Abstract
Context:
The use of high tibial osteotomies (HTOs) in elite and professional athletes has been slow to gain acceptance by both the athlete and the surgeon because it is generally thought that return to competitive sports will be unlikely. Conversely, HTOs have been used extensively and effectively in managing degenerative knee arthrosis in the less active recreational patient with varus deformity who wishes to maintain activity and delay the need for knee arthroplasty. Unfortunately, situations arise where elite athletes develop debilitating pain secondary to malalignment that prevents them from participation, at which time corrective osteotomy may be indicated. Return to sport is not necessarily the goal of osteotomy surgery, but success with correction may allow the athlete to return to high-level activity. Return to elite competition is not the singular goal of HTO in the athlete; however, if the surgery is successful, then consideration can be given to return to play.
Evidence Acquisition:
Despite an extensive literature on return to elite competition after many orthopaedic procedures, there are relatively few data following osteotomies.
Results:
With expanded indications, osteotomies have become increasingly popular in young patients with malalignment and arthrosis. In addition to addressing malalignment and degenerative processes, HTO can be used in elite athletes in combination with knee reconstructive procedures to address articular defects, meniscal deficiency, and instability, thereby optimizing knee function.
Conclusion:
When performed with the proper indications in competitive athletes, HTO can result in unloading of joint resurfacing procedures, pain reduction, increased functional stability, and restored joint mechanics. Furthermore, as performed in select elite athletes, HTO realignment may not only result in return to play but also improve function and possibly prolong competition at a high level.
Keywords: knee, tibial osteotomy, athletes, alignment
For many elite athletes, knee joint degeneration and malalignment occur by 1 of 2 mechanisms: acute trauma or repetitive overload. Traumatic joint injury—including ligamentous, meniscal, or articular injury—can lead to focal degeneration. When such an injury occurs in the setting of an associated malalignment, the injury can be exacerbated over time. With regard to repetitive overload, years of intense training and competition may accelerate the onset of arthrosis and ultimately become career threatening.16,75 Malalignment also exacerbates the problems associated with repetitive overload. Sports such as football, basketball, soccer, and others that require repetitive running, jumping, and cutting can place significant loads across weightbearing joints. These activities can result in microtrauma of articular cartilage and lead to early degenerative processes.33 Conservative treatment modalities for osteoarthritis in athletes have been extensively studied and are omnipresent at training and competition facilities. Anti-inflammatory pharmaceuticals are commonplace. Other nonsurgical treatment options for degenerative knee arthrosis include activity modification, custom orthotics, and use of hyaluronic acid or steroid injections. Recently, the use of platelet-derived growth factors has gained momentum for various orthopaedic indications, but long-term outcome studies have not been conducted on the use of them in cases of knee joint arthrosis.63 These treatments are often used in conjunction with physical therapy that uses strengthening, biofeedback, and pain-relieving modalities. Although the use of these conservative measures is routine in elite athletics, the degenerative process is often progressive. Once conservative management has failed to provide a sustainable solution, an athlete’s career may be threatened, and surgical options can be considered.
Compared with conservative treatment options, the surgical treatment of knee osteoarthritis or joint overload in the elite athlete has not been extensively studied. Three surgical approaches in this setting include arthroscopy, osteotomy, and joint replacement.47 Arthroscopy and debridement for focal and early degenerative knee arthrosis are commonly performed. Aaron et al1 studied 122 patients who underwent arthroscopic debridement of knee arthritis that was refractory to conservative management. They found that arthroscopy provided pain relief in cases of mild knee arthritis as defined by the Kellgren-Lawrence radiographic scale34 and grading of cartilage lesions intraoperatively by the Noyes system.56 However, patients with more advanced arthritis did not have favorable outcomes.1 Furthermore, many arthroscopic techniques require various activity modifications for the operation to be successful. Microfracture in athletes, for instance,20,46 sometimes requires giving up competition to facilitate favorable outcomes.
Total or unicondylar knee replacement may be an alternative for recreational athletes or those competitive athletes willing to consider retirement. However, elite-level competition in impact sports is not compatible to good long-term outcomes following joint replacement surgery. Specifically, the forces placed across a knee arthroplasty during elite athletic competition that includes running, jumping, and cutting can result in accelerated polyethylene wear, periprosthetic fractures at the sites of stress risers, debonding of the implant-cement interface, and ultimately, early failure of either total or unicondylar replacements.38,64 No known competitive jumping athlete has returned to play following knee replacement.
For those athletes with underlying knee malalignment who desire to continue competing at a high level in the face of a focal or progressive knee injury, high tibial osteotomy (HTO) may provide a plausible solution. Historically, studies have shown that HTO can reliably relieve pain and provide functional restoration in cases of unicompartmental knee osteoarthritis.18,29-32,43,48,76 None of these studies, however, focused on elite athletes or addressed ability to return to competitive athletic careers following surgery. Furthermore, these studies generally suggested that outcomes following HTO deteriorated with time.19,59 However, recent advances in technique, fixation, and postoperative care may provide the opportunity to improve outcomes compared to previous analyses of HTO. A recent Cochrane review on 13 studies of HTO concluded that despite significant deficiencies in the literature to make definitive recommendations, the surgery does improve knee function and relieve pain.† This review evaluated effectiveness and safety; it did not directly address elite athletes, nor did it judge outcomes based on ability to return to elite competition. In a review addressing young athletes, Wolcott concluded that osteotomy remains the procedure of choice for this patient population with knee malalignment and that favorable outcomes are influenced by lower relative weight, slight overcorrection, and lower level of overall knee pathology preoperatively.3,19,29,44,74 A key advantage to HTO over replacement is that HTO may allow unlimited activity following surgery, including running, jumping, and cutting. In a subjective outcome study of HTO in active individuals, Nagel et al51 found that many patients were able to return to competitive activities, including skiing, tennis, and other activities that involved running and jumping. Furthermore, 82% of patients in this study stated that in retrospect they were pleased they had the surgery. In a recent study by Salzmann et al,62 65 patients were evaluated an average of 3 years following opening-wedge HTO to assess ability to return to recreational sporting activity. Although none of the patients in the study were involved in high-level competitive or professional sports, HTO was successful in returning these patients to a similar activity level based on the Lysholm score, visual analogue score, and sport participation.
Aside from the chronic overload and microtrauma from sports, acute injuries to the meniscus, ligaments, and articular cartilage are frequent. These injuries highlight another important element of HTO: Surgery can be performed in combination with other procedures on the athlete’s knee to improve outcomes of acute soft tissue injuries. Articular defects, meniscal deficiency, and knee instability, individually or in combination, are often associated with focal compartment overload. Treatment of the instability, meniscal, or articular problem often has to be accompanied by an unloading osteotomy to ensure longevity of the soft tissue procedure.26,27,35,54,55,58,66,72 Techniques described using tibial osteotomies in combination with soft tissue procedures include meniscal repair or transplantation,72 articular resurfacing,26,27,45,64,66 and instability.11,53-55,68 By unloading the involved compartment, HTO can be beneficial to meniscus transplants if a deformity exists. Articular cartilage injuries such as osteochondral defects can be addressed with traditional procedures, such as microfracture, osteochondral autologous transplantation, or autologous chondrocyte implantation in combination with HTO to improve load dissipation.5 For patients with anterior cruciate ligament or posterior cruciate ligament (PCL) deficiency, HTO may improve sagittal stability by altering the posterior slope.4,21,24,25 In summary, osteotomies have been shown to be essential in the treatment of the symptomatic knee with malalignment associated with focal arthrosis, articular and/or meniscal deficiency, and/or instability.
Indications for Knee Osteotomy in the Elite Athlete
Knee arthritis in active patients, including competitive athletes, is increasingly common. For older athletes, discontinuation of the sport or knee replacement is a plausible option once the arthritis becomes a significant barrier to play. Osteotomy can be considered for (1) younger athletes who wish to continue competing and for whom total knee arthroplasty is not a reasonable option given their age and (2) those whom all other surgical options have been exhausted. The International Society of Arthroscopy, Knee Surgery, and Orthopaedic Sports Medicine has formulated guidelines for indications and contraindications to HTO, and Brinkman et al12 has published a comprehensive review discussing it. Indications for considering HTO in the elite athlete include malalignment with associated joint pathology, after all other possible treatments have been explored.12,36 Osteotomy may improve symptoms, relieve pain, and allow a return to a “normal” lifestyle—that is, one not specifically based on competition, although that may be a consideration.
Surgical Technique
The medial opening wedge is preferred over the lateral closing wedge in the athlete. With the opening wedge, precise correction is more likely and overcorrection is less likely. An acute correction with medial plate fixation is preferred. The opening wedge can increase knee stability; it avoids osteotomy of the fibula or disruption of the proximal tibiofibular joint. Proximal migration of the fibula can cause increased laxity of the posterolateral corner ligamentous complex of the knee.17,37,70 If the fibula is not osteotomized in a closing-wedge technique, the tibial slope will be forced to decrease secondary to hinging at the proximal tibiofibular joint.7 Peroneal nerve injury is a known complication of lateral-closing wedge osteotomies, and because peroneal nerve injury to the athlete is potentially career threatening, the medial approach is preferred to a lateral-sided dissection.60,70
Preoperative Planning
Evaluation begins by assessing the extent of knee arthrosis and lower extremity alignment with bilateral weightbearing anteroposterior views in full extension, bilateral weightbearing posteroanterior tunnel views in 30° of flexion, and lateral and Merchant views. A double-leg weightbearing anteroposterior view is also obtained, and the desired HTO correction is calculated according to the method described by Dugdale et al.22 In athletes, the osteotomy places the weightbearing line (as measured from the center of the femoral head to the center of the tibiotalar joint) through the center of the knee joint. Although the idea of overcorrection has been introduced in the treatment of medial compartment arthritis in the general population, significant overcorrection in the athlete is not recommended. The goal is to re-create neutral anatomical and biomechanical environments for the athlete’s knee. The osteotomy is also planned to achieve the desired posterior tibial slope in the sagittal plane to enhance the stability of the knee if an anterior cruciate ligament or PCL deficiency exists.4,21,24,25
Operative Procedure
Concurrent arthroscopy using low pressures and frequent compartment checks is performed as necessary to evaluate the menisci and the status of the articular cartilage. Following arthroscopy, the extremity is elevated and exsanguinated, and the rest of the procedure is carried out under tourniquet control. A vertical incision is made over the pes anserinus insertion halfway between the medial border of the patellar ligament and the posterior margin of the tibia, followed by exposure and incision of the sartorial fascia and, finally, subperiosteal elevation of the medial collateral ligament(Figure 1). Blunt retractors are then placed anteriorly to protect the patellar ligament and posteriorly to protect the hamstring tendons and superficial medial collateral ligament. Under fluoroscopic control, a guide wire is drilled across the proximal tibia from medial to lateral. The guide is positioned at the level of the superior aspect of the tibial tubercle and oriented obliquely to end at least 1 cm below the joint line at the lateral tibial cortex (Figure 2). By aiming approximately 1 cm below the lateral joint line, one can stay proximal to the patellar tendon insertion while being sufficiently inferior to the articular surface to predictably prevent intra-articular fracture during the cut. The proximal osteotomy maximizes the metaphyseal location and likelihood of healing. In addition, if the osteotomy cut is too distal, it becomes extracapsular, thereby reducing the stability of the osteotomy site. The osteotomy is performed with an oscillating saw below the guide pin to prevent superior migration and to decrease risk of an intra-articular fracture. The osteotomy is deepened with flexible and rigid osteotomes via fluoroscopic confirmation (Figure 3).
Figure 1.
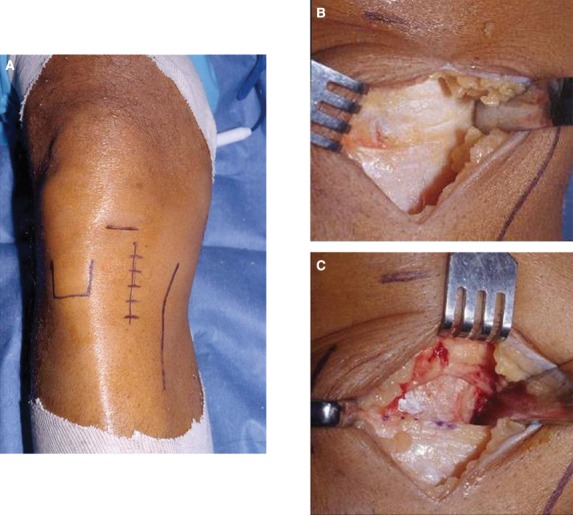
A, surgical landmarks and skin incision; B, sartorial fascia is exposed and incised; C, subperiosteal elevation of the medial collateral ligament.
Figure 2.

Intraoperative fluoroscopic image showing placement of the guide pin. Notice that the pin is just shy of the lateral cortex, approximately 1 cm below the articular surface.
Figure 3.
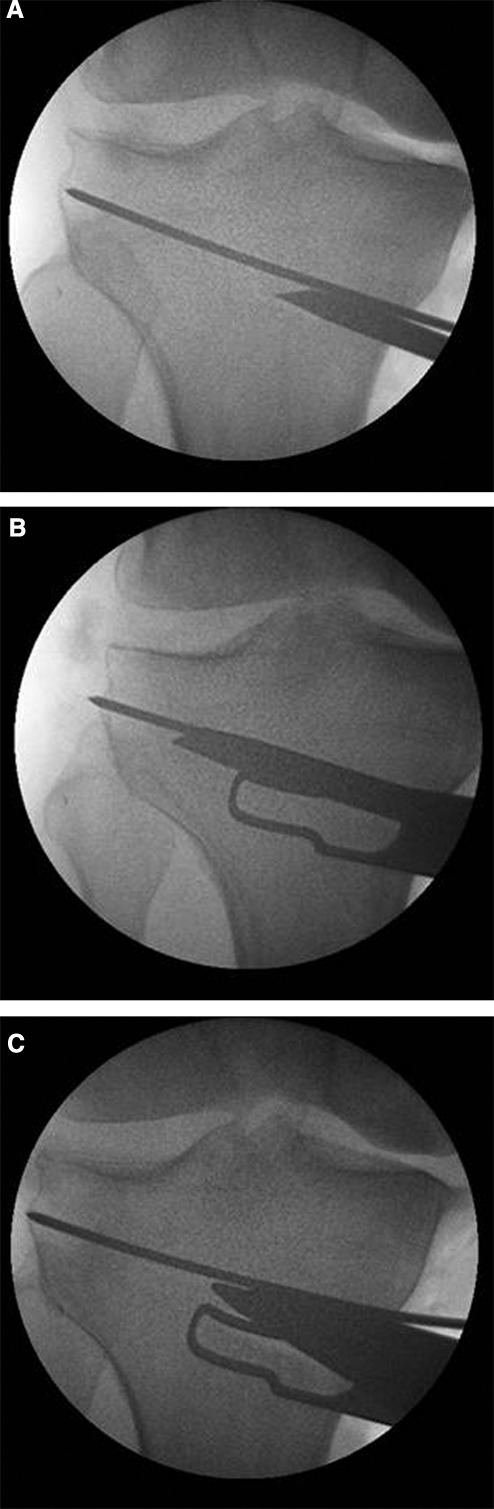
Opening the medial wedge by “stacking” sequentially larger osteotomes.
Once the osteotomy has been completed, the medial opening is created with an osteotomy wedge to the predetermined depth. Intraoperative femorotibial alignment is verified by fluoroscopy, and an extramedullary alignment guide is used to ensure that the weightbearing axis is passing through the center of the knee joint (Figure 4). Sabharwal and Zhao61 recently cautioned that for obese patients or those with substantial malalignment, supine fluoroscopy alignment measurements without loading of the knee joint does not reflect the axis as accurately as preoperative standing films. In such cases, careful scrutiny of both the preoperative weightbearing films and the intraoperative fluoroscopic images can still predictably lead to favorable results. The posterior tibial slope is also assessed intraoperatively and can be changed by distracting the osteotomy more anteriorly or posteriorly if the patient has symptomatic cruciate deficiency or excessive anteroposterior translation preoperatively. Case 2 in the discussion highlights the use of HTO to help stabilize an athlete’s knee with PCL deficiency by increasing the tibial slope. If the opening is greater than 1 cm anteriorly, a tibial tubercle osteotomy is performed to advance the tubercle the same height of the osteotomy. When the desired opening has been achieved, the osteotomy is secured with a plate and bone graft (corticocancellous wedges cut from femoral head allograft) (Figure 5). The plate is fixed proximally with 6.5-mm cancellous screws and distally with 4.5-mm cortical screws. Last, placement of fixation is confirmed with fluoroscopic imaging.
Figure 4.
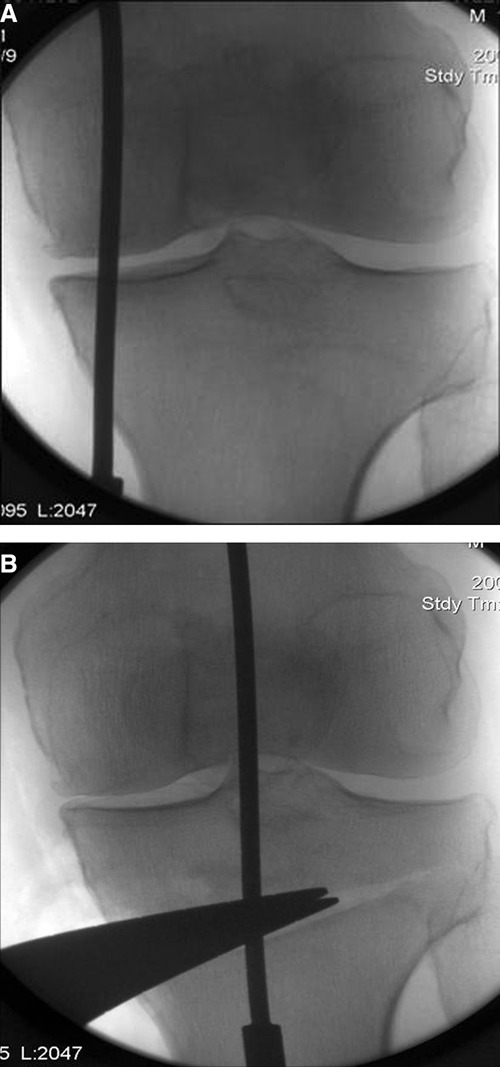
A, fluoroscopic image before the high tibial osteotomy demonstrating where the mechanical axis passes through the knee, as shown with an extramedullary guide traveling from the center of the hip joint to the center of the ankle joint; B, fluoroscopic images confirming that the mechanical axis has been realigned to pass through the center of the knee after performing the osteotomy.
Figure 5.
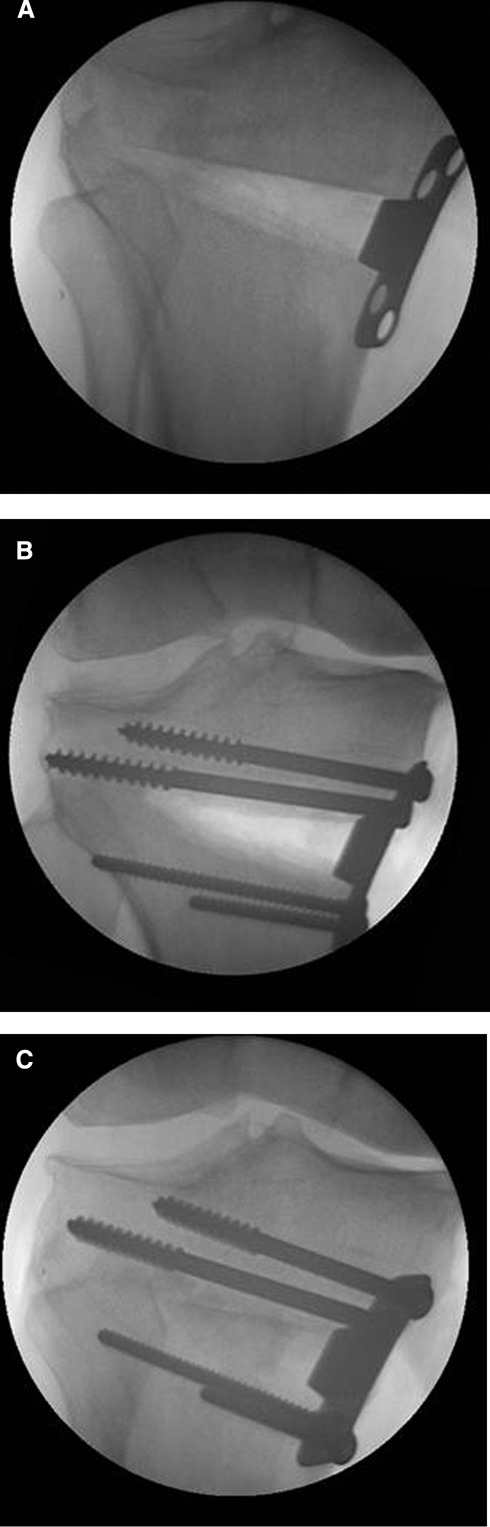
A, intraoperative fluoroscopic image showing medial opening wedge osteotomy held in place by the Puddu Plate (Arthrex, Naples, Florida); B, plate fixed in place with 6.5-mm cancellous screws proximally and 4.5-mm cortical screws distally; C, opening wedge filled by femoral head allograft wedge.
Following surgery, a hinged brace allows 0° to 90° of motion for 6 weeks while the patient remains toe-touch weightbearing. Radiographs are performed at 6 weeks; if the osteotomy is consolidating, the brace is discontinued, and full weightbearing is initiated with a strengthening program. Radiographs are repeated at 10 weeks; if osseous consolidation has been achieved, sport-specific rehabilitation is initiated.
Complications
Complications associated with HTO include fracture, nonunion, symptomatic hardware or hardware failure, infection, compartment syndrome, and peroneal nerve palsy. The incidence of intra-articular fractures has been reported to be 11% in medial-opening HTO and between 10% and 20% in lateral-closing HTO.28,44 As mentioned previously, staying inferior to a guide pin positioned 1 cm below the joint line on the lateral side during the osteotomy helps to reduce the risk of intra-articular fracture. If such fracture does occur, congruity of the plateau must be achieved with stable fixation. Nonunion is a more common complication in opening-wedge techniques, with risks reported from 0.7% to 4.4%.8,9,65,69 Bone autograft and allograft, bone substitutes, and growth factors have been used to fill the void in opening HTO and to decrease nonunion. Recent research supports the use of a locking plate design to enhance fixation and allow earlier weightbearing to decrease risk of nonunion.71,77 The Puddu Plate (Arthrex, Naples, Florida), however, is less often symptomatic than the larger locking plate; it usually does not require a second surgery for hardware removal; and it has not been associated with hardware failure or nonunion.
Infection risk with open reduction internal fixation has been reported to be 4%.10 Although compartment syndrome associated with HTO has been described, the exact incidence is unknown.28,65 An increased risk of compartment syndrome during HTO has been associated with concomitant arthroscopic ligament reconstruction.28,42 When concomitant arthroscopy is necessary, use of low pressures and frequent compartment checks can minimize risks during the operation. The incidence of peroneal nerve palsy associated with closing-wedge HTO ranges from 2% to 16%.23,65 The medial-side approach helps to avoid this potentially career-threatening complication in athletes.
Case Discussions
The use of HTO in select competitive athletes has led to favorable outcomes. With athletes that undergo HTO, the goal of surgery is not to allow resumption of competition but rather to allow daily and recreational-level activities. Only after successfully completing rehabilitation with complete resolution of symptoms can the athletes begin discussion of the risks and benefits of resuming play. Two cases are highlighted where HTO was performed in combination with other procedures. Following rehabilitation and counseling, the athletes returned to play in the National Football League.
Case 1: HTO and Osteochondritis Dissecans
The first case illustrates the use of a HTO in the treatment of a medial femoral condylar osteochondritis dissecans (OCD) lesion (fourth HTO indication, Table 1). The patient was a collegiate football player who presented with complaints of right medial knee pain and swelling. Imaging revealed a large OCD lesion of the medial femoral condyle (Figure 6). Initially, the OCD lesion base was arthroscopically debrided and bone grafted, and the fragment was fixed with an osteochondral autograft plug placed in the center of the lesion. This enabled the player to resume football, but he returned the following year with recurrent complaints of medial knee pain. Magnetic resonance imaging at that time revealed partial healing of the OCD lesion. Evaluation of his lower limb mechanical axis showed varus malalignment with increased medial compartment loading. Figure 7 shows images of the OCD lesion at the time of repeat arthroscopy.
Table 1.
Indications for high tibial osteotomies in elite athletes.
| Malalignment With . . . |
|---|
|
Figure 6.
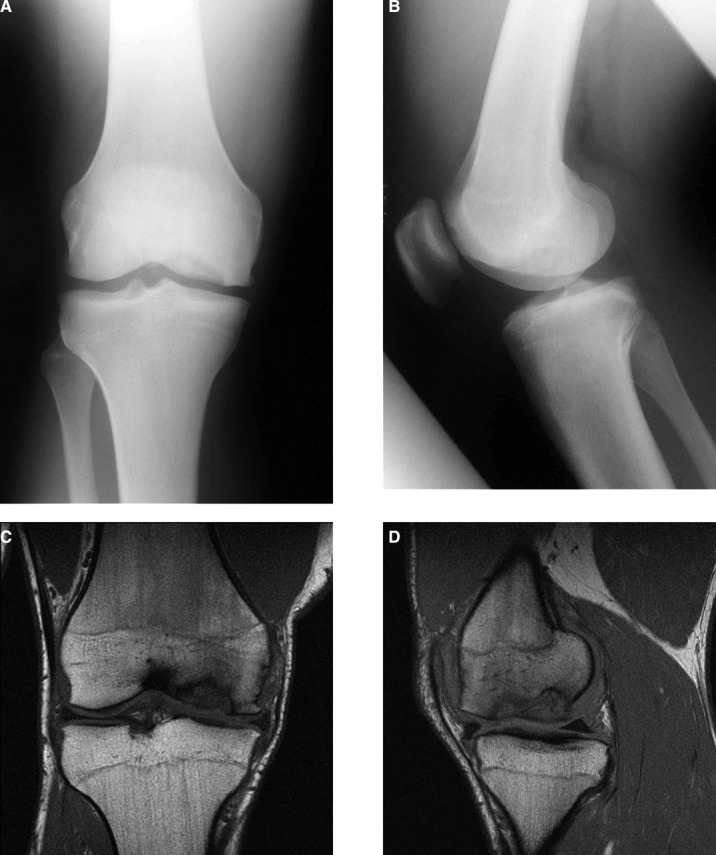
Anteroposterior (A) and lateral (B) plain films alongside coronal (C) and sagittal (D) magnetic resonance imaging images showing the patient’s large osteochondritis dissecans lesion.
Figure 7.
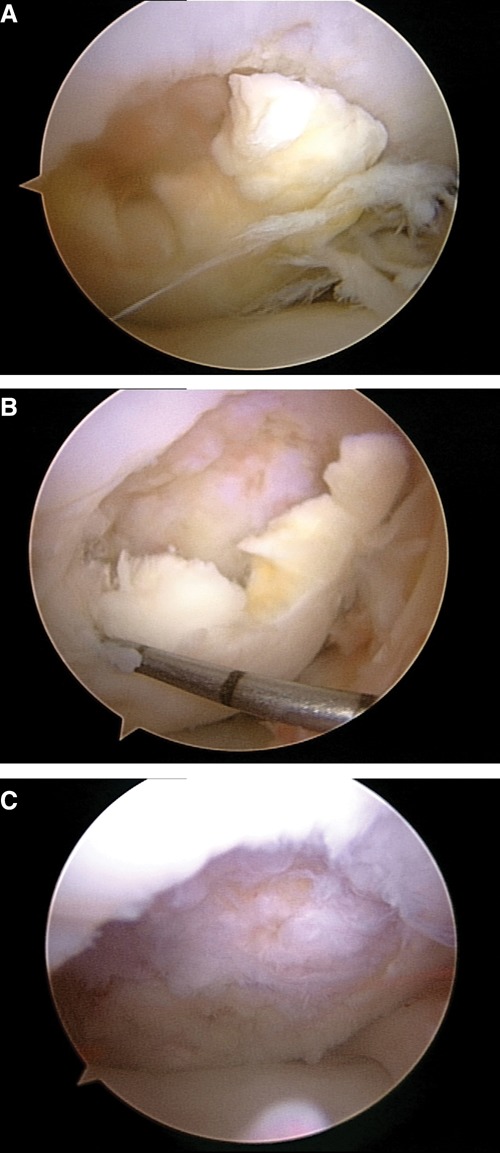
Intraoperative images at the time of repeat arthroscopy showing a large medial femoral condyle osteochondritis dissecans lesion, before and after debridement.
Ultimately, the lesion was debrided and treated with autologous chondrocyte implantation, combined with a HTO to off-load the medial compartment and better facilitate healing of the OCD lesion (Figure 8). Before proceeding with the HTO, the patient was informed that the goal of the HTO and autologous chondrocyte implantation was to allow him to resume normal daily activities and not necessarily high-level athletic competition. The patient had complete resolution of knee pain, and after proper rehabilitation and counseling regarding risks of return to play, he resumed competition following graduation from college in the National Football League.
Figure 8.
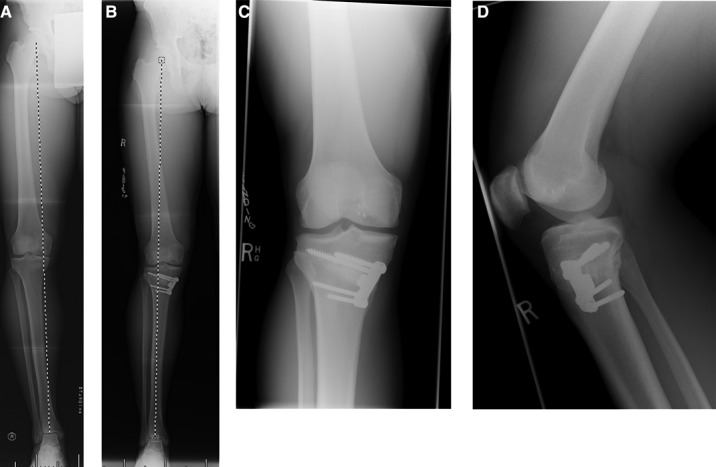
Preoperative (A) and postoperative (B) long leg-alignment images showing high tibial osteotomy and corrected mechanical axis to the lateral tibial spine. Postoperative anteroposterior (C) and lateral (D) plain films demonstrating the healed high tibial osteotomy.
Case 2: HTO and PCL Deficiency
The second case demonstrates the use of HTO in the treatment of instability and varus malalignment (second HTO indication, Table 1). The patient was a professional football player unable to compete secondary to medial knee pain. He previously had an isolated PCL injury and developed subsequent medial compartment disease with varus malalignment. He had undergone arthroscopic debridement of a medial meniscus tear, but not PCL reconstruction. Arthroscopy had also revealed chondromalacia and generalized laxity of the medial compartment. Radiographs and magnetic resonance imaging at presentation showed early degenerative changes of the medial compartment, including subchondral sclerosis and edema. Bone scan at that time confirmed the medial compartment overload.
Physical exam revealed varus alignment and slight lateral/posterolateral thrust on the affected side during ambulation, which went into slight recurvatum on range of motion testing and had modest posteromedial joint line tenderness. Grade II posterior sag was noted, as was grade II medial collateral ligament laxity, likely pseudolaxity secondary to the medial compartment wear.
The patient’s goal at presentation was to resume his National Football League career. Biplanar osteotomy with an opening wedge placed anteromedially was recommended because it would improve his posterior instability and off-load the medial compartment. After discussing the proposed procedure with his team physicians, the player elected to proceed with surgery (Figure 9). Postoperatively, his posterior sag was no longer present, and his medial knee pain had completely resolved. He did well overall and was cleared to return to play after appropriate rehabilitation and counseling. One year after surgery, the player developed some irritation of the pes anserinus from the fixation plate, and hardware removal was performed without incident.
Figure 9.
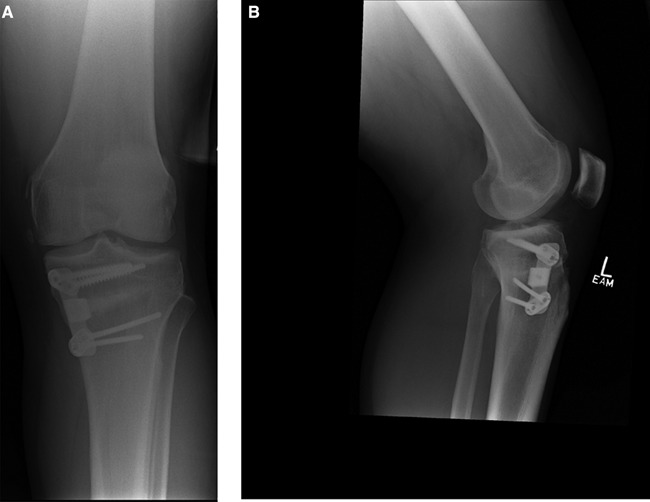
Anteroposterior (A) and lateral (B) plain films of the biplanar high tibial osteotomy with an anteromedial plate to address both the posterior cruciate ligament deficiency and the varus malalignment.
Footnotes
References
- 1. Aaron RK, Skolnick AH, Reinert SE, Ciombor DM. Arthroscopic debridement for osteoarthritis of the knee. J Bone Joint Surg Am. 2006;88(5):936-943 [DOI] [PubMed] [Google Scholar]
- 2. Adili A, Bhandari M, Giffin R, Whately C, Kwok DC. Valgus high tibial osteotomy: comparison between an Ilizarov and a Coventry wedge technique for the treatment of medial compartment osteoarthritis of the knee. Knee Surg Sports Traumatol Arthrosc. 2002;10(3):169-176 [DOI] [PubMed] [Google Scholar]
- 3. Aglietti P, Rinonapoli E, Stringa G, Taviani A. Tibial osteotomy for the varus osteoarthritic knee. Clin Orthop Relat Res. 1983;176:239-251 [PubMed] [Google Scholar]
- 4. Agneskirchner JD, Hurschler C, Stukenborg-Colsman C, Imhoff AB, Lobenhoffer P. Effect of high tibial flexion osteotomy on cartilage pressure and joint kinematics: a biomechanical study in human cadaveric knees. Arch Orthop Trauma Surg. 2004;124(9):575-584 [DOI] [PubMed] [Google Scholar]
- 5. Agneskirchner JD, Hurschler C, Wrann CD, Lobenhoffer P. The effects of valgus medial opening wedge high tibial osteotomy on articular cartilage pressure of the knee: a biomechanical study. Arthroscopy. 2007;23(8):852-861 [DOI] [PubMed] [Google Scholar]
- 6. Akizuki S, Yasukawa Y, Takizawa T. Does arthroscopic abrasion arthroplasty promote cartilage regeneration in osteoarthritic knees with eburnation? A prospective study of high tibial osteotomy with abrasion arthroplasty versus high tibial osteotomy alone. Arthroscopy. 1997;13(1):9-17 [DOI] [PubMed] [Google Scholar]
- 7. Amendola A, Rorabeck CH, Bourne RB, Apyan PM. Total knee arthroplasty following high tibial osteotomy for osteoarthritis. J Arthroplasty. 1989;4:S11-S17 [DOI] [PubMed] [Google Scholar]
- 8. Aydogdu S, Sur H. High tibial osteotomy for varus deformity of more than 20 degrees [In French]. Rev Chir Orthop Reparatrice Appar Mot. 1997;84(5):439-446 [PubMed] [Google Scholar]
- 9. Bettin D, Karbowski A, Schwering L, Matthiass HH. Time-dependent clinical and roentgenographical results of Coventry high tibial valgisation osteotomy. Arch Orthop Trauma Surg. 1998;117(1-2):53-57 [DOI] [PubMed] [Google Scholar]
- 10. Billings A, Scott DF, Camargo MP, Hofmann AA. High tibial osteotomy with a calibrated osteotomy guide, rigid internal fixation, and early motion: long-term follow-up. J Bone Joint Surg Am. 2000;82(1):70-79 [DOI] [PubMed] [Google Scholar]
- 11. Boss A, Stutz G, Oursin C, Gachter A. Anterior cruciate ligament reconstruction combined with valgus tibial osteotomy (combined procedure). Knee Surg Sports Traumatol Arthrosc. 1995;3(3):187-191 [DOI] [PubMed] [Google Scholar]
- 12. Brinkman JM, Lobenhoffer P, Agneskirchner JD, Staubli AE, Wymenga AB, van Heerwaarden RJ. Osteotomies around the knee: patient selection, stability of fixation and bone healing in high tibial osteotomies. J Bone Joint Surg Br. 2008;90(12):1548-1557 [DOI] [PubMed] [Google Scholar]
- 13. Brouwer RW, Bierma-Zeinstra SM, van Koeveringe AJ, Verhaar JA. Patellar height and the inclination of the tibial plateau after high tibial osteotomy: the open versus the closed-wedge technique. J Bone Joint Surg Br. 2005;87(9):1227-1232 [DOI] [PubMed] [Google Scholar]
- 14. Brouwer RW, Bierma-Zeinstra SM, van Raaij TM, Verhaar JA. Osteotomy for medial compartment arthritis of the knee using a closing wedge or an opening wedge controlled by a Puddu plate; a one-year randomised, controlled study. J Bone Joint Surg Br. 2006;88(11):1454-1459 [DOI] [PubMed] [Google Scholar]
- 15. Brouwer RW, Raaij van TM, Bierma-Zeinstra SM, Verhagen AP, Jakma TS, Verhaar JA. Osteotomy for treating knee osteoarthritis. Cochrane Database Syst Rev. 2007(3):CD004019 [DOI] [PubMed] [Google Scholar]
- 16. Chen AL, Mears SC, Hawkins RJ. Orthopaedic care of the aging athlete. J Am Acad Orthop Surg. 2005;13(6):407-416 [DOI] [PubMed] [Google Scholar]
- 17. Chun YM, Kim SJ, Kim HS. Evaluation of the mechanical properties of posterolateral structures and supporting posterolateral instability of the knee. J Orthop Res. 2008;26(10):1371-1376 [DOI] [PubMed] [Google Scholar]
- 18. Coventry MB. Proximal tibial varus osteotomy for osteoarthritis of the lateral compartment of the knee. J Bone Joint Surg Am. 1987;69(1):32-38 [PubMed] [Google Scholar]
- 19. Coventry MB, Ilstrup DM, Wallrichs SL. Proximal tibial osteotomy: a critical long-term study of eighty-seven cases. J Bone Joint Surg Am. 1993;75(2):196-201 [DOI] [PubMed] [Google Scholar]
- 20. Crawford K, Philippon MJ, Sekiya JK, Rodkey WG, Steadman JR. Microfracture of the hip in athletes. Clin Sports Med. 2006;25(2):327-335 [DOI] [PubMed] [Google Scholar]
- 21. Dejour H, Bonnin M. Tibial translation after anterior cruciate ligament rupture: two radiological tests compared. J Bone Joint Surg Br. 1994;76(5):745-749 [PubMed] [Google Scholar]
- 22. Dugdale TW, Noyes FR, Styer D. Preoperative planning for high tibial osteotomy: the effect of lateral tibiofemoral separation and tibiofemoral length. Clin Orthop Relat Res. 1992;274:248-264 [PubMed] [Google Scholar]
- 23. Georgoulis AD, Makris CA, Papageorgiou CD, Moebius UG, Xenakis T, Soucacos PN. Nerve and vessel injuries during high tibial osteotomy combined with distal fibular osteotomy: a clinically relevant anatomic study. Knee Surg Sports Traumatol Arthrosc. 1999;7(1):15-19 [DOI] [PubMed] [Google Scholar]
- 24. Giffin JR, Stabile KJ, Zantop T, Vogrin TM, Woo SL, Harner CD. Importance of tibial slope for stability of the posterior cruciate ligament deficient knee. Am J Sports Med. 2007;35(9):1443-1449 [DOI] [PubMed] [Google Scholar]
- 25. Giffin JR, Vogrin TM, Zantop T, Woo SL, Harner CD. Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med. 2004;32(2):376-382 [DOI] [PubMed] [Google Scholar]
- 26. Gomoll AH, Minas T, Farr J, Cole BJ. Treatment of chondral defects in the patellofemoral joint. J Knee Surg. 2006;19(4):285-295 [DOI] [PubMed] [Google Scholar]
- 27. Gross AE. Cartilage resurfacing: filling defects. J Arthroplasty. 2003;18(3)(suppl 1):14-17 [DOI] [PubMed] [Google Scholar]
- 28. Hernigou P, Medevielle D, Debeyre J, Goutallier D. Proximal tibial osteotomy for osteoarthritis with varus deformity: a ten to thirteen-year follow-up study. J Bone Joint Surg Am. 1987;69(3):332-354 [PubMed] [Google Scholar]
- 29. Holden DL, James SL, Larson RL, Slocum DB. Proximal tibial osteotomy in patients who are fifty years old or less: a long-term follow-up study. J Bone Joint Surg Am. 1988;70(7):977-982 [PubMed] [Google Scholar]
- 30. Insall JN. High tibial osteotomy in the treatment of osteoarthritis of the knee. Surg Annu. 1975;7:347-359 [PubMed] [Google Scholar]
- 31. Insall JN, Joseph DM, Msika C. High tibial osteotomy for varus gonarthrosis: a long-term follow-up study. J Bone Joint Surg Am. 1984;66(7):1040-1048 [PubMed] [Google Scholar]
- 32. Jackson JP, Waugh W. Tibial osteotomy for osteoarthritis of the knee. J Bone Joint Surg Br. 1961;43:746-751 [DOI] [PubMed] [Google Scholar]
- 33. Kaplan FS, Hayes WC, Keaveny TM, Boskey A, Einhorn TA, Iannotti JP. Form and function of bone. In: Simon SR, ed. Orthopaedic Basic Science. Rosemont, IL: American Academy of Orthopaedic Surgeons; 1994:127-184 [Google Scholar]
- 34. Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494-502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kish G, Modis L, Hangody L. Osteochondral mosaicplasty for the treatment of focal chondral and osteochondral lesions of the knee and talus in the athlete: rationale, indications, techniques, and results. Clin Sports Med. 1999;18(1):45-66 [DOI] [PubMed] [Google Scholar]
- 36. Koshino T, Wada S, Ara Y, Saito T. Regeneration of degenerated articular cartilage after high tibial valgus osteotomy for medial compartmental osteoarthritis of the knee. Knee. 2003;10(3):229-236 [DOI] [PubMed] [Google Scholar]
- 37. Laprade RF, Engebretsen L, Johansen S, Wentorf FA, Kurtenbach C. The effect of a proximal tibial medial opening wedge osteotomy on posterolateral knee instability: a biomechanical study. Am J Sports Med. 2008;36(5):956-960 [DOI] [PubMed] [Google Scholar]
- 38. Lavernia CJ, Sierra RJ, Hungerford DS, Krackow K. Activity level and wear in total knee arthroplasty: a study of autopsy retrieved specimens. J Arthroplasty. 2001;16(4):446-453 [DOI] [PubMed] [Google Scholar]
- 39. Magyar G, Ahl TL, Vibe P, Toksvig-Larsen S, Lindstrand A. Open-wedge osteotomy by hemicallotasis or the closed-wedge technique for osteoarthritis of the knee: a randomised study of 50 operations. J Bone Joint Surg Br. 1999;81(3):444-448 [DOI] [PubMed] [Google Scholar]
- 40. Magyar G, Toksvig-Larsen S, Lindstrand A. Changes in osseous correction after proximal tibial osteotomy: radiostereometry of closed- and open-wedge osteotomy in 33 patients. Acta Orthop Scand. 1999;70(5):473-477 [DOI] [PubMed] [Google Scholar]
- 41. Mammi GI, Rocchi R, Cadossi R, Massari L, Traina GC. The electrical stimulation of tibial osteotomies: double-blind study. Clin Orthop Relat Res. 1993;288:246-253 [PubMed] [Google Scholar]
- 42. Marti CB, Jakob RP. Accumulation of irrigation fluid in the calf as a complication during high tibial osteotomy combined with simultaneous arthroscopic anterior cruciate ligament reconstruction. Arthroscopy. 1999;15(8):864-866 [DOI] [PubMed] [Google Scholar]
- 43. Marti RK, Verhagen RA, Kerkhoffs GM, Moojen TM. Proximal tibial varus osteotomy: indications, technique, and five to twenty-one-year results. J Bone Joint Surg Am. 2001;83(2):164-170 [PubMed] [Google Scholar]
- 44. Matthews LS, Goldstein SA, Malvitz TA, Katz BP, Kaufer H. Proximal tibial osteotomy: factors that influence the duration of satisfactory function. Clin Orthop Relat Res. 1988;229:193-200 [PubMed] [Google Scholar]
- 45. McNickle AG, Provencher MT, Cole BJ. Overview of existing cartilage repair technology. Sports Med Arthrosc. 2008;16(4):196-201 [DOI] [PubMed] [Google Scholar]
- 46. Mithoefer K, Williams RJ, III, Warren RF, Wickiewicz TL, Marx RG. High-impact athletics after knee articular cartilage repair: a prospective evaluation of the microfracture technique. Am J Sports Med. 2006;34(9):1413-1418 [DOI] [PubMed] [Google Scholar]
- 47. Mont MA, Stuchin SA, Paley D, et al. Different surgical options for monocompartmental osteoarthritis of the knee: high tibial osteotomy versus unicompartmental knee arthroplasty versus total knee arthroplasty: indications, techniques, results, and controversies. Instr Course Lect. 2004;53:265-283 [PubMed] [Google Scholar]
- 48. Morrey BF. Upper tibial osteotomy for secondary osteoarthritis of the knee. J Bone Joint Surg Br. 1989;71(4):554-559 [DOI] [PubMed] [Google Scholar]
- 49. Motycka T, Eggerth G, Landsiedl F. The incidence of thrombosis in high tibial osteotomies with and without the use of a tourniquet. Arch Orthop Trauma Surg. 2000;120(3-4):157-159 [DOI] [PubMed] [Google Scholar]
- 50. Myrnerts R. High tibial osteotomy with overcorrection of varus malalignment in medial gonarthrosis. Acta Orthop Scand. 1980;51(3):557-560 [DOI] [PubMed] [Google Scholar]
- 51. Nagel A, Insall JN, Scuderi GR. Proximal tibial osteotomy: a subjective outcome study. J Bone Joint Surg Am. 1996;78(9):1353-1358 [DOI] [PubMed] [Google Scholar]
- 52. Nakamura E, Mizuta H, Kudo S, Takagi K, Sakamoto K. Open-wedge osteotomy of the proximal tibia hemicallotasis. J Bone Joint Surg Br. 2001;83(8):1111-1115 [DOI] [PubMed] [Google Scholar]
- 53. Naudie DD, Amendola A, Fowler PJ. Opening wedge high tibial osteotomy for symptomatic hyperextension-varus thrust. Am J Sports Med. 2004;32(1):60-70 [DOI] [PubMed] [Google Scholar]
- 54. Naudie D, Bourne RB, Rorabeck CH, Bourne TJ. Survivorship of the high tibial valgus osteotomy: a 10- to 22-year followup study. Clin Orthop Relat Res. 1999;367:18-27 [PubMed] [Google Scholar]
- 55. Noyes FR, Barber-Westin SD, Hewett TE. High tibial osteotomy and ligament reconstruction for varus angulated anterior cruciate ligament-deficient knees. Am J Sports Med. 2000;28(3):282-296 [DOI] [PubMed] [Google Scholar]
- 56. Noyes FR, Stabler CL. A system for grading articular cartilage lesions at arthroscopy. Am J Sports Med. 1989;17(4):505-513 [DOI] [PubMed] [Google Scholar]
- 57. Odenbring S, Tjornstrand B, Egund N, et al. Function after tibial osteotomy for medial gonarthrosis below aged 50 years. Acta Orthop Scand. 1989;60(5):527-531 [DOI] [PubMed] [Google Scholar]
- 58. Phisitkul P, Wolf BR, Amendola A. Role of high tibial and distal femoral osteotomies in the treatment of lateral-posterolateral and medial instabilities of the knee. Sports Med Arthrosc. 2006;14(2):96-104 [DOI] [PubMed] [Google Scholar]
- 59. Rudan JF, Simurda MA. Valgus high tibial osteotomy: a long-term follow-up study. Clin Orthop Relat Res. 1991;268:157-160 [PubMed] [Google Scholar]
- 60. Ryan W, Mahony N, Delaney M, O’Brien M, Murray P. Relationship of the common peroneal nerve and its branches to the head and neck of the fibula. Clin Anat. 2003;16(6):501-505 [DOI] [PubMed] [Google Scholar]
- 61. Sabharwal S, Zhao C. Assessment of lower limb alignment: supine fluoroscopy compared with a standing full-length radiograph. J Bone Joint Surg Am. 2008;90(1):43-51 [DOI] [PubMed] [Google Scholar]
- 62. Salzmann GM, Ahrens P, Naal FD, et al. Sporting activity after high tibial osteotomy for the treatment of medial compartment knee osteoarthritis. Am J Sports Med. 2009;37(2):312-318 [DOI] [PubMed] [Google Scholar]
- 63. Sanchez M, Anitua E, Azofra J, Aguirre JJ, Andia I. Intra-articular injection of an autologous preparation rich in growth factors for the treatment of knee OA: a retrospective cohort study. Clin Exp Rheumatol. 2008;26(5):910-913 [PubMed] [Google Scholar]
- 64. Shasha N, Aubin PP, Cheah HK, Davis AM, Agnidis Z, Gross AE. Long-term clinical experience with fresh osteochondral allografts for articular knee defects in high demand patients. Cell Tissue Bank. 2002;3(3):175-182 [DOI] [PubMed] [Google Scholar]
- 65. Spahn G. Complications in high tibial (medial opening wedge) osteotomy. Arch Orthop Trauma Surg. 2004;124(10):649-653 [DOI] [PubMed] [Google Scholar]
- 66. Sterett WI, Steadman JR. Chondral resurfacing and high tibial osteotomy in the varus knee. Am J Sports Med. 2004;32(5):1243-1249 [DOI] [PubMed] [Google Scholar]
- 67. Stukenborg-Colsman C, Wirth CJ, Lazovic D, Wefer A. High tibial osteotomy versus unicompartmental joint replacement in unicompartmental knee joint osteoarthritis: 7-10-year follow-up prospective randomised study. Knee. 2001;8(3):187-194 [DOI] [PubMed] [Google Scholar]
- 68. Stutz G, Boss A, Gachter A. Comparison of augmented and non-augmented anterior cruciate ligament reconstruction combined with high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 1996;4(3):143-148 [DOI] [PubMed] [Google Scholar]
- 69. Tjornstrand B, Hagstedt B, Persson BM. Results of surgical treatment for non-union after high tibial osteotomy in osteoarthritis of the knee. J Bone Joint Surg Am. 1978;60(7):973-977 [PubMed] [Google Scholar]
- 70. Tunggal JA, Higgins GA, Waddell JP. Complications of closing wedge high tibial osteotomy [published online ahead of print June 24, 2009]. Int Orthop. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. van den Bekerom MP, Patt TW, Kleinhout MY, van der Vis HM, Albers GH. Early complications after high tibial osteotomy: a comparison of two techniques. J Knee Surg. 2008;21(1):68-74 [DOI] [PubMed] [Google Scholar]
- 72. Verdonk PC, Demurie A, Almqvist KF, Veys EM, Verbruggen G, Verdonk R. Transplantation of viable meniscal allograft: survivorship analysis and clinical outcome of one hundred cases. J Bone Joint Surg Am. 2005;87(4):715-724 [DOI] [PubMed] [Google Scholar]
- 73. Weidenhielm L, Olsson E, Brostrom LA, Borjesson-Hederstrom M, Mattsson E. Improvement in gait one year after surgery for knee osteoarthrosis: a comparison between high tibial osteotomy and prosthetic replacement in a prospective randomized study. Scand J Rehabil Med. 1993;25(1):25-31 [PubMed] [Google Scholar]
- 74. Wolcott M. Osteotomies around the knee for the young athlete with osteoarthritis. Clin Sports Med. 2005;24(1):153-161 [DOI] [PubMed] [Google Scholar]
- 75. Wolf BR, Amendola A. Impact of osteoarthritis on sports careers. Clin Sports Med. 2005;24(1):187-198 [DOI] [PubMed] [Google Scholar]
- 76. Wright JM, Crockett HC, Slawski DP, Madsen MW, Windsor RE. High tibial osteotomy. J Am Acad Orthop Surg. 2005;13(4):279-289 [DOI] [PubMed] [Google Scholar]
- 77. Yacobucci GN, Cocking MR. Union of medial opening-wedge high tibial osteotomy using a corticocancellous proximal tibial wedge allograft. Am J Sports Med. 2008;36(4):713-719 [DOI] [PubMed] [Google Scholar]


