Abstract
Context:
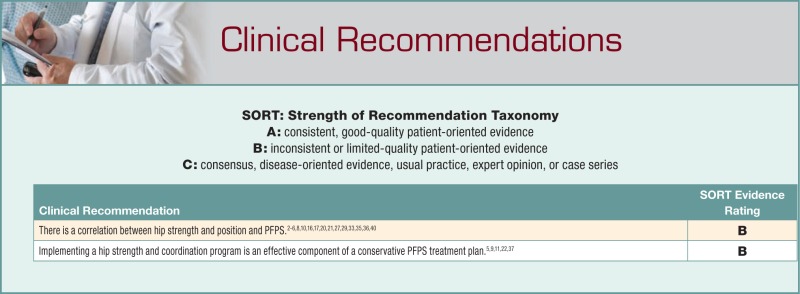
Patellofemoral pain syndrome (PFPS) is one of the most common conditions limiting athletes. There is a growing body of evidence suggesting that dysfunction at the hip may be a contributing factor in PFPS.
Data Sources:
MEDLINE (1950–September 2010), CINAHL (1982–September 2010), and SPORTDiscus (1830–September 2010) were searched to identify relevant research to this report.
Study Selection:
Studies were included assessing hip strength, lower extremity kinematics, or both in relation to PFPS were included.
Data Extraction:
Studies included randomized controlled trials, quasi-experimental designs, prospective epidemiology, case-control epidemiology, and cross-sectional descriptive epidemiology in a scientific peer-reviewed journal.
Results:
PFPS is associated with decreased hip strength, specifically at the abductors and external rotators. There is a correlation between PFPS and faulty hip mechanics (adduction and internal rotation).
Conclusions:
There is a link between the strength and position of the hip and PFPS. These patients have a common deficit once symptomatic. Hip strengthening and a coordination program may be useful in a conservative treatment plan for PFPS.
Keywords: patellofemoral pain syndrome, hip strength, hip position, kinematics
Patellofemoral pain syndrome (PFPS) is often used as an umbrella term for anterior or retropalletar pain.9 Many factors present in patients with PFPS: patellar tracking dysfunction; decreased flexibility of the quadriceps, hamstrings, iliotibial band, and gastrocnemius; decreased strength of the quadriceps and hamstrings; joint laxity; deviations in patellar mobility and tilting; and increased quadriceps angle.38 While therapeutic interventions are performed to address these factors in the injured athlete, the significance of each factor to the onset of PFPS is unclear. A strong psychological component is often associated with these conditions, including higher rates of depression, fear-avoidance, and anxiety.25,26 Interestingly, the predominant factor for the development of PFPS may be outside the region.28
A systematic review by Crossley et al9 evaluated popular physical interventions, including vastus medialis oblique (VMO) retraining, open kinetic chain and isokinetic strengthening, patellar realignment orthoses, patellar mobilization, sacroiliac manipulation, low-level laser, acupuncture, and patellar taping. They found little evidence in support of these interventions. Pain reduction across all interventions was short-term at best and no more effective than a home-based exercise program.
The concept of a muscular imbalance between the VMO and the vastus lateralis is often faulted,§ although the literature is inconsistent.19 Laprade et al19 evaluated the recruitment of the VMO during specific open kinetic chain exercises, concluding that hip adduction, hip adduction during knee extension, medial tibial rotation, and medial tibial rotation during knee extension in open kinetic chain did not increase VMO activity. Earl et al12 showed that it was possible to selectively bias the VMO but only during minisquats with isometric hip adduction.
Methods
Data Sources
MEDLINE (from 1950–September 2010), CINAHL (1982–September 2010), and SPORTDiscus (1830– September 2010) were searched to identify relevant research.
Selection of Articles
Searches were performed using a subject heading alone (eg, patellofemoral pain) or in combination with other subjects (eg, patellofemoral pain AND hip strength) (Table 1). If a search term generated more than 200 articles, additional searches were performed. When fewer than 200 articles were identified, abstracts were reviewed to identify relevant articles. Randomized controlled trials, quasi-experimental designs, prospective epidemiology, case-control epidemiology, and cross-sectional descriptive epidemiology were included from scientific peer-reviewed journals. In addition, the reference list of each selected article was reviewed to identify other relevant publications. Studies must have assessed hip strength, lower extremity kinetics, or both in relation to PFPS.
Table 1.
Search strategy by heading and number of articles.
| Medical Subject Headings | Identified | Determined as Potentially Relevant | Included in Critical Appraisal |
|---|---|---|---|
| Anterior knee pain | 3220 | — | — |
| Patellofemoral pain | 3021 | — | — |
| Patellofemoral pain syndrome | 1807 | — | — |
| Patellofemoral pain AND biomechanics | 536 | — | — |
| Patellofemoral dysfunctiona | 145 | 2 | 2 |
| Retropatellar pain | 88 | 2 | 0 |
| Patellofemoral pain AND hip strength | 87 | 15 | 13 |
| Patellofemoral pain AND hip position | 18 | 0 | 0 |
The 2 articles identified in the patellofemoral dysfunction category were also identified in the patellofemoral pain AND hip strength category.
Results
The Influence of the Hip
An increase in hip adduction or internal rotation increases the Q angle by increasing the relative valgus of the lower extremity. This increased Q angle increases the peak lateral contact pressure on the patellofemoral joint.16,20 An increase of 10° in the Q angle can increase contact pressure on the patellofemoral joint by 45%.16 Internal rotation of the femur or external rotation of the tibia also increases patellofemoral contact pressure.20
Hip Position
Hip adduction during functional activities has been evaluated in several studies (Table 2).3,6,10,29,35,36,40 Females with PFPS demonstrate no difference in hip position during functional tasks, including running, stepping down, and landing from a jump.36 Bolgla et al3 reported no difference in hip position on stair descent. However, Wilson and Davis40 reported that females with PFPS demonstrated greater hip adduction during running, hopping, and performing the single-leg squat. Dierks et al10 found an increase in hip adduction in PFPS patients after a prolonged run, suggesting that this may represent fatigue.
Table 2.
Studies assessing the relationship between hip adduction and individuals with patellofemoral pain syndrome.a
| Study | Study Design; Level of Evidence | Participants | Activity Studied | Findings |
|---|---|---|---|---|
| Powers et al29 | Repeated measures; 5 | Six females (mean age, 32 years; range, 15-39 years) receiving treatment for PFP from a university sports medicine center. A participant must have demonstrated lateral patellar subluxation during kinematic MRI. | Weightbearing and nonweightbearing knee extension during kinematic MRI. | Significantly greater lateral patellar displacement during nonweightbearing knee extension. Significantly greater hip internal rotation during weightbearing knee extension. |
| Bolgla et al3 | Cross-sectional; 4 | Thirty-six women: 18 symptomatic (24.5 ± 3.2 years) and 18 matched for age, body mass, and height (23.9 ± 2.8 years) | Kinematic motion analysis during stair-stepping sequence. | No kinematic differences found between groups during the stair-stepping sequence. |
| Dierks et al10 | Cross-sectional; 4 | Forty runners: 20 with diagnosis of PFP (5 males, 15 females, 24.1 ± 7.4 years) and 20 asymptomatic sex-matched runners serving as controls (22.7 ± 5.6 years) | Kinematic motion analysis during running. Variables analyzed: knee adduction, hip adduction, and hip internal rotation peak angles. | A significant association between hip abductor weakness and hip adduction peak angle was observed in runners with a diagnosis of PFP. |
| Willson and Davis40 | Cross-sectional; 4 | Forty females: 20 with PFP (mean age, 23.3 years) and 20 serving as controls (mean age, 23.7 years) | Kinematic motion analysis during 3 activities: single-leg squat, run, and single-leg jump. | Females with PFP performed activities with significantly greater hip adduction and significantly less hip internal rotation. Trending toward significance, females with PFP demonstrated larger knee external rotation. |
| Boling et al6 | Prospective cohort; 2 | 1597 US Naval Academy midshipmen | Kinematic motion analysis during a jump-land-jump sequence (jump from box, land on force plate, vertical jump). | A risk factor associated with individuals who later developed PFP include “increased hip internal rotation angle during the jump-landing task.” |
| Souza and Powers36 | Cross-sectional; 4 | Forty-one females: 21 with PFP (27 ± 6 years old) and 20 asymptomatic controls (26 ± 5 years old) | Kinematic motion analysis during 3 activities: a step down, drop jump, and running. | Females with PFP demonstrated significantly greater hip internal rotation. |
| Souza et al35 | Cross-sectional; 4 | Thirty females: 15 with PFP (30.8 ± 8.9 years old) and 15 asymptomatic controls (29.1 ± 4.2 years old) | Kinetic imaging of a single-leg squat performed in a vertically open MRI. | Significantly greater lateral patella tilt at 3 angles (30°, 15°, 0°) and lateral patella displacement in females with PFP. Significantly greater internal rotation of the femur in females with PFP (measured at 45°, 15°, 0°). |
MRI, magnetic resonance imaging; PFP, patellofemoral pain.
Dynamic magnetic resonance imaging techniques have been used to compare patellar tilting and tracking during nonweightbearing and weightbearing activities in females with lateral patellar subluxation.29 In nonweightbearing, the patella tilts and tracks laterally on a stable femur. In weightbearing, the femur internally rotates, causing a stable patella to track laterally relative to the femur. Two studies compared PFPS patients with a control group, finding that the former had up to double the femoral internal rotation as the latter.35,36 This may be a link between PFPS and hip strength/coordination.28
A prospective 3-dimensional motion analysis during a jump-landing task in over 1500 participants demonstrated an increase in femoral internal rotation in those who later developed PFPS.6 Wilson and Davis40 found an increase in hip adduction in those with PFPS that demonstrated less internal rotation than controls. Bolgla et al3 found no difference in femoral internal rotation during step-down activities.
Hip Strength
Several studies demonstrate a correlation between decreased hip strength and PFPS (Tables 3 and 4).* A systematic review of 5 studies3,8,17,27,33 assessing hip strength in patients with PFPS found that external rotation and abduction were weaker than in controls.30 Robinson and Nee33 noted strength deficits in hip extension, while Cichanowski et al8 also found weakness in the adductors and internal rotators. Both studies found that the most significant difference (up to 27%) was in abductor strength.
Table 3.
Studies assessing the relationship between patients with patellofemoral pain syndrome and hip weakness.a
| Study | Study Design; Level of Evidence | Participants | Inclusion and Exclusion Criteria | Results |
|---|---|---|---|---|
| Ireland et al17 | Cross-sectional; 4 | Thirty females: 15 patients (15.7 ± 2.7 years old) and 15 asymptomatic age-matched controls (15.7 ± 2.7 years old) |
Inclusion: For the PFP group, “a thorough evaluation at a local orthopaedic practice.” Patients reported pain for a minimum of 3 months experienced during stair climbing, prolonged sitting, or sports and presented with “objective signs consistent with PFP.” Exclusion: Other comorbidities ruled out by orthopaedist during the patient’s examination, a history of significant lower extremity trauma, history of knee surgery, or history of patella dislocation. |
Patients with PFPS were significantly weaker than age-matched counterparts (P < 0.001). Patients’ hip abduction isometric strength and hip external rotation isometric strength were reported to be 26% and 36% less than those in the control group. |
| Piva et al27 | Case control; 4 | Sixty participants: 30 patients with PFPS (females = 17, males = 13) and 30 asymptomatic sex- and age-matched controls |
Inclusion: Age range from 20 to 42 years, experienced symptoms for at least 4+ weeks, nontraumatic onset, pain in either knee or both. In addition, reproduction of pain in a minimum of 3 of the following tests or positions: “manual compression of the patella against femur (at rest or during quad set), palpation of posteromedial or posterolateral borders of the patella, resisted is isometric quad contraction at 60° of flexion, squats, stair climbing, kneeling, or prolonged sitting” (Piva). Exclusion: Pregnancy, history of patella dislocation, a surgery to the knee in the prior 2 years, comorbid condition of the knee, condition that affects gait. |
The authors found no differences in hip external rotation and hip abduction strength between groups. |
| Cichanowski et al8 | Cross-sectional; 4 | Division III female athletes who reported to the school’s sports medicine team: 13 women diagnosed with PFPS (19.3 ± 1.1 years old) and 13 sport-matched controls (19.5 ± 1.3 years old) |
Inclusion: PFPS diagnosis based on physician examination. Exclusion: Previous history of knee trauma, surgery, or diagnoses. |
Athletes with a diagnosis of PFPS were significantly weaker in their ipsilateral hip abductors (P = 0.003) and external rotators (P = 0.049) when compared with the contralateral side. The athletes’ involved leg was significantly weaker in all hip muscle groups, except the adductors, when compared with controls. |
| Robinson et al33 | Cross-sectional; 4 | Twenty females: 10 with unilateral PFP (mean age, 21 years) and 10 serving as controls (mean age, 26.6 years) | Inclusion: 12 to 35 years old, nontraumatic onset of symptoms, pain during prolonged sitting, sports, or stair climbing. | The patient’s symptomatic leg was weaker than her uninvolved leg, with the symptomatic leg significantly weaker in hip extension and abduction (both P < 0.001). The patients’ symptomatic legs were significantly weaker in hip extension and external rotation when compared with the weaker legs of those in the control group. |
| Bolgla et al3 | Cross-sectional; 4 | Thirty-six women: 18 symptomatic women (24.5 ± 3.2 years old) and 18 women matched for age, body mass, and height (23.9 ± 2.8 years old) |
Inclusion: Experimental group—minimum of 1 month of anterior knee pain experienced during stair descent and during 2 or more of the following: squatting, stair ascent, prolonged sitting, kneeling. Control group—no previous history of knee or hip pathology and no pain with any of the aforementioned provocative activities Exclusion: History of knee surgery, significant injury, patellar dislocation; abnormal gait due to neurologic diagnosis, history of hip surgery, or prior injury to the hip. |
Symptomatic women were weaker than controls, generating significantly less torque with the hip external rotators (P = 0.002) and abductors (P = 0.006). |
| Dierks et al10 | Cross-sectional; 5 | Forty runners: 20 runners with diagnosis of PFP (5 males, 15 females; 24.1 ± 7.4 years old) and 20 asymptomatic sex-matched runners (22.7 ± 5.6 years old) | Inclusion: 18 to 45 years old, heel-strike running pattern, no foot orthoses. | Those with PFP presented with significantly lower isometric hip abduction strength than asymptomatic counterparts. |
| Baldon et al2 | Cross-sectional; 4 | Twenty females: 10 patients with PFPS (22.9 ± 5.2 years old) and 10 asymptomatic females matched for age (23.9 ± 2.4 years old), height, and body mass serving as controls |
Inclusion (for patients with PFPS): Anterior knee pain in typical provocative activities (at least 3), nontraumatic onset with symptoms for at least 4 weeks, pain response with palpation of facets when one performs a squat or a step-down maneuver. Exclusion: History of knee surgery to patellofemoral joint, history of patella dislocation or patellar apprehension sign, history and signs/symptoms of intra-articular dysfunction, patella tendon pain with palpation, iliotibial band tenderness, apophysitis, knee swelling, or proximal joint pain. |
Patients presented with lower eccentric hip adduction and abduction peak torque scores than controls. While the differences were not significant, there was a trend toward significance. |
| Boling et al6 | Prospective cohort; 2 | 1597 US Naval Academy midshipmen | Inclusion: Enrolled in freshman year with no current injury that would prevent one from performing baseline tests. | Increased hip external rotation strength is a potential risk factor for midshipmen who developed PFPS. |
| Long-Rossi and Salisch21 | Observational, cohort; 4 | Twenty-one women (26 ± 7 years old) with PFP |
Inclusion: Pain from the patellofemoral joint reproduced during unilateral squat and step down and during a quadriceps muscle manual test; in addition, pain for at least 2 months. Exclusion: History of previous traumatic knee injury, knee surgery, current knee pathology. |
Increased hip external rotation strength correlates with higher functional scores in patients with PFPS. |
PFP, patellofemoral pain; PFPS, patellofemoral pain syndrome.
Table 4.
Summary of strength testing methodology.a
| Study | Testing Procedure | Muscle Groups Assessed | General Strength Test Positions |
|---|---|---|---|
| Ireland et al17 | Isometric strength with HHD (make test); peak value of 3 tests | Hip abduction, ER | Abduction: side lying, hip abduction to 10°.ER: sitting, hips and knees at 90°. |
| Piva et al27 | Isometric strength with HHD (make test); average score of 2 tests recorded | Hip abduction, ER | Abduction: side lying, abduction to approximately 30°.ER: prone, knee flexed to 90°. |
| Cichanowski et al8 | Isometric strength with HHD (make test); best score of 2 tests | Hip flexion, abduction, adduction, extension, ER, IR | Flexion, IR, ER: sitting, hip and knee flexed to 90°.Abduction and adduction: side lying. Extension: prone, leg extended. |
| Robinson and Nee33 | Isometric strength with HHD (break test); average score of 3 tests recorded | Hip abduction, extension, ER | Abduction: side lying, hip abduction to 30°.Extension: prone, knee flexed to 90°.ER: sitting, hips and knees at 90°. |
| Bolgla et al3 | Isometric strength with HHD (make test); average score of 3 tests | Hip abduction, ER | Abduction: side lying, hip abduction to 10°.ER: sitting, hips and knees at 90°. |
| Dierks et al10 | Isometric strength with HHD performed prior to and right after a run (make test); 5 tests performed | Hip abduction, ER | Abduction: side lying, hip abduction to 10°.ER: sitting, hips and knees at 90°. |
| Baldon et al2 | Isokinetic strength with isokinetic dynamometer (mean peak torque); 2 sets of 5 repetitions | Eccentric hip abduction, adduction, IR, ER | Abduction and adduction: side lying. ER and IR: sitting. |
| Boling et al6 | Isometric strength with HHD (make test); average score of 2 tests | Hip ER, IR, extension, abduction | Abduction: side lying. ER, IR, extension: prone, knee flexed to 90°. |
| Long-Rossi and Salsich21 | Isometric strength with HHD (break test); average score of 3 tests | Gluteus maximus, gluteus medius, hip ER | Gluteus maximus: prone, knee flexed to 90°.Gluteus medius: side lying. Hip ER: sitting, hip and knee flexed to 90°. |
HHD, handheld dynamometer; ER, external rotation; IR, internal rotation.
The prospective study by Boling et al6 analyzed 3-dimensional motion and 6 lower extremity isometric tests: knee extension, hip external rotation, hip internal rotation, knee flexion, hip extension, and hip abduction. Those with PFPS demonstrated decreased strength in hip abduction, knee flexion, and knee extension. Interestingly, hip external rotation strength increased in those who developed PFPS compared to controls.
Baldon et al2 evaluated eccentric strength between a group of females with PFPS and a control group (abduction, adduction, external rotation, and internal rotation). Peak torque was 28% lower in the abductors and 14% lower in the adductors in the PFPS group. The eccentric adduction:abduction torque ratio was also 11% higher in the PFPS group.
Hip musculature fatigue testing in runners with PFPS compared decreased strength in the hip abductors and external rotators at the end of the prolonged run.10 The PFPS group demonstrated 12% lower strength at the end of the run compared to the control group.
Long-Rossi and Salsich21 correlated hip strength and functional status in PFPS patients using the Anterior Knee Pain Questionnaire (Kujala score).18 They found a correlation between strength and pain but not between external rotator strength and the Kujala score.21
Clinical Application
It is unknown if the hip weakness demonstrated in the reviewed studies is the cause of PFPS or the result.10,28 There are inconsistencies in these studies emphasizing the differences in study design measurement techniques.28 Variations in hip mechanics may become much more pronounced with fatigue.31 Most studies evaluate peak strength and not endurance.31
Since the hip abductors can affect knee valgus by controlling the frontal plane position of the femur,15 increasing abduction strength may help patients with PFPS. Strengthening programs often begin with isometrics (prone heel squeezes) to encourage muscle recruitment. Manual perturbations side lying (Figure 1) may add a low-intensity random component to the early phases of rehabilitation. This exercise can also be performed to fatigue to encourage an endurance response. Patients can then be progressed to standing abduction against a resistance band.4 Side-to-side walking with a resistance band around the ankles (Figure 2) may further challenge the hip abductors and add an eccentric component to the training program. The pelvic drop exercise encourages high activity in the hip musculature while demonstrating low stress at the knee.1,4 This activity can be progressed to a lateral step-up. Research has shown that increasing squat depth progressively increases the activity in the gluteus medius7 and may be a good functional progression for athletes. Adding single-leg squats on a physioball (Figure 3) may address lower extremity coordination and hip position in relation to the knee.
Figure 1.

Manual perturbations applied against the hip musculature in side lying.
Figure 2.

Side-to-side walking with a resistance band around the ankles.
Figure 3.

Single-leg squats with a physioball. The focus should be on proper knee and hip position with this activity.
In the later phases of rehab, progressing through higher level exercises, such as the modified single-leg squat,24 side bridge,13 and lunge while twisting (Figure 4), provides a higher level of challenge. The Smith machine may minimize challenges to stability, but it allows a higher resistance for building strength.
Figure 4.

Lunge with twist.
Conclusions
There is a link between the strength and position of the hip and PFPS. Common deficits are often seen in these patients. Incorporating a hip strengthening and coordination program may be a useful component of a treatment plan for PFPS.
Footnotes
References
- 1. Ayotte N, Stetts D, Keenan G, Greenway E. Electromyographical analysis of selected lower extremity muscles during 5 unilateral weight-bearing exercises. J Orthop Sports Phys Ther. 2007;37(2):48-55 [DOI] [PubMed] [Google Scholar]
- 2. Baldon R, Nakagawa T, Muniz T, et al. Eccentric hip muscle function in females with and without patellofemoral pain syndrome. J Athl Train. 2009;44:490-496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bolgla L, Malone T, Umberger B, Uhl T. Hip strength and hip and knee kinematics during stair descent in females with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2008;38:12-18 [DOI] [PubMed] [Google Scholar]
- 4. Bolgla L, Uhl T. Electromyographic analysis of hip rehabilitation exercises in a group of healthy subjects. J Orthop Sports Phys Ther. 2005;35:487-494 [DOI] [PubMed] [Google Scholar]
- 5. Boling M, Bolgla L, Mattacola C, et al. Outcomes of a weight-bearing rehabilitation program for patients diagnosed with patellofemoral pain syndrome. Arch Phys Med Rehabil. 2006;87:1428-1435 [DOI] [PubMed] [Google Scholar]
- 6. Boling M, Padua D, Marshall S, et al. A prospective investigation of biomechanical risk factors for patellofemoral pain syndrome: the Joint Undertaking to Monitor and Prevent ACL Injury (JUMP-ACL) cohort. Am J Sports Med. 2009;37:2108-2116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Caterisano A, Moss R, Pellinger T, et al. The effect of back squat depth on the EMG activity of 4 superficial hip and thigh muscles. J Strength Cond Res. 2002;16(3):428-432 [PubMed] [Google Scholar]
- 8. Cichanowski H, Schmitt J, Johnson R, Niemuth P. Hip strength in collegiate female athletes with patellofemoral pain. Med Sci Sports Exerc. 2007;39:1227-1232 [DOI] [PubMed] [Google Scholar]
- 9. Crossley K, Bennell K, Green S, McConnell J. A systematic review of physical interventions for patellofemoral pain syndrome. Clin J Sport Med. 2001;11:103-110 [DOI] [PubMed] [Google Scholar]
- 10. Dierks T, Manal K, Hamill J, Davis I. Proximal and distal influences on hip and knee kinematics in runners with patellofemoral pain during a prolonged run. J Orthop Sports Phys Ther. 2008;38:448-456 [DOI] [PubMed] [Google Scholar]
- 11. Douchette S, Goble R. The effect of exercise on patellar tracking in lateral patellar compression syndrome. Am J Sports Med. 1992;20:434-440 [DOI] [PubMed] [Google Scholar]
- 12. Earl J, Schmitz R, Arnold B. Activation of the VMO and VL during dynamic mini-squat exercises with and without isometric hip adduction. J Electromyogr Kinesiol. 2001;11:381-386 [DOI] [PubMed] [Google Scholar]
- 13. Ekstrom R, Donatelli R, Carp K. Electromyographical analysis of core trunk, hip, and thigh muscles during 9 rahabilitation exercises. J Orthop Sports Phys Ther. 2007;37(12):754-762 [DOI] [PubMed] [Google Scholar]
- 14. Hanten W, Schulthies S. Exercise effect on electromyographic activity of the vastus medialis oblique and vastus lateralis muscles. Phys Ther. 1990;70:561-565 [DOI] [PubMed] [Google Scholar]
- 15. Hollman J, Ginos B, Kozuchowski J, et al. Relationships between knee valgus, hip-muscle strength, and hip-muscle recruitment during a single-limb step-down. J Sport Rehabil. 2009;18:104-117 [DOI] [PubMed] [Google Scholar]
- 16. Huberti H, Hayes W. Patellofemoral contact pressures: the influence of Q-angle and tendofemoral contact. J Bone Joint Surg Am. 1984;66:715-724 [PubMed] [Google Scholar]
- 17. Ireland M, Wilson J, Ballantyne B, Davis I. Hip strength in females with and without patellofemoral pain. J Orthop Sports Phys Ther. 2003;33:671-676 [DOI] [PubMed] [Google Scholar]
- 18. Kujala U, Jaakkola L, Koskinen S, et al. Scoring of patellofemoral disorders. Arthroscopy. 1993;9:159-163 [DOI] [PubMed] [Google Scholar]
- 19. Laprade J, Culham E, Brouwer B. Comparison of five isometric exercises in the recruitment of the vastus medialis oblique in persons with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther. 1998;27:197-204 [DOI] [PubMed] [Google Scholar]
- 20. Lee T, Morris G, Csintalan R. The influence of tibial and femoral rotation on patellofemoral contact area and pressure. J Orthop Sports Phys Ther. 2003;33:686-693 [DOI] [PubMed] [Google Scholar]
- 21. Long-Rossi F, Salsich G. Pain and hip lateral rotator muscle strength contribute to functional status in females with patellofemoral pain. Physiother Res Int. 2009;15:57-64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mascal C, Landel R, Powers C. Management of patellofemoral pain targeting hip, pelvis, and trunk muscle function: 2 case reports. J Orthop Sports Phys Ther. 2003;33:647-660 [DOI] [PubMed] [Google Scholar]
- 23. McConnell J. The management of chondromalacia patellae: a long term solution. Aust J Physiother. 1987;32:24-32 [DOI] [PubMed] [Google Scholar]
- 24. McCurdy K, O’Kelley E, Kutz M, et al. Comparison of lower extremity EMG between the 2-leg squat and modified single-leg squat in female athletes. J Sport Rehabil. 2010;19:57-70 [DOI] [PubMed] [Google Scholar]
- 25. Piva S, Fitzgerald G, Wisniewski S, Delitto A. Predictors of pain and function outcome after rehabilitation in patients with patellofemoral pain syndrome. J Rehabil Med. 2009;41:604-612 [DOI] [PubMed] [Google Scholar]
- 26. Piva S, Fitzgerald K, Irrgang J, et al. Associates of physical function and pain in patients with patellofemoral pain syndrome. Arch Phys Med Rehabil. 2009;90:285-295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Piva S, Goodnite E, Childs J. Strength around the hip and flexibility of soft tissues in individuals with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2005;35:793-801 [DOI] [PubMed] [Google Scholar]
- 28. Powers C. The influence of abnormal hip mechanics on knee injury: a biomechanical perspective. J Orthop Sports Phys Ther. 2010;40(2):42-51 [DOI] [PubMed] [Google Scholar]
- 29. Powers C, Ward S, Fredericson M, et al. Patellofemoral kinematics during weight-bearing and non-weight-bearing knee extension in persons with lateral subluxation of the patella: a preliminary study. J Orthop Sports Phys Ther. 2003;33:677-685 [DOI] [PubMed] [Google Scholar]
- 30. Prins M, van der Wurff P. Females with palleofemoral pain syndrome have weak hip muscles: a systematic review. Aust J Physiother. 2009;55:9-15 [DOI] [PubMed] [Google Scholar]
- 31. Reiman M, Bolgla L, Lorenz D. Hip functions influence on knee dysfunction: a proximal link to a distal problem. J Sport Rehabil. 2009;18:33-46 [DOI] [PubMed] [Google Scholar]
- 32. Reynolds L, Levin T, Medeiros J, et al. EMG activity of the vastus medialis oblique and the vastus lateralis in their role in patellar alignment. Am J Phys Med. 1983;62:61-70 [PubMed] [Google Scholar]
- 33. Robinson R, Nee R. Analysis of hip strength in females seeking physical therapy treatment for unilateral patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2007;37:232-238 [DOI] [PubMed] [Google Scholar]
- 34. Souza D, Gross M. Comparison of vastus medialis oblique: vastus lateralis muscle integrated electromyographic ratios between healthy subjects and patients with patellofemoral pain. Phys Ther. 1991;71:310-320 [DOI] [PubMed] [Google Scholar]
- 35. Souza R, Draper C, Fredericson M, Powers C. Femur rotation and patellofemoral joint kinematics: a weight-bearing MRI analysis. J Orthop Sports Phys Ther. 2010;40(5):277-285 [DOI] [PubMed] [Google Scholar]
- 36. Souza R, Powers C. Differences in hip kinematics, muscle strength, and muscle activation between subjects with and without patellofemoral pain. J Orthop Sports Phys Ther. 2009;39:12-19 [DOI] [PubMed] [Google Scholar]
- 37. Tyler T, Nicholas S, Mullaney M, McHugh M. The role of hip muscle function in the treatment of patellofemoral pain syndrome. Am J Sports Med. 2006;34:630-636 [DOI] [PubMed] [Google Scholar]
- 38. Waryasz G, McDermott A. Patellofemoral pain syndrome (PFPS): a systematic review of anatomy and potential risk factors. Dyn Med. 2008;7:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Wilk K, Davies G, Mangine R, Malone T. Patellofemoral disorders: a classification system and clinical guidelines for nonoperative rehabilitation. J Orthop Sports Phys Ther. 1998;28(5):307-322 [DOI] [PubMed] [Google Scholar]
- 40. Willson J, Davis I. Lower extremity mechanics of females with and without patellofemoral pain across activities with progressively greater task demands. Clin Biomech (Bristol, Avon). 2008;23:203-211 [DOI] [PubMed] [Google Scholar]
- 41. Zappala F, Taffel C, Scuderi G. Rehabilitation of patellofemoral joint disorders. Orthop Clin North Am. 1992;23:555-566 [PubMed] [Google Scholar]