Abstract
Background:
Collegiate baseball pitchers, as well as position players, exhibit increased humeral retrotorsion compared with individuals with no history of overhead sport participation. Whether the humeral retrotorsion plays a role in the development of throwing-related injuries that are prevalent in collegiate baseball pitchers is unknown.
Hypotheses:
Humeral retrotorsion will be significantly different in collegiate pitchers with throwing-related shoulder or elbow injury history compared with pitchers with no injury history. Humeral retrotorsion can also discriminate participants with and without shoulder or elbow injury.
Study Design:
Cross-sectional study.
Methods:
Comparisons of ultrasonographically-obtained humeral retrotorsion were made between 40 collegiate pitchers with and without history of throwing-related shoulder or elbow injury. The ability of humeral retrotorsion to discriminate injury history was determined from the receiver operating characteristic area under the curve.
Results:
Participants with an elbow injury history demonstrated a greater humeral retrotorsion limb difference (mean difference = 7.2°, P = 0.027) than participants with no history of upper extremity injury. Participants with shoulder injury history showed no differences in humeral torsion compared with participants with no history of injury. Humeral retrotorsion limb difference exhibited a fair ability (receiver operating characteristic area under the curve = 0.74) to discriminate elbow injury history.
Conclusions:
Collegiate pitchers with a history of elbow injury exhibited a greater limb difference in humeral retrotorsion compared with pitchers with no history of injury. No differences in humeral retrotorsion variables were present in participants with and without shoulder injury history.
Clinical Relevance:
Baseball players with a history of elbow injury demonstrated increased humeral retrotorsion, suggesting that the amount of retrotorsion and the development of elbow injury may be associated.
Keywords: shoulder, elbow, baseball, injury, retroversion
Bilateral difference in the glenohumeral rotation range of motion is a common characteristic among competitive baseball players. Specifically, a typical baseball player would present with greater external rotation and less internal rotation on the dominant limb.4,5,12,17,35,39 While this bilateral difference is considered a healthy adaptation in baseball players, studies demonstrate that these limb differences in humeral rotation are more pronounced in those individuals diagnosed with a throwing-related shoulder or elbow injury, which indicates that changes in soft tissue characteristics (ie, passive joint rotation range of motion) beyond what is considered a normal adaptation may be associated with injuries.7,14,26,27,36
The bilateral limb difference in humeral rotation is often attributed to soft tissue tightness in the posterior shoulder. However, the limb difference is also influenced by the amount of humeral retrotorsion present within the upper extremity.28,35,40 For example, Myers et al28 demonstrated that the almost 15° of limb difference in humeral internal rotation found in baseball players became negligible once the amount of retrotorsion was accounted for. As such, the range of motion differences that are seen clinically with throwing-related upper extremity pain/injury may be partially explained by the amount of retrotorsion present and not soft tissue tightness alone.
Research studies that examine the role that retrotorsion plays in throwing-related upper extremity injury are limited. It has been suggested that overhead athletes with increased humeral retrotorsion may be at less risk of shoulder injury.12,31,33 For example, Pieper et al33 demonstrated that competitive handball players with chronic shoulder pain had less retrotorsion in the dominant limb compared with the players with no shoulder pain. The authors hypothesized that the increased humeral retrotorsion may be an adaptation to repetitive external rotation from throwing during growth and that the athletes who failed to acquire the retrotorsion adaptations may experience the shoulder pain and anterior glenohumeral instability because they place more strain on their anterior capsules as the arm moves into external rotation during throwing.
Whiteley et al43 conducted the only study to date specific to baseball players and throwing-related injury and demonstrated that the amount of retrotorsion present in the nondominant arm was predictive of whether upper extremity injury occurred in adolescent baseball players. In adolescent baseball players, having less retrotorsion in the nondominant limb was found to be predictive of throwing arm injury incidence. The retrotorsion on the nondominant limb is considered to represent the amount of retrotorsion the individual was born with (congenital retrotorsion). Yet the amount of humeral retrotorsion in the dominant limb represents the amount of retrotorsion gained from throwing adaptation superimposed on the congenital retrotorsion. Thus, the limb difference in humeral retrotorsion represents the amount of retrotorsion acquired on the dominant limb. It is thought that the less congenital retrotorsion an athlete has, the more retrotorsion the athlete has to acquire to place one’s limb in a cocking position. The authors speculated that the greater need/room for osseous adaptation makes the athlete susceptible to a throwing-related injury. However, due to the limited number of studies conducted in this area, it is still unclear what role retrotorsion plays in injury in the overhead athlete.
Baseball pitchers are especially prone to throwing-related shoulder and elbow injuries, with higher incidences of injury reported at the high school,20 collegiate,13,24 and professional levels11 when compared with their position player counterparts. Thus, understanding the role that retrotorsion plays in the injuries that occur in a pitching population will be beneficial given the high incidence of pitching injuries reported. The purpose of this study was to compare dominant-limb retrotorsion, nondominant-limb retrotorsion, and bilateral limb difference retrotorsion in collegiate pitchers with and without a history of throwing-related shoulder or elbow injury.
Methods
Participants
Forty collegiate division I baseball pitchers participated in the current study. All participants reported playing baseball for at least 10 years (14.0 ± 1.9 years) and having pitched for at least 5 years (7.8 ± 4.1 years). The average age that participants started playing baseball was 5.2 years (range, 2-9 years). Complete participant demographics appear in Table 1. Prior to the initiation of this study, an a priori sample size estimate was conducted based on pilot humeral retrotorsion data as well as our previous work.28 It was determined that 10 participants would sufficiently power the analyses.
Table 1.
Participant demographics.a
| Dominant Limb | Nondominant Limb | |||
|---|---|---|---|---|
| ER (°) | IR (°) | ER (°) | IR (°) | |
| All participantsb | 126.0 ± 12.1 | 40.6 ± 13.0 | 120.2 ± 10.8 | 50.8 ± 10.7 |
| Shoulder injury | ||||
| History | 129.0 ± 12.3 | 39.2 ± 10.6 | 124.8 ± 8.8 | 51.6 ± 10.6 |
| No history | 124.6 ± 11.9 | 41.2 ± 14.1 | 118.0 ± 11.1 | 50.4 ± 11.0 |
| Elbow injury | ||||
| History | 126.8 ± 12.3 | 47.4 ± 17.8 | 121.2 ± 8.7 | 55.5 ± 10.7 |
| No history | 125.7 ± 12.1 | 36.9 ± 7.6 | 119.7 ± 11.9 | 48.3 ± 10.0 |
ER, external rotation range of motion; IR, internal rotation range of motion.
Age, 19.3 ± 1.2 years; height, 186.0 ± 7.4 cm; mass, 88.1 ± 9.9 kg.
Procedures
All participants attended 1 testing session where University of North Carolina at Chapel Hill–approved informed consent was obtained. Throwing-related injury history was obtained for each participant, allowing for documentation of the upper extremity injuries sustained in the past 3 years. Injury histories beyond 3 years were not obtained, because of concerns for participant recall, ability to verify injuries, and changes in skeletal maturity. All injuries were verified when possible through injury surveillance records kept by the sports medicine staff that provided medical coverage. An injury was defined as the diagnosis of some pathology to the shoulder or elbow that (1) directly resulted from throwing and (2) resulted in either participation loss or significant participation modification (eg, a player not able to pitch/throw but perhaps play another position or bat in the game or practice).
Humeral retrotorsion was assessed utilizing the indirect ultrasonographic techniques described by Myers et al,28 Whiteley et al,42 and Yamamoto et al.45 Prior to the current study, we established construct validity, reliability, and precision of the retrotorsion assessment, yielding intrasession, intersession, and intertester reliability coefficients ranging from 0.96 to 0.98, with an average of 2.3° of measurement error.28 Participants lay supine on a treatment table with 90° of shoulder abduction and elbow flexion. A tester positioned a 4-cm linear array ultrasound transducer (LOGIQe, General Electric, Milwaukee, Wisconsin) on the participant’s anterior shoulder with the ultrasound transducer level with the plane of the treatment table (verified with a bubble level) and aligned perpendicular to the long axis of the humerus in the frontal plane. The second tester then rotated the humerus so that the bicipital groove appeared in the center of the ultrasound image, with the line connecting the apexes of greater and lesser tubercles parallel to the horizontal plane. A grid was applied to the display of the ultrasound unit to aid examiners with positioning of the humeral tubercles. The second tester then placed a digital inclinometer on the ulnar side of the forearm, pressing firmly against the ulna, and recorded the forearm inclination angle with respect to horizontal (Figure 1). Since the ulna extends perpendicular to the elbow epicondylar axis (line connecting the medial and lateral epicondyles), this angle reflects the angular difference between the epicondylar axis (distal humerus) and the line perpendicular to the line connecting the apexes of the greater and lesser tubercles (proximal humerus), thus representing humeral retrotorsion. Three trials were performed bilaterally and averaged to obtain the dependent variables—namely, dominant-limb humeral retrotorsion, nondominant-limb humeral retrotorsion, and humeral retrotorsion limb difference (dominant-limb humeral retrotorsion minus nondominant-limb humeral retrotorsion). The injury history data were examined after the conclusion of the humeral retrotorsion testing, so the testers were blinded to whether participants reported an injury history. To assist with interpretation of the results of the humeral retrotorsion data, passive humeral rotation range of motion data collected during the retrotorsion data collection session is included in the participant demographics table (Table 1). Passive humeral rotation range of motion data were collected using previously published methodology.28
Figure 1.

Ultrasonographic assessment of humeral retrotorsion.
After data collection was completed, the 40 participants were stratified on the basis of their throwing-related injury history. Of the 40 participants, 19 reported no history of shoulder or elbow injury (no injury history group), 12 reported a history of shoulder injury (shoulder injury history group), and 13 reported an elbow injury history (elbow injury history group).
Two-way analysis of variance models were used to make group comparisons between participants with shoulder injury history and without injury history for the dominant- and nondominant-limb humeral retrotorsion and range of motion variables (limb × group factors). Similarly, participants with an elbow injury history were compared with participants with no history of injury using a 2-way analysis of variance model. Bonferroni correction post hoc analyses were utilized when significant analyses of variance were encountered. To account for risk of type I error, the α levels of the post hoc analyses were corrected from 0.05 to 0.025 to account for the 2 comparisons of interest (between-group comparisons of humeral retrotorsion on dominant and nondominant limb).
Two independent-sample t tests were used to make group comparison of shoulder injury history versus no shoulder injury history and elbow injury versus no elbow injury history for the humeral retrotorsion difference variable. For all variables, comparisons were not made between shoulder and elbow injury history groups, because 4 participants reported a history of both injury types and were thus included in both groups. An α level of 0.05 was set a priori.
In addition, the overall ability of each retrotorsion variable to discriminate between those individuals with and without injury history was assessed using receiver operating characteristic (ROC) curve analysis. An ROC curve provides graphic means for assessing the ability of a screening test to discriminate between healthy and diseased persons (history of injury in the current study).30 The area under the curve is commonly used as a summary measure of diagnostic accuracy and can range from 0.0 to 1.0 (< 0.60 = failed diagnostic capability, 0.60 to 0.70 = poor, 0.70 to 0.80 = fair, 0.80 to 0.90 = good, 0.90 to 1.00 = excellent). All statistical analyses were conducted with SPSS 17.0.
Results
Descriptive statistics, 95% confidence intervals, and ROC statistics for all humeral retrotorsion variables are presented in Table 2. The primary result of this study was that participants with a history of elbow injury demonstrated a significantly greater humeral retrotorsion limb difference (mean difference = 7.2°, P = 0.03) than participants with no history of upper extremity injury (Figure 2). There was a significant limb × group interaction (F1,38 = 4.56, P = 0.04), but the post hoc analyses indicated that there were no significant differences in both dominant and nondominant humeral retrotorsion between participants with and without elbow injury history. No significant interactions were present for either external rotation range of motion (F1,38 = 0.008, P = 0.10) or internal rotation range of motion (F1,38 = 0.819, P = 0.37) between elbow injury history groups.
Table 2.
Humeral retrotorsion descriptive and ROC AUC statistics.a
| Humeral Retrotorsion: Injury History | Mean ± SD (°) | 95% CI (°) | ROC AUC | AUC 95% CI |
|---|---|---|---|---|
| Dominant limb | ||||
| Shoulder | 82.7 ± 9.8 | 76.4-89.0 | 0.485 | 0.268-0.701 |
| Elbow | 83.9 ± 9.4 | 78.2-89.6 | 0.608 | 0.408-0.808 |
| None | 81.4 ± 7.1 | 78.0-84.8 | ||
| Nondominant limb | ||||
| Shoulder | 67.1 ± 11.2 | 60.0-74.2 | 0.543 | 0.321-0.766 |
| Elbow | 63.6 ± 12.9 | 55.8-71.4 | 0.389 | 0.195-0.583 |
| None | 67.0 ± 7.9 | 63.2-70.8 | ||
| Difference | ||||
| Shoulder | 15.6 ± 12.2 | 7.8-23.3 | 0.477 | 0.256-0.698 |
| Elbow | 21.7 ± 7.7b | 16.8-26.5 | 0.735 | 0.580-0.890 |
| None | 14.4 ± 9.4 | 9.8-19.0 |
CI, confidence interval; ROC, receiver operating characteristic; AUC = area under the ROC curve.
Statistically significant difference from the participants with no history of injury (P = 0.03).
Figure 2.
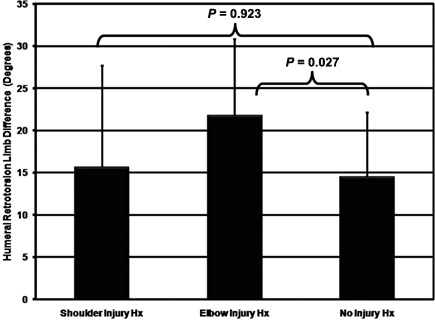
Group descriptive statistics in humeral retrotorsion limb difference.
When comparing participants with shoulder injury history and no history of injury, there were no significant differences (F1,38 = 0.001, P = 0.98) in dominant-limb humeral retrotorsion or nondominant-limb humeral retrotorsion. There were no humeral retrotorsion limb differences (t = −0.667, P = 0.92) between participants with and without shoulder injury history. No significant interactions were present for either external rotation range of motion (F1,38 = 0.611, P = 0.44) or internal rotation range of motion (F1,38 = 0.711, P = 0.40) between shoulder injury history groups.
Of the humeral retrotorsion variables assessed, humeral retrotorsion limb difference best discriminated elbow injury history from participants with no history of injury (ROC area under curve = 0.74).
Discussion
Participants in the current study who reported a throwing-related elbow injury history demonstrated significantly greater humeral retrotorsion limb difference when compared with the participants with no history of injury. However, no differences were present in dominant- or nondominant-limb humeral retrotorsion between groups. This difference represents the amount of throwing-acquired retrotorsion (ie, the difference that results from acquisition of torsion on the throwing-side limb). While side-to-side differences can be observed in all individuals regardless of sports participation history, the amount of humeral retrotorsion limb difference present in baseball players is more pronounced compared with participants with no history of overhead sports participation.28,42 This is most likely a result of the repeated long axis torques placed on the epiphyseal plate of the proximal humerus during throwing.37 Sabick et al37 described the long axis torques that are present during throwing and concluded that they are sufficient to result in humeral retrotorsion alterations.
The participants in the no injury history group demonstrated approximately 15° of difference between limbs. The results of the current study are consistent with our previous work28 and others12,31,35,42-44 that have examined (with radiologic and ultrasonographic methods) side-to-side differences in humeral retrotorsion. In the current study, the participants who reported a history of elbow injury demonstrated approximately 7° of greater torsional limb difference than the participants with no elbow injury history. Our results are in partial agreement with those reported by Whiteley et al43 in that both their findings and ours demonstrated that humeral retrotorsion variables are associated with throwing-related injury. Unlike the current study, however, their study reported that the amount of congenital retrotorsion (ie, the amount of retrotorsion in the nondominant limb) was predictive of upper extremity injury in adolescent baseball players. Our results demonstrated that the amount of acquired retrotorsion (ie, difference in the amount of retrotorsion between limbs) was associated with elbow injury. The differences in results despite similar methodology might be attributed to the difference in age of the baseball players examined (adolescent vs college). For example, Edelson et al15,16 demonstrated that the humeral retrotorsion alterations that occur from natural maturation ceases at approximately 16 years of age. In contrast to the collegiate pitchers studied in this study, who were near full skeletal maturity (average age = 19.3 years), the adolescent pitchers in the study by Whiteley et al43 were skeletally immature (average age = 16.6 years) and therefore may not have developed significant acquired retrotorsion at the time.
Biomechanically, the increased retrotorsion obtained during throwing could contribute to the development of elbow injuries in baseball pitchers. For example, increased humeral retrotorsion is partly responsible for the increased humeral external rotation that is often observed in baseball players.28,31 This increased external rotation contributes to the extreme external rotation achieved during the late cocking phase of pitching. The greater maximum external rotation at the late-cocking-phase position of throwing has been linked to increased valgus torques experienced at the elbow,1,18,38 which has been linked to an increased risk of elbow injury.3 As such, increased humeral retrotorsion may be contributing to the development of elbow injury commonly seen in collegiate baseball players. While the current study cannot determine if the humeral retrotorsion has a causal effect on the elbow injury given the retrospective research design utilized, the study demonstrates a link between the amount of humeral retrotorsion and elbow injury history.
In addition to the group differences seen in the variables associated with humeral retrotorsion limb difference, the ROC curve analyses support the finding that humeral retrotorsion is associated with elbow injury. The area under an ROC curve quantifies the ability of the test to discriminate between those individuals with and without an injury history. In the current study, humeral retrotorsion limb difference was able to discriminate elbow injury history with fair ability (area under the curve = 0.74). For example, if 2 patients were selected at random, 1 with an elbow injury history and 1 without, the probability is 74% that the participant with an elbow injury history will have increased humeral retrotorsion difference. All other humeral retrotorsion variables provided less diagnostic capability.
At the shoulder, there is disagreement regarding the hypothesized role that retrotorsion plays regarding injury. Increased humeral retrotorsion has been hypothesized to play both a detrimental and a protective mechanism for shoulder injury in the overhead athlete. For example, it has been hypothesized that the increased external rotation range offered by the increased retrotorsion reduces the ability of the shoulder musculature to handle the high velocities and forces during throwing, resulting in the development of shoulder pain.17,40 In addition, the increased humeral rotation may perpetuate the “peel back” injury mechanism associated with superior labral anterior posterior lesions that are common in throwing athletes.2,6-9 However, others hypothesize that the retrotorsion is protective of the shoulder injury because the greater retrotorsion allows throwers to obtain more external humeral rotation during throwing while placing less stress on the soft tissue of the anterior shoulder.12,31,33 A study demonstrating decreased humeral retrotorsion in handball players with chronic shoulder pain supports this view.33 Our results failed to demonstrate that amount of humeral retrotorsion on each limb independently plays either a detrimental or a protective role at the shoulder. In addition, none of the humeral retrotorsion variables assessed appeared to have diagnostic capabilities given the low area under the curves from the ROC analyses. Differences in results between Pieper et al33 and the current study may be due to the specificity in the inclusion criteria for the shoulder injury/pain group. Pieper et al33 made a retrotorsion comparison between the handball players with and without chronic shoulder pain, which may be of variety of severity (time loss vs no time loss) and stemming from repetitive throwing or acute contact injuries (eg, dislocation, subluxation, acromioclavicular joint injury). However, the current study made a comparison between the pitchers with and without a history of shoulder injury directly resulting from throwing that resulted in time loss. While we used more specific inclusion criteria for the injury group compared with the study by Pieper et al,33 “shoulder injury” in throwers encompasses a number of pathologies (impingement, superior labral anterior posterior lesions, biceps injury, etc) with varying injury mechanisms. More research regarding the association between retrotorsion and specific shoulder injuries/mechanisms is necessary.
Our work as well as others demonstrated how skeletally mature baseball players and other throwing athletes demonstrate increased humeral retrotorsion.12,28,35 It is suggested that increased humeral retrotorsion is acquired or gained as a result of throwing prior to skeletal maturity. While the torsional forces occurring during throwing most likely affect the amount of humeral retrotorsion present, it may be that throwing slows the natural maturation process where humeral retrotorsion is maintained rather than acquired. Several studies have demonstrated that humeral retrotorsion naturally decreases from birth through skeletal maturity.15,16,45 As such, the torsional forces placed on the humerus during throwing may be maintaining the increased humeral retrotorsion that typically decreases as part of the maturation process in human beings. A true longitudinal study is necessary to best understand how throwing affects the skeletally immature humerus.
While clinicians often utilize assessments of humeral rotation range of motion as part of preseason screening and injury evaluation, the limitation of the range of motion measurement is that it may be affected by a variety of factors, including flexibility training,23 acute stretching,21,32 and sport activity,41 and thus may not be an optimal way to screen and identify athletes with potential injury risk factors. For example, there were no significant differences in any of the range of motion variables assessed despite injury history status. While differences might be expected given that the amount of humeral retrotorsion influences humeral rotation,28 the lack of statistically significant differences in the current study most likely resulted from the fact that the participants were under the care of collegiate sports medicine programs and completed rehabilitation after the injuries occurred. Humeral retrotorsion might be a more stable measure given that it is less susceptible to therapeutic exercise, especially in skeletally mature individuals. In addition, the variability associated with range of motion testing may have resulted in these variables being underpowered in the current study.27-29 A priori power estimates for the current study were based on the humeral retrotorsion variables (the primary variables of interest in the current study) and were calculated from a combination of our previous published work28 as well as humeral retrotorsion pilot data but not for range of motion variables. This current study was to set the groundwork for utilizing humeral retrotorsion measures as means to screen for injury risk. The current study found an association between retrotorsion and elbow injury, suggesting its usefulness. Prospective analyses are necessary to eventually establish injury risk.
There were limitations in the current study that warrant acknowledgment. The current study was a retrospective design, thus allowing only for associations and not true injury risk to be determined. This study also utilized self-reported injury history. However, because all participants were part of division I collegiate baseball teams, the sports medicine staffs were able to confirm injury histories through injury records. Also, measures of retrotorsion were taken after injury history developed. As such, the amount of retrotorsion could have changed since the time of injury. Yet, given the age of the participants (approximately 20 years), the amount of skeletal maturity that is present suggests minimal torsional adaptation occurring since injury. The osseous adaptations that result from throwing appear to occur earlier in the maturation process.10,19,22,25,34 An additional limitation of this study is that it examined only the osseous component, despite the interactive role that osseous adaptation and soft tissue flexibility play in range of motion measures obtained clinically. Because of the potential time length between the development of injury and testing of the participants in the current study, the soft tissue contribution to range of motion could have changed given that these characteristics change acutely21,32 and as a result of training.23 As such, the range of motion data were included for descriptive purposes only. A final limitation of the current study is that the ultrasonographic assessment of humeral retrotorsion has not been validated against computed tomography, the gold standard for humeral torsion assessment. However, the retrotorsion data reported in the current study are consistent with our previous work that established construct validity,28 as well as previously published literature utilizing similar ultrasonographic42-44 and radiologic assessments.12,31,33,35
Conclusions
Collegiate pitchers with a history of elbow injury exhibited a greater limb difference in humeral retrotorsion. Therefore, the greater humeral retrotorsion limb difference present in the participants with elbow injury history suggests that humeral retrotorsion may be associated with the development of elbow injury in pitchers. Humeral retrotorsion on dominant or nondominant limb independently appears to play no detrimental or beneficial role in shoulder injury, given that those retrotorsion characteristics were not different between the participants with and without a history of shoulder injury. Prospective study is needed to determine the cause-and-effect relationship between the bilateral humeral retrotorsion measures and development of elbow injury.
References
- 1.Aguinaldo AL, Chambers H. Correlation of throwing mechanics with elbow valgus load in adult baseball pitchers. Am J Sports Med. 2009;37(10):2043-2048 [DOI] [PubMed] [Google Scholar]
- 2.Andrews JR, Carson WG, Jr, McLeod WD. Glenoid labrum tears related to the long head of the biceps. Am J Sports Med. 1985;13(5):337-341 [DOI] [PubMed] [Google Scholar]
- 3.Anz AW, Bushnell BD, Griffin LP, Noonan TJ, Torry MR, Hawkins RJ. Correlation of torque and elbow injury in professional baseball pitchers. Am J Sports Med. 2010;38(7):1368-1374 [DOI] [PubMed] [Google Scholar]
- 4.Bigliani LU, Codd TP, Connor PM, Levine WN, Littlefield MA, Hershon SJ. Shoulder motion and laxity in the professional baseball player. Am J Sports Med. 1997;25(5):609-613 [DOI] [PubMed] [Google Scholar]
- 5.Brown LP, Niehues SL, Harrah A, Yavorsky P, Hirshman HP. Upper extremity range of motion and isokinetic strength of the internal and external shoulder rotators in major league baseball players. Am J Sports Med. 1988;16(6):577-585 [DOI] [PubMed] [Google Scholar]
- 6.Burkhart SS, Morgan CD. The peel-back mechanism: its role in producing and extending posterior type II SLAP lesions and its effect on SLAP repair rehabilitation. Arthroscopy. 1998;14(6):637-640 [DOI] [PubMed] [Google Scholar]
- 7.Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology. Part I: pathoanatomy and biomechanics. Arthroscopy. 2003;19(4):404-420 [DOI] [PubMed] [Google Scholar]
- 8.Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology. Part II: evaluation and treatment of SLAP lesions in throwers. Arthroscopy. 2003;19(5):531-539 [DOI] [PubMed] [Google Scholar]
- 9.Burkhart SS, Morgan CD, Kibler WB. Shoulder injuries in overhead athletes: the “dead arm” revisited. Clin Sports Med. 2000;19(1):125-158 [DOI] [PubMed] [Google Scholar]
- 10.Carson WG, Jr, Gasser SI. Little Leaguer’s shoulder: a report of 23 cases. Am J Sports Med. 1998;26(4):575-580 [DOI] [PubMed] [Google Scholar]
- 11.Conte SRR, Garrick JG. Disability days in major league baseball. Am J Sports Med. 2001;29(4):431-436 [DOI] [PubMed] [Google Scholar]
- 12.Crockett HC, Gross LB, Wilk KE, et al. Osseous adaptation and range of motion at the glenohumeral joint in professional baseball pitchers. Am J Sports Med. 2002;30(1):20-26 [DOI] [PubMed] [Google Scholar]
- 13.Dick R, Sauers EL, Agel J, et al. Descriptive epidemiology of collegiate men’s baseball injuries: National Collegiate Athletic Association Injury Surveillance System, 1988-1989 through 2003-2004. J Athl Train. 2007;42(2):183-193 [PMC free article] [PubMed] [Google Scholar]
- 14.Dines JS, Frank JB, Akerman M, Yocum LA. Glenohumeral internal rotation deficits in baseball players with ulnar collateral ligament insufficiency. Am J Sports Med. 2009;37(3):566-570 [DOI] [PubMed] [Google Scholar]
- 15.Edelson G. The development of humeral head retroversion. J Shoulder Elbow Surg. 2000;9(4):316-318 [DOI] [PubMed] [Google Scholar]
- 16.Edelson G. Variations in the retroversion of the humeral head. J Shoulder Elbow Surg. 1999;8(2):142-145 [DOI] [PubMed] [Google Scholar]
- 17.Ellenbecker TS, Roetert EP, Bailie DS, Davies GJ, Brown SW. Glenohumeral joint total rotation range of motion in elite tennis players and baseball pitchers. Med Sci Sports Exerc. 2002;34(12):2052-2056 [DOI] [PubMed] [Google Scholar]
- 18.Fleisig GS, Andrews JR, Dillman CJ, Escamilla RF. Kinetics of baseball pitching with implications about injury mechanisms. Am J Sports Med. 1995;23(2):233-239 [DOI] [PubMed] [Google Scholar]
- 19.Kocher MS, Waters PM, Micheli LJ. Upper extremity injuries in the paediatric athlete. Sports Med. 2000;30(2):117-135 [DOI] [PubMed] [Google Scholar]
- 20.Krajnik S, Fogarty KJ, Yard EE, Comstock RD. Shoulder injuries in US high school baseball and softball athletes, 2005-2008. Pediatrics. 2010;125(3):497-501 [DOI] [PubMed] [Google Scholar]
- 21.Laudner KG, Sipes RC, Wilson JT. The acute effects of sleeper stretches on shoulder range of motion. J Athl Train. 2008;43(4):359-363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mair SD, Uhl TL, Robbe RG, Brindle KA. Physeal changes and range-of-motion differences in the dominant shoulders of skeletally immature baseball players. J Shoulder Elbow Surg. 2004;13(5):487-491 [DOI] [PubMed] [Google Scholar]
- 23.McClure P, Balaicuis J, Heiland D, Broersma ME, Thorndike CK, Wood A. A randomized controlled comparison of stretching procedures for posterior shoulder tightness. J Orthop Sports Phys Ther. 2007;37(3):108-114 [DOI] [PubMed] [Google Scholar]
- 24.McFarland EG, Wasik M. Epidemiology of collegiate baseball injuries. Clin J Sport Med. 1998;8(1):10-13 [DOI] [PubMed] [Google Scholar]
- 25.Meister K, Day T, Horodyski M, Kaminski TW, Wasik MP, Tillman S. Rotational motion changes in the glenohumeral joint of the adolescent/Little League baseball player. Am J Sports Med. 2005;33(5):693-698 [DOI] [PubMed] [Google Scholar]
- 26.Morgan CD, Burkhart SS, Palmeri M, Gillespie M. Type II SLAP lesions: three subtypes and their relationships to superior instability and rotator cuff tears. Arthroscopy. 1998;14(6):553-565 [DOI] [PubMed] [Google Scholar]
- 27.Myers JB, Laudner KG, Pasquale MR, Bradley JP, Lephart SM. Glenohumeral range of motion deficits and posterior shoulder tightness in throwers with pathologic internal impingement. Am J Sports Med. 2006;34(3):385-391 [DOI] [PubMed] [Google Scholar]
- 28.Myers JB, Oyama S, Goerger BM, Rucinski TJ, Blackburn JT, Creighton RA. Influence of humeral torsion on interpretation of posterior shoulder tightness measures in overhead athletes. Clin J Sport Med. 2009;19(5):366-371 [DOI] [PubMed] [Google Scholar]
- 29.Myers JB, Oyama S, Wassinger CA, et al. Reliability, precision, accuracy, and validity of posterior shoulder tightness assessment in overhead athletes. Am J Sports Med. 2007;35(11):1922-1930 [DOI] [PubMed] [Google Scholar]
- 30.Obuchowski NA. Receiver operating characteristic curves and their use in radiology. Radiology. 2003;229:3-8 [DOI] [PubMed] [Google Scholar]
- 31.Osbahr DC, Cannon DL, Speer KP. Retroversion of the humerus in the throwing shoulder of college baseball pitchers. Am J Sports Med. 2002;30(3):347-353 [DOI] [PubMed] [Google Scholar]
- 32.Oyama S, Goerger CP, Goerger BM, Lephart SM, Myers JB. Effects of non-assisted posterior shoulder stretches on shoulder range of motion among collegiate baseball pitchers. Ath Train Sport Health Care. 2010;2(4):163-107 [Google Scholar]
- 33.Pieper HG. Humeral torsion in the throwing arm of handball players. Am J Sports Med. 1998;26(2):247-253 [DOI] [PubMed] [Google Scholar]
- 34.Pritchett JW. Growth and predictions of growth in the upper extremity. J Bone Joint Surg Am. 1988;70(4):520-525 [PubMed] [Google Scholar]
- 35.Reagan KM, Meister K, Horodyski MB, Werner DW, Carruthers C, Wilk K. Humeral retroversion and its relationship to glenohumeral rotation in the shoulder of college baseball players. Am J Sports Med. 2002;30(3):354-360 [DOI] [PubMed] [Google Scholar]
- 36.Ruotolo C, Price E, Panchal A. Loss of total arc of motion in collegiate baseball players. J Shoulder Elbow Surg. 2006;15(1):67-71 [DOI] [PubMed] [Google Scholar]
- 37.Sabick MB, Kim YK, Torry MR, Keirns MA, Hawkins RJ. Biomechanics of the shoulder in youth baseball pitchers: implications for the development of proximal humeral epiphysiolysis and humeral retrotorsion. Am J Sports Med. 2005;33(11):1716-1722 [DOI] [PubMed] [Google Scholar]
- 38.Sabick MB, Torry MR, Lawton RL, Hawkins RJ. Valgus torque in youth baseball pitchers: a biomechanical study. J Shoulder Elbow Surg. 2004;13(3):349-355 [DOI] [PubMed] [Google Scholar]
- 39.Safran MR, Borsa PA, Lephart SM, Fu FH, Warner JJ. Shoulder proprioception in baseball pitchers. J Shoulder Elbow Surg. 2001;10(5):438-444 [DOI] [PubMed] [Google Scholar]
- 40.Schwab LM, Blanch P. Humeral torsion and passive shoulder range in elite volleyball players. Phys Ther Sport. 2009;10(2):51-56 [DOI] [PubMed] [Google Scholar]
- 41.Thomas SJ, Swanik KA, Swanik C, Huxel KC. Glenohumeral rotation and scapular position adaptations after a single high school female sports season. J Athl Train. 2009;44(3):230-237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Whiteley R, Ginn K, Nicholson L, Adams R. Indirect ultrasound measurement of humeral torsion in adolescent baseball players and non-athletic adults: Reliability and significance. J Sci Med Sport. 2006;9(4):310-318 [DOI] [PubMed] [Google Scholar]
- 43.Whiteley RJ, Adams RD, Nicholson LL, Ginn KA. Reduced humeral torsion predicts throwing-related injury in adolescent baseballers. J Sci Med Sport. 2010;13(4):392-396 [DOI] [PubMed] [Google Scholar]
- 44.Whiteley RJ, Ginn KA, Nicholson LL, Adams RD. Sports participation and humeral torsion. J Orthop Sports Phys Ther. 2009;39(4):256-263 [DOI] [PubMed] [Google Scholar]
- 45.Yamamoto N, Itoi E, Minagawa H, et al. Why is the humeral retroversion of throwing athletes greater in dominant shoulders than in nondominant shoulders? J Shoulder Elbow Surg. 2006;15(5):571-575 [DOI] [PubMed] [Google Scholar]


