Abstract
Return from athletic injury can be a lengthy and difficult process. The injured athlete commonly receives care from several providers during rehabilitation. As their condition improves, injured athletes resume strength and conditioning programs and sport-specific activities in preparation for return to play. Until full medical clearance is provided to return to sport and the athlete is psychologically ready to return to play, the injured athlete remains a patient regardless of who is developing and supervising each component of the recovery process. An understanding of and commitment to the plan of care for each athlete, as well as communication among health care providers, strength and conditioning specialists, coaches, and the athletes, are essential to the safest and most efficient recovery from injury.
Keywords: sports injury, sports medicine, strength training
Return from athletic injury can be a lengthy and difficult process. The injured athlete commonly receives care from several providers, including physicians, athletic trainers, physical therapists, and strength and conditioning specialists. At some point in the recovery process, athletes return to strength and conditioning programs and resume sport-specific activities in preparation for return to play. The transition is important for several reasons. First, although the athlete may have recovered in medical terms (ie, improvements in flexibility, range of motion, functional strength, pain, neuromuscular control, inflammation), preparation for competition requires the restoration of strength, power, speed, agility, and endurance at levels exhibited in sport. Such sport-specific training may be beyond what those attending to the athlete’s medical needs are qualified or prepared to provide.1 Returning from injury is a process requiring additional work from the injured athlete to regain competitive ability. Exercise must be prescribed with an emphasis on the fundamental components of the exercise prescription,2 which progressively incorporates activities and skills displayed in sport.2,3 When athletes resume team-based strength and conditioning activities, emphasis should be on generic movements (exercises inherent to most sports, such as closed kinetic chain squats) and sport-specific movements that makes up the complete strength training program for an athlete. Both exercise templates are vital in the recovery process.2
In contrast to linear improvement, rehabilitation is often a haphazard process with positives and negatives occurring daily. Consequently, athletes usually benefit from input from all providers throughout the process of returning to play. Unfortunately, athletes often pay the price for poorly coordinated recovery plans within the return-to-play process.4 Communication is a vital factor. A lack of communication between medical providers, strength and conditioning specialists, and team coaches can slow or prevent athletes from returning to peak capability and increase the risk of new injuries and even more devastating reinjuries.5 In addition, care providers must consider the possible psychological consequences of injuries, and they should position themselves to identify and address or refer such issues to appropriate parties when identified. Unfortunately, communication between clinicians is often suboptimal, face-to-face meetings infrequent, and clearly defined roles lacking in the return-to-play process.5
Coaching staffs and administrative personnel must work to ensure that care can be provided at all points of the rehabilitation process, especially when funding dictates the need to hire personnel capable of addressing injuries at multiple levels.6,7 Under most circumstances, individual providers should not be expected to possess the knowledge and training needed to ensure complete recovery for athletes through all stages of the return-to-play process.
Our purpose is to address the process of transition that takes place once rehabilitation from injury is near completion and athletes are ready to begin strength and conditioning activities, highlighting some common considerations en route to an expedient and successful injury recovery.
From Injury Resolution to Performance Resumption
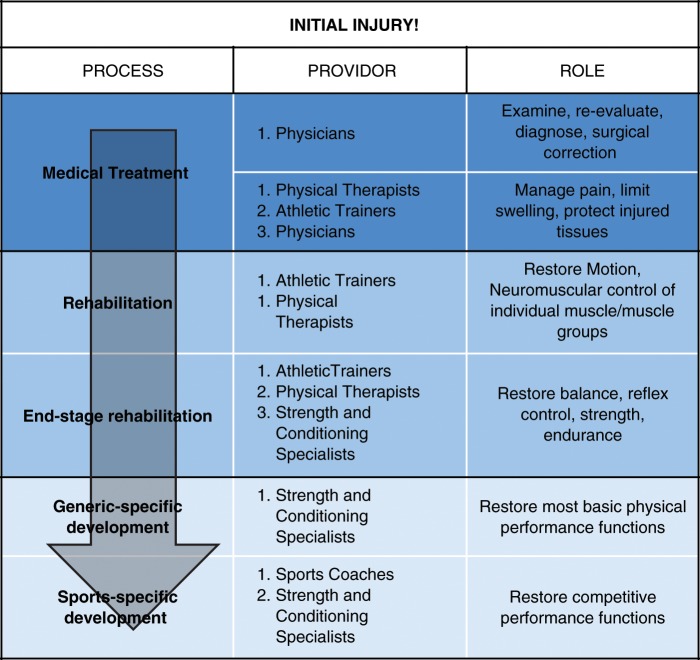
The paradigm found in Figure 1 provides an overview of the injury and recovery process. A thorough examination of the injured athlete and a careful evaluation of all findings are essential to an accurate diagnosis, from a structural and biomechanical perspective. A clear understanding of the injury and of the interventions from each provider is vital to an efficient and successful return to play. Each provider must make clear the purpose of each treatment and the restrictions from specific activities during the rehabilitation process while providing supervision at points of progression and when new activities are initiated.
Figure 1.
The process of care for an athlete who is returning to play, with different providers and roles.
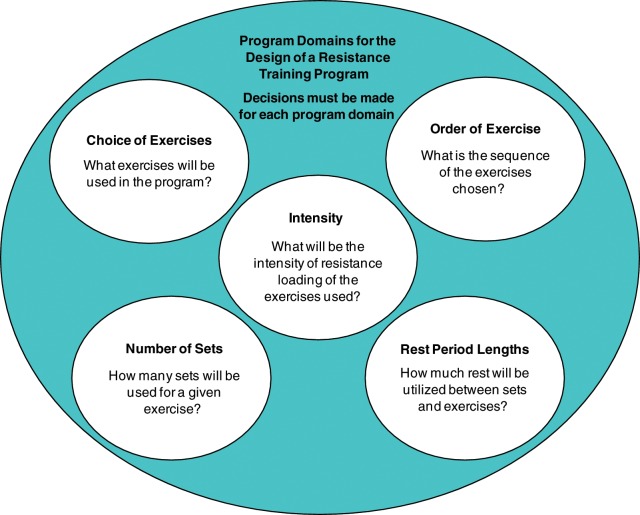
Resistance training is critical to the resolution of impairment and the recovery of function.2,10,12 Early in rehabilitation, resistance training is typically of lower intensity and often supervised by a physical therapist or athletic trainer in a clinical setting or in close tandem with strength and conditioning specialists. Early resistance exercise is prescribed for a number of reasons, including the restoration of balance, the development of reflex control, the redevelopment of neuromuscular control and function, and the development of strength and endurance in injured tissues.2,10,12 During the latter stages of rehabilitation treatment, goals shift from the resolution of impairment to functional recovery.8,11 During this period, exercises directed toward overall fitness are initiated, as are more aggressive but closely supervised strength, endurance, and neuromuscular retraining activities.2 In many cases, these activities occur in the weight room or in open spaces, outside the confines of a clinic. Acute program variable prescriptions (see Figure 2) are increasingly focused on encouraging adaptations that will improve physical abilities of high specificity to the performance demands of the athlete’s sport.3
Figure 2.
Program design variables.
Care and proper progression (or periodization) are needed with conventional heavier resistance training programs. The injured tissues must be carefully monitored to assess tolerance to exercise stress. Initially, recovery exercises (closed kinetic chain using body weight) may be highly stressful. Although well intended to stimulate tissue, they can cause overload damage and inflame previously injured or immobilized tissue. For example, after an initial strength improvement session, a recovering patellar tendon may be irritated, requiring therapeutic interventions such as rest, ice, compression, and elevation to mitigate symptoms and expedite the process of recovery so that further progressive resistance exercise sessions can take place with minimal delay.9,10 The athlete must be monitored for signs and symptoms of overload to the healing tendon that would not be of concern for a healthy athlete participating in the same conditioning program. Training might begin with carefully monitored unilateral exercises using open kinetic chain movements, progressing to weightbearing closed kinetic chain movements, and finally, bilateral closed kinetic chain movements. Such a progression would help permit the periodization of exercise stress and a central focus on the tissues in need of gains in force production and conditioning.
An awareness of the exercise prescription on any given day will better enable rehabilitation providers to anticipate, collaborate, and administer treatments. Furthermore, clinicians must inform strength and conditioning specialists on the status of injuries. Regardless of an athlete’s apparent level of recovery, constant feedback from the athlete is needed to gauge and adjust exercise prescriptions. The athlete’s perception during periods of recovery from injury can provide valuable direction in the decision-making process.
In addition, athletes must be regularly assessed to ensure that they are not attempting to conceal worsening conditions or delay return to play because of a lack of confidence or disagreement in the perceived severity of the injury. Such monitoring is the responsibility of all involved until the athlete has been provided medical clearance to discontinue all rehabilitative care and return to unrestricted sports participation.
Of critical importance is mutual agreement between all involved parties over the athlete’s readiness to rejoin highly demanding sports and conditioning activities.13 Medical providers must be assured that injured tissue is capable of withstanding the demands of sports and that muscle and joint impairments have been sufficiently resolved13,14; moreover, coaches must be confident that the athlete is adequately conditioned and physically capable of performing at a high level. Before athletes rejoin practice and other live competitive scenarios, coaches must believe that he or she can contribute to the success of the team.
Injury is more than physical; that is, the athlete must be psychologically ready for the demands of his or her sport. Many individuals assist athletes through the recovery process and can foster psychological readiness, but they can also identify those who are physically recovered but require more time or intervention to be fully prepared to return to competition. Thus, rehabilitation and recovery are not purely physical but also psychological.16,17
Individuals cope with illness and injury in different ways. Despite the ineffective and sometimes counterproductive coping behaviors, a number of approaches may be effective in assisting psychological recovery.16 Beyond the physical impairments relating to sport, limitations and disabilities associated with injury and recovery may cause additional distress. Concerns over reinjury, regaining status on a team, and failing to perform at preinjury levels are common and can affect the rate of recovery through overuse, avoidance, and other compliance issues. In some cases, clinical or sports psychologists will best provide the psychological care for an athlete who is recovering from injury.16 Athletes may train excessively for return to play and quickly become the biggest threat to successful recovery from injury. In many cases, educating athletes on the process of recovery and the physiological process taking place throughout each component may help to offset a natural inclination to overtrain injured tissues.
In a healthy state, the tissues of the musculoskeletal system respond to exercise through a process of damage and repair.2 If the tissues are excessively overloaded, injury can occur. When an athlete is recovering from an injury or surgery, tissue is already compromised and thus requires far more attention despite the recovery of joint motion and strength.13,18 Moreover, injuries and surgical procedures can create detraining issues that increase the likelihood of further injury. For example, when the midportion of the patella tendon is harvested for use in the reconstruction of the anterior cruciate ligament, the bone of the distal pole of the patella is weakened, as is the tendon itself. Excessive loading of these tissues can result in fracture or tendon rupture during training, thus creating an entirely new injury and process of recovery outside of what was already planned for the anterior cruciate ligament.12,15 Strength and conditioning specialists must have an awareness of the risks created by some of the common operative and rehabilitative procedures.18 For example, ankle immobilization designed to promote healing of an injured anterior talofibular ligament could lead to significant strength loss in muscles associated with the immobilized ankle joint. Consequently, strength and conditioning specialists must be sensitive to vulnerabilities and weaknesses caused by injuries.
Summary
The severity of an injury and the complexity of the medical and surgical care affect the rate of recovery and the extent to which rehabilitation must be supervised in some cases. In all cases, clear and open communication is required from each person who is participating in the care process. Until full medical clearance is provided to return to sport and the athlete is psychologically ready to return to play, the injured athlete remains a patient regardless of who is developing and supervising each respective component of the recovery process.
Strength and conditioning specialists should give assessments of performance to health care providers with objective and quantifiable information that can show reliable, time-based trends indicative of improvement or lack of progress. Ultimately, successful rehabilitation depends on trust. The athlete must trust that all who participate in the treatment and rehabilitation process place the welfare of the athlete first.
Footnotes
No potential conflict of interest declared.
NATA Members: Receive 3 free CEUs each year when you subscribe to Sports Health and take and pass the related online quizzes! Not a subscriber? Not a member? The Sports Health–related quizzes are also available for purchase. For more information and to take the quiz for this article, visit www.nata.org/sportshealthquizzes.
References
- 1. Walsh JM, Swangard DM, Davis T, McPhee SJ. Exercise counseling by primary care physicians in the era of managed care. Am J Prev Med. 1999;16(4):307-313 [DOI] [PubMed] [Google Scholar]
- 2. Kraemer WJ, Ratamess NA, French DN. Resistance training for health and performance. Curr Sports Med Rep. 2002;1(3):165-171 [DOI] [PubMed] [Google Scholar]
- 3. Campos GE, Luecke TJ, Wendeln HK, et al. Muscular adaptations in response to three different resistance-training regimens: specificity of repetition maximum training zones. Eur J Appl Physiol. 2002;1-2:50-60 [DOI] [PubMed] [Google Scholar]
- 4. Kautz CM, Gittell JH, Weinberg DB, Lusenhop RW, Wright J. Patient benefits from participating in an integrated delivery system: impact on coordination of care. Health Care Manage Rev. 2007;32(3):284-294 [DOI] [PubMed] [Google Scholar]
- 5. Brandon TA, Lamboni P. Care of collegiate athletes. Md Med J. 1996;45(8): 669-675 [PubMed] [Google Scholar]
- 6. Olsen D. A descriptive survey of management and operations at selected sports medicine centers in the United States. J Orthop Sports Phys Ther. 1996;124(5):315-322 [DOI] [PubMed] [Google Scholar]
- 7. Verrall GM, Brukner PD, Seward HG. Doctor on the sidelines. Med J Aust. 2006;184(5):244-248 [DOI] [PubMed] [Google Scholar]
- 8. Kennedy JC, Alexander IJ, Hayes KC: Nerve supply to the human knee and its functional importance. Am J Sports Med. 1982;10:329-335 [DOI] [PubMed] [Google Scholar]
- 9. Kraemer WJ, Bush JA, Wickham RB, et al. Influence of compression therapy on symptoms following soft tissue injury from maximal eccentric exercise. J Orthop Sports Phys Ther. 2001;31(6):282-290 [DOI] [PubMed] [Google Scholar]
- 10. Järvinen TA, Järvinen TL, Kääriäinen M, et al. Muscle injuries: optimising recovery. Best Pract Res Clin Rheumatol. 2007;21(2):317-331 [DOI] [PubMed] [Google Scholar]
- 11. Patel DR, Baker RJ. Musculoskeletal injuries in sports. Prim Care. 2006;33(2):545-579 [DOI] [PubMed] [Google Scholar]
- 12. Baechle T, Earle R. Essentials of Strength Training and Conditioning. Champaign, IL: Human Kinetics; 2000 [Google Scholar]
- 13. Coris EE, Walz S, Konin J, Pescasio M. Return to activity considerations in a football player predisposed to exertional heat illness: a case study. J Sport Rehabil. 2007;16(3):260-270 [DOI] [PubMed] [Google Scholar]
- 14. Lee GH, McCulloch P, Cole BJ, Bush-Joseph CA, Bach BR., Jr. The incidence of acute patellar tendon harvest complications for anterior cruciate ligament reconstruction. Arthroscopy. 2008;24:162-166 [DOI] [PubMed] [Google Scholar]
- 15. Tay GH, Warrier SK, Marquis G. Indirect patella fractures following ACL reconstruction: a review. Acta Orthop. 2006;77:494-500 [DOI] [PubMed] [Google Scholar]
- 16. Walker N, Thatcher J, Lavallee D. Psychological responses to injury in competitive sport: a critical review. J R Soc Health. 2007;127(4): 174-180 [DOI] [PubMed] [Google Scholar]
- 17. Kiefhaber TR, Stern PJ. Upper extremity tendinitis and overuse syndromes in the athlete. Clin Sports Med. 1992;11(1):39-55 [PubMed] [Google Scholar]
- 18. Jones MH, Amendola AS. Acute treatment of inversion ankle sprains: immobilization versus functional treatment. Clin Orthop Relat Res. 2007; 455:169-172 [DOI] [PubMed] [Google Scholar]