Abstract
Context:
The vast differences between individual athletes makes identifying and evaluating sports-related concussion one of the most complex and perplexing injuries faced by medical personnel.
Evidence Acquisition:
This review summarizes the existing literature supporting the use of a multifaceted approach to concussion evaluation on the sideline of the athletic field. Information was drawn from a PubMed search (MEDLINE) for the terms sport concussion for the most recent and relevant literature.
Conclusions:
By using a standardized clinical examination that is supported by objective measures of concussion-related symptoms, mental status, and postural control, the medical professional becomes well equipped to make an informed diagnosis.
Keywords: mild traumatic brain injury, symptoms, postural control, neurocognitive status
Concussion, as that occurring in the context of sports, is defined as a complex pathophysiological process that affects the brain, as induced by traumatic biomechanical forces.2,30,31 Although concussions occur in a number of other settings (eg, automobile accidents), injuries resulting from sports participation typically represent, not a structural change, but an alteration in the functional capacity of the cerebral tissue.13 Traditional concussion incidence estimates (300 000 cases in a given year6) grossly underestimate the true injury occurrence by excluding injuries that do not result in a loss of consciousness. More recent estimates propose that many injuries have gone unreported and undiagnosed, suggesting that the true injury incidence is between 1.6 and 3.8 million per year.20 The incidence of concussion varies widely between sports,10 and for some sports (ie, women’s ice hockey), the incidence of concussion may exceed that of all other injuries.1 Regardless of the setting, certified athletic trainers (ie, ATCs) and other sports medicine professionals will likely deal with this complex and highly misunderstood injury at least once in their careers.
Much of the inherent complexity in evaluating athletes suspected of sustaining a concussion lies in the broad spectrum of outcomes associated with the injury. For example, impact location and magnitude,17 previous history of concussive injuries,16 learning disabilities,7 and age11 have all been shown to influence the risk of concussion and outcomes following injury. To further complicate matters, no definitive diagnostic tool is available for concussion at this time. Standard computed tomography and magnetic resonance imaging are insensitive to the functional deficits observed following concussion.31 In addition, although functional magnetic resonance imaging, diffuse tensor imaging, and single photon emission computed tomography show promise, their widespread use as an objective diagnostic tool has not yet been substantiated. Thus, several objective measures are recommended to support the clinical examination. Although the advent of these tools has vastly improved the concussion diagnosis, the clinical examination remains the gold standard for evaluation.14
The athletic trainer often represents the frontline of defense in protecting concussed athletes from returning to a game or practice and placing themselves at risk for further injury. Athletic trainers have the distinct advantage of knowing the personalities and habits of their athletes, which affords them the opportunity to rapidly identify alterations that would lead one to suspect a concussion. Once an athlete has been suspected of sustaining a concussion, a physician must be involved in the return-to-play decision, but the certified athletic trainer often manages the injury alone on the sideline. Similar to the evaluation of orthopaedic injuries, a systematic approach to concussion assessment permits medical personnel to rule out other, more serious injuries.
The On-Field Assessment
Primary Survey
The identification of the concussed athlete remains the most difficult aspect of the assessment process. Most athletes neglect to inform medical personnel if they have a concussion,27 and most will not show visible signs of concussion. In fact, only 10% of concussive injuries will involve a loss of consciousness.9,16 If an athlete is rendered unconscious, medical personnel should suspect a cervical spine injury when approaching the athlete on the playing field. The initial assessment should first include a determination of level of consciousness, then a primary survey of the athlete’s airway, breathing, and circulation while the cervical spine is maintained in a neutral position. Once the athlete regains consciousness and more severe injuries have been ruled out (eg, cervical spine or cranial fracture), the athlete can be taken to the sideline for further evaluation. If the athlete remains in an unconscious state, he or she should be transported to the nearest medical facility for further evaluation.
Secondary Survey
The sideline assessment for concussion begins before the competitive season. The highly variable nature of concussion mandates an individualized approach to injury management,2,30 and it necessitates the use of baseline assessments for each athlete, when injury free. Regardless of the tests employed, the evaluation should include measures of concussion-related symptoms, postural control, and neurocognitive function15 (each of which is addressed in detail below). When an athlete is evaluated following a suspected concussive blow, the premorbid data can be used to objectively identify postinjury change that will support the decision derived from the clinical examination.
History
The sideline assessment for concussion should follow a standardized protocol similar to the orthopaedic evaluation, with the initial appraisal related to the injury history. In many instances, the concussive blow was witnessed and the mechanism of injury known. The athlete, teammates, coaches, or other personnel may provide beneficial information concerning the mechanism of injury. Questioning the athlete about the injury will provide pertinent information relative to the injury. First, a level of consciousness can be established through dialogue with the athlete. If the athlete is not alert enough to understand the questions or is passing in and out of consciousness, he or she should be transported to a medical facility for further evaluation. Second, it is important to determine whether the athlete is suffering from retrograde or anterograde amnesia. To establish the presence or absence of retrograde amnesia, injury history questions should start at the time of impact and work backward. For example, the athlete may be asked the following: “Do you remember getting hit?” “Do you recall the play you were running?” “What team are we playing against?” and “Do you remember arriving at the field before the game?” Conversely, the assessment of anterograde amnesia should begin with questions surrounding events following injury, such as “Who was the first person you saw on the field?” and “Do you recall coming over to the bench?”
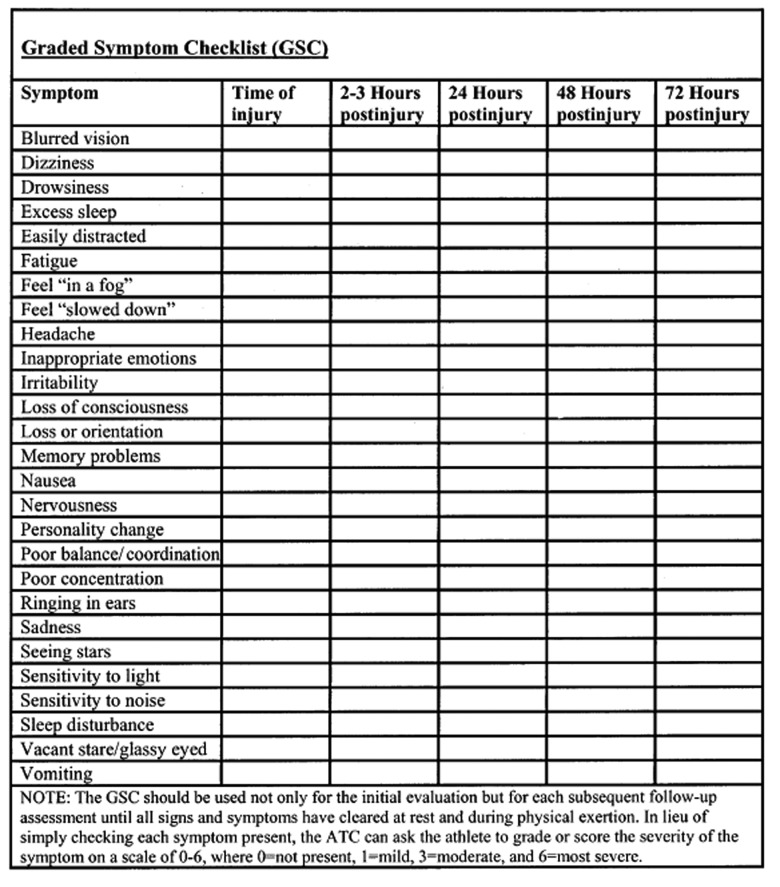
A follow-up series of questions should address the presence or absence of concussion-related symptoms—a number of which have been identified. The National Athletic Trainers’ Association recommends the use of the Graded Symptom Checklist (Figure 1),15 although a number of similar assessment tools are available.21,34,35 These scales implement a Likert-type rating of concussion-related symptoms, permitting the quantification of severity and/or duration. The presentation of symptoms will vary widely between concussed individuals, but some symptoms appear more often than others. For instance, headache has been reported in up to 83% of concussed athletes, whereas dizziness (65%) and confusion (57%) may also appear but less frequently.9,16,19,29 Some athletes who are removed from the field of play may report symptoms related to dehydration (up to 2.5%) and not injury.33 Notably, the notion that loss of consciousness must occur for the injury to be classified as a concussion is obsolete because only 10% of all concussions result in this clinical sign.23 Regardless of which signs and symptoms appear, the endorsement of any symptom related to a concussion is enough to withhold an athlete from play.
Figure 1.
The Graded Symptom Checklist. Reprinted with permission from The Journal of Athletic Training.15
Observation and Palpation
Observation and palpation of the athlete can be completed throughout the injury evaluation process. Attention should be paid to variance in the athlete’s normal speech pattern, with difficulty finding or saying the correct words when responding to questions (ie, aphasia).37 Pupil size, reaction to light, and fluidity of eye movement in multiple directions (ie, nystagmus) should also be noted. Furthermore, an evaluation of pulse and blood pressure should be completed to rule out a life-threatening condition. A high pulse pressure (ie, systolic minus diastolic > 60 mmHg) immediately following exercise is a common result of increased stroke volume8 but should restore itself within 10 minutes. If the pulse pressure remains high and is combined with a pulse rate that is substantially lower than that expected following physical exertion, the athlete may be suffering from increased intracranial pressure possibly attributed to a brain hemorrhage.38
A clinical examination that reveals abnormalities in any of these areas suggests that the injury is more significant than a concussion and so warrants immediate transport and examination at a medical facility. The cervical spine and facial bones should be palpated to rule out fractures or other trauma to these areas.
Special Tests
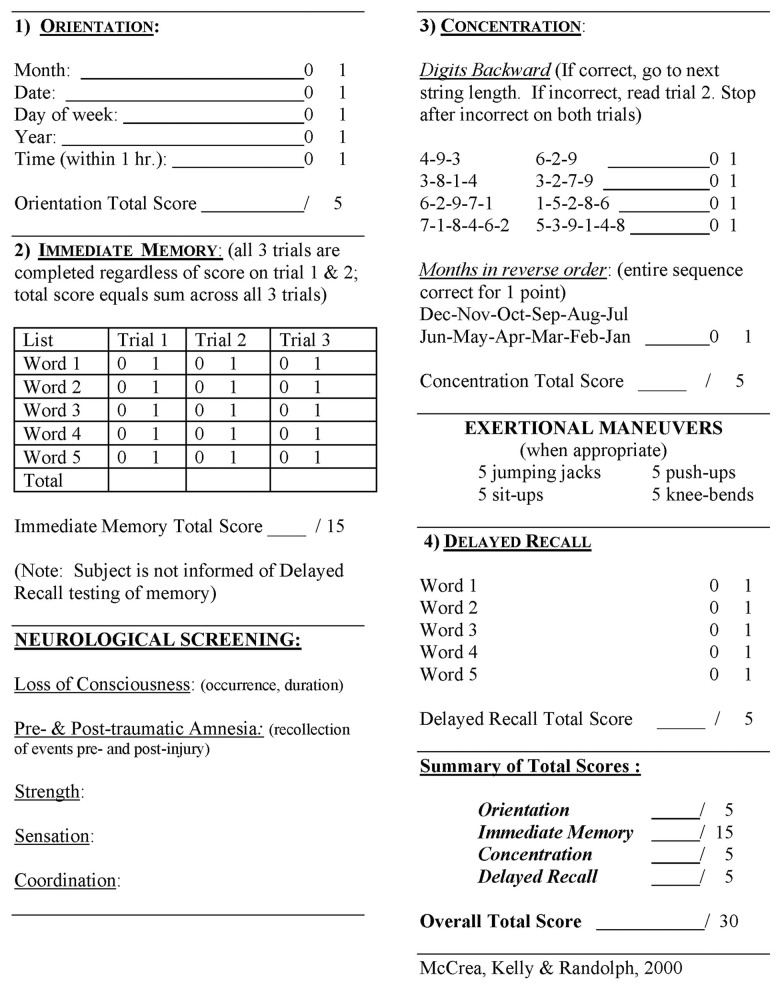
Special tests to evaluate for concussion on the sideline should consist of an evaluation of neurocognitive status, postural control, and cranial nerve integrity. Although a variety of tests and questions have been implemented in the past, traditional evaluations of concentration have been found to be insensitive to the effects of concussion—such as the serial seven examination and asking questions such as “What is your name?”24,28 Alternatively, the Standardized Assessment of Concussion (SAC) was developed as a quick and reliable mental status exam for the field practitioner.28 Different from more comprehensive pen-and-paper or computer-based neurocognitive assessments, the SAC does not require training in neuropsychology for the purposes of administration or interpretation.25 These characteristics make it an ideal test for administration on the sideline, requiring only 5 or 6 minutes.
The SAC consists of 4 sections that evaluate the areas of orientation, immediate memory, concentration, and delayed recall (Figure 2); a brief screening is included to rule out gross neurological deficiencies. Performance on the cognitive domains is summed for a total possible score of 30. The most accurate postmorbid assessment is completed when the postinjury score is compared to a preseason baseline assessment. Multiple versions of the SAC are available to reduce potential practice effects associated with multiple test administrations. Performance decrements of 1 point or more are consistent with impaired cognitive functioning following concussion. Specifically, when the assessment is administered immediately following injury, a 94% sensitivity and 76% specificity are obtained when a 1-point drop in test performance is used as a cutoff for concussion.3 A follow-up investigation yielded similar sensitivity (80%) and specificity (91%) when concussed and control athletes were evaluated at similar time points following injury.26 Other sideline assessment measures, such as the Sideline Concussion Assessment Tool,30 have similar uses in sports medicine but are limited by undefined psychometric properties and evolving content.30,31
Figure 2.
The Standardized Assessment of Concussion. Reprinted with permission from M. McCrea.
A decreased ability to maintain balance is one of the hallmark signs of concussion. Concussed individuals will commonly show increased postural sway following injury, the degree of which will often increase when the eyes are closed, thereby removing visual referencing. The Romberg test follows this protocol and has been used clinically.36 The test, however, is limited by the subjective nature of the postinjury interpretation, and it has never been validated for clinical management of sport concussion. The Balance Error Scoring System (BESS), however, was developed as an objective postural control measure that can be implemented on the sideline,36 and it has been studied extensively for the past 10 years. The BESS test is conducted under 6 stance conditions (Figure 3): a double-leg stance, single-leg stance, and heel-to-toe tandem stance—all on a firm surface, then all on a compliant foam surface (Alcan Airex AG, Switzerland). Each stance is evaluated for 20 seconds, and the athlete places his or her hands on the hips with the eyes closed. During the trials, the number of errors that the athlete commits are counted (Table 1), with a higher number of errors representing suppressed balance. An increase of 3 errors or more over the baseline score may represent a significant change indicative of a balance impairment,40 with a sensitivity to concussion reported at 34% and with the specificity at 91%.26
Figure 3.
Stances for the Balance Error Scoring System.
Table 1.
Balance Error Scoring System countable errors.18
| Errors |
|---|
| Hands lifted off the iliac crests |
| Opening eyes |
| Step, stumble, or fall |
| Moving the hip into more than 30° of flexion or extension |
| Lifting the forefoot or heel |
| Remaining out of the testing position for more than 5 seconds |
Similar to the SAC assessment, an individualized approach to interpreting the postinjury BESS scores provides the clinician with the most accurate information. Thus, comparing the postconcussion assessment to the athlete’s baseline assessment is recommended. Certain factors should be noted to obtain the most accurate results. For example, application of an external ankle support (eg, taping or bracing) has been shown to negatively influence BESS scores.4 Thus, when athletes are evaluated on the sideline, it may be necessary to remove any ankle support not present at the time of baseline testing. Furthermore, Wilkins et al41 noted a decrease in BESS performance when individuals were subjected to a 20-minute fatigue protocol. Athletes removed from a competition for an injury evaluation are likely experiencing some level of fatigue, thereby necessitating some pretest rest (13 to 20 minutes12,39).
If a significant increase in the athlete’s presentation of symptoms, SAC score (1 or more point decrement3), or BESS score (3 or more point increase40) is present during the sideline evaluation, the athlete should be removed from play. In the event that the SAC and BESS scores are normal in the postinjury evaluation and the symptoms resolve within 20 minutes, the athlete should still be withheld. Emerging evidence has revealed that symptoms may continue evolving in the subsequent hours following injury16 and that concussed athletes whose symptoms resolved within 25 minutes of injury have displayed impaired neurocognitive function 36 hours following the trauma.22
Although complete disruption of one or more cranial nerves is rare in the sporting context, the cranial nerves may be impaired as a result of the concussive blow. The assessment of many cranial nerves is imbedded throughout the concussion assessment (eg, CN VIII is evaluated during the BESS test), but the integrity of the remaining nerves should be appraised as part of the sideline assessment (Table 2). A cranial nerve assessment revealing functional decrements may indicate a more severe injury and so warrant a timely assessment at a medical facility.
Table 2.
Cranial nerve functions with suggested field tests.a
| No. | Name | Function | Nerve Type | Clinical Assessment |
|---|---|---|---|---|
| I | Olfactory | Smell | Sensory | Provide distinct smelling objects |
| II | Optic | Visual acuity | Sensory | Read small print |
| IIIb | Oculomotor | Pupillary reaction | Motor | Shine light in each eye to assess reaction: upward, downward, and medial gaze |
| IVb | Trochlear | Eye movement | Motor | Have eye follow finger downward and laterally without moving head |
| V | Trigeminal | Mastication and facial sensation | Both | Identify location of touch about face, hold mouth open against resistance, clench teeth |
| VIb | Abducens | Lateral eye movement | Motor | Have patient move eyes from side to side, lateral gaze |
| VII | Facial | Facial expressions and taste | Both | Smile, wrinkle forehead, wink, puff cheeks, close eyes tight, identify tastes with anterior tongue |
| VIIIc | Vestibulocochlear | Equilibrium and hearing | Sensory | Identify sounds, balance assessment |
| IX | Glossopharyngeal | Voice and swallow | Both | Say “ah,” swallow, test gag reflex |
| Xd | Vagus | Voice and gag reflex | Both | Hoarse voice, test gag reflex |
| XIe | Accessory | Neck strength: sternocleidomastoid and trapezius | Motor | Resist head rotation and shoulder shrugs |
| XII | Hypoglossal | Tongue movement | Motor | Stick out tongue, resist with tongue depressor |
Adapted from Moore and Dalley.32
Evaluated during the observation portion of the concussion assessment.
Evaluated during the special tests when performing the Balance Error Scoring System or other balance tests.
Evaluated when obtaining a history from the athlete.
Evaluated when performing manual muscle tests on the athlete.
Manual Muscle Testing
Should the symptom reports and BESS and SAC scores all appear normal, manual muscle testing and an evaluation of the neck’s range of motion should follow. Range of motion for flexion, extension, and rotation in both directions should be conducted actively and passively; manual muscle testing in the same directions should be similarly performed. If limitations are noted in either range of motion or muscle strength, the athlete should be withheld for additional evaluation. Limitations in these areas may place the athlete at risk for further injury by restricting his or her ability to scan the field for oncoming opponents, or it may reduce his or her ability to brace for a pending impact.
Functional Testing
The final step in the sideline concussion assessment is the functional testing of the athlete. Functional testing should not be confused with same-day return-to-play decision making, which is not recommended in most instances. Rather, functional testing should be completed only if the athlete has performed at or above the baseline level of evaluation on concussion-related symptoms, BESS, and SAC and there are no other contraindications that appeared during the remainder of the clinical examination. Functional testing is performed to elicit symptoms that may occur under the physical demands that the athlete will face once he or she returns to play. A progressive approach to the physical activity should be taken—namely, asking whether concussion-related symptoms have been elicited before moving to the next step. Simple tasks such as a Valsalva maneuver, push-ups, and sit-ups should be performed first, followed by jogging and short sprints. In the final step, the athlete should be able to complete a series of sport-specific activities at an intensity necessitated by the level of play. At each step in the progression, the athlete should be asked whether concussion-related symptoms have emerged. If symptoms have resulted from the exertion, then the athlete should not be allowed back into play. If no symptoms emerge and all other tests demonstrate normal findings, the athlete has likely not sustained a concussion and can thus return to play.
Conclusion
There is no doubt that concussion remains one of the most complicated injuries faced by athletic trainers and other medical personnel. The injury typically has no visible signs, thus leaving a heavy reliance on the keen eye of medical personnel to detect subtle differences in the athlete. Furthermore, no diagnostic test is available for this injury, which leaves the clinical examination and a battery of indirect objective tests as the primary means of clinical diagnosis. The clinical examination of concussion should follow the same systematic process used with orthopaedic injuries. After conducting a primary survey, the examiner should garner an injury history and observe and palpate the athlete for indications of more severe trauma. Special tests for mental status and postural control, along with reports of concussion-related symptoms, will provide the objective information that supports the clinical exam. Use of assessment tools that evaluate each domain provides the highest sensitivity (94%) and specificity (89%) to concussion26 and so gives the clinician the most information to make an informed decision. If these tests appear normal, range of motion of the neck and manual muscle testing of the surrounding musculature should be completed to reduce the risk of subsequent injury. Finally, should all these measures indicate a healthy status, a functional evaluation should be completed. Throughout the evaluation process, the medical team should inquire about the development, presence, intensity, or return of concussion-related symptoms. In no instance should an athlete return to play if he or she reports a symptom consistent with concussion, substantiating the dictum “When in doubt, sit them out.”5 In the end, the management of and return to participation following a sports-related concussion should involve a team approach, which includes educating athletes, parents, and coaches about the injury. Consultation with a physician may be necessary on the day of injury, but it is mandated in all cases before a return to participation (Table 3).
Table 3.
Physician referral checklist.15
| Immediate Referral (Day of Injury) |
|---|
| 1. Loss of consciousness on the field |
| 2. Amnesia lasting longer than 15 minutes |
| 3. Deterioration of neurologic functiona |
| 4. Decreasing level of consciousnessa |
| 5. Decrease or irregularity in respirationsa |
| 6. Decrease or irregularity in pulsea |
| 7. Increase in blood pressure |
| 8. Unequal, dilated, or unreactive pupilsa |
| 9. Cranial nerve deficits |
| 10. Any signs or symptoms of associated injuries, spine or skull fracture, or bleedinga |
| 11. Mental status changes: lethargy, difficulty maintaining arousal, confusion, agitationa |
| 12. Seizure activitya |
| 13. Vomiting |
| 14. Motor deficits subsequent to initial on-field assessment |
| 15. Sensory deficits subsequent to initial on-field assessment |
| 16. Balance deficits subsequent to initial on-field assessment |
| 17. Cranial nerve deficits subsequent to initial on-field assessment |
| 18. Postconcussion symptoms that worsen |
| 19. Additional postconcussion symptoms as compared with those on the field |
| 20. Athlete still symptomatic at the end of the game (especially at high school level) |
| Delayed Referral (After the Day of Injury) |
| 1. Any of the findings in the day-of-injury referral category |
| 2. Postconcussion symptoms worsen or do not improve over time |
| 3. Increase in the number of postconcussion symptoms reported |
| 4. Postconcussion symptoms begin to interfere with the athlete’s daily activities (eg, sleep disturbances, cognitive difficulties) |
Requires that the athlete be immediately transported to the nearest emergency department.
Footnotes
No potential conflict of interest declared.
NATA Members:Receive 3 free CEUs each year when you subscribe to Sports Health and take and pass the related online quizzes! Not a subscriber? Not a member? The Sports Health–related quizzes are also available for purchase. For more information and to take the quiz for this article, visit www.nata.org/sportshealthquizzes.
References
- 1. Agel J, Dick R, Nelson B, Marshall SW. Descriptive epidemiology of collegiate women’s ice hockey injuries: National Collegiate Athletic Association Injury Surveillance System, 2000-2001 through 2003-2004. J Athl Train. 2007;42(2):249-254 [PMC free article] [PubMed] [Google Scholar]
- 2. Aubry M, Cantu R, Dvorak J, et al. Summary and agreement statement of the first International Conference on Concussion in Sport, Vienna 2001. Br J Sports Med. 2002;36(1):6-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Barr WB, McCrea M. Sensitivity and specificity of standardized neurocognitive testing immediately following sports concussion. J Int Neuropsychol Soc. 2001;7(6):693-702 [DOI] [PubMed] [Google Scholar]
- 4. Broglio SP, Monk A, Sopiarz K, Cooper ER. The influence of ankle support on postural control. J Sci Med Sport. 2009;12(3):388-392 [DOI] [PubMed] [Google Scholar]
- 5. Cantu RC. Athletic concussion: current understanding as of 2007. Neurosurgery. 2007;60(6):963-964 [DOI] [PubMed] [Google Scholar]
- 6. Center for Disease Control Sports-related recurrent brain injuries: United States. MMRW. 1997;46(10):224-227 [PubMed] [Google Scholar]
- 7. Collins MW, Grindel SH, Lovell MR, et al. Relationship between concussion and neuropsychological performance in college football players. JAMA. 1999;282(10):964-970 [DOI] [PubMed] [Google Scholar]
- 8. Dart AM, Kingwell BA. Pulse pressure: a review of mechanisms and clinical relevance. J Am Coll Cardiol. 2001;37(4):975-984 [DOI] [PubMed] [Google Scholar]
- 9. Delaney JS, Lacroix VJ, Leclerc S, Johnston KM. Concussions among university football and soccer players. Clin J Sport Med. 2002;12(6):331-338 [DOI] [PubMed] [Google Scholar]
- 10. Dick R, Agel J, Marshall SW. National Collegiate Athletic Association Injury Surveillance System commentaries: introduction and methods. J Athl Train. 2007;42(2):173-182 [PMC free article] [PubMed] [Google Scholar]
- 11. Field M, Collins MW, Lovell MR, Maroon JC. Does age play a role in recovery from sports-related concussion? A comparison of high school and collegiate athletes. J Pediatr. 2003;142(5):546-553 [DOI] [PubMed] [Google Scholar]
- 12. Fox ZG, Mihalik JP, Blackburn JT, Battaglini CL, Guskiewicz KM. Return of postural control to baseline after anaerobic and aerobic exercise protocols. J Athl Train. 2008;43(5):456-463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Giza CC, Hovda DA. The neurometabolic cascade of concussion. J Athl Train. 2001;36(3):228-235 [PMC free article] [PubMed] [Google Scholar]
- 14. Grindel SH, Lovell MR, Collins MW. The assessment of sport-related concussion: the evidence behind neuropsychological testing and management. Clin J Sport Med. 2001;11(3):134-143 [DOI] [PubMed] [Google Scholar]
- 15. Guskiewicz KM, Bruce SL, Cantu RC, et al. National Athletic Trainers’ Association position statement: management of sport-related concussion. J Athl Train. 2004;29(3):280-297 [PMC free article] [PubMed] [Google Scholar]
- 16. Guskiewicz KM, McCrea M, Marshall SW, et al. Cumulative effects associated with recurrent concussion in collegiate football players: the NCAA concussion study. JAMA. 2003;290(19):2549-2555 [DOI] [PubMed] [Google Scholar]
- 17. Guskiewicz KM, Mihalik JP, Shankar V, et al. Measurement of head impacts in collegiate football players: relationship between head impact biomechanics and acute clinical outcome after concussion. Neurosurgery. 2007;61(6):1244-1252 [DOI] [PubMed] [Google Scholar]
- 18. Guskiewicz KM, Ross SE, Marshall SW. Postural stability and neuropsychological deficits after concussion in collegiate athletes. J Athl Train. 2001;36(3):263-273 [PMC free article] [PubMed] [Google Scholar]
- 19. Guskiewicz KM, Weaver NL, Padua DA, Garrett WE. Epidemiology of concussion in collegiate and high school football players. Am J Sports Med. 2000;28(5):643-650 [DOI] [PubMed] [Google Scholar]
- 20. Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil. 2006;21(5):375-378 [DOI] [PubMed] [Google Scholar]
- 21. Lovell MR, Collins MW. Neuropsychological assessment of the college football player. J Head Trauma Rehabil. 1998;13(2):9-26 [DOI] [PubMed] [Google Scholar]
- 22. Lovell MR, Collins MW, Iverson GL, Johnston K, Bradley JP. Grade 1 or “ding” concussions in high school athletes. Am J Sports Med. 2004;32(1):47-54 [DOI] [PubMed] [Google Scholar]
- 23. Lovell MR, Iverson GL, Collins MW, McKeag DB, Maroon JC. Does loss of consciousness predict neuropsychological decrements after concussion? Clin J Sport Med. 1999;9(4):193-198 [DOI] [PubMed] [Google Scholar]
- 24. Maddocks DL, Dicker GD, Saling MM. The assessment of orientation following concussion in athletes. Clin J Sport Med. 1995;5(1):32-35 [DOI] [PubMed] [Google Scholar]
- 25. McCrea M. Standardized mental status assessment of sports concussion. Clin J Sport Med. 2001;11(3):176-181 [DOI] [PubMed] [Google Scholar]
- 26. McCrea M, Barr WB, Guskiewicz KM, et al. Standard regression-based methods for measuring recovery after sport-related concussion. J Int Neuropsychol Soc. 2005;11:58-69 [DOI] [PubMed] [Google Scholar]
- 27. McCrea M, Hammeke T, Olsen G, Leo P, Guskiewicz K. Unreported concussion in high school football players: implications for prevention. Clin J Sport Med. 2004;14(1):13-17 [DOI] [PubMed] [Google Scholar]
- 28. McCrea M, Kelly JP, Kluge J, Ackley B, Randolph C. Standardized assessment of concussion in football players. Neurology. 1997;48(3): 586-588 [DOI] [PubMed] [Google Scholar]
- 29. McCrory PR, Ariens M, Berkovic SF. The nature and duration of acute concussive symptoms in Australian football. Clin J Sport Med. 2000;10: 235-238 [DOI] [PubMed] [Google Scholar]
- 30. McCrory P, Johnston K, Meeuwisse W, et al. Summary and agreement statement of the second International Conference on Concussion in Sport, Prague 2004. Br J Sports Med 2005;39(4):196-204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. McCrory P, Meeuwisse W, Johnston K, et al. Consensus statement on concussion in sport: the 3rd International Conference on Concussion in Sport held in Zurich, November 2008. Clin J Sport Med 2009;19: 185-200 [DOI] [PubMed] [Google Scholar]
- 32. Moore KL, Dalley AF, eds. Summary of cranial nerves. In: Clinically Oriented Anatomy. 4th ed. Philidelphia, PA: Lippincott Williams & Wilkins; 1999:1082-1111 [Google Scholar]
- 33. Patel AV, Mihalik JP, Notebaert AJ, Guskiewicz KM, Prentice WE. Neuropsychological performance, postural stability, and symptoms after dehydration. J Athl Train. 2007;42(1):66-75 [PMC free article] [PubMed] [Google Scholar]
- 34. Piland SG, Motl RW, Ferrara MS, Peterson CL. Evidence for the factorial and construct validity of a self-report concussion symptoms scale. J Athl Train. 2003;38(2):104-112 [PMC free article] [PubMed] [Google Scholar]
- 35. Potter S, Leigh E, Wade D, Fleminger S. The Rivermead Post Concussion Symptoms Questionnaire: a confirmatory factor analysis. J Neurol. 2006;253(12):1603-1614 [DOI] [PubMed] [Google Scholar]
- 36. Riemann BL, Guskiewicz KM, Shields EW. Relationship between clinical and forceplate measures of postural stability. J Sport Rehabil. 1999;8(2):71-82 [Google Scholar]
- 37. Ropper AH, Gorson KC. Clinical practice: concussion. N Engl J Med. 2007;356(2):166-172 [DOI] [PubMed] [Google Scholar]
- 38. Sanders MJ, McKenna K. Head and facial trauma. In: Mosby’s Paramedic Textbook. 2nd ed. St Louis, MO: Mosby; 2001:624-651 [Google Scholar]
- 39. Susco TM, Valovich McLeod TC, Gansneder BM, Shultz SJ. Balance recovers within 20 minutes after exertion as measured by the Balance Error Scoring System. J Athl Train. 2004;39(3): 241-246 [PMC free article] [PubMed] [Google Scholar]
- 40. Valovich McLeod TC, Barr WB, McCrea M, Guskiewicz KM. Psychometric and measurement properties of concussion assessment tools in youth sports. J Athl Train. 2006;41(4):399-408 [PMC free article] [PubMed] [Google Scholar]
- 41. Wilkins JC, Valovich TC, Perrin DH, Gansneder BM. Performance on the Balance Error Scoring System decreases after fatigue. J Athl Train. 2004;39(2):156-161 [PMC free article] [PubMed] [Google Scholar]