 facet dislocation. The hangman fracture can be obvious or subtle. The spinolaminar line is an excellent tool for identifying the subtle hangman fracture because this line at C2 should not fall more than 2 mm from the spinolaminar line connecting C1 and C3. An additional sign, helpful in identifying the subtle hangman’s fracture, is the fat C2 sign, where the C2 body appears widened in the anteroposterior dimension as compared to that of C3 (the anteroposterior dimensions of the C2 and C3 bodies are normally equal) (see Figure 6).27 Hangman fractures are unstable with greater than 3 mm of fragment displacement, 15° or greater angulation at the fracture site, C2-C3 disk space abnormality, and/or C2-C3 facet dislocation.9
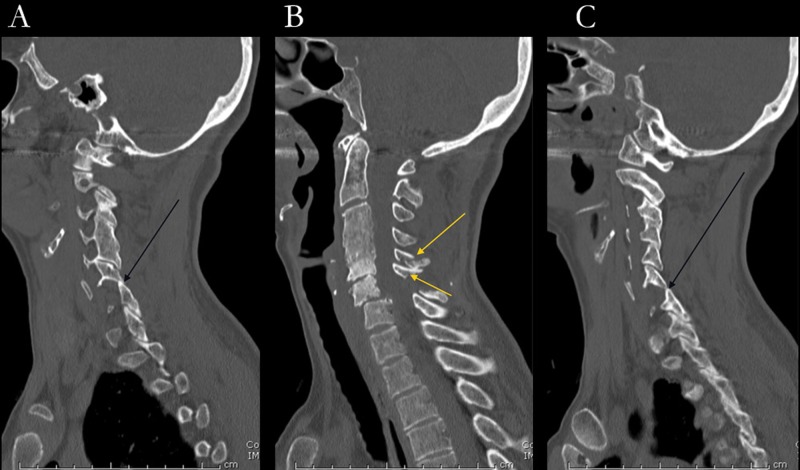
Figure 6.

Two examples of hangman’s fractures, or bilateral pedicle/posterior arch fractures of C2. On the more subtle fracture (A), note that the spinolaminar line from C1 to C3 (dotted line) falls greater than 2 mm posterior to the spinolaminar junction of C2 (double-headed arrow). Also note the fat C2 vertebral body relative to that of C3 (yellow single line versus yellow double lines).
Radiographic Assessment of Stability
Because the assessment of stability is such a critical issue in cervical spine injury, great effort has been made in delineating the findings that indicate instability—the majority of which have been applied to radiographs and CT given their increasing and now almost-ubiquitous usage. The same findings would indicate instability on MRI, but as described earlier, the soft tissue detail on MRI allows additional evaluation of ligament injury for instability. Findings of instability include those discussed for hangman fractures and Jefferson fractures, but they also include anterior translation of more than 3.5 mm of one vertebrae relative to the adjacent vertebrae, greater than 20° angulation of one vertebrae to the adjacent vertebrae, unilateral facet dislocation, and bilateral facet dislocations. The last 2 injuries are typically seen in the setting of a hyperflexion injury, often with concomitant rotation. The paired facet joints of the cervical spine are oriented such that the inferior facet (articular pillar) of the vertebrae above is posterior to the superior facet (articular pillar) of the vertebrae below. Although rudimentary, rigorous evaluation of this alignment is essential in assessing the facet joints. Unilateral facet dislocation is associated with a 25% to 50% anterolisthesis of one vertebrae on the other, an offset of the articular pillars yielding a so-called bowtie sign, a widening of the laminar space secondary to the rotational component, and a widening of the interspinous distance related to hyperflexion (Figure 7). The bilateral facet dislocation gives rise to greater than 50% anterolisthesis and implies a disruption of all the major supporting ligaments of the cervical spine. Secondary to the anterolisthesis is a severe narrowing of the central canal (Figures 8-10). However, there is often an associated traumatic disk herniation, further exacerbating the situation (Figure 11).8
Figure 7.
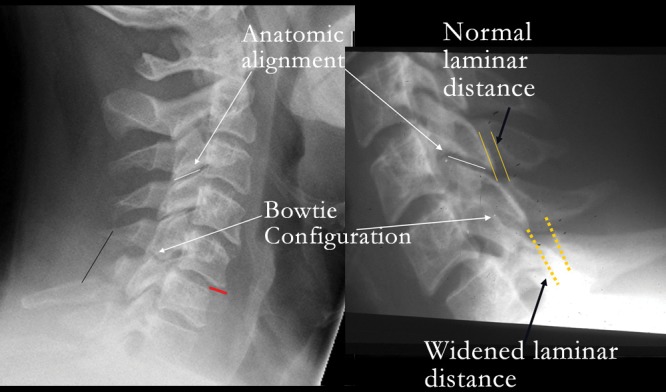
Unilateral facet dislocation. Lateral radiographs in 2 hyperflexion/rotation injuries. With hyperflexion, the posterior ligaments are stretched and torn, yielding a widening of the posterior elements (black line) and a subluxation of the vertebrae (red line). Note the loss of the normal alignment of the facet joints with the pathologic bow-tie configuration on the lateral view. Dotted yellow lines show the widening of the laminar line (distance between the spinolaminar junction and the posterior aspect of the articular pillars).
Figure 8.

Lateral and magnified lateral views of the cervical spine demonstrate approximately 25% anterolisthesis in this setting of bilateral facet subluxation. There is a narrowing of the central canal secondary to the anterolisthesis.
Figure 10.
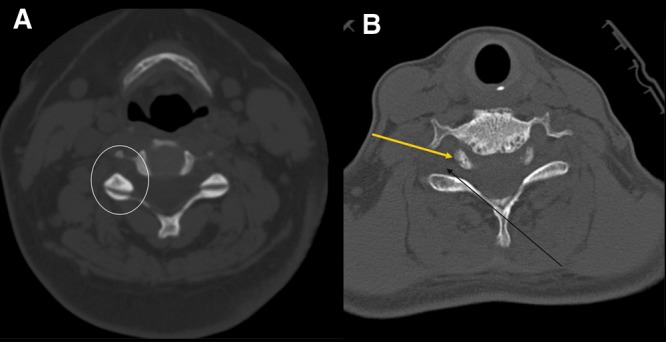
Axial images of patient in Figure 8 demonstrate the normal configuration (A) and abnormal configuration (B) of the facet joints. A, the so-called hamburger bun configuration. In the circle, note an architecture similar to a hamburger bun. B, there is an uncovering of the facets, or naked facets, with little articulation (black arrow). Note that the top of the bun now points posterior (yellow arrow), instead of the orthotopic anterior.
Figure 11.

A (T1) and B (T2) sagittal images of a different patient sustaining a hyperflexion injury. Not only is there central canal stenosis from the anterolisthesis, but an associated traumatic disk herniation exacerbates the stenosis and contributes to cord compression (arrow).
Figure 9.
Three sagittal reformation views of patient in Figure 8: A and C, subluxation, or perched bilateral facets (black arrows); B, the anterolisthesis and multiple fractures of the posterior elements (yellow arrows).
Other Injuries
Traumatic disk herniation is much more common in the cervical spine than in the lumbar spine, and within the cervical spine, it typically occurs from C4 to C7.7,23 As stated previously, there is a high correlation with bilateral facet dislocation but also with hyperextension and certain flexion injuries. Disk herniation is an important determinant in treatment because the disk may be removed during surgery performed for stabilization purposes. As expected, residual cord compression secondary to an acutely herniated disk is associated with a greater degree of morbidity.26 Given the well-accepted fact that MRI allows much better soft tissue detail than that of CT, MRI is an invaluable tool in assessing the degree of cervical spine injury. The value of MRI has been substantiated in multiple trials, nicely delineated in the meta-analysis by Muchow et al,20 which showed an injury rate of 20.9% detected by MRI but not appreciated on CT or radiographs. The authors clearly state that it particularly relates to the identification of ligamentous, disk, and extradural soft tissue injury. This is an important point to qualify because MRI is notoriously insensitive to fractures in the cervical spine and within the posterior elements.19 Compare this to CT, which routinely shows sensitivity and specificity values higher than 98%,3,17 which underscores the importance of using modalities in concert and not isolation (Figure 5).
One clinical setting frequently encountered in athletics is that of cervical cord neurapraxia, which is defined as sensory and/or motor disturbance involving the upper, lower, or both sets of extremities that lasts for several minutes to a few days. This relates to a temporary compression of the cord that may result from marked flexion or extension of the cervical spine.21,30,32 Great attention has been paid to the role of congenital or developmental stenosis of the cervical spine and its role in cervical cord neurapraxia as well as posttraumatic quadraparesis. Developmental stenosis of the cervical spine is defined as a sagittal canal diameter of less than 14 mm or a Torg ratio of less than 0.80: the ratio between the diameter of the spinal canal and the diameter of a midcervical sagittal vertebral body (Figure 12).13,14,32 Developmental stenosis has been found to be a predisposition to cervical cord neurapraxia but not to permanent injury and, as such, does not preclude athletes from activity.31 The patient with developmental stenosis is inherently more predisposed to cord impingement from a disk herniation, such as that in a traumatic disk herniation (Figure 13). Thus, MRI may have a greater role in the setting of trauma in the patient with developmental stenosis but no CT or radiographic findings of acute injury. As of yet, no data have been published directly addressing this issue, and this may be a source of future investigation.
Figure 12.

Measurements of the same patient on MRI and CT demonstrating congenital/developmental spinal stenosis.
Figure 13.

Manual proprioceptive neuromuscular facilitation upper extremity D2 patterns with rhythmic stabilization.
Imaging of Acute Spinal Trauma
Cervical spine trauma is fraught with medico legal implications. As such, the role of imaging is frequently called into question. Two large studies addressed the need for imaging in cervical spine trauma: the National Emergency X-ray Utilization Study (NEXUS) and the Canadian Cervical Spine Rule Group (CCR). Both studies were successful at identifying patients at low risk for cervical spine injury and so decreased the use of imaging in this population.15,29 The NEXUS study states that imaging is not necessary if all of the following criteria are met: no midline cervical tenderness, no focal neurological deficit, normal level of alertness, no intoxication, and no painful distracting injury. The CCR criteria are somewhat more elaborate and include an absence of high-risk criteria, the presence of any low-risk factor, and the ability to actively rotate the neck 45°. Both studies showed a sensitivity greater than 99%, but the specificity of the CCR was more than 3 times that of the NEXUS study, indicating that it is likely to cause a decrease in unnecessary imaging.
Radiograph or CT in the Evaluation of Cervical Spine Trauma
A Harborview study tried to delineate what type of imaging should be employed for the evaluation of cervical spine trauma.12 Patients were stratified into high-risk and low-risk groups. High risk was defined as a high-energy injury mechanism or a high-risk clinical parameter. High-energy injury included motor vehicle accident at greater than 35 mph (56 kph), motor vehicle accident with a death at the scene, or a fall from a height of greater than 10 feet (3.05 m). High-risk clinical parameters included significant head injury, neurological signs or symptoms referred to the cervical spine, and pelvic or multiple extremity fractures. What the researchers found, after evaluating for optimal patient care and cost-effectiveness, was that patients who met the high-risk criteria should have an initial CT study and those who did not, should have the standard 3-view set of radiographs (anteroposterior, lateral, open mouth).
In 2006, Platzer reported that in cervical trauma, CT was the most efficient modality in detecting skeletal injuries and it was almost 40% more sensitive than a single lateral radiograph.22 In 2007, the American College of Radiology formulated appropriateness criteria in the setting of cervical spine trauma after an initial investigation of over 5700 patients and a literature review involving more than 55 000 patients.5 They stated that (1) if NEXUS or CCR criteria indicate low risk, then no imaging should be performed and (2) if NEXUS or CCR criteria indicate imaging, then a CT of the cervical spine with sagittal and coronal reformations is highly recommended. In 2008, Fisher reported that, secondary to the increased sensitivity of CT and the now increased speed from multidetector CT units, lateral radiogrpahs should be eliminated; that is, CT is the sole choice for initial evaluation in cervical spine trauma.10
The role of MRI in acute cervical trauma is still being defined. The indications set by the American College of Radiology that relate to MRI are as follows: (1) If NEXUS or CCR criteria are met and there are clinical findings of myelopathy, then CT with reformations, MRI of the cervical spine, and lateral radiograph should be obtained. (2) If NEXUS or CCR criteria are met and there are clinical or imaging findings to suggest ligamentous injury, then CT with reformations and MRI of the cervical spine should be obtained. (3) If NEXUS or CCR criteria indicate imaging and the mechanically unstable spine is anticipated, then CT with reformations, MRI, and radiographs should be obtained.5 The role that magnetic resonance plays in the evaluation of instability will continue to evolve, and attention should be paid to guidelines set forth in the future.
In summary, the use of cross-sectional imaging has greatly enhanced the imaging of cervical spine trauma. The gamut of cervical spine trauma pathology is vast, but of great importance is the assessment of stability for present and future injuries.
Acknowledgments
I would like to thank Richard J. Herzog, MD, for his continued input and recommendations, as well as multiple radiological cases, and Alex B. Maderazo, MD, for his multiple radiological cases.
Footnotes
No potential conflict of interest declared.
References
- 1. Berkowitz M. Assessing the socioeconomic impact of improved treatment of head and spinal cord injuries. J Emerg Med. 1993;11(suppl 1):63-67 [PubMed] [Google Scholar]
- 2. Blackmore CC. Evidence-based imaging evaluation of the cervical spine in trauma. Neuroimaging Clin N Am. 2003;13(2):283-291 [DOI] [PubMed] [Google Scholar]
- 3. Brohi K, Healy M, Fotheringham T, et al. Helical computed tomographic scanning for the evaluation of the cervical spine in the unconscious, intubated trauma patient. J Trauma. 2005;58(5):897-901 [DOI] [PubMed] [Google Scholar]
- 4. Chiu WC, Haan JM, Cushing BM, Kramer ME, Scalea TM. Ligamentous injuries of the cervical spine in unreliable blunt trauma patients: incidence, evaluation, and outcome. J Trauma. 2001;50(3):457-464 [DOI] [PubMed] [Google Scholar]
- 5. Daffner RH, Hackney DB. ACR Appropriateness Criteria on suspected spine trauma. J Am Coll Radiol. 2007;4(11):762-775 [DOI] [PubMed] [Google Scholar]
- 6. Davis JW, Phreaner DL, Hoyt DB, Mackersie RC. The etiology of missed cervical spine injuries. J Trauma. 1993;34(3):342-346 [DOI] [PubMed] [Google Scholar]
- 7. Davis SJ, Teresi LM, Bradley WG, Jr, Ziemba MA, Bloze AE. Cervical spine hyperextension injuries: MR findings. Radiology. 1991;180(1):245-251 [DOI] [PubMed] [Google Scholar]
- 8. Doran SE, Papadopoulos SM, Ducker TB, Lillehei KO. Magnetic resonance imaging documentation of coexistent traumatic locked facets of the cervical spine and disc herniation. J Neurosurg. 1993;79(3):341-345 [DOI] [PubMed] [Google Scholar]
- 9. Effendi B, Roy D, Cornish B, Dussault RG, Laurin CA. Fractures of the ring of the axis: a classification based on the analysis of 131 cases. J Bone Joint Surg Br. 1981;63(3):319-327 [DOI] [PubMed] [Google Scholar]
- 10. Fisher A, Young WF. Is the lateral cervical spine x-ray obsolete during the initial evaluation of patients with acute trauma? Surg Neurol. 2008; 70(1):53-58 [DOI] [PubMed] [Google Scholar]
- 11. Greenspan A. Orthopedic Imaging: A Practical Approach. Vol 4 Philadelphia, PA: Lippincott Williams & Wilkins; 2004 [Google Scholar]
- 12. Hanson JA, Blackmore CC, Mann FA, Wilson AJ. Cervical spine injury: a clinical decision rule to identify high-risk patients for helical CT screening. AJR Am J Roentgenol. 2000;174(3):713-717 [DOI] [PubMed] [Google Scholar]
- 13. Herzog RJ, Wiens JJ, Dillingham MF, Sontag MJ. Normal cervical spine morphometry and cervical spinal stenosis in asymptomatic professional football players: plain film radiography, multiplanar computed tomography, and magnetic resonance imaging. Spine. 1991;16(6)(suppl):S178-S186 [DOI] [PubMed] [Google Scholar]
- 14. Hinck VC, Hopkins CE, Savara BS. Sagittal diameter of the cervical spinal canal in children. Radiology. 1962;79:97-108 [DOI] [PubMed] [Google Scholar]
- 15. Hoffman JR, Mower WR, Wolfson AB, Todd KH, Zucker MI, National Emergency X-Radiography Utilization Study Group Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. N Engl J Med. 2000;343(2):94-99 [DOI] [PubMed] [Google Scholar]
- 16. Holdsworth F. Fractures, dislocations, and fracture-dislocations of the spine. J Bone Joint Surg Am. 1970;52(8):1534-1551 [PubMed] [Google Scholar]
- 17. Holmes JF, Akkinepalli R. Computed tomography versus plain radiography to screen for cervical spine injury: a meta-analysis. J Trauma. 2005;58(5):902-905 [DOI] [PubMed] [Google Scholar]
- 18. Jones C, Jazayeri F. Evolving standards of practice for cervical spine imaging in trauma: a retrospective review. Australas Radiol. 2007;51(5):420-425 [DOI] [PubMed] [Google Scholar]
- 19. Klein GR, Vaccaro AR, Albert TJ, et al. Efficacy of magnetic resonance imaging in the evaluation of posterior cervical spine fractures. Spine. 1999;24(8):771-774 [DOI] [PubMed] [Google Scholar]
- 20. Muchow RD, Resnick DK, Abdel MP, Munoz A, Anderson PA. Magnetic resonance imaging (MRI) in the clearance of the cervical spine in blunt trauma: a meta-analysis. J Trauma. 2008;64(1):179-189 [DOI] [PubMed] [Google Scholar]
- 21. Penning L. Some aspects of plain radiography of the cervical spine in chronic myelopathy. Neurology. 1962;12:513-519 [DOI] [PubMed] [Google Scholar]
- 22. Platzer P, Jaindl M, Thalhammer G, et al. Clearing the cervical spine in critically injured patients: a comprehensive C-spine protocol to avoid unnecessary delays in diagnosis. Eur Spine J. 2006;15(12):1801-1810 [DOI] [PubMed] [Google Scholar]
- 23. Rizzolo SJ, Piazza MR, Cotler JM, Balderston RA, Schaefer D, Flanders A. Intervertebral disc injury complicating cervical spine trauma. Spine. 1991;16(6)(suppl):S187-S189 [DOI] [PubMed] [Google Scholar]
- 24. Schlicke LH, Callahan RA. A rational approach to burst fractures of the atlas. Clin Orthop Relat Res. 1981;154:18-21 [PubMed] [Google Scholar]
- 25. Segal LS, Grimm JO, Stauffer ES. Non-union of fractures of the atlas. J Bone Joint Surg Am. 1987;69(9):1423-1434 [PubMed] [Google Scholar]
- 26. Silberstein M, Tress BM, Hennessy O. Prediction of neurologic outcome in acute spinal cord injury: the role of CT and MR. AJNR Am J Neuroradiol. 1992;13(6):1597-1608 [PMC free article] [PubMed] [Google Scholar]
- 27. Smoker WR, Dolan KD. The “fat” C2: a sign of fracture. AJR Am J Roentgenol. 1987;148(3):609-614 [DOI] [PubMed] [Google Scholar]
- 28. Stabler A, Eck J, Penning R, et al. Cervical spine: postmortem assessment of accident injuries: comparison of radiographic, MR imaging, anatomic, and pathologic findings. Radiology. 2001;221(2):340-346 [DOI] [PubMed] [Google Scholar]
- 29. Stiell IG, Wells GA, Vandemheen KL, et al. The Canadian C-spine rule for radio-graphy in alert and stable trauma patients. JAMA. 2001;286(15):1841-1848 [DOI] [PubMed] [Google Scholar]
- 30. Torg JS, Corcoran TA, Thibault LE, et al. Cervical cord neurapraxia: classification, pathomechanics, morbidity, and management guidelines. J Neurosurg. 1997;87(6):843-850 [DOI] [PubMed] [Google Scholar]
- 31. Torg JS, Naranja RJ, Jr, Pavlov H, Galinat BJ, Warren R, Stine RA. The relationship of developmental narrowing of the cervical spinal canal to reversible and irreversible injury of the cervical spinal cord in football players. J Bone Joint Surg Am. 1996;78(9):1308-1314 [DOI] [PubMed] [Google Scholar]
- 32. Torg JS, Pavlov H, Genuario SE, et al. Neurapraxia of the cervical spinal cord with transient quadriplegia. J Bone Joint Surg Am. 1986;68(9):1354-1370 [PubMed] [Google Scholar]
- 33. White AA, III, Panjabi MM. Clinical Biomechanics of the Spine. Vol 2 Philadelphia, PA: J B Lippincott; 1991 [Google Scholar]