Abstract
Context:
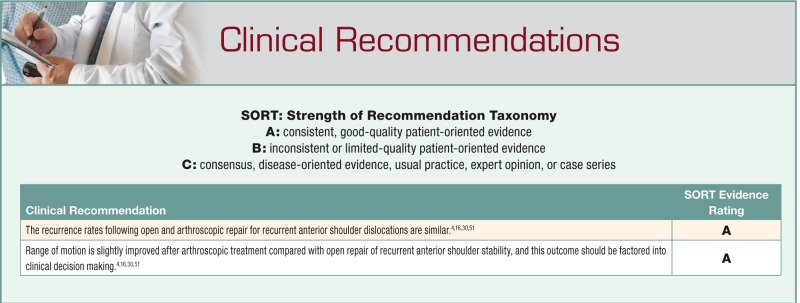
It remains unknown if arthroscopic repair of recurrent anterior shoulder instability is as effective as open repair.
Objective:
The purpose of this study is to analyze the literature to provide clinical recommendations regarding the most appropriate therapeutic intervention for recurrent anterior shoulder instability.
Study Design:
Systematic review of level I and II studies.
Data Sources:
PubMed, EMBASE, the Cochrane Database of Systematic Reviews, and secondary references from 1967 to March 2010 were appraised for studies that met the inclusion criteria.
Study Selection:
Inclusion criteria were English-language level I or level II trials involving the treatment of recurrent anterior shoulder instability. Exclusion criteria included non-English-language studies; level III, IV, or V studies; and trials examining treatment of first-time shoulder dislocation, posterior shoulder dislocation, or diagnoses other than recurrent anterior shoulder dislocations.
Data Extraction:
Included studies underwent quality appraisal independently by each author identifying strengths, weaknesses, and biases.
Results:
Four randomized controlled trials compared the use of arthroscopic and open repair for recurrent anterior shoulder dislocations. These studies show no statistically significant difference between the 2 operative approaches. No long-term follow-up data describing the effects of either surgical approach are available at this time. Each investigation had weaknesses in study design that decreased the validity of its findings.
Conclusions:
While limited, the available evidence from randomized controlled trials does not show a statistically significant difference in redislocation rates, return to activity, and functional outcomes between the arthroscopic and open repair groups. Range of motion is marginally better following arthroscopic treatment when compared with open repair. Recommendations on the optimal surgical intervention cannot be provided.
Keywords: systematic review, recurrent anterior shoulder instability, open, arthroscopic, repair
The shoulder is the most commonly dislocated major joint, with a reported incidence of 1.7%.28 Symptomatic instability following dislocation is common, especially in young, active people.33 Recurrent instability, occurring in 50% to 96% of patients who first dislocate under the age of 20 years and in 40% to 74% of patients between the ages of 20 and 40 years, limits range of movement of the joint, requires multiple hospital and emergency department admissions for treatment, and often calls for surgical procedures to prevent further dislocation.6,7,34,46,48-50,60 Prior to arthroscopy, recurrent dislocations were managed by open repair, and the results of this approach, with only a 4% failure rate, were initially published by Dickson and Devas in 1957.13 There have been many studies documenting low recurrence rates ranging from 0% to 11% after open Bankart stabilization.§
The development of arthroscopic stabilization for recurrent anterior instability has undergone significant changes in the past 20 years. Possible benefits of arthroscopic stabilization include decreased length of hospital or outpatient surgery center stay, decreased postoperative pain, and improved range of motion (ROM). Initial arthroscopic fixation was performed by staple capsulorrhaphy, which resulted in recurrent instability in 16% to 33% of patients.11,24,35,40 Additional methods of arthroscopic stabilization have included transglenoid suturing, with a failure rate ranging from 0% to 49%,2,19,29,53 and bioabsorbable tack fixation, with a failure rate ranging from 9% to 23%.14,19,31,36,45 Newer techniques for arthroscopic stabilization have been developed, including suture anchor fixation and capsular plication, with failure rates ranging from 8% to 11%.||
There are several reasons this systematic review is reasonable. Despite the proponents for both methods, it is unclear whether arthroscopic techniques equal the success of open techniques for the treatment of recurrent instability. There are a number of published reports directly comparing arthroscopic and open shoulder stabilization repairs.¶ Several meta-analyses and reviews of this topic have been conducted.19,26,37,42 However, each of these reviews included studies classified as level III evidence or lower. In contrast, this systematic review examines only level I and II trials.
The high incidence of recurrent dislocation has implications for the individual and for society because chronic instability of the joint may prevent the individual from gaining employment or working at his or her potential. Moreover, with the growth in the number of orthopaedic surgeons specializing in shoulder surgery and sports injuries, as well as the advancement in arthroscopic techniques and sports medicine devices, there has been heightened interest in minimally invasive shoulder surgery for recurrent anterior instability. Thus, the comparison of arthroscopic versus open surgery for recurrent anterior shoulder instability is an area necessitating scrupulous review.
Methods
Search Strategy
A systematic review of level I and II trials between 1967 and 2010 was performed. PubMed, the Cochrane Database of Systematic Reviews, EMBASE, and secondary references were appraised for studies that met the inclusion criteria. Reference lists of retrieved articles were screened for additional publications. Specifically, the bibliographies of studies assessed for inclusion in this review, as well as periodicals focusing on the shoulder, were analyzed.
Study Selection
Publications included met strict selection criteria. Randomized controlled trials (RCTs) directly comparing arthroscopic with open repair for recurrent anterior shoulder instability were given priority, though level II evidence was included in the review. Patients were limited to adults (age 18 years or older) with recurrent anterior shoulder instability, which was confirmed by physical examination with a positive apprehension sign or increased anterior translation. Studies using outcome measures for shoulder function or pain—including recurrence (redislocation, subluxation, laxity), return to activity, Rowe and Constant scores,10,47 and ROM—were included. Studies with the following characteristics were not included: studies with no direct comparison of arthroscopic and open repair; non-English-language studies; level III, IV, or V studies; and studies examining treatment of first-time shoulder dislocation, posterior shoulder dislocation, or diagnoses other than recurrent anterior shoulder dislocations.
These criteria were used to independently select the relevant articles for this review by a reading of all titles and abstracts retrieved by the search strategy. The abstracts found from the search were reviewed for evidence of a direct comparison between open and arthroscopic stabilization of recurrent anterior shoulder dislocations. The 2 independent reviewers arrived at a consensus for including 4 studies in this review. The complete articles were then obtained for the selected abstracts, and a manual cross-reference was conducted. The final selected articles were independently critically appraised to classify the study design as a measure of the level of evidence.
Methodological Quality Assessment
All publications were assessed according to a methodological quality list for the assessment of RCTs (Table 1).26,44 The quality assessment list was modified and adapted to better fit this study. The requirement of blinding patients or health care providers to the intervention was excluded because this kind of blinding is not possible in this type of RCT. Each assessment criterion was graded as positive/yes, negative/no, or unclear. A quality score was calculated for the selected studies by summing the positive answers. Items D or F, or both, were answered only if C or E, respectively, or both, were scored negatively. The maximum attainable score was 9. Studies were considered to be methodologically high quality when at least 7 items scored positively, while a score of 4 to 6 was considered medium quality and 0 to 3 was low quality. The quality appraisal was then discussed between the authors, and consensus was reached regarding the strengths, weaknesses, and value of the included studies.
Table 1.
Results of the methodological quality assessment for all included randomized controlled trials.a
| Randomized Controlled Trial | ||||
|---|---|---|---|---|
| Item | Bottoni4 (2006) | Fabbriciani16 (2004) | Sperber30 (2001) | Jorgensen51 (1999) |
| A. Was the treatment allocation randomized and concealed? | + | + | + | − |
| B. Was the outcome assessor blinded to the intervention? | + | − | − | + |
| C. Were the groups similar at baseline? | + | + | + | + |
| D. If not, were adjustments made in the analysis for differences of prognostic indicators at baseline and/or for confounding variables? | NA | NA | NA | NA |
| E. Was a sufficient proportion (≥80%) of included patients available for the full length of follow-up? | + | + | + | + |
| F. If not, was selective loss to follow-up excluded? | NA | NA | NA | NA |
| G. Was an intention-to-treat analysis included? | − | − | − | − |
| H. Were the interventions clearly defined? | + | + | + | + |
| I. Were the inclusion and exclusion criteria for study entry clearly defined? | + | + | + | + |
| J. Were the outcome measures suitable to measure clinically relevant differences in treatment effects? | + | + | + | + |
| K. Was the follow-up duration adequate to measure clinical differences between treatment modalities (≥1 year)? | + | + | + | + |
| Quality score (%)b | 8 (88) | 7 (77) | 7 (77) | 7 (77) |
+, positive or yes; −, negative or no; NA, not applicable.
Minimum, 0; maximum, 9.
Data Extraction
Data on the study population, description and standardization of interventions, outcome measures, and results were extracted from the selected studies. First-time outcomes include the following: recovery defined as return to preinjury level of activity (sports or work), reinjury or recurrence (including subsequent surgery), subjective instability, results from validated shoulder rating scales. Secondary outcomes include ROM, complications, patient satisfaction, stiffness, and strength. A systematic review was performed because meta-analysis was not possible because of the diversity in outcome measures among the included studies and the differing presentations of data (median scores, mean scores, relative risk ratios). The results were summarized by means of a qualitative analysis.
Results
Search Results
The PubMed search resulted in 34 citations. Six more citations were found through the Cochrane Database. Citation tracking identified no other studies.
Excluded Studies
The title or abstract, or both, was used to exclude 12 articles based on the aforementioned study selection criteria, and 22 were retrieved for a more detailed evaluation. Next, 4 reviews19,37,42,44 were excluded because they are Cochrane Database reviews or meta-analyses of RCTs on the topic. An additional 11 studies were excluded because they are not RCTs.# A study by Mohtadi et al43 was excluded because it is an interim report of an ongoing trial examining multidirectional instability of the shoulder, as opposed to unilateral anterior instability. Finally, 2 additional studies were excluded because the reports are limited to abstracts.18,49 Consequently, 4 RCTs met our inclusion criteria.4,16,30,51
Data Extraction and Analysis
There were difficulties in extracting data from the included studies, and there is little consistency in the outcome measures used in them. There were 218 patients enrolled in the selected studies (Table 2). Each trial directly compared arthroscopic and open repair for recurrent anterior shoulder instability. Each RCT-enrolled patient had unilateral, isolated, posttraumatic, recurrent anterior shoulder instability as verified by physical examination.4,16,30,51 In addition, Bottoni et al included patients experiencing both posttraumatic and atraumatic recurrent anterior shoulder instability.4
Table 2.
Patient demographics.
| Total, No. | Sex, Men/Women | Age, y, Mean (Range) | Follow-up, mos, Mean | |||||
|---|---|---|---|---|---|---|---|---|
| Study | Arthroscopic | Open | Arthroscopic | Open | Arthroscopic | Open | Arthroscopic | Open |
| Bottoni4 | 32 | 29 | 31/1 | 29/0 | 25.2 (20-40) | 25.1 (19-42) | 28.5 | 30.0 |
| Fabbriciani16 | 30 | 30 | 24/6 | 26/4 | 24.5 (19-33) | 26.8 (21-30) | — | — |
| Sperber51 | 30 | 26 | 21/9 | 19/7 | 25.0 (18-51) | 27.5 (19-45) | — | — |
| Jorgensen30 | 21 | 20 | 15/6 | 15/5 | 28.0 (20-41) | 28.0 (18-51) | 36.2 | 36.6 |
Diagnostic arthroscopy was done prior to surgical randomization in 3 of the 4 trials.4,16,51 All 4 trials used suture anchors to repair the capsular laxity through the open technique (Table 3). However, there was variation in the arthroscopic stabilization method. Arthroscopic stabilization was performed using bioabsorbable tacks in the Sperber trial, while Jorgensen et al employed transglenoid sutures. Bottoni et al and Fabbriciani et al used suture anchors, thereby providing more consistent treatment regimens across the 2 groups.
Table 3.
Surgical techniques (No.).
Postoperatively, both treatment groups in all 4 studies were immediately immobilized with subsequent rehabilitation. The time spent in a sling varied among the trials, ranging from 3 weeks30,51 to 6 weeks.16 This difference in sling immobilization timing potentially affects the validity of the study’s results. Range of motion exercises were introduced after immobilization, and muscle-strengthening exercises were initiated thereafter in a consecutive manner in each study. Different regimens on the return to full external rotation and preinjury sporting activities were employed by the 5 trials. Bottoni et al allowed a return to sports or full active military duty at 4 to 6 months, depending on individual progress, while Fabbriciani et al allowed a return to sports activity after 6 months. Conversely, Sperber et al “discouraged overhead motion and contact sports for six months,” while Jorgensen et al allowed a return to sports activity after only 3 months.
Summary of Included Trials
Bottoni
This is a level I trial conducted with a military patient population and a mean follow-up time of 29 months.4 Inclusion criteria included patients at least 18 years of age, subjective recurrent anterior shoulder instability, 6 months of failed rehabilitation, at least a 2+ anterior load shift test, and positive apprehension and relocation signs.4 Exclusion criteria included multidirectional instability, prior shoulder surgery, and less than 12 months at military assignment.4 Patients were randomized by sealed envelope, and participants wore T-shirts during postoperative physical examinations to aid blinding.4 Three patients were lost to follow-up, including 1 patient who was killed in military combat.4 Study results showed no statistically significant difference in ROM, similar failure rates between the 2 groups, and comparable functional outcome scores.4 The authors concluded that patients should be treated arthroscopically given the similar outcomes.4
Fabbriciani
This is a level I trial conducted with a civilian patient population and a mean follow-up time of 24 months for isolated Bankart lesion using metallic suture anchors.16 Inclusion criteria included anterior shoulder instability secondary to trauma, no symptoms or shoulder surgery prior to trauma, no more than 4 episodes of anterior shoulder instability, Hill-Sachs lesion equal to or less than 30% of the humeral head surface, and a lack of multidirectional instability.16 Exclusion criteria included gross elongation or absence of the anteroinferior glenohumeral ligament, labrum detachment extended to the inferior part of the glenoid, anterior labrum periosteal sleeve avulsion lesion, rotator interval tear, elongation or tear of the middle glenohumeral ligament, superior labral anterior posterior lesion, glenoid bone defect, and rotator cuff tear.16 Patients were randomized by SPSS software, and the authors did not state the loss of any patients to follow-up.16 Study results showed no statistically significant Constant score difference, no recurrent dislocations in either group, ROM significantly greater in the arthroscopic group, higher Rowe score in the arthroscopic group (not statistically significant), no difference in pain between the 2 groups, nonstatistically significant increase in stability in the open group.16 The authors concluded that arthroscopic repair with suture anchors is effective for isolated Bankart lesions.16
Jorgensen
This is a level II trial conducted with a mean follow-up time of 36 months in civilian patients with recurrent anterior shoulder dislocation.30 Inclusion criteria included a history of posttraumatic, recurrent, unilateral, anterior shoulder dislocation; complaints of shoulder instability that did not respond to a shoulder training program; normal ROM; positive apprehension sign; increased anterior translation; or negative sulcus test result on physical examination.30 Exclusion criteria included multidirectional instability or previous shoulder surgery.30 Patients were randomized by their address within Copenhagen, and participants wore T-shirts during postoperative physical examinations to aid blinding.30 No patients were lost to follow-up.30 Study results showed 1 arthroscopic group and no open group redislocations, 1 arthroscopic group subluxation and 2 open group subluxations, higher Rowe score in the open group (nonstatistically significant), higher Constant score in the arthroscopic group (nonstatistically significant), or greater ROM in the arthroscopic group.30 Given the results, in conjunction with fewer cosmetic problems and shorter hospital stays, arthroscopic repair for the treatment of recurrent anterior shoulder dislocation was recommended.30
Sperber
This is a level I trial conducted with a mean follow-up time of 24 months.51 Inclusion criteria included patients at least 18 years of age; unilateral, recurrent, posttraumatic anterior shoulder dislocations or subluxations; and arthroscopically verified Bankart lesion.51 Exclusion criteria included bony Bankart lesion greater than 5 mm, primary dislocation, generalized joint laxity, bilateral instability, multidirectional instability, and soft tissue injury that could lead to instability.51 Patients were randomized by sealed envelope, and the authors did not state the loss of any patients to follow-up.51 Study results showed 7 arthroscopic group and 3 open group redislocations (nonstatistically significant), higher Rowe and Constant scores in the arthroscopic group (nonstatistically significant), and greater loss of external rotation in the arthroscopic group.51 They concluded that the arthroscopic repair with absorbable tacks resulted in less pain and minimal loss of external rotation but also a tendency toward a higher number of redislocations than in the open repair group.51
Methodological Quality and Risk of Bias
The quality assessment scores of the 4 trials range from 7 to 8. According to our cutoff values for quality, all 4 trials were classified as high (Table 1); the 4 trials appear well conducted with minimum follow-up periods of 2 years. However, several methods utilized in the trials have the potential to inflict bias on the results. The relatively small sample sizes compared with the prevalence of the condition (218 total patients in the 4 studies combined) may yield random bias as a result of limited power. While treatment group allocation was randomized in all trials, it was not concealed in the Jorgensen trial. Patients were randomly assigned to arthroscopic or open treatment based on their address within Copenhagen.30 Blinding of outcome assessors was reported in detail in the Bottoni and Jorgensen studies, but it was not explicitly stated in the Fabbriciani and Sperber trials.
Another potential source of bias is the method used for data analysis. Intention-to-treat analysis was briefly mentioned in the Bottoni study, but it was not used in the other 3 trials. Patient baseline characteristics, percentage of patients available for follow-up, clinical appropriateness of outcome measures, and length of follow-up were comparable in all 3 trials. All the patients in the Bottoni study are active military personnel who may place more burden on their shoulders compared with the study participants enrolled from the civilian public in the other trials. This is a potential source of bias because it is not a true representation of the general population because of the rigorous physical demands placed on the cadets and their strict compliance with rehabilitation.5
Primary Outcome Measures
Reinjury/recurrent instability
There was one redislocation in the arthroscopic group of the Jorgensen trial, while 1 patient treated arthroscopically and 2 patients treated with open repair in the Jorgensen trial suffered from postoperative subluxations.30 There were no recurrent dislocations in either group of the Bottoni or Fabbriciani studies. Two patients from the open repair group of the Bottoni study suffered reinjury. One patient had recurrent subluxation, and the other sustained a shoulder injury from an assault.4 There was no report of subluxation or reinjury in the Fabbriciani study. Two traumatic redislocations, 1 atraumatic redislocation, and 4 subluxations/reinjuries occurred in the arthroscopically treated patients from the Sperber trial.51 In the open repair group of the Sperber trial, there were 3 reinjuries, including 1 traumatic redislocation. It is not clear if any of the remaining 4 recurrences in the open group and the 2 other recurrences in the arthroscopic group were subluxations.
As a result of reinjury, 1 patient from the arthroscopic group in the Jorgensen trial underwent reoperation at 120 months.30 Three patients from the Bottoni study, all from the open repair group, underwent reoperation.4 Two patients in the arthroscopic group of the Sperber trial underwent reoperation, 1 for recurrent instability and the other to remove a broken Suretac tack.51 Similarly, the only reoperation in the open group of the Sperber trial was to remove a loose anchor.51 Fabbriciani et al did not report any reoperations.16
Return to activity
Jorgensen et al employed a subjective patient survey to classify return to activity into 4 distinct groups.30 In the arthroscopic group, 18 patients (85.7%) regained good (7 patients, 33%) or excellent (11 patients, 52.4%) return to preinjury activity levels, while 2 patients (9.5%) were unchanged, and 1 patient (4.8%) suffered a reduction in activity level compared with pretreatment levels.30 Twenty patients (100%) treated by open technique in the Jorgensen trial regained activity, while 8 (40%) did so with some restrictions.30 Bottoni et al defined return to pre-injury activity as full, active military duty without physical limitations and restrictions.4 Fifty-seven patients (93.4%) returned to preinjury activity levels, while 1 patient in the arthroscopic group reported persistent shoulder pain without instability and was discharged from the military.4
Functional assessment measures and shoulder rating scales
All 4 trials used the Rowe score,47 and none of them found a statistically significant difference in mean score between the arthroscopic and open repair groups. Three of the trials16,30,51 measured the Constant score10 without a statistically significant difference in mean score between the arthroscopic and open repair groups. In addition, Bottoni et al measured the Single Assessment Numeric Evaluation score, University of California–Los Angeles score, Simple Shoulder Test score, and Western Ontario Shoulder Instability score (Table 4). There were no statistically significant differences between the 2 treatment groups for any of these measures.4
Table 4.
Functional score outcomes.a
| Rowe | Constant | SANE | UCLA | SST | WOSI | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | Arthro | Open | Arthro | Open | Arthro | Open | Arthro | Open | Arthro | Open | Arthro | Open |
| Bottoni4 | 91.6 | 86.0 | — | — | 93.5 | 90.6 | 94.4 | 90.0 | 95.0 | 90.8 | 433.6 | 505.8 |
| Fabbriciani16 | 91 | 86.5 | 89.5 | 86.7 | — | — | — | — | — | — | — | — |
| Sperber51 | 100 (90-100) | 95 (75-100) | 100 (82-100) | 98 (67-100) | — | — | — | — | — | — | — | — |
| Jorgensen30 | 92.5 (45-100) | 95 (55-100) | 62 (41-74) | 59.5 (30-71) | — | — | — | — | — | — | — | — |
In means, with ranges in parentheses. SANE, Single Assessment Numeric Evaluation; UCLA, University of California–Los Angeles; SST, Simple Shoulder Test; WOSI, Western Ontario Shoulder Instability.
Pain
Persistent pain was reported with regard to treatment failure in the Bottoni trial. One patient from the arthroscopic group had persistent shoulder pain without instability and was medically discharged from the military.4 Fabbriciani et al reported pain as a subset of the Rowe and Constant scores. The study described identical results for the arthroscopic and open repair groups for both the Rowe score (8.5 ± 2.42) and Constant score (13.5 ± 2.42), thereby raising suspicion for the validity of the results.16 Sperber et al noted lasting pain in 3 participants, all of whom were in the open repair group.51 Jorgensen et al did not specifically report data on pain.30
Secondary Outcome Measures
Range of motion
None of the 4 trials found clinically significant differences in postoperative ROM between the 2 groups. Jorgensen et al found that 5 patients in the open group and 1 patient in the arthroscopic group had up to a 25% reduction in external rotation.30 In addition, 2 patients in the open group had up to a 50% reduction in external rotation and up to 25% reduction in abduction (P = 0.04).30 Bottoni et al found miniscule differences in 3 measures of ROM. The patients in the arthroscopic group exhibited statistically significant increases in external rotation compared with that of patients in the open group.4 However, the clinical ramifications and significance of these results are difficult to interpret. For example, Fabbriciani et al found a statistically significant difference between the 2 groups in the ROM portion of the Constant score,16 while Sperber et al found only a 1-degree-greater external rotation ROM in the arthroscopic group.51
Objective instability
Jorgensen et al measured objective instability with the most analytic rigor. They incorporated an instrumented test with the DonJoy Knee Laxity Tester (Smith & Nephew) to assess anteroposterior translation of the shoulder joint.30 They reported a very small, statistically nonsignificant difference between the 2 groups. Objective instability was not reported in the Bottoni or Fabbriciani trial. Sperber et al reported a positive apprehension test result in 3 patients treated with open repair, while none of the patients in the arthroscopic group had a positive apprehension test result.
Patient satisfaction (subjective instability)
None of the studies explicitly reported patient satisfaction. However, subjective stability was assessed as a component of the Rowe score in the Fabbriciani and Jorgensen trials. The difference between the 2 groups in each study was not statistically significant.16,30
Complications
Neither Bottoni et al nor Fabbriciani et al reported any perioperative complications. Sperber et al reported injury to the long thoracic nerve in 1 patient treated by arthroscopic intervention.51 Furthermore, 1 patient in each group of the Sperber trial underwent reoperation for broken surgical implants.51 Jorgensen et al reported 1 superficial wound infection and 1 patient complaining of hyperesthesia in the arthroscopic group.30 In addition, 4 patients in the open group complained of hyperesthesia around the scar.30
Discussion
The 4 included trials each directly compare arthroscopic versus open treatment for recurrent, unilateral, anterior shoulder instability. The results displayed no statistically significant difference between the 2 groups with regard to recurrent instability, return to activity, and reoperation rates. For other outcomes, including shoulder function, either there were no statistically significant differences between the 2 groups, or the differences were small.
We identified 3 previously published systematic reviews with meta-analyses comparing arthroscopic and open repair for recurrent anterior shoulder instability.19,37,42 All 3 reviews combined studies with a variety of study designs and outcome measures, which can lead to heterogeneity in results.12
Does open or arthroscopic repair lead to lower recurrence rates?
The RCTs included in this review demonstrated no significant difference in recurrence rates between patients treated by open technique and those treated by arthroscopic intervention.4,16,30,51 Two studies, Bottoni et al and Fabbriciani et al, compared arthroscopic and open repair using suture anchors, which is the current gold standard surgical technique. These studies did not show statistically significant differences in recurrence rates between the 2 treatment groups.4,16 Meta-analyses reviewing this clinical question have drawn a different conclusion. Mohtadi et al42 documented a 2.04 odds ratio (P = 0.0003) of recurrent instability in those treated arthroscopically compared with those treated by open repair. Similarly, Lenters et al37 noted a 2.27 relative risk (RR; P < 0.00001) of recurrent instability, a 2.74 RR of recurrent dislocation (P < 0.0001), and a RR of 2.23 (P = 0.002) for reoperation in patients undergoing arthroscopic stabilization compared with those treated by open technique. In a systematic review of 6 studies, Freedman et al reported that arthroscopic Bankart repair using transglenoid sutures or bioabsorbable tacks resulted in a higher rate of recurrence compared with open techniques (P = 0.01).19 It is important to note that each of these studies contained studies that are not level I or II evidence. In addition, surgical techniques varied by study, many of which are not currently accepted treatment methods.
Is ROM superior following open or arthroscopic repair?
Arthroscopic intervention leads to a small improvement in postoperative ROM. Bottoni et al4 and Sperber et al51 found no statistically significant difference in ROM between patients in the 2 treatment groups. Meanwhile, Fabbriciani et al16 and Jorgensen et al30 noted a statistically significant improvement in ROM along several axes following arthroscopic surgery when compared with ROM following open repair. These differences were most notable in external rotation.
Does arthroscopic or open intervention lead to a better return to activity or function?
Bottoni et al reported that 93.4% of patients had a sufficient return to activity level.4 However, 1 patient in the arthroscopic group was discharged from the military, while 3 patients in the open group were lost to follow-up. Joregensen et al found that 85.7% of patients in the arthroscopic group and 100% of patients in the open group returned to preinjury activity levels.30 However, 7 patients in the arthroscopic group and 8 patients in the open group did so with some restrictions.30 In addition, Cole et al found that 14% of patients in the arthroscopic group and 18% of patients in the open group experienced moderate return to activity limitations, while 11% in the arthroscopic treatment group and 5% in the open repair group suffered from severe limitations in return to activity.8 Mohtadi et al noted that open repair offers a better outcome than arthroscopic repairs with respect to return to activity.42 However, the inclusion of studies with a wide variety of study designs and a high risk of bias limits the reliability of these findings. Lenters et al also found that open repair is superior with respect to postoperative functioning. They noted a RR of 0.87 (P = 0.03) for return to sports and work in the arthroscopic group compared with the open repair group.37
Limitations
A major limitation of this review is that only 4 level I or II RCTs comparing arthroscopic and open surgical repair have been conducted for this common shoulder injury. Because of this shortcoming, there is a potential for systematic bias in the validity of the evidence. Therefore, these findings should be interpreted with caution. During the review process, all of the qualified studies may not have been identified. The 4 RCTs vary in their inclusion and exclusion criteria, surgical techniques, suture material, number of tacks/suture anchors, and postoperative rehabilitation programs. Some results, such as ROM and return to activity, are difficult to compare because of differences in reporting throughout the studies.
A major limitation of the Jorgensen trial is that the patient treatment group allocation was not completely randomized; that is, the patient’s address determined the treatment.30 In addition, limited data on cost-effectiveness of varying treatments was available from the 4 RCTs. This information is indispensable for the decision-making process of care providers.
Conclusions
While the treatment of recurrent anterior shoulder instability has traditionally been treated by an open approach, more recently, arthroscopic techniques have achieved similar results. While limited, the available evidence from RCTs does not show a statistically significant difference in outcome measures between arthroscopic and open repair for the treatment of recurrent anterior shoulder instability. Specifically, studies comparing the currently accepted surgical techniques involving suture anchors did not show statistically significant differences in recurrence rates between the 2 treatment groups. Given the similar results between the 2 groups, differences in length of hospital stay and cost to the patient and society point to arthroscopic repair as the more judicious treatment approach.
Footnotes
References
- 1. Akpinar S, Demirhan M, Kilicoglu O, et al. Modification of Bankart reconstruction with lateral capsulotomy and selective anatomic repair using suture anchors. Bull Hosp Jt Dis. 2000;59:88-93 [PubMed] [Google Scholar]
- 2. Bacilla P, Field LD, Savoie FH., 3rd Arthroscopic Bankart repair in a high demand patient population. Arthroscopy. 1997;13:51-60 [DOI] [PubMed] [Google Scholar]
- 3. Bhagia SM, Ali MS. Bankart operation for recurrent anterior dislocation of the shoulder using suture anchor. Orthopedics. 2000;23:589-591 [DOI] [PubMed] [Google Scholar]
- 4. Bottoni CR, Smith EL, Berkowitz MJ, Towle RB, Moore JH. Arthroscopic versus open shoulder stabilization for recurrent anterior instability: a prospective randomized clinical trial. Am J Sports Med. 2006;34:1730-1737 [DOI] [PubMed] [Google Scholar]
- 5. Bottoni CR, Wilckens JH, DeBerardino TM, et al. A prospective, randomized evaluation of arthroscopic stabilization versus nonoperative treatment in patients with acute, traumatic, first-time shoulder dislocations. Am J Sports Med. 2002;30:576-580 [DOI] [PubMed] [Google Scholar]
- 6. Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy. 2000;16:677-694 [DOI] [PubMed] [Google Scholar]
- 7. Caspari RB. Arthroscopic reconstruction for anterior shoulder instability. Tech Orthop. 1988;3:59-66 [PubMed] [Google Scholar]
- 8. Cole BJ, Linsalata J, Irrgang J, Warner JJ. Comparison of arthroscopic and open anterior shoulder stabilization: a two to six-year follow-up study. J Bone Joint Surg Am. 2000;82:1108-1114 [DOI] [PubMed] [Google Scholar]
- 9. Cole BJ, Warner JJ. Arthroscopic versus open Bankart repair for traumatic anterior shoulder instability. Clin Sports Med. 2000;19:19-48 [DOI] [PubMed] [Google Scholar]
- 10. Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160-164 [PubMed] [Google Scholar]
- 11. Coughlin LP, Rubinovich M, Johansson J, et al. Arthroscopic staple capsulorrhaphy for anterior shoulder instability. Am J Sports Med. 1992;20:253-256 [DOI] [PubMed] [Google Scholar]
- 12. Dersimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177-188 [DOI] [PubMed] [Google Scholar]
- 13. Dickson JW, Devas MB. Bankarts operation for recurrent dislocation of the shoulder. J Bone Joint Surg Br. 1957;39:114-119 [DOI] [PubMed] [Google Scholar]
- 14. Dora C, Gerber C. Shoulder function after arthroscopic anterior stabilization of the glenohumeral joint using an absorbable tac. J Shoulder Elbow Surg. 2000;9:294-298 [DOI] [PubMed] [Google Scholar]
- 15. Ejerhed L, Kartus J, Funck E, et al. Absorbable implants for open shoulder stabilization: a clinical and serial radiographic evaluation. J Shoulder Elbow Surg. 2000;9:93-98 [PubMed] [Google Scholar]
- 16. Fabbriciani C, Milano G, Demontis A, Fadda S, Ziranu F, Mulas PD. Arthroscopic versus open treatment of Bankart lesion of the shoulder: a prospective randomized study. Arthroscopy. 2004;20:456-462 [DOI] [PubMed] [Google Scholar]
- 17. Ferretti A, De Carli A, Calderaro M, et al. Open capsulorrhaphy with suture anchors for recurrent anterior dislocation of the shoulder. Am J Sports Med. 1998;26:625-629 [DOI] [PubMed] [Google Scholar]
- 18. Field L, Savoie F, Griffith P. A comparison of open and arthroscopic Bankart repair [abstract]. J Shoulder Elbow Surg. 1999;8:195 [Google Scholar]
- 19. Freedman KB, Smith AP, Romeo AA, Cole BJ, Bach BR., Jr Open Bankart repair versus arthroscopic repair with transglenoid sutures or bioabsorbable tacks for recurrent anterior instability of the shoulder: a meta-analysis. Am J Sports Med. 2004;6:1520-1527 [DOI] [PubMed] [Google Scholar]
- 20. Gartsman GM, Roddey TS, Hammerman SM. Arthroscopic treatment of anterior-inferior glenohumeral instability: two- to five-year followup. J Bone Joint Surg Am. 2000;82:991-1003 [DOI] [PubMed] [Google Scholar]
- 21. Geiger D, Hurley J, Tovey J, Rao J. Results of arthroscopic versus open Bankart suture repair. Clin Orthop Relat Res. 1997;337:111-117 [DOI] [PubMed] [Google Scholar]
- 22. Gill TJ, Micheli LJ, Gebhard F, et al. Bankart repair for anterior instability of the shoulder: long-term outcome. J Bone Joint Surg Am. 1997;79:850-857 [DOI] [PubMed] [Google Scholar]
- 23. Green MR, Christensen KP. Arthroscopic versus open Bankart procedures: a comparison of early morbidity and complications. Arthroscopy. 1993;4:371-374 [DOI] [PubMed] [Google Scholar]
- 24. Gross RM. Arthroscopic shoulder capsulorraphy: does it work? Am J Sports Med. 1989;17:495-499 [DOI] [PubMed] [Google Scholar]
- 25. Guanche C, Quick D, Sodergen K. Arthroscopic versus open reconstruction of the shoulder with isolated Bankart lesions. Am J Sports Med 1996;24:144-148 [DOI] [PubMed] [Google Scholar]
- 26. Handoll HH, Almaiyah MA, Rangan A. Surgical versus non-surgical treatment for acute anterior shoulder dislocation. Cochrane Database Syst Rev. 2004;1:CD004325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hobby J, Griffin D, Dunbar M, Boileau P. J Bone Joint Surg Br. 2007;89(9):1188-1196 [DOI] [PubMed] [Google Scholar]
- 28. Hovelius L. Incidence of shoulder dislocation in Sweden. Clin Orthop Relat Res. 1982;166:127-131 [PubMed] [Google Scholar]
- 29. Hubbell JD, Ahmad S, Bezenoff LS, Fond J, Pettrone FA. Comparison of shoulder stabilization using arthroscopic transglenoid sutures versus open capsulolabral repairs: a 5-year minimum follow-up. Am J Sports Med. 2004;3:650-654 [DOI] [PubMed] [Google Scholar]
- 30. Jorgensen U, Svend-Hansen H, Bak K, Pedersen I. Recurrent post-traumatic anterior shoulder dislocation: open versus arthroscopic repair. Knee Surg Sports Traumatol Arthrosc. 1999;7:118-124 [DOI] [PubMed] [Google Scholar]
- 31. Karlsson J, Kartus J, Ejerhed L, et al. Bioabsorbable tacks for arthroscopic treatment of recurrent anterior shoulder dislocation. Scand J Med Sci Sports. 1998;8:411-415 [DOI] [PubMed] [Google Scholar]
- 32. Karlsson J, Magnusson L, Ejerhed L, Hultenheim I, Lundin O, Kartus J. Comparison of open and arthroscopic stabilization for recurrent shoulder dislocation in patients with a Bankart lesion. Am J Sports Med. 2001;5:538-542 [DOI] [PubMed] [Google Scholar]
- 33. Kazar R, Relovszky E. Prognosis of primary dislocation of the shoulder. Acta Orthop Scand. 1969;2:216-224 [DOI] [PubMed] [Google Scholar]
- 34. Kim SH, Ha KI, Kim SH. Bankart repair in traumatic anterior shoulder instability: open versus arthroscopic technique. Arthroscopy. 2002;7:755-763 [DOI] [PubMed] [Google Scholar]
- 35. Lane JG, Sachs RA, Riehl B. Arthroscopic staple capsulorrhaphy: a long-term follow-up. Arthroscopy. 1993;9:190-194 [DOI] [PubMed] [Google Scholar]
- 36. Laurencin CT, Stephens S, Warren RF, et al. Arthroscopic Bankart repair using a degradable tack: a followup study using optimized indications. Clin Orthop. 1996;332:132-137 [DOI] [PubMed] [Google Scholar]
- 37. Lenters TR, Franta FM, Leopold SS, Matsen FA. Arthroscopic compared with open repairs for recurrent anterior shoulder instability: a systematic review and meta-analysis of the literature. J Bone Joint Surg Am. 2007;89:244-254 [DOI] [PubMed] [Google Scholar]
- 38. Levine WN, Richmond JC, Donaldson WR. Use of the suture anchor in open Bankart reconstruction: a follow-up report. Am J Sports Med. 1994;22:723-726 [DOI] [PubMed] [Google Scholar]
- 39. Martinez Martin AA, Herrera Rodriguez A, Panisello Sebastian JJ, et al. Use of the suture anchor in modified open Bankart reconstruction. Int Orthop. 1998;22:312-315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Matthews LS, Vetter WL, Oweida SJ, et al. Arthroscopic staple capsulorrhaphy for recurrent anterior shoulder instability. Arthroscopy. 1988;4:106-111 [DOI] [PubMed] [Google Scholar]
- 41. Mizuno K, Nabeshima Y, Hirohata K. Analysis of Bankart lesion in the recurrent dislocation or subluxation of the shoulder. Clin Orthop. 1993;288:158-165 [PubMed] [Google Scholar]
- 42. Mohtadi NG, Bitar IJ, Sasyniuk TM, Hollinshead RM, Harper WP. Arthroscopic versus open repair for traumatic anterior shoulder instability: a meta-analysis. Arthroscopy. 2005;21:652-658 [DOI] [PubMed] [Google Scholar]
- 43. Mohtadi NG, Hollinshead RM, Ceponis PJ, Chan DS, Fick GH. A multi-centre randomized controlled trial comparing electrothermal arthroscopic capsulorrhaphy versus open inferior capsular shift for patients with shoulder instability: protocol implementation and interim performance: lessons learned from conducting a multi-centre RCT [ISRCTN68224911; NCT00251160]. Trials. 2006;7:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Pulavarti RS, Symes TH, Rangan A. Surgical interventions for anterior shoulder instability in adults. Cochrane Database Syst Rev. 2009;1:CD005077 [DOI] [PubMed] [Google Scholar]
- 45. Resch H, Povacz P, Wambacher M, et al. Arthroscopic extra-articular Bankart repair for the treatment of recurrent anterior shoulder dislocation. Arthroscopy. 1997;13:188-200 [DOI] [PubMed] [Google Scholar]
- 46. Rowe CR. Prognosis in dislocations of the shoulder. J Bone Joint Surg Am. 1956;5:957-977 [PubMed] [Google Scholar]
- 47. Rowe CR, Patel D, Southmayd WW. The Bankart procedure: a long-term end-result study. J Bone Joint Surg Am. 1978;60:1-16 [PubMed] [Google Scholar]
- 48. Rowe CR, Sakellarides HT. Factors related to recurrences of anterior dislocations of the shoulder. Clin Orthop. 1961;20:40-48 [PubMed] [Google Scholar]
- 49. Salomonsson B, Jonsson U, Abbaszadegan H, Halvorsen D. Randomized study between capsular shift with Bankart repair and Putti-Platt (abstract). J Shoulder Elbow Surg. 1996;5:S55 [Google Scholar]
- 50. Simonet WT, Melton LJ, 3rd, Cofield RH, Ilstrup DM. Incidence of anterior shoulder dislocation in Olmsted County, Minnesota. Clin Orthop Relat Res. 1984;186:186-191 [PubMed] [Google Scholar]
- 51. Sperber A, Hamberg P, Karlsson J, Sward L, Wredmark T. Comparison of an arthroscopic and an open procedure for posttraumatic instability of the shoulder: a prospective, randomized multicenter study. J Shoulder Elbow Surg. 2001;10:105-108 [DOI] [PubMed] [Google Scholar]
- 52. Sperling JW, Duncan SF, Torchia ME, ODriscoll SW, Cofield RH. Bankart repair in patients aged fifty years or greater: results of arthroscopic and open repairs. J Shoulder Elbow Surg. 2005;2:111-113 [DOI] [PubMed] [Google Scholar]
- 53. Steinbeck J, Jerosch J. Arthroscopic transglenoid stabilization versus open anchor suturing in traumatic anterior instability of the shoulder. Am J Sports Med. 1998;26:373-378 [DOI] [PubMed] [Google Scholar]
- 54. Takeda H, Watarai K, Ganev GG, et al. Modified Bankart procedure for recurrent anterior dislocation and subluxation of the shoulder in athletes. Int Orthop. 1998;22:361-365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Thomas SC, Matsen FA. An approach to the repair of avulsion of the glenohumeral ligaments in the management of traumatic anterior glenohumeral instability. J Bone Joint Surg Am. 1989;71:506-513 [PubMed] [Google Scholar]
- 56. Traina SM, Holtgrewe JL, King S. Modification of the Bankart reconstruction using a suture anchor. J South Orthop Assoc. 1998;7:180-186 [PubMed] [Google Scholar]
- 57. Uhorchak JM, Arciero RA, Huggard D, et al. Recurrent shoulder instability after open reconstruction in athletes involved in collision and contact sports. Am J Sports Med. 2000;28:794-799 [DOI] [PubMed] [Google Scholar]
- 58. Ungersbock A, Michel M, Hertel R. Factors influencing the results of a modified Bankart procedure. J Shoulder Elbow Surg. 1995;4:365-369 [DOI] [PubMed] [Google Scholar]
- 59. Weber SC. Arthroscopic suture anchor versus traditional open Bankart repair in the management of recurrent anterior shoulder dislocation [abstract]. J Shoulder Elbow Surg. 1999;2:181-182 [Google Scholar]
- 60. Wolf EM, Wilk RM, Richmond JC. Arthroscopic Bankart repair using suture anchors. Oper Tech Orthop. 1991;1:184-191 [Google Scholar]