Abstract
Background:
Effective treatments for chronic lateral epicondylosis have not been studied adequately. Eccentric overload exercises have been used with success for other chronic tendinopathy, mainly Achilles and patellar.
Hypothesis/Purpose:
To compare a wrist extensor eccentric strengthening exercise program with a wrist extensor stretching/modality program for the treatment of chronic lateral epicondylosis. The authors hypothesized that the eccentric strengthening program would produce more favorable results than a stretching/modality program.
Study Design:
Prospective randomized controlled trial.
Methods:
Twenty-eight adults with lateral epicondylosis of greater than 4 weeks’ duration were randomized to an eccentric strengthening group or a stretching group. Exercises were taught by a physical therapist, and participants performed most of the exercises on their own at home. Pain scores with visual analog scale from 0 to 100 were obtained at baseline and then at 4, 8, 12, 16, and 20 weeks after the start of the exercise program.
Results:
Both groups improved their pain scores from baseline to the 4-week time point, followed by nonsignificant further decreases in pain scores thereafter. No statistically significant differences were found between the eccentric strengthening group and stretching groups at any follow-up time point.
Conclusions:
Despite previous reports documenting favorable results with eccentric exercises for other tendinopathy, the authors were unable to show any statistical advantage to eccentric exercises for lateral epicondylosis during these periods compared with local modalities and stretching exercises.
Keywords: tendinopathy, tennis elbow, eccentric exercise, overuse injury
Lateral epicondylosis is a common clinical entity seen in general practice, as well as orthopaedics and sports medicine. Despite its high prevalence, the etiology and pathophysiology remain poorly understood, and treatment methods have not been adequately studied.
The etiology of lateral epicondylosis is unclear. Histologic studies have not documented evidence of inflammation in chronic lateral epicondylosis11,14 or in other chronic tendinopathy, including Achilles,2,15 patellar,10 and rotator cuff.8 These conditions all appear to represent tendinosis, with disordered collagen bundles, abnormal cellularity, increased mucoid ground substance, and random neovascularization, commonly termed mucoid degeneration.2 In lateral epicondylosis, this degeneration occurs in the tendon of the extensor carpi radialis brevis.
With our relatively poor understanding of the etiology and pathophysiology of lateral epicondylosis, it is not surprising that optimal treatment methods are unclear. Most recommended treatment modalities are empiric and based on intuition and expert opinion. Commonly advocated treatments include activity modification, local modalities, medications, bracing, stretching, strengthening, local injections, and surgery. Very few controlled studies exist that document efficacy for any of these treatment methods.3
The efficacy of heavy-load eccentric strengthening exercises has been demonstrated for chronic Achilles tendinosis1,12,16 and patellar tendinosis.4,7,9,18
The purpose of this study was to evaluate the efficacy of a specifically designed eccentric overload program for chronic lateral epicondylosis, compared with a control group receiving local modalities and stretching exercises. We hypothesized that eccentrically trained participants would have greater rates of improvement.
Methods
This study was approved by the University of Missouri Health Sciences Institutional Review Board. After completing a questionnaire, participants were randomized by a computer-generated sequence either to the eccentric exercises or to the stretching and modality group.
Participants
Participants were recruited from a university-based outpatient family medicine practice. Inclusion criteria included the following: age older than 18 years; lateral elbow pain for at least 4 weeks; and physical examination evidence of lateral epicondylosis, including local tenderness at or just distal to the lateral epicondyle, along with reproduction of pain with resisted wrist extension, with the elbow completely extended, regardless of previous treatments. Exclusion criteria included medical contraindication to the exercises, mental incompetence, and age younger than 18 years.
Questionnaire
The questionnaire (see appendix) included basic demographic information, including age, sex, hand dominance, occupation, and recreational or sporting activities involving the upper extremities. Duration of symptoms, severity of pain (based on a visual analog scale), previous and current treatments, workers’ compensation status, and history of past episodes were recorded.
Eccentric Exercise Training Group
The eccentric exercise began with the wrist and elbow in the extended position and the volar forearm resting on the edge of a table (Figure 1). The contralateral uninvolved hand pushed the involved wrist from its original extended position to a fully flexed position over 6 to 8 seconds. The involved wrist counteracted this flexion force by actively extending against resistance. The amount of force applied was the maximum load tolerated for 3 sets of 15 repetitions daily. The participants were warned that the exercises would be quite painful. They met with the therapist twice a week for the first 2 weeks, then once per week for 12 weeks. They were instructed to apply more force as pain tolerance improved. No other treatments were administered by the therapist, and participants were asked to stop any other treatments for their condition. No activity restrictions were made.
Figure 1.
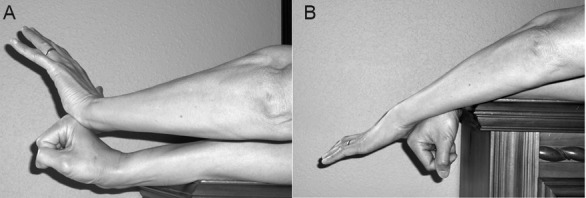
Eccentric strengthening exercise: A, the starting position for the eccentric strengthening exercise. The participant’s involved right wrist actively extends against the contralateral left hand, which attempts to push the right wrist into a flexed position. B, the finishing position of the eccentric exercise with the involved right wrist pushed into the fully flexed position.
Control Group
The control group had local modality treatments, iontophoresis (2 mL of 4% dexamethasone with a 40-mA/min phoresor) as well as other modalities at the therapist’s discretion, according to the same schedule as for the eccentric training group. Participants who had more tenderness in the muscle mass just distal to the lateral epicondyle were treated with ultrasound using 1.0 MHz frequency, 100% duty cycle, and 1.0 W/cm2 for 8 minutes. Of the 16 participants originally randomized to this control group, 13 received at least 1 treatment of both iontophoresis and ultrasound, 1 received only ultrasound treatments, and 2 received only iontophoresis treatments. This group also performed stretching exercises for the wrist extensor muscles 3 times daily, and no specific activity restrictions were made (Figure 2).
Figure 2.

Wrist extensor stretching exercise. The uninvolved left hand assists passive stretching of the involved right wrist extensor muscles.
Follow-up
A researcher, who was blinded to participants’ group assignments and not involved with the care of the participants, collected the follow-up data at 4, 8, 12, 16, and 20 weeks after commencement of the exercise program. A follow-up questionnaire was completed at each of these time points. Overall satisfaction with treatment was graded by 3 choices: very satisfied, moderately satisfied, or dissatisfied. Compliance with the exercises was assessed at these time points. Participants dissatisfied with their outcomes were allowed to switch to the opposite treatment arm of the study at any time during the study.
Statistics
A sample size estimate was not performed. The participants’ levels of pain at baseline and the follow-up time points were the primary outcome variables. Wilcoxon 2-sample tests were performed to compare the treatment and control groups at each time point. Signed-rank test was used to compare within-group differences in pain level over time. Secondary outcomes included pain at each time point compared with baseline. Signed-rank test was used to compare grip strength within each group over time. Spearman correlation coefficients were derived for each group between duration of symptoms and improvement in pain level.
Results
Three participants switched from the control group to the treatment group at variable time points during the study. These 3 participants’ data were treated as missing after they switched groups. Participants who received a local lateral epicondylar injection during the course of the study were treated as missing after the injection.
A post hoc power analysis showed that with a standard deviation of 19, a sample size of 14 would have 77% power to detect a difference of 20 on the pain scale (0-100) between the 2 groups.
The eccentric exercise group had 14 participants with mean age of 48.0 ± 9.0 years. There were 9 men and 5 women. The dominant arm was involved in 11 participants; the nondominant arm was involved in 2 participants; and 1 participant was ambidextrous. The mean duration of pain in this group was 85.9 ± 42.8 days. The mean baseline pain score from 0 to 100 was 63 ± 19.
The control group had 14 participants with mean age of 43.9 ± 4.7 years. There were 6 men and 8 women. The dominant arm was involved in 8 participants; the nondominant arm was involved in 5 participants; and 1 participant had bilateral symptoms. The mean duration of pain was 116.6 ± 85.8 days. The mean baseline pain score was 61 ± 19.
The eccentric exercise group mean decrease in pain score between baseline and the 4-week follow-up was 34 points, which was statistically significant (P = 0.01). Only slight further decreases in pain (scores from 1 to 11) occurred at subsequent follow-up times. These decreases were not statistically significant compared with previous time points.
For the control group, a statistically significant decrease of 28 points occurred between baseline and the 4-week follow-up with P <0.01. None of the other subsequent time points had further statistically significant decreases in pain scores, which ranged from 4- to 10-point decreases.
No statistically significant differences between the groups existed at any of the time points. Repeating the comparison of mean pain scores between the groups with participants who either crossed over to the opposite group or received an injection, with last observation carried forward, revealed similar results.
Spearman correlation coefficient showed no statistically significant correlation between duration of pain and improvement at 4 weeks for either group. At 8 weeks, the eccentric exercise group had statistically significantly greater pain relief than the control group (P <0.01) but not at any other time point. No statistically significant differences were found between the groups for grip strength at any time point. The overall satisfaction score at last available follow-up time point was not statistically different between the groups (P = 0.84). No statistically significant linear correlations were found for either group between compliance scores and pain scores at the 4-week time point.
Discussion
This study has several limitations, including the low number of participants, lack of sample size estimate, short duration of symptoms in some participants, and varied treatment programs in the control group. However, both groups improved between baseline and the 4-week follow-up point.
Secondary outcomes did indicate a statistically significant improvement in pain level compared with baseline favoring the eccentric strengthening group at the 8-week time point. Grip strength and overall satisfaction showed no statistically significant differences between the groups.
Recent controlled studies have suggested that heavy-load eccentric exercises are efficacious for chronic midsubstance Achilles tendinosis and, to a lesser degree, for chronic patellar tendinosis.1,4,7,9,12,16,18 Alfredson et al demonstrated clear clinical success with use of this eccentric strengthening program, lasting 12 weeks, in a nonrandomized study comparing 15 participants with recalcitrant Achilles tendinosis to a similar group of 15 participants who received no treatment.1 A randomized controlled trial comparing (1) 22 participants with recalcitrant Achilles tendinosis using the same eccentric overload program with (2) 22 participants using concentric exercises showed an 82% success rate for the eccentric exercise group and a 36% success rate for the concentric exercise group.12
Svernlov and Adolfsson randomized 30 participants with lateral epicondylosis to a stretching group and an eccentric exercise group, both home based.17 Both groups achieved reductions in pain, with nonstatistically significant trends favoring the eccentric exercise group. The number of participants may have been too low to detect small differences between groups. Eighty-one participants were randomized to a stretching group, a stretching + eccentric strengthening group, or a stretching + concentric exercise group.13 All 3 groups improved over time with no statistical differences among them. In a nonrandomized study, 46 participants using conventional local modalities and stretching were compared with 46 participants treated with eccentric exercises 3 times a week.5 Both groups improved, with greater improvement for the eccentric exercise group.
Lateral epicondylosis is a form of insertional tendinopathy and therefore possibly less amenable to an eccentric training program. An eccentric overload program is much more effective in the midsubstance of the tendon for chronic Achilles tendinosis than at the insertion site.6
Two technical points to emphasize with eccentric overload programs for Achilles tendinosis: the amount of load applied to the tendon (which is usually very painful) and the need to reach the end range of dorsiflexion.12 This program usually caused pain, but painful overload was not consistently emphasized.
In conclusion, contrary to our hypothesis, this study did not demonstrate a clear benefit of an eccentric strengthening program for chronic lateral epicondylosis compared with a program of local modalities and wrist extensor stretching. Unfortunately, we were limited by small numbers of participants, the short duration of symptoms, variation in the control treatment, and uncontrolled concurrent treatments.
References
- 1. Alfredson A, Pietila T, Jonsson P, et al. Heavy-load eccentric calf muscle training for the treatment of chronic Achilles tendinosis. Am J Sports Med. 1998;26:360-366 [DOI] [PubMed] [Google Scholar]
- 2. Astrom M, Rausing A. Chronic Achilles tendinopathy: a survey of surgical and histopathologic findings. Clin Orthop. 1995;316:151-164 [PubMed] [Google Scholar]
- 3. Bisset L, Paungmali A, Vicenzino B, et al. A systematic review and meta-analysis of clinical trials on physical interventions for lateral epicondylalgia. Br J Sports Med. 2005;39:411-422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cannell LJ, Taunton JE, Clement DB, et al. A randomized clinical trial of the efficacy of drop squats or leg extension/leg curl exercises to treat clinically diagnosed jumper’s knee in athletes: pilot study. Br J Sports Med. 2001;35:60-64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Croisier JL, Foidart-Dessalle M, Tinant F, et al. An isokinetic eccentric programme for the management of chronic lateral epicondylar tendinopathy. Br J Sports Med. 2007;41:269-275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Fahlstrom M, Jonsson P, Lorentzon R, et al. Chronic Achilles tendon pain treated with eccentric calf-muscle training. Knee Surg Sports Traumatol Arthrosc. 2003;11:327-333 [DOI] [PubMed] [Google Scholar]
- 7. Frohm A, Saartok T, Halvorsen K, et al. Eccentric treatment for patellar tendinopathy: a prospective randomized short-term pilot study of two rehabilitation protocols. Br J Sports Med. 2007;41:e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fukuda H, Hamada K, Yamanaka K. Pathology and pathogenesis of bursal side rotator cuff tears viewed from en bloc histologic sections. Clin Orthop. 1990;254:75-80 [PubMed] [Google Scholar]
- 9. Jonsson P, Alfredson H. Superior results with eccentric compared to concentric quadriceps training in patients with jumper’s knee: a prospective randomized study. Br J Sports Med. 2005;39:847-850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Khan KM, Cook JL, Bonar F, et al. Histopathology of common tendinopathies: update and implications for clinical management. Sports Med. 1999;27:393-408 [DOI] [PubMed] [Google Scholar]
- 11. Kraushaar BS, Nirshl RP. Tendinosis of the elbow (tennis elbow): clinical features and findings of histological, immunohistochemical, and electron microscopy studies. J Bone Joint Surg Am. 1999;81:259-278 [PubMed] [Google Scholar]
- 12. Mafi N, Lorentzon R, Alfredson H. Superior short-term results with eccentric calf muscle training compared to concentric training in a randomized prospective multicenter study on patients with chronic Achilles tendinosis. Knee Surg Sports Traumatol Arthrosc. 2001;9:42-47 [DOI] [PubMed] [Google Scholar]
- 13. Martinez-Silvestrini JA, Newcomer KL, Gay RE, et al. Chronic lateral epicondylitis: comparative effectiveness of a home exercise program including stretching alone versus stretching supplemented with eccentric or concentric strengthening. J Hand Ther. 2005;18:411-420 [DOI] [PubMed] [Google Scholar]
- 14. Nirschl RP, Pettrone FA. Tennis elbow: the surgical treatment of lateral epicondylitis. J Bone Joint Surg Am. 1979;61:832-839 [PubMed] [Google Scholar]
- 15. Puddu G, Ippolito E, Postacchini F. A classification of Achilles tendon disease. Am J Sports Med. 1976;4:145-150 [DOI] [PubMed] [Google Scholar]
- 16. Silbernagel KG, Thomee R, Thomee P, et al. Eccentric overload training for patients with chronic Achilles tendon pain: a randomized controlled study with reliability testing of the evaluation methods. Scand J Med Sci Sports. 2001;11:197-206 [DOI] [PubMed] [Google Scholar]
- 17. Svernlov B, Adolfsson L. Non-operative treatment regime including eccentric training for lateral humeral epicondylalgia. Scand J Med Sci Sports. 2001;11:328-334 [DOI] [PubMed] [Google Scholar]
- 18. Young MA, Cook JL, Purdam CR, et al. Eccentric decline squat protocol offers superior results at 12 months compared with traditional eccentric protocol for patellar tendinopathy in volleyball players. Br J Sports Med. 2005;39:102-105 [DOI] [PMC free article] [PubMed] [Google Scholar]


