Abstract
A professional baseball player presented to the orthopaedic clinic for a preseason assessment because of continued lumbar spine and flank pain. He had a laparoscopic appendectomy for a perforated appendix 8 months before his presentation. He was able to finish the previous season with only mild limitation. He presented with back pain that limited his activity. His examination was nonlocalizing, but subsequent computed tomography revealed a hepatic abscess. The abscess was drained; he was treated with intravenous antibiotics; and his symptoms resolved.
Keywords: low back pain, liver abscess, baseball, magnetic resonance imaging, preseason physical
Low back pain (LBP) is an extremely common complaint in athletes; estimates of its prevalence range from 1% to more than 30%.3,20 The differential diagnosis of LBP in athletes includes musculoskeletal conditions and many other visceral or metabolic causes. Mechanical LBP and leg pain with spinal causes compose approximately 97% of the diagnoses.7 Nonmechanical spinal conditions—including neoplasia, infection, inflammatory arthritis, Scheuermann disease, and Paget disease—are estimated to cause approximately 1% of the cases of LBP.7 Other uncommon causes of back pain include diseases of the pelvic organs, renal malfunction, aortic aneurysm, and gastrointestinal problems.7
In athletes, LBP is common and most frequently a result of self-limited musculoskeletal causes.2 In baseball players, LBP is a common cause of disability, accounting for approximately 15% of their injuries and 5% of their disabled-list days.6,13 The present case is important for clinicians who perform preseason physical examinations and who see athletes with LBP. It reminds them to carefully correlate the symptoms and examination findings of LBP with the medical history.
Case Report
Early in the baseball season, a 23-year-old male professional minor league baseball player developed an insidious onset of midepigastric and midabdominal pain that later localized to the right lower quadrant. The pain worsened until it disrupted his sleep, prevented him from standing straight, and decreased his appetite. Three days later, his pain was severe enough to seek evaluation in an emergency room, where he was diagnosed with acute appendicitis on the basis of blood tests, radiographs, and an abdominal computed tomography (CT) scan. The CT scan showed a dilated inflamed appendix, an appendicolith, and moderate free fluid in the pelvis. A laparoscopic appendectomy was performed within 12 hours, which revealed an inflamed omentum on top of the acutely inflamed appendix but no localized abscess. Drains were not placed in the wound postoperatively. There was no free perforation or gangrene noted intraoperatively; however, pathologic examination of the specimen indicated a ragged-edge defect in the wall of the appendix consistent with perforation.
The morning after surgery, the patient had an elevated white blood cell count of 21 000 (an increase from 16 300 on the previous day) and a slight fever. As a result, he received intravenous (IV) antibiotics as an inpatient for 2 days. His white blood cell count subsequently returned to normal, and his fever resolved. He was discharged at 3 days postsurgery and sent back to the team without additional antibiotics.
Seven days after surgery, he was reevaluated because of fatigue and intermittent low fevers (maximum, 102°F [39°C]). He complained of mild abdominal pain, increased urinary frequency, and nocturia. Despite a normal urinalysis, he was treated by a team physician for a presumed urinary tract infection with a course of oral azithromycin (500 mg on day 1, then 250 mg for the next 4 days).
Despite this treatment, he continued to have abdominal pain, and complained of loss of appetite, sweats, fevers, and chills. He was evaluated at a different hospital emergency room 11 days after surgery, where he was febrile with an elevated white blood cell count. A triple-contrast IV-oral-rectal spiral CT scan of his abdomen and pelvis identified a moderate-sized abscess (4.1 × 7.6 cm) in the pelvis between the bladder and the rectum and moderate inflammation in the area of the removed appendix. He also had bilateral small pleural effusions with a concomitant infiltrate or atelectasis. He was treated with IV antibiotics. At the time, he was in the middle of his baseball season and an invasive procedure would have set him back in his professional career. He was admitted to the hospital and prescribed IV piperacillin/tazobactam (3.375 g every 6 hours).
Despite this treatment, he continued to have moderate, constant, but nonradiating pain in the right lower quadrant. He was not septic and did not have wound drainage. On the third day of this admission, a peripherally inserted central catheter was established. His white count normalized; his temperature returned to normal; and he was discharged the next day with arrangements to finish the 1-week course of IV antibiotics at home via the catheter line.
Two days after his last dose of antibiotics, an abdominal CT scan showed that the pelvic abscess had diminished in size. An abdominal magnetic resonance imaging (MRI) scan was performed the next day for continued right upper-quadrant pain. The MRI results were unremarkable. The radiologist did note a benign hepatic hemangioma along the posterior margin of the right liver lobe (Figure 1).
Figure 1.

Axial magnetic resonance imaging views of the liver at the time of presentation: A, axial T1-weighted image showing an ovoid structure of low signal intensity in the liver (spin echo, repetition / echo time = 500/9 ms); B, axial T2-weighted image showing signal intensity greater than that of the spleen (fast spin echo, repetition / echo time = 52 501 / 105 ms); C, axial T1-weighted image after contrast administration in the venous phase showing noninterrupted peripheral enhancement of the lesion (fast spoiled gradient echo, repetition / echo time = 170 / 4.2 ms; flip angle, 70°). The characteristics exhibited do not meet established criteria for a hemangioma.
An orthopaedic evaluation by one of the minor league team physicians the following day yielded no restrictions from his residual back pain; thus, he was cleared to begin light activity. The physician elected not to repeat any studies to evaluate the pelvic abscess. Four weeks later, the player was allowed to return to unrestricted participation in minor league baseball. Despite a negative examination, he continued to have LBP. He was treated symptomatically with anti-inflammatory medications, cryotherapy, and physical therapy. He did not experience pain when active but had difficulty with activities of daily living, including getting out of bed, leaning over to tie his shoes, and inspiring deeply. He also could not lie on his right side because of the pain. By the end of the season (6 months later), his pain worsened, he was fatigued, and he periodically had low-grade fevers up to 100.5°F (38.1°C). He was reevaluated with radiographs of his abdomen. He was diagnosed with a bruised rib and treated with anti-inflammatory medication and physical therapy.
The training room staff was concerned with his continued right flank pain. At presentation to the orthopaedic clinic (8 months postappendectomy), he complained of LBP in the right upper lumbar region, as well as right flank pain. He commented that his back soreness was similar to what he had felt after his appendectomy. It did not radiate into his groin or around to his abdomen. He had no paresthesias or lower extremity weakness. He did continue to have intermittent fever, chills, and night sweats. His weight had been stable with a normal appetite, and he did not have bowel or bladder dysfunction.
On examination he appeared in mild distress because of his pain. His vital signs were stable, and he was afebrile (temperature = 98.6°F [37°C]). He had full range of motion of his lumbar spine with mild discomfort in the right flank area with lateral bending. He also had tenderness to palpation of the right costovertebral angle and the right lateral lumbar area. His abdominal examination was notable for mild right upper-quadrant tenderness to palpation and mild tenderness in the perinephric area. He had no signs of nerve root irritation and no long tract signs.
Conventional radiographs of his chest, thoracic spine, lumbar spine, and abdomen were negative. An abdominal CT scan of the abdomen with oral and IV contrast revealed a moderate-sized hepatic abscess (5.2 × 7.4 cm) with hepatic perfusion changes consistent with inflammation surrounding the lesion (total area 11 × 7.5 cm; Figure 2). The abscess extended through the retroperitoneal fat, into the posterior transversus abdominis muscle. Blood work showed a white blood cell count of 8400 with a left shift. Results of liver function tests were within normal limits, except that albumin was decreased to 3.3 g/dL (normal, 3.5 to 5.5 g/dL).
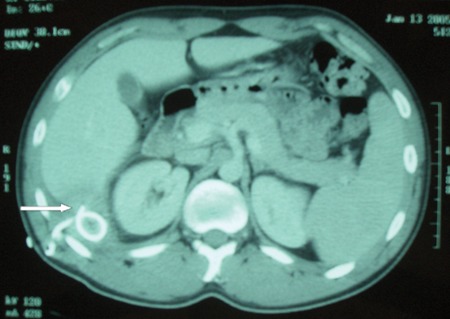
Figure 2.

Axial postcontrast computed tomography image showing a rim-enhancing fluid collection (5 × 7 cm) with surrounding hepatic perfusion changes.
The patient underwent CT-guided percutaneous drainage of the abscess (Figure 3). Grossly purulent material drained over the next 2 days. The culture showed many polymorphonuclear leukocytes, gram-negative pleomorphic bacilli, small bacilli, moderate gram-positive cocci in pairs, aerobic beta Streptococcus that could not be specified (not group A, B, or D), and anaerobic bacteroides fragilis, Peptostreptococcus, and fusobacterium. The patient was started on imipenem (500 mg IV every 6 hours). A peripherally inserted central catheter line was placed in the upper superior vena cava region for long-term antibiotic administration. A repeat abdominal CT with contrast 5 days later revealed a small right pleural effusion and a small amount of fluid beneath the right hemidiaphragm posteriorly. Decreased inflammatory change without any obvious residual fluid collection was also noted.
Figure 3.
Axial postcontrast computed tomography image showing the percutaneous drain in the fluid collection.
After 7 days in the hospital, the patient was discharged with a catheter to drain the abscess and was placed on ertapenem (1 g IV daily for 2 weeks). The catheter was removed 5 weeks after its insertion when a CT scan showed near resolution of the abscess. A CT scan performed 3 weeks later showed that the abscess had cleared (Figure 4). The patient was allowed progressive athletic activity, and 9 weeks after his hospitalization he returned to professional baseball with no restrictions and resolution of his back pain.
Figure 4.

Axial postcontrast computed tomography image showing minimal residual perihepatic fluid and/or scarring without a definable fluid collection.
Discussion
This case reminds clinicians of the importance of obtaining a good history when evaluating athletes complaining of LBP. This patient had seen multiple providers, without the diagnosis of an abdominal process as a cause of his symptoms. Several physicians assumed that he had mechanical LBP. Because the physical examination of the abdomen may not localize, a thorough history can be beneficial in the diagnosis. Similarly, this case emphasizes the importance of distinguishing between a hepatic abscess and a benign hepatic hemangioma on CT or MRI scans.
The liver is the abdominal organ most susceptible to abscess formation, and the most common cause is bacterial infection of the portal and biliary tracts.1 Before antibiotics, appendicitis was the most common source of pyogenic liver abscess (PLA).1 The most frequent other causes of PLA include diverticulitis, pylephlebitis, inflammatory bowel disease, and bacterial endocarditis.19 The cause is unknown in up to 20% of patients with PLA.4
Despite the low incidence of postoperative abdominal infection, a febrile patient postsurgery must be carefully examined. This patient’s postoperative fever was initially misdiagnosed as a urinary tract infection, which did not respond to antibiotic treatment. This confusion likely resulted from the frequent urination and dysuria. Fever, however, is the most common presenting symptom of a liver abscess (90% of patients). Nonspecific symptoms such as chills (38% to 49%), anorexia (38%), weight loss (25% to 43%), nausea and vomiting (28% to 43%), weakness and malaise (30%) may also be present. Fifty percent of patients with a liver abscess have hepatomegaly, right upper-quadrant tenderness, or jaundice.9,14,16,17 With a liver abscess, 70% to 90% have elevated serum alkaline phosphatase, 50% have elevated serum bilirubin, and 48% have elevated aspartate aminotransferase.9,16,17 Patients with a liver abscess also have leukocytosis (77%), anemia (50%), and hypoalbuminemia (33%).9,14,16,17 Elevation of the right hemidiaphragm, a right basilar infiltrate, or a unilateral pleural effusion may also be seen.9,16,17
Bacterial speciation of PLA depends on the source of infection. Intra-abdominal sources often produce gram-positive and gram-negative aerobes and anaerobes. Common species include Escherichia coli, Klebsiella pneumonia, and Bacteroides fragilis. PLA from bacterial endocarditis may yield gram-positive aerobes such as Staphylococcus aureus or Streptococcus pyogenes.19
Antibiotic therapy should be directed to the cultured organisms; first-line treatment includes broad-spectrum antibiotic coverage.18 Percutaneous drainage should be considered for abscesses larger than 5 cm. Repeat CT scanning is indicated in those with continued pain and a leukocytosis. Although sensitive, the C-reactive protein and sedimentation rate are not necessary if the symptoms are resolving. Physical examination and a white blood cell count are typically sufficient to determine the effectiveness of the treatment. Open surgical drainage should be considered if the abscess is multiloculated or ruptured.5 Surgical intervention may also be necessary to treat the cause of the PLA (eg, severe diverticulitis).
The MRI scan was interpreted as an incidental benign hepatic hemangioma, but the features of the lesion did not meet the criteria for that diagnosis. MRI has a sensitivity of approximately 90% and a specificity of 91% to 99% for hemangiomas.10,12 The characteristic features of a hepatic hemangioma are decreased signal intensity on T1-weighted images. Increased signal intensity on T2-weighted images with a nodular, discontinuous peripheral enhancement; and gradual fill-in on delayed postcontrast imaging is expected.12
The diagnostic methods of choice for detecting a liver abscess are ultrasound and CT.21 MRI can also be used for characterizing liver lesions. MRI can present a confusing picture of an abscess because the signal intensity of an abscess on T1- and T2-weighted MRIs can vary depending on the protein content of the lesion.15 Liver abscesses on contrast-enhanced CT typically appear as well-defined hypoattenuating lesions with faint rim enhancement and perilesional edema.15 Large abscesses may be unilocular with smooth margins or complex with internal septa and irregular contours.15 The presence of gas in the lesion is relatively uncommon but is a helpful clue to the diagnosis of an abscess.8,11
In summary, this case illustrates the importance of the history in the evaluation and treatment of athletes with LBP. The pain and constitutional symptoms led to the successful diagnosis of a liver abscess. The use of imaging and blood studies are indicated when there is a high index of suspicion for visceral causes of LBP.
Footnotes
No potential conflict of interest declared.
References
- 1. Altemeier WA, Culbertson WR, Fullen WD, Shook CD. Intra-abdominal abscesses. Am J Surg. 1973;125(1):70-78 [DOI] [PubMed] [Google Scholar]
- 2. Baker RJ, Patel D. Lower back pain in the athlete: common conditions and treatment. Prim Care. 2005;32(1):201-229 [DOI] [PubMed] [Google Scholar]
- 3. Bono CM. Low-back pain in athletes. J Bone Joint Surg Am. 2004;86(2):382-396 [DOI] [PubMed] [Google Scholar]
- 4. Chiche L, Dargere S, Le Pennec V, Dufay C, Alkofer B. Pyogenic-liver abscess: diagnosis and management. Gastroenterol Clin Biol. 2008;32(12):1077-1091 [DOI] [PubMed] [Google Scholar]
- 5. Chung YFA, Tan YM, Lui HF, et al. Management of pyogenic liver abscesses—percutaneous or open drainage? Singapore Med J. 2007;48(12):1158-1164 [PubMed] [Google Scholar]
- 6. Conte S, Requa RK, Garrick JG. Disability days in major league baseball. Am J Sports Med. 2001;29(4):431-436 [DOI] [PubMed] [Google Scholar]
- 7. Deyo RA, Weinstein JN. Low back pain. N Engl J Med. 2001;344(5):363-370 [DOI] [PubMed] [Google Scholar]
- 8. Halvorsen RA, Korobkin M, Foster WL, Silverman PM, Thompson WM. The variable CT appearance of hepatic abscesses. AJR Am J Roentgenol. 1984;142(5):941-946 [DOI] [PubMed] [Google Scholar]
- 9. Huang CJ, Pitt HA, Lipsett PA, et al. Pyogenic hepatic abscess: changing trends over 42 years. Ann Surg. 1996;223(5):600-607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lee MG, Baker ME, Sostman HD, et al. The diagnostic accuracy/efficacy of MRI in differentiating hepatic hemangiomas from metastatic colorectal/breast carcinoma: a multiple reader ROC analysis using a jackknife technique. J Comput Assist Tomogr. 1996;20(6):905-913 [DOI] [PubMed] [Google Scholar]
- 11. Mathieu D, Vasile N, Fagniez PL, Segui S, Grably D, Larde D. Dynamic CT features of hepatic abscesses. Radiology. 1985;154(3):749-752 [DOI] [PubMed] [Google Scholar]
- 12. McFarland EG, Mayo-Smith WW, Saini S, Hahn PF, Goldberg MA, Lee MJ. Hepatic hemangiomas and malignant tumors: improved differentiation with heavily T2-weighted conventional spin-echo MR imaging. Radiology. 1994;193(1):43-47 [DOI] [PubMed] [Google Scholar]
- 13. McFarland EG, Wasik M. Epidemiology of collegiate baseball injuries. Clin J Sport Med. 1998;8(1):10-13 [DOI] [PubMed] [Google Scholar]
- 14. Mohsen AH, Green ST, Read RC, McKendrick MW. Liver abscess in adults: ten years experience in a UK centre. QJM. 2002;95(12):797-802 [DOI] [PubMed] [Google Scholar]
- 15. Mortele KJ, Segatto E, Ros PR. The infected liver: radiologic-pathologic correlation. Radiographics. 2004;24(4):937-955 [DOI] [PubMed] [Google Scholar]
- 16. Rahimian J, Wilson T, Oram V, Holzman RS. Pyogenic liver abscess: recent trends in etiology and mortality. Clin Infect Dis. 2004;39(11):1654-1659 [DOI] [PubMed] [Google Scholar]
- 17. Rubin RH, Swartz MN, Malt R. Hepatic abscess: changes in clinical, bacteriologic and therapeutic aspects. Am J Med. 1974;57(4):601-610 [DOI] [PubMed] [Google Scholar]
- 18. Schropp KP, Kaplan S, Golladay ES, et al. A randomized clinical trial of ampicillin, gentamicin and clindamycin versus cefotaxime and clindamycin in children with ruptured appendicitis. Surg Gynecol Obstet. 1991;172(5):351-356 [PubMed] [Google Scholar]
- 19. Sielaff TD, Curley SA. Liver. In: Brunicardi FC, Andersen DK, Billiar TR, Dunn DL, Hunter JG, Pollock RE, eds. Schwartz’s Principles of Surgery. 8th ed. New York, NY: McGraw-Hill; 2005:1139-1186 [Google Scholar]
- 20. Tall RL, DeVault W. Spinal injury in sport: epidemiologic considerations. Clin Sports Med. 1993;12(3):441-448 [PubMed] [Google Scholar]
- 21. Zaleznik DF, Kasper DL. Intra-abdominal abscesses. In: LaMont JT, ed. Gastrointestinal Infections: Diagnosis and Management. New York, NY: Marcel Dekker; 1997:397-409 [Google Scholar]


