Abstract
Context:
Low back injuries are a common occurrence in athletes and often result in missed competition and practice time. The examination of athletes with low back pain commonly involves diagnostic imaging, which rarely guides the clinician in selecting the appropriate interventions.
Data Acquisition:
All years of PubMed, CINAHL, PEDro, and SPORTDiscus were searched in December 2010. Keywords included treatment based classification and lumbar with the following terms: rehabilitation, treatment, athlete, low back pain, sports, and outcomes.
Results:
A treatment-based classification approach is preferred for the management of the athlete with low back pain. The treatment-based classification approach involves 3 steps. First is to screen the patient for potentially serious conditions that are not appropriate for conservative management. Second is staging the athlete (based on current disability ratings and ability to perform functional activities). Finally, treatment interventions are selected on the basis of the athlete’s signs and symptoms.
Conclusion:
The treatment-based classification scheme provides the clinician with a reliable algorithm for matching an athlete’s symptom presentation to the optimal intervention, potentially reducing participation loss. Managing individuals with low back pain using a treatment-based classification approach significantly reduces disability and pain compared with current clinical practice guideline standards.
Keywords: treatment-based classification, lumbar, low back pain, sports
Low back injuries are commonly experienced by athletes during competition and practice.3,22,62 Men’s collegiate wrestling, American football, and women’s gymnastics have the highest rates of low back injury, with an occurrence of 0.36 to 0.49 injuries per 1000 athlete exposures.3,22,62 The majority of low back injuries occur during competition,3,23,25-27,62 although some sports have a higher risk during practice.1,2,24 Athletes may be at greater risk than nonathletes for having a history of back pain,7 as well as for exhibiting abnormalities on magnetic resonance imaging (MRI).7,46,66
Low back pain (LBP) is commonly diagnosed and managed in accordance with diagnostic imaging findings.20 However, imaging findings in athletic populations may not correlate well with clinical presentation.7,59,77 Lundin and colleagues reported higher incidence of abnormal diagnostic imaging findings in athletes compared with nonathletes.59 In contrast, Baranto et al7 reported similar frequencies of abnormalities on MRI in athletic and nonathletic populations; however, the athletic group reported a significantly higher rate of LBP.
Many abnormalities observed on MRI may occur as the athlete experiences a growth spurt.7,70 MRI abnormalities are uncommon in athletes prior to growth spurt but more common after,50,81,84 suggesting that these findings may be part of a normal aging or growth process.28 Degenerative findings, including disc protrusions or Scheuermann-type abnormalities at early ages, have been associated with recurrent LBP.70,71 Additionally, degenerative disc disease occurs more frequently in adolescent athletes compared with nonathletic controls.77 With the increasing competitive nature of adolescent sports, abnormal diagnostic imaging findings may be present in athletes at a very young age and may be associated with recurrent LBP.7
Diagnostic imaging should not be the only guide for the clinician in making appropriate intervention choices.20 Diagnostic imaging is particularly useful for determining serious conditions, such as spinal fractures, cauda equina syndrome, neoplastic conditions, ankylosing spondylitis, and spinal infection. Red flag signs or symptoms may alert the clinician to the need for further workup (Table 1).31,60
Table 1.
Differential for low back pain.a
| Spinal Fractures | Cauda Equina Syndrome | Neoplastic Conditions | Ankylosing Spondylitis | Spinal Infection |
|---|---|---|---|---|
| Major trauma | Saddle anesthesia | Older athlete with age over 50 years | Getting out of bed at night due to back pain | Recent fever and chills |
| Compression fracture: minor trauma or strenuous lifting in older or potentially osteoporotic athletes; prolonged corticosteroid use | Recent onset of bladder dysfunction, such as urinary retention, increased frequency, or overflow incontinence | Prior history of cancer Unexplained weight loss No relief with bed rest |
Morning stiffness Male sex Age at onset < 35 years |
Recent bacterial infection, intravenous drug abuse, or immune suppression (from steroids, transplant, or HIV) |
| Pars interarticularis stress fracture: persistent back pain in younger athletes involved in repetitive hyperextension activities (ie, gymnastics, wrestling, weight lifting) | Serious or progressive neurologic deficit in the lower extremity | No relief when lying down Relief with exercise and activity |
Adapted from Cleland and Fritz American Physical Therapy Association Monograph 2007.
The majority of low back injuries in athletes are diagnosed as nonspecific: contusions, sprains, or strains.51 In these cases, there is little to guide the clinician in determining the most appropriate intervention. Classification of these nonspecific injuries may assist clinicians in determining the most effective intervention for an individual with LBP.11,21 Several classification systems exist, including the treatment-based classification.21 This system provides a framework for the clinician to screen, stage, and apply an appropriately matched intervention to an individual with LBP.21 The clinician utilizes patient historical information, self-report measures, and physical examination to classify and manage the patient.
Components Of The Treatment-Based Classification System
Step 1: Is the Athlete Appropriate for Conservative Management?
The first stage of the treatment-based classification is to screen for signs and symptoms of nonmusculoskeletal origin and potentially serious pathology: neoplasms, fractures, infection, ankylosing spondylitis, and cauda equina syndrome (Table 1). Because of the vulnerability of the spine during development, the young athlete with extension-related LBP should be evaluated for lumbar stress injuries, including spondylolysis and spondylolisthesis.38,39,42
Medical questionnaires, self-reported disability, and pain scales are utilized to screen for serious pathology.21,33 Key questions include unexplained weight loss, history of metastatic disease, immunosuppressive illness, night pain, and/or changes in bowel or bladder function.48 All positive responses should be reviewed with the athlete. If warranted, a full screen of the organ system is conducted.21
In addition to red flags, the clinician screens psychosocial issues, attitudes, beliefs, or behaviors that may worsen prognosis and prolong pain and disability. A key yellow flag is fear-avoidance beliefs and behaviors, which are assessed using the Fear Avoidance Beliefs Questionnaire (FABQ).43,78 There are 2 subscales to measure athletes’ beliefs regarding the effects of movement on their LBP. The FABQ–Work subscale has a maximum value of 42, with scores greater than 29 indicating potentially high fear-avoidance beliefs that may affect outcome.43 The FABQ–Physical Activity subscale has a maximum value of 24 and may identify fear-avoidance beliefs regarding physical activity measures. The FABQ is most predictive of prolonged disability in work-related back pain but has not been studied in an athletic population. Additional yellow flag findings include depression, anxiety, and pain catastrophizing. Yellow flags may indicate the need to alter the management approach using cognitive behavioral therapy and/or referral to mental health professionals.42
Step 2: Staging the Athlete
Traditionally, staging has been based on duration of symptoms (ie, acute, subacute, or chronic), although the temporal cutoff values are arbitrarily set and offer little guidance for proper intervention selection. The treatment-based classification categorizes athletes on the basis of current functional capacity and disability rating. This staging scheme is a dynamic and fluid system whereby an athlete can enter at any given stage and progress at different rates. Each of the 3 stages includes recommendations for intervention. Two patient self-report measures assist with the staging process: the modified Oswestry Disability Index (ODI) and the Numerical Pain Rating Scale (NPRS) (Tables 2 and 3).21 The ODI is a reliable and responsive 10-question condition-specific self-report measure for individuals with LBP.39 The ODI is scored on a scale from 0% to 100%, with higher scores indicating higher levels of disability. A 6–percentage point change on a 0-100 scale represents clinically meaningful improvement,39 and a reduction in the ODI score by 50% is considered a benchmark of successful intervention.38 Pain intensity is evaluated using the 11-point NPRS: pain at best, at worst, and average pain over the past 24 hours. It is a reliable and valid assessment of LBP severity.16,18 A change of 2 points on the NPRS represents clinically meaningful improvement.16,18
Table 2.
Description and psychometric properties of self-report questionnaires.a
| Outcome Measure | Description | Reliability | MDC and MCID |
|---|---|---|---|
| Modified Oswestry Disability Index | 10-question condition-specific measurement for individuals with low back pain; involves questions relating to pain and functional limitations | ICC = 0.9035 | MDC = 4-10 points79
MCID = 6 percentage points39 |
| Fear Avoidance Beliefs Questionnaire | Designed to assess beliefs regarding movement and its effects on low back pain; 2 subscales: Work and Physical Activity | 0.64-0.8080 | MDC: Work = 12 points; Physical Activity = 9 points43 |
| Numeric Pain Rating Scale | 11-point scale asking the individual to rate pain level based on severity | 0.7621 | MCID = 2 points16,18,43 |
ICC, intraclass correlation coefficient; MDC, minimum detectable change; MCID, minimal clinical important difference.
Table 3.
Three stages of classification.a
| Stage I | Stage II | Stage III | |
|---|---|---|---|
| ADLs | Unable to stand ≥ 15 minutes Unable to sit ≥ 30 minutes Unable to walk ≥ 1/4 mile |
Exceeds all ADL criteria of stage I Difficulty with basic functional ADLs (ie, vacuuming, lifting) |
Able to perform basic functional ADLs Cannot participate fully in sport |
| Typical modified ODI scores | ≥ 20% | ≤ 20% | ≤ 20% |
Athletes in stage I often have elevated modified ODI (≥ 20%) and NPRS scores coupled with a limited ability to perform basic activities of daily living, such as sitting, standing, and walking.21 The athlete is matched to 1 (or more) of 4 interventions depending on history and physical examination: manipulation, specific exercise, stabilization, or traction (Table 4). A 33% drop in modified ODI score or a score of ≤ 20% progresses the athlete to stage II or III.11
Table 4.
Stage I subgroup variables.a
| Manipulation | No symptoms distal to the knee Symptom duration ≤ 16 days Fear Avoidance Beliefs Questionnaire–Work ≤ 19 Lumbar hypomobility Hip internal rotation ≥ 35° |
| Specific exercise | |
| Extension | Symptoms distal to the buttock Directional preference for extension Symptoms peripheralize with flexion Centralization with extension |
| Flexion | Age ≥ 50 years Directional preference for flexion Evidence of spinal stenosis on imaging |
| Lateral shift | Visible frontal plane deviation Directional preference for lateral translational movements |
| Stabilization | Age ≤ 40 years Straight leg raise ≥ 91° Aberrant motions + prone instability test |
| Traction | Presence of leg symptoms Signs of nerve root compression Peripheralization with extension + crossed straight leg raise |
Adapted from Fritz et al.36
Stage II athletes have modified ODI scores ≤ 20% with little difficulty during basic activities of daily living. The athlete presents with difficulty performing more demanding daily activities and exercise, such as jogging.11,21 Interventions include pain modulation, flexibility, strength, posture, body mechanics, and aerobic conditioning.21
Athletes in stage III may have modified ODI scores ≤ 20% with no difficulty with daily activities but are unable to resume full sports participation.11,41 The athlete may be able to practice or compete, but one’s full capacity is still limited. Athletes with recurrent LBP complaints may be in stage III.41 Interventions for stage III include sports-specific training, spinal stabilization, an exercise program designed to limit the recurrence of LBP, and functional training. For the athletic population, this may be the most important classification because it returns the athlete to sports participation.41
Step 3: Managing the Athlete
Stage I Athlete
Traditionally, an athlete in stage I was in the acute phase of the injury (appendix).
Thrust manipulation
Despite widespread use of the thrust manipulation, clinical practice guidelines have limited recommendations regarding this modality because of the conflicting results.53 There are 2 main reasons for this diversity: Spinal manipulative therapy has included nonthrust manipulations, thrust manipulations, and soft tissue techniques, which does not allow for adequate comparison, and most studies utilized heterogeneous populations to examine the effectiveness of manipulative therapy.44,45 LBP is a heterogeneous condition,52 highlighting the need for the identification of subgroups based on history and physical to improve outcomes.11,36
A clinical prediction rule can be used to identify those who may experience rapid and dramatic improvement from a lumbopelvic thrust manipulation and an active range of motion exercise.32 Seventy-one patients received a thrust manipulation at the lumbar region. A successful outcome was a 50% or greater reduction in ODI score; 45% were successful. A regression analysis yielded 5 predictor variables: symptoms ≤ 16 days, no symptoms distal to the knee, FABQ–Work subscale ≤ 19, at least 1 hip with 35° of internal rotation, and hypomobility of the lumbar spine.
If an individual demonstrated 4 or more predictor variables, the likelihood of reducing his or her ODI scores by at least 50% within 2 treatment sessions was 95%. These results were validated in a multicenter randomized clinical trial of 131 patients randomized into a thrust manipulation + exercise group or exercise-alone group.15 Those who were positive on the rule and received thrust manipulation and exercise had significantly better outcomes. A subsequent data analysis pooling the results of these 2 studies resulted in a 2-factor rule that simplified clinical decision making.35 Individuals with no symptoms below the knee and a symptom onset of ≤ 16 days had a 91% probability of experiencing statistically significant and clinically meaningful reductions in disability and pain.35
The rapid improvement in disability following thrust manipulation may minimize an athlete’s loss of practice time and competition. Studies suggest superior outcomes when an individual meets these criteria and receives thrust manipulation, whereas not providing thrust manipulation may delay recovery.11,14,37
Utilizing a nonthrust manipulation technique yielded inferior results compared with the thrust techniques, indicating the velocity is important.19 Clinicians frequently combine manipulation with exercise, advice, and additional manual therapy techniques.8,15
Direction-specific exercise
Patients respond most favorably to exercises that match their directional preference (DP), or movement that decreases pain, with a primary goal of centralization of symptoms.12 Centralization occurs when symptoms diminish from distal to proximal in response to movements or postures.4 Twenty-nine to seventy percent of individuals with acute LBP achieve centralization with specific exercises,4,86 indicating a favorable prognosis.4,85,86
A posture or movement often reduces pain, improves range of motion, and centralizes symptoms in a distal-to-proximal fashion. Conversely, these positions or movements may worsen or peripheralize symptoms proximal to distal.12 The patient’s history may identify the DP. Symptoms may worsen with sitting and bending activities and improve with standing and walking, suggesting an extension DP. In a recent study, eighty-four percent of individuals matched to the appropriate direction of exercise (extension, flexion, lateral shift) had significant reductions in pain and disability within the first 2 weeks of treatment.58
The most common DP is extension, which often indicates lumbar disc pathology.29 In a systematic review, 40% to 56% of individuals with acute LBP and radicular symptoms achieved centralization with extension exercises.4 For patients with an extension DP and stiffness or pain, manual therapy techniques are utilized.12 The most common manual therapy procedure for this purpose is the nonthrust posterior-to-anterior manipulation with the patient prone. Patients temporarily avoid flexion activities and postures until their acute symptoms resolve.
A lateral shift is an observable deviation in frontal plane posture after lumbar disc herniation.55 Up to 25% of individuals with LBP present with a lateral shift,64 which has a poor prognosis.69 With a lateral shift, active movements in the frontal plane are assessed first to find a DP and movement that centralize the patient’s symptoms. For individuals who are unable to move in the frontal plane, the clinician may provide passive manual assistance.55 Those who centralize frontal plane or with side-glide movements are provided an exercise program in this direction.55 For some, frontal plane movement of the pelvis followed by extension leads to centralization; patients may centralize if they shift their pelvis to the left or right prior to performing a prone extension exercise.
The least common DP is flexion. It is commonly found in older adults with lumbar spinal stenosis.86 Football lineman, oarsmen, dancers, and gymnasts have higher rates of spondylolisthesis and may benefit from flexion exercises.57,74,80
Stabilization
Core stability training enhances sports performance in athletes; however, there is no consensus on the optimal method.6,61,72 For athletes, a phasic approach can be utilized combining specific muscle training and progressing to global strengthening before implementing sports-specific training.
Fifty-four consecutive patients with LBP without signs of nerve root compression or pregnancy-related LBP underwent an extensive examination and participated in an 8-week lumbar stabilization exercise program that retrained the transversus abdominous, multifidi, erector spinae, quadratus lumborum, and obliques.49 They had 2 supervised sessions per week and completed exercises at home daily. Progress was at the discretion of the clinician. A third of patients reported 50% or greater reduction on the modified ODI, with a mean reduction of 75%. Four positive predictor variables were identified: age < 40 years, average straight leg raise ≥ 91°, aberrant movements, and positive prone instability test.
Aberrant movements indicate lumbar spine instability, including “instability catch,”65 thigh climbing (or Gower sign), painful arc of motion, or reversal of lumbopelvic rhythm.21 The prone instability test is performed with the torso supported on the table with the feet resting on the floor.63 The examiner applies posterior to anterior force over each lumbar vertebrae. If pain occurs, the patient lifts his or her feet off the floor, and the force is reapplied to that segment. A decrease in pain is considered a positive test result.63
Traction
The use of mechanical traction is not endorsed by any clinical practice guidelines5,54,76 but is widely used.47,67,68 Some research suggests that traction is indicated for a small subgroup of patients, while randomized clinical trials have not shown benefits.9,10,17,40,47,73
Four predictor variables may assist the clinician in determining who may benefit from mechanical traction: leg symptoms, nerve root compression, peripheralization with extension, and positive crossed straight leg raise.
Peripheralization of symptoms occurs with pain, or numbness moves distally when performing extension of the lumbar spine. Those with peripheralization have a poorer prognosis4,29 and an increased likelihood of surgery.75
The crossed straight leg raise test is performed with the athlete supine, and the examiner passively performs a straight leg raise of the contralateral lower extremity.82 The test result is positive if there are contralateral lower extremity symptoms. The crossed straight leg raise has high specificity (0.85-0.94) and low sensitivity (0.22-0.35).82
Stage II and III Athletes
The most appropriate management of the athlete in stage II or III is not known, but impairments in flexibility, strength, endurance, and neuromuscular control should be targeted with exercise and manual therapy.30 Deficits around the hips and thoracic spine may also contribute to LBP.13,83,87
A comprehensive exercise program (HEP) that targets musculoskeletal impairments and incorporates sport-specific exercises is preferred and should reduce the recurrence of LBP.21,41 Education regarding adherence, proper progression, and avoidance of overtraining is essential. With acute LBP, advice and education appear beneficial, but there is conflicting evidence on the recurrence.56
Conclusion
LBP is a common condition in athletes, and appropriate management is critical to limiting missed game and practice participation. The treatment-based classification approach provides an evidence-based framework detailing the appropriate conservative management of individuals with LBP. The 3 steps involved in the treatment-based classification approach include (1) screening for emergent conditions not suitable for conservative management, (2) staging the athlete based on disability and basic performance of activities of daily living, and (3) providing matched interventions depending on the stage.
The treatment-based classification approach is a reliable, valid, and cost-effective algorithm that yields successful outcomes and rapid return to function.34,37
Appendix
Appendix.
Criteria for appropriate subgrouping of athletes in stage I.
| Manipulation | No symptoms distal to the knee (Figure 1) Symptom duration ≤ 16 days Fear Avoidance Beliefs Questionnaire–Work subscale ≤ 19 Lumbar hypomobility (Figure 2): The examiner provides a posterior-anterior force on each spinous process, assessing for relative differences in mobility and symptom reproduction Hip internal rotation ≥ 35°, at least 1 side (Figure 3): The examiner assesses prone hip internal rotation using a bubble inclinometer placed on the distal portion of the fibula |
| Specific exercise (extension/lateral shift) | Symptoms distal to the buttock (Figure 4) Directional preference for extension Symptoms peripheralize with flexion Centralization of symptoms with extension (Figure 5) Visible frontal plane deviation (Figure 6) Directional preference for lateral translational movements (Figure 7) |
| Stabilization | Age ≤ 40 years Straight leg raise ≥ 91° (Figure 8): While maintaining the knee in an extended position, the examiner passively flexes to the hip Aberrant motions: thigh climbing, reversal of lumbopelvic rhythm, painful arc, or “instability catch” Positive prone instability test (Figure 9) |
| Traction | Presence of leg symptoms (Figure 10) Signs of nerve root compression: myotomal, dermatomal, and/or deep tendon reflex abnormalities Peripheralization with extension (Figure 11) Positive crossed straight leg raise (Figure 12): While maintaining the contralateral knee in extension, the examiner passively flexes the contralateral hip |
Figure 1.
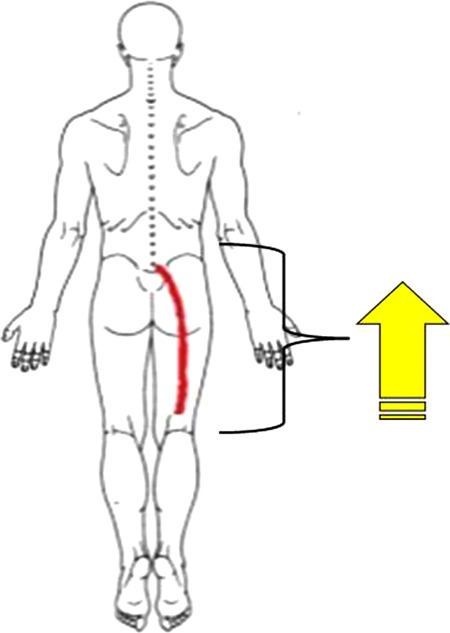
Body diagram indicating symptoms proximal to the knee.32
Figure 2.

Posterior-anterior lumbar segmental mobility assessment. The arrow indicates the direction of force applied by the examiner. 32
Figure 3.

Prone hip internal rotation range of motion measurement using a bubble inclinometer. Arrow indicates direction that the distal lower extremity courses to assess left hip internal rotation range of motion. 32
Figure 4.
Body diagram indicating symptoms distal to the buttock.12
Figure 5.

Lumbar extension in prone position. Arrow indicates the centralization of leg symptoms.12
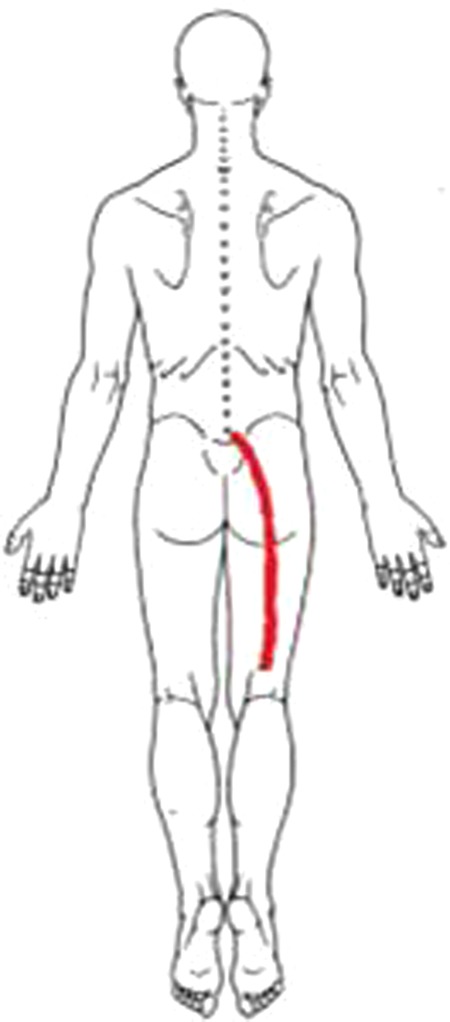
Figure 6.

Visible frontal plane deviation with the line indicating symptoms in the contralateral lower extremity.55
Figure 7.

Visible frontal plane deviation with the arrow indicating symptoms centralizing to lumbar spine region.55
Figure 8.

Ipsilateral straight leg raise.49
Figure 9.
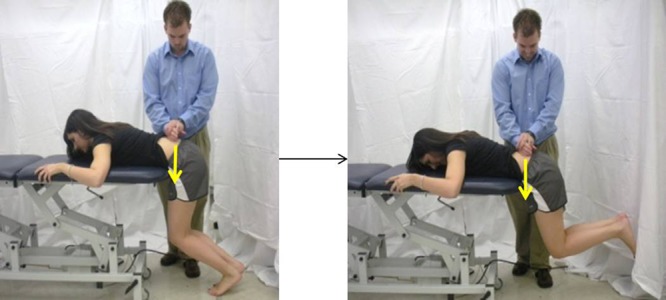
Prone instability test. The left image indicates the starting position with feet on the floor. The right image indicates the end position of the test with the feet lifted off the floor. The white arrows indicate the posterior-anterior force applied by the examiner.49
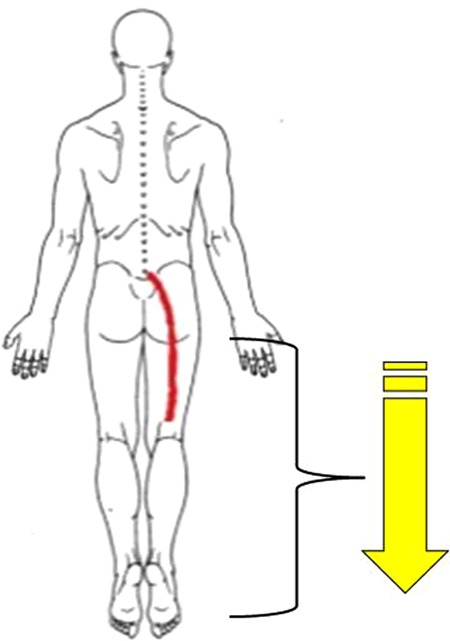
Figure 10.
Body diagram indicating the presence of leg symptoms.76
Figure 11.

Prone lumbar extension with the arrow indicating the peripheralization of symptoms.76
Figure 12.

Crossed straight leg raise. The contralateral lower extremity is flexed by the examiner assessing for the peripheralization of symptoms into the ipsilateral lower extremity.76,82
References
- 1. Agel J, Olson DE, Dick R, et al. Descriptive epidemiology of collegiate women’s basketball injuries: National Collegiate Athletic Association Injury Surveillance System, 1988-1989 through 2003-2004. J Athl Train. 2007;42(2):202-210 [PMC free article] [PubMed] [Google Scholar]
- 2. Agel J, Palmieri-Smith RM, Dick R, Wojtys EM, Marshall SW. Descriptive epidemiology of collegiate women’s volleyball injuries: National Collegiate Athletic Association Injury Surveillance System, 1988-1989 through 2003-2004. J Athl Train. 2007;42(2):295-302 [PMC free article] [PubMed] [Google Scholar]
- 3. Agel J, Ransone J, Dick R, Oppliger R, Marshall SW. Descriptive epidemiology of collegiate men’s wrestling injuries: National Collegiate Athletic Association Injury Surveillance System, 1988-1989 through 2003-2004. J Athl Train. 2007;42(2):303-310 [PMC free article] [PubMed] [Google Scholar]
- 4. Aina A, May S, Clare H. The centralization phenomenon of spinal symptoms: a systematic review. Man Ther. 2004;9(3):134-143 [DOI] [PubMed] [Google Scholar]
- 5. Airaksinen O, Brox JI, Cedraschi C, et al. Chapter 4: European guidelines for the management of chronic nonspecific low back pain. Eur Spine J. 2006;15(suppl 2):S192-S300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Asplund C, Ross M. Core stability and bicycling. Curr Sports Med Rep. 2010;9(3):155-160 [DOI] [PubMed] [Google Scholar]
- 7. Baranto A, Hellström M, Cederlund C, Nyman R, Swärd L. Back pain and MRI changes in the thoraco-lumbar spine of top athletes in four different sports: a 15-year follow-up study. Knee Surg Sports Traumatol Arthrosc. 2009;17(9):1125-1134 [DOI] [PubMed] [Google Scholar]
- 8. Beattie PF, Arnot CF, Donley JW, Noda H, Bailey L. The immediate reduction in low back pain intensity following lumbar joint mobilization and prone press-ups is associated with increased diffusion of water in the L5-S1 intervertebral disc. J Orthop Sports Phys Ther. 2010;40(5):256-264 [DOI] [PubMed] [Google Scholar]
- 9. Beurskens AJ, de Vet HC, Köke AJ, et al. Efficacy of traction for nonspecific low back pain: 12-week and 6-month results of a randomized clinical trial. Spine. 1997;22(23):2756-2762 [DOI] [PubMed] [Google Scholar]
- 10. Beurskens AJ, de Vet HC, Köke AJ, et al. Efficacy of traction for non-specific low back pain: a randomised clinical trial. Lancet. 1995;346(8990):1596-1600 [DOI] [PubMed] [Google Scholar]
- 11. Brennan GP, Fritz JM, Hunter SJ, et al. Identifying subgroups of patients with acute/subacute “nonspecific” low back pain: results of a randomized clinical trial. Spine. 2006;31(6):623-631 [DOI] [PubMed] [Google Scholar]
- 12. Browder DA, Childs JD, Cleland JA, Fritz JM. Effectiveness of an extension-oriented treatment approach in a subgroup of subjects with low back pain: a randomized clinical trial. Phys Ther. 2007;87(12):1608-1618 [DOI] [PubMed] [Google Scholar]
- 13. Burns SA, Mintken PE, Austin GP. Clinical decision making in a patient with secondary hip-spine syndrome [published online ahead of print August 26, 2010]. Physiother Theory Pract. [DOI] [PubMed]
- 14. Childs JD, Flynn TW, Fritz JM. A perspective for considering the risks and benefits of spinal manipulation in patients with low back pain. Man Ther. 2006;11(4):316-320 [DOI] [PubMed] [Google Scholar]
- 15. Childs JD, Fritz JM, Flynn TW, et al. A clinical prediction rule to identify patients with low back pain most likely to benefit from spinal manipulation: a validation study. Ann Intern Med. 2004;141(12):920-928 [DOI] [PubMed] [Google Scholar]
- 16. Childs JD, Piva SR, Fritz JM. Responsiveness of the numeric pain rating scale in patients with low back pain. Spine. 2005;30(11):1331-1334 [DOI] [PubMed] [Google Scholar]
- 17. Clarke JA, van Tulder MW, Blomberg SEI, et al. Traction for low-back pain with or without sciatica. Cochrane Database Syst Rev. 2007;(2):CD003010 [DOI] [PubMed] [Google Scholar]
- 18. Cleland JA, Childs JD, Whitman JM. Psychometric properties of the Neck Disability Index and Numeric Pain Rating Scale in patients with mechanical neck pain. Arch Phys Med Rehabil. 2008;89(1):69-74 [DOI] [PubMed] [Google Scholar]
- 19. Cleland JA, Fritz JM, Childs JD, Kulig K. Comparison of the effectiveness of three manual physical therapy techniques in a subgroup of patients with low back pain who satisfy a clinical prediction rule: study protocol of a randomized clinical trial [NCT00257998]. BMC Musculoskelet Disord. 2006;7:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Curtis C, d’Hemecourt P. Diagnosis and management of back pain in adolescents. Adolesc Med State Art Rev. 2007;18(1):140-164 [PubMed] [Google Scholar]
- 21. Delitto A, Erhard RE, Bowling RW. A treatment-based classification approach to low back syndrome: identifying and staging patients for conservative treatment. Phys Ther. 1995;75(6):470-485 [DOI] [PubMed] [Google Scholar]
- 22. Dick R, Ferrara MS, Agel J, et al. Descriptive epidemiology of collegiate men’s football injuries: National Collegiate Athletic Association Injury Surveillance System, 1988-1989 through 2003-2004. J Athl Train. 2007;42(2):221-233 [PMC free article] [PubMed] [Google Scholar]
- 23. Dick R, Hertel J, Agel J, Grossman J, Marshall SW. Descriptive epidemiology of collegiate men’s basketball injuries: National Collegiate Athletic Association Injury Surveillance System, 1988-1989 through 2003-2004. J Athl Train. 2007;42(2):194-201 [PMC free article] [PubMed] [Google Scholar]
- 24. Dick R, Hootman JM, Agel J, et al. Descriptive epidemiology of collegiate women’s field hockey injuries: National Collegiate Athletic Association Injury Surveillance System, 1988-1989 through 2002-2003. J Athl Train. 2007;42(2):211-220 [PMC free article] [PubMed] [Google Scholar]
- 25. Dick R, Lincoln AE, Agel J, et al. Descriptive epidemiology of collegiate women’s lacrosse injuries: National Collegiate Athletic Association Injury Surveillance System, 1988-1989 through 2003-2004. J Athl Train. 2007;42(2):262-269 [PMC free article] [PubMed] [Google Scholar]
- 26. Dick R, Putukian M, Agel J, Evans TA, Marshall SW. Descriptive epidemiology of collegiate women’s soccer injuries: National Collegiate Athletic Association Injury Surveillance System, 1988-1989 through 2002-2003. J Athl Train. 2007;42(2):278-285 [PMC free article] [PubMed] [Google Scholar]
- 27. Dick R, Romani WA, Agel J, Case JG, Marshall SW. Descriptive epidemiology of collegiate men’s lacrosse injuries: National Collegiate Athletic Association Injury Surveillance System, 1988-1989 through 2003-2004. J Athl Train. 2007;42(2):255-261 [PMC free article] [PubMed] [Google Scholar]
- 28. Difiori JP. Evaluation of overuse injuries in children and adolescents. Curr Sports Med Rep. 2010;9(6):372-378 [DOI] [PubMed] [Google Scholar]
- 29. Donelson R, Aprill C, Medcalf R, Grant W. A prospective study of centralization of lumbar and referred pain: a predictor of symptomatic discs and anular competence. Spine. 1997;22(10):1115-1122 [DOI] [PubMed] [Google Scholar]
- 30. Evans K, Cady K, Dobson A, Towers P. Results of a musculoskeletal preparticipation screening programme in BUCS Super 8 Rugby League players. Br J Sports Med. 2010;44(14):i5 [Google Scholar]
- 31. Ferguson F, Holdsworth L, Rafferty D. Low back pain and physiotherapy use of red flags: the evidence from Scotland. Physiotherapy. 2010;96(4):282-288 [DOI] [PubMed] [Google Scholar]
- 32. Flynn T, Fritz J, Whitman J, et al. A clinical prediction rule for classifying patients with low back pain who demonstrate short-term improvement with spinal manipulation. Spine. 2002;27(24):2835-2843 [DOI] [PubMed] [Google Scholar]
- 33. Fritz JM. Use of a classification approach to the treatment of 3 patients with low back syndrome. Phys Ther. 1998;78(7):766-777 [DOI] [PubMed] [Google Scholar]
- 34. Fritz JM, Brennan GP, Clifford SN, Hunter SJ, Thackeray A. An examination of the reliability of a classification algorithm for subgrouping patients with low back pain. Spine. 2006;31(1):77-82 [DOI] [PubMed] [Google Scholar]
- 35. Fritz JM, Childs JD, Flynn TW. Pragmatic application of a clinical prediction rule in primary care to identify patients with low back pain with a good prognosis following a brief spinal manipulation intervention. BMC Fam Pract. 2005;6(1):29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Fritz JM, Cleland JA, Childs JD. Subgrouping patients with low back pain: evolution of a classification approach to physical therapy. J Orthop Sports Phys Ther. 2007;37(6):290-302 [DOI] [PubMed] [Google Scholar]
- 37. Fritz JM, Delitto A, Erhard RE. Comparison of classification-based physical therapy with therapy based on clinical practice guidelines for patients with acute low back pain: a randomized clinical trial. Spine. 2003;28(13):1363-1371 [DOI] [PubMed] [Google Scholar]
- 38. Fritz JM, Hebert J, Koppenhaver S, Parent E. Beyond minimally important change: defining a successful outcome of physical therapy for patients with low back pain. Spine. 2009;34(25):2803-2809 [DOI] [PubMed] [Google Scholar]
- 39. Fritz JM, Irrgang JJ. A comparison of a modified Oswestry Low Back Pain Disability Questionnaire and the Quebec Back Pain Disability Scale. Phys Ther. 2001;81(2):776-788 [DOI] [PubMed] [Google Scholar]
- 40. Fritz JM, Lindsay W, Matheson JW, et al. Is there a subgroup of patients with low back pain likely to benefit from mechanical traction? Results of a randomized clinical trial and subgrouping analysis. Spine. 2007;32(26): E793-E800 [DOI] [PubMed] [Google Scholar]
- 41. George SZ, Delitto A. Management of the athlete with low back pain. Clin Sports Med. 2002;21(1):105-120 [DOI] [PubMed] [Google Scholar]
- 42. George SZ, Fritz JM, Childs JD. Investigation of elevated fear-avoidance beliefs for patients with low back pain: a secondary analysis involving patients enrolled in physical therapy clinical trials. J Orthop Sports Phys Ther. 2008;38(2):50-58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Grotle M, Brox JI, Vøllestad NK. Reliability, validity and responsiveness of the fear-avoidance beliefs questionnaire: methodological aspects of the Norwegian version. J Rehabil Med. 2006;38(6):346-353 [DOI] [PubMed] [Google Scholar]
- 44. Hancock MJ, Maher CG, Latimer J. Spinal manipulative therapy for acute low back pain: a clinical perspective. J Man Manip Ther. 2008;16(4):198-203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Hancock MJ, Maher CG, Latimer J, et al. Assessment of diclofenac or spinal manipulative therapy, or both, in addition to recommended first-line treatment for acute low back pain: a randomised controlled trial. Lancet. 2007;370(9599):1638-1643 [DOI] [PubMed] [Google Scholar]
- 46. Hangai M, Kaneoka K, Hinotsu S, et al. Lumbar intervertebral disk degeneration in athletes. Am J Sports Med. 2009;37(1):149-155 [DOI] [PubMed] [Google Scholar]
- 47. Harte AA, Gracey JH, Baxter GD. Current use of lumbar traction in the management of low back pain: results of a survey of physiotherapists in the United Kingdom. Arch Phys Med Rehabil. 2005;86(6):1164-1169 [DOI] [PubMed] [Google Scholar]
- 48. Henschke N, Maher CG, Refshauge KM. A systematic review identifies five “red flags” to screen for vertebral fracture in patients with low back pain. J Clin Epidemiol. 2008;61(2):110-118 [DOI] [PubMed] [Google Scholar]
- 49. Hicks GE, Fritz JM, Delitto A, McGill SM. Preliminary development of a clinical prediction rule for determining which patients with low back pain will respond to a stabilization exercise program. Arch Phys Med Rehabil. 2005;86(9):1753-1762 [DOI] [PubMed] [Google Scholar]
- 50. Jackson DW, Wiltse LL, Cirincoine RJ. Spondylolysis in the female gymnast. Clin Orthop Relat Res. 1976;(117):68-73 [PubMed] [Google Scholar]
- 51. Junge A, Langevoort G, Pipe A, et al. Injuries in team sport tournaments during the 2004 Olympic Games. Am J Sports Med. 2006;34(4):565-576 [DOI] [PubMed] [Google Scholar]
- 52. Kent P, Keating J. Do primary-care clinicians think that nonspecific low back pain is one condition? Spine. 2004;29(9):1022-1031 [DOI] [PubMed] [Google Scholar]
- 53. Koes BW, van Tulder M, Lin CC, et al. An updated overview of clinical guidelines for the management of non-specific low back pain in primary care. Eur Spine J. 2010;19(12):2075-2094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Koes BW, van Tulder MW, Ostelo R, Kim Burton A, Waddell G. Clinical guidelines for the management of low back pain in primary care: an international comparison. Spine. 2001;26(22):2504-2513 [DOI] [PubMed] [Google Scholar]
- 55. Laslett M. Manual correction of an acute lumbar lateral shift: maintenance of correction and rehabilitation: a case report with video. J Man Manip Ther. 2009;17(2):78-85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Liddle SD, Gracey JH, Baxter GD. Advice for the management of low back pain: a systematic review of randomised controlled trials. Man Ther. 2007;12(4):310-327 [DOI] [PubMed] [Google Scholar]
- 57. Long A, Donelson R, Fung T. Does it matter which exercise? A randomized control trial of exercise for low back pain. Spine. 2004;29(23):2593-2602 [DOI] [PubMed] [Google Scholar]
- 58. Long A, May S, Fung T. Specific directional exercises for patients with low back pain: a case series. Physiother Can. 2008;60(4):307-317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Lundin O, Hellström M, Nilsson I, Swärd L. Back pain and radiological changes in the thoraco-lumbar spine of athletes: a long-term follow-up. Scand J Med Sci Sports. 2001;11(2):103-109 [DOI] [PubMed] [Google Scholar]
- 60. Lurie JD. What diagnostic tests are useful for low back pain? Best Pract Res Clin Rheumatol. 2005;19(4):557-575 [DOI] [PubMed] [Google Scholar]
- 61. Lust KR, Sandrey MA, Bulger SM, Wilder N. The effects of 6-week training programs on throwing accuracy, proprioception, and core endurance in baseball. J Sport Rehabil. 2009;18(3):407-426 [DOI] [PubMed] [Google Scholar]
- 62. Marshall SW, Covassin T, Dick R, Nassar LG, Agel J. Descriptive epidemiology of collegiate women’s gymnastics injuries: National Collegiate Athletic Association Injury Surveillance System, 1988-1989 through 2003-2004. J Athl Train. 2007;42(2):234-240 [PMC free article] [PubMed] [Google Scholar]
- 63. McGill SM, Childs A, Liebenson C. Endurance times for low back stabilization exercises: clinical targets for testing and training from a normal database. Arch Phys Med Rehabil. 1999;80(8):941-944 [DOI] [PubMed] [Google Scholar]
- 64. McKenzie RA. Manual correction of sciatic scoliosis. N Z Med J. 1972;76(484):194-199 [PubMed] [Google Scholar]
- 65. Nachemson A. Lumbar spine instability: a critical update and symposium summary. Spine. 1985;10(3):290-291 [PubMed] [Google Scholar]
- 66. Ong A, Anderson J, Roche J. A pilot study of the prevalence of lumbar disc degeneration in elite athletes with lower back pain at the Sydney 2000 Olympic Games. Br J Sports Med. 2003;37(3):263-266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Pensri P, Foster NE, Srisuk S, Baxter GD, McDonough SM. Physiotherapy management of low back pain in Thailand: a study of practice. Physiother Res Int. 2005;10(4):201-212 [DOI] [PubMed] [Google Scholar]
- 68. Poitras S, Blais R, Swaine B, Rossignol M. Management of work-related low back pain: a population-based survey of physical therapists. Phys Ther. 2005;85(11):1168-1181 [PubMed] [Google Scholar]
- 69. Porter RW, Miller CG. Back pain and trunk list. Spine. 1986;11(6):596-600 [DOI] [PubMed] [Google Scholar]
- 70. Salminen JJ, Erkintalo M, Laine M, Pentti J. Low back pain in the young: a prospective three-year follow-up study of subjects with and without low back pain. Spine. 1995;20(19):2101-2107 [DOI] [PubMed] [Google Scholar]
- 71. Salminen JJ, Erkintalo MO, Pentti J, Oksanen A, Kormano MJ. Recurrent low back pain and early disc degeneration in the young. Spine. 1999;24(13):1316-1321 [DOI] [PubMed] [Google Scholar]
- 72. Sato K, Mokha M. Does core strength training influence running kinetics, lower-extremity stability, and 5000-M performance in runners? J Strength Cond Res. 2009;23(1):133-140 [DOI] [PubMed] [Google Scholar]
- 73. Schimmel JJP, de Kleuver M, Horsting PP, et al. No effect of traction in patients with low back pain: a single centre, single blind, randomized controlled trial of Intervertebral Differential Dynamics Therapy. Eur Spine J. 2009;18(12):1843-1850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Sinaki M, Lutness MP, Ilstrup DM, Chu CP, Gramse RR. Lumbar spondylolisthesis: retrospective comparison and three-year follow-up of two conservative treatment programs. Arch Phys Med Rehabil. 1989;70(8):594-598 [PubMed] [Google Scholar]
- 75. Skytte L, May S, Petersen P. Centralization: its prognostic value in patients with referred symptoms and sciatica. Spine. 2005;30(11):E293-E299 [DOI] [PubMed] [Google Scholar]
- 76. Staal JB, Hlobil H, van Tulder MW, et al. Occupational health guidelines for the management of low back pain: an international comparison. Occup Environ Med. 2003;60(9):618-626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Swärd L, Hellstrom M, Jacobsson B, Pëterson L. Back pain and radiologic changes in the thoraco-lumbar spine of athletes. Spine. 1990;15(2):124-129 [DOI] [PubMed] [Google Scholar]
- 78. Swinkels-Meewisse EJCM, Swinkels RAHM, Verbeek ALM, Vlaeyen JWS, Oostendorp RAB. Psychometric properties of the Tampa Scale for kinesiophobia and the fear-avoidance beliefs questionnaire in acute low back pain. Man Ther. 2003;8(1):29-36 [DOI] [PubMed] [Google Scholar]
- 79. Tacci JA, Webster BS, Hashemi L, Christiani DC. Clinical practices in the management of new-onset, uncomplicated, low back workers’ compensation disability claims. J Occup Environ Med. 1999;41(5):397-404 [DOI] [PubMed] [Google Scholar]
- 80. Tallarico RA, Madom IA, Palumbo MA. Spondylolysis and spondylolisthesis in the athlete. Sports Med Arthrosc. 2008;16(1):32-38 [DOI] [PubMed] [Google Scholar]
- 81. Tertti M, Paajanen H, Kujala UM, et al. Disc degeneration in young gymnasts: a magnetic resonance imaging study. Am J Sports Med. 1990;18(2):206-208 [DOI] [PubMed] [Google Scholar]
- 82. van der Windt DA, Simons E, Riphagen, et al. Physical examination for lumbar radiculopathy due to disc herniation in patients with low-back pain. Cochrane Database Syst Rev. 2010;(2):CD007431 [DOI] [PubMed] [Google Scholar]
- 83. Wainner RS, Whitman JM, Cleland JA, Flynn TW. Regional interdependence: a musculoskeletal examination model whose time has come. J Orthop Sports Phys Ther. 2007;37(11):658-660 [DOI] [PubMed] [Google Scholar]
- 84. Waris E, Eskelin M, Hermunen H, Kiviluoto O, Paajanen H. Disc degeneration in low back pain: a 17-year follow-up study using magnetic resonance imaging. Spine. 2007;32(6):681-684 [DOI] [PubMed] [Google Scholar]
- 85. Werneke M, Hart DL. Centralization phenomenon as a prognostic factor for chronic low back pain and disability. Spine. 2001;26(7):758-764 [DOI] [PubMed] [Google Scholar]
- 86. Werneke MW, Hart DL, Resnik L, Stratford PW, Reyes A. Centralization: prevalence and effect on treatment outcomes using a standardized operational definition and measurement method. J Orthop Sports Phys Ther. 2008;38(3):116-125 [DOI] [PubMed] [Google Scholar]
- 87. Whitman JM, Flynn TW, Childs JD, et al. A comparison between two physical therapy treatment programs for patients with lumbar spinal stenosis: a randomized clinical trial. Spine. 2006;31(22):2541-2549 [DOI] [PubMed] [Google Scholar]


