Abstract
Context:
Passive stretching exercise protocols, as part of outpatient treatment or home exercise programs, are used to improve hypomobility. Despite the cosmopolitan use of stretching exercises, little is known about the forces being applied to the joint during these routine treatments.
Type of Study:
Clinical review.
Evidence Acquisition:
Articles were identified using MEDLINE and Google Scholar databases, with searches initially limited to those articles published after 1995. Seminal articles that were referenced were also included.
Results:
Many factors contribute to the clinical success of a stretching program, including the frequency, intensity, and duration of the stretching exercises, as well as patient- and joint-specific factors.
Conclusions:
The goal of a stretching protocol is to maximize total end-range time both in the clinic and at home. Higher intensity, prolonged, and frequent stretching (10- to 15-minute bouts, 3 to 6 times per day) used as an adjunct to high-grade mobilizations may be beneficial for certain hypomobility conditions.
Keywords: range of motion, stiffness, rehabilitation, stretching
Hypomobility can be defined as increased resistance to passive movement. It can be the result of neural factors (eg, spasticity after stroke), systemic conditions (eg, diabetes mellitus), or peripheral changes in the mechanical properties of the muscles and joint capsule caused by adhesive capsulitis or arthrofibrosis. Adhesive capsulitis is the fibrosis and contracture of the capsuloligamentous complex and rotator interval, resulting in restricted range of glenohumeral external rotation.20,21,26 Arthrofibrosis is an excessive inflammatory response to a surgery or injury, associated with increases in both the production of fibroblasts and the deposition of extracellular matrix proteins.27
Stretching exercises have been traditionally used in treating hypomobility, based on the biological principle that connective tissue will remodel over time in response to physical stress. At the cellular level, motion restrictions involve the formation of cross bonds of the periarticular connective tissue that forms between the collagen bundles.5,6
Effective stretching exercises denature these cross bonds, allowing the collagen fibers to be reoriented parallel to the line of stress over time, thus creating the opportunity for plastic deformation of the collagen tissue.5,6
The ability of a given stretching exercise to create lasting gains in motion is dependent on the ability to permanently elongate the soft tissue. Permanent elongation, also called plastic deformation, is dependent on the amount of force that is applied, the amount of time that force is applied, and how often a stretching exercise is performed. This is the basis for the TERT formula—that is, the total end-range time, or the product of the intensity, frequency, and duration of the stretching exercises.17 This concept applies to passive stretching and mobilizations performed by clinicians, static splints, serial casting, home exercise programs, and mechanical therapy devices.
Tert Dose
All 3 factors in the TERT dose—intensity, duration, and frequency—are important to the clinical success of a stretching program. The TERT dose calculated in this article is the weekly stretching force instead of the daily TERT dose; the remodeling of connective tissue does not occur in a matter of minutes but over an extended period.17
Intensity
The intensity is the magnitude of force or torque being applied to the joint during a stretching exercise.17 Using an instrumented artificial leg, Uhl and Jacobs measured the torque applied by 14 physical therapists when performing knee extension mobilizations during common home exercises and by mechanical therapy devices.25 As expected, the physical therapists applied greater torque than the home exercises and devices.25
The intensity of stretch is important because too little force may result in an elastic response with little or no gain in range of motion.6 On the contrary, applying too much force may injure tissue, resulting in an inflammatory response.3,17 Hypomobility patients should maximize intensity during home exercises without risking a negative tissue response or actually injuring the tissue.
In a small study of nursing home patients, low-load prolonged stretching demonstrated better results than high-load brief stretching.16 A study of more than 60 000 knee arthrofibrosis patients under the age of 65 years were divided into 3 groups: physical therapy and low-intensity stretch with a mechanical therapy device, physical therapy and high-intensity stretch with a mechanical therapy device, and physical therapy alone.24 The high-intensity device resulted in a significantly reduced risk of rehospitalization and knee-related costs when compared with the low-intensity device. Those treated with the high-intensity device were 1.7 times less likely to require reoperation than those with physical therapy alone.
The stretch intensities may vary depending on the joint being treated. Based on anthropometric data and the forces and clinical results from previously reported studies of treatments for hypomobility,4,10,18 the intensities and TERT doses of several common stretching exercises performed by patients or clinicians for the knee, ankle, shoulder, and elbow can be calculated. For those motions with a lack of published references of applied forces (shoulder internal and external rotation, elbow extension), we used a handheld dynamometer to collect the amount of force applied by one of the authors (A.D.S.) immediately proximal to the wrist joint when a healthy volunteer performed these stretches. In addition, the distance from the elbow joint to the point of force application with the dynamometer was recorded (C.A.J. and A.D.S., unpublished data, 2010). By knowing the applied force, the relative joint angles during treatment, and the length and weight of limb from anthropometric data,4,10,18 we were able to calculate the stretch intensities for the average American male and female. The values were calculated for both sexes, as the lever arms and body segment masses differ, thus resulting in different applied torques between the sexes even if the force applied by the clinician remains the same.
Extrapolating from the values reported by Uhl and Jacobs25 by taking into account the aforementioned anthropometric information, we can calculate the intensities for the average American male and female as 72.6 N·m and 68.0 N·m, respectively, during knee extension mobilizations performed by physical therapists. Slant board exercise to improve ankle dorsiflexion demonstrated similar stretch intensities as the knee extension mobilizations, producing intensities of 73.9 N·m (male) and 56.3 N·m (female), respectively (Figure 1). Much lower forces were induced by a clinician for shoulder external rotation (abducted to 90°) (male = 9.5 N·m, female = 8.3 N·m) (Figure 2) and shoulder internal rotation (male = 12.0 N·m, female = 10.7 N·m) (Figure 3). The sleeper stretch is often used to target the posterior capsule to improve internal rotation. In the sleeper position, the clinician applied less force, resulting in lower stretch intensities (male = 10.0 N·m, female = 8.9 N·m). Elbow extension mobilizations produced the lowest intensities (male = 8.2 N·m, female = 7.1 N·m) (C.A.J. and A.D.S., unpublished data, 2010).
Figure 1.
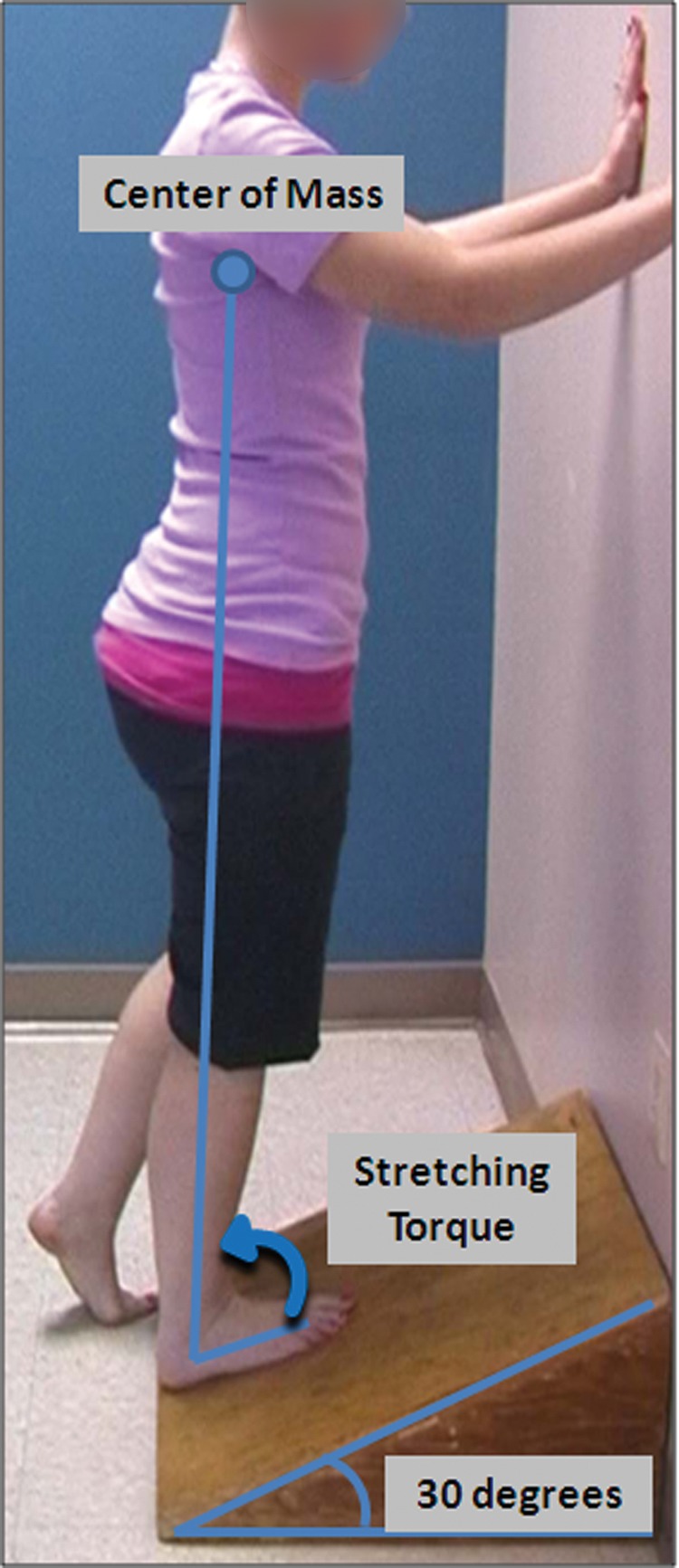
Patient performing the slant board exercise to increase ankle dorsi flexion. Using anthropometric data,4,10,18 we calculated the dorsiflexion torque of the average American male and female.
Figure 2.

Patient and clinician position while measuring the force applied during passive shoulder external rotation.
Figure 3.

Patient and clinician position while measuring the force applied during passive shoulder internal rotation.
Duration
Generally, stretch duration and intensity are inversely related. High-grade joint mobilizations may be performed in 30-second bouts,1 whereas low-intensity stretches can last 10 to 12 minutes,29 30 minutes,2,19 1 hour,16 3 hours,23 6 to 12 hours,12,13 or 24 hours per day, in the case of serial casting.
If the intensity and frequency of a given stretching exercise remain constant, increasing the duration will result in a proportional increase in the TERT dose. Increasing the TERT dose by solely increasing the duration of stretch may be effective. One example is that patients in splints for 6 to 12 hours per day demonstrated significantly improved results compared with those in splints for fewer than 6 hours per day.12
Connective tissue remodels over an extended period,17 emphasizing the importance of stretch duration. The overall treatment duration determines the weekly TERT dose and is a function of intensity, duration of each stretching bout performed, and frequency. Overall treatment duration is vital to the successful treatment of hypomobility.22
Frequency
Frequency has 2 components in the TERT dose: daily and weekly. High-grade mobilizations performed only 2 to 3 times per week, whereas home stretching exercises may be used 5 to 7 days per week. Stretching exercises cause the cross bonds to mechanically denature between collagen fibers; however, the cross bonds may be reestablished over the course of the next 24 hours.5 Lasting gains in range of motion require the prevention of cross-bond formation by stretching within the next 24 hours. In short, daily stretching is necessary to promote consistent, lasting range of motion improvement.5
Updated TERT formula
The weekly TERT dose is as follows:
The goal of calculating the minimum weekly TERT is to determine the dose necessary for lasting gains in range of motion. Weekly TERT doses greater than 10 000 N·m minutes per week are successful for knee flexion contractures7,25; however, joints have different anatomies, functions, and mobilities that influence the TERT dose necessary to increase range of motion. Greater torques may be necessary to increase motion of larger joints because of the amount and density of connective tissue, and future studies are necessary to determine joint-specific TERT doses.
Patient-Related Factors
Pain tolerance, duration of the contracture, and concomitant treatments influence the TERT dose needed for effective treatment.
Pain Tolerance
Stretch intensity is inherently mediated by pain. In the clinical setting, high-grade joint mobilizations may exceed the pain threshold but may be well tolerated by the patient because of the short bout duration. However, when at home, pain can be a protective mechanism. Stretching beyond the pain threshold for prolonged periods may result in an inflammatory response.3,17 Patients should stretch below the pain threshold, as setbacks can occur if they are too aggressive. Each patient’s pain tolerance should be taken into account when one designs the treatment protocol; that is, assume that patients with low pain tolerance will use lower stretch intensities and will therefore need to increase the duration and/or frequency of their stretching exercises. Special care must be used in prescribing stretching exercises for patients with sensory deficits that prevent or alter the perception of pain.
Duration of Contracture
The tensile strength of scar tissue increases throughout the first year following an injury or surgery.11 At 5 days, the tissue is at only 10% of its maximum strength, which increases to 40% at 40 days, 70% at 60 days, and 100% at 1 year.11 Chronic contractures are less responsive to stretching treatments, leading to smaller improvements in range of motion.22 Clinically, a low force may result in little or no gain in motion.
Other Treatments
Increased tissue temperature results in less force being required to increase tissue length.6,8,9,15 Warm-up, moist heat, ultrasound, and diathermy may increase tissue extensibility when used in conjunction with stretching exercises.6,8,9,15 Modalities that decrease pain may also allow patients to tolerate higher stretch intensities.
Complementary or accessory motions can increase the effectiveness of a stretching protocol.14,28 Adhesive capsulitis patients treated with posterior glides increased mean shoulder external rotation by 31.3° with posterior glides, compared to 3.0° with anterior glides.14 In addition, knee range of motion may improve when patellar mobility increases.28
Conclusions
Many factors contribute to the clinical success of a stretching program. The frequency, intensity, and duration are critical to achieve plastic deformation of the tissue and lasting gains in range of motion. Patient-related factors—including age, quality of tissue, duration of disuse or immobilization, pain tolerance, and exercise quality—influence the forces that must be applied to increase motion. The resulting TERT dose differs not only between patients but also joints. The goal of a stretching protocol is to maximize TERT both in the clinic and at home. Higher intensity, prolonged, and frequent stretching (10- to 15-minute bouts, 3 to 6 times per day) may be more beneficial for certain conditions.
References
- 1. Bandy W, Irion J, Briggler M. The effect of time and frequency of static stretching on flexibility of the hamstring muscles. Phys Ther. 1997;77(10):1090-1096 [DOI] [PubMed] [Google Scholar]
- 2. Bonutti P, Windau J, Ables B, Miller B. Static progressive stretch to reestablish elbow range of motion. Clin Orthop Relat Res. 1994;303:128-134 [PubMed] [Google Scholar]
- 3. Brand P. Clinical Mechanics of the Hand. St Louis, MO: CV Mosby; 1984 [Google Scholar]
- 4. Chaffin D, Andersson G, Martin B. Occupational Biomechanics. 3rd ed. New York: John Wiley & Sons; 1999 [Google Scholar]
- 5. Cummings G, Tillman L. Remodeling of dense connective tissue in normal adult tissues. In: Currier D, Nelson R, ed. Dynamics of Human Biologic Tissues. Philadelphia, PA: FA Davis Co; 1992:45-73 [Google Scholar]
- 6. Davies G, Ellenbecker T. Focused exercise aids shoulder hypomobility. Biomechanics. 1999;6:77-81 [Google Scholar]
- 7. Dempsey A, Branch T, Mills T, Karsch R. High-intensity mechanical therapy for loss of knee extension for worker’s compensation and non-compensation patients. Sports Med Arthrosc Rehabil Ther Technol. 2010;2:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Draper D, Anderson C, Schulthies S, Ricard M. Immediate and residual changes in dorsiflexion range of motion using an ultrasound heat and strech routine. J Athl Train. 1998;33:141-144 [PMC free article] [PubMed] [Google Scholar]
- 9. Draper D, Castro J, Feland B, Schulthies S, Eggett D. Shortwave diathermy and prolonged stretching increase hamstring flexibility more than prolonged stretch alone. J Orthop Sports Phys Ther. 2004;34:13-20 [DOI] [PubMed] [Google Scholar]
- 10. Drillis R, Contini R. Body Segment Parameters. New York, NY: Office of Vocational Rehabilitation; 1966. Report No. 1166-03 [Google Scholar]
- 11. Elhorn A, Sawyer M. The problem knee: soft tissue consideration. In: Engle R, ed. Knee Ligament Rehabilitation. New York, NY: Churchill Livingstone; 1991:197-212 [Google Scholar]
- 12. Glasgow C, Wilton J, Tooth L. Optimal daily total end range time for contracture: resolution in hand splinting. J Hand Ther. 2003;16:207-218 [DOI] [PubMed] [Google Scholar]
- 13. Hepburn G. Case studies: contracture and stiff joint management with Dynasplint. J Orthop Sports Phys Ther. 1987;8:498-504 [Google Scholar]
- 14. Johnson A, Godges J, Zimmerman G, Ounanian L. The effect of anterior versus posterior glide joint mobilization on external rotation range of motion in patients with shoulder adhesive capsulitis. J Orthop Sports Phys Ther. 2007;37(3):88-99 [DOI] [PubMed] [Google Scholar]
- 15. Lentell G, Hetherington T, Eagan J, Morgan M. The use of thermal agents to influence the effectiveness of a low-load prolonged stretch. J Orthop Sports Phys Ther. 1992;16(5):200-207 [DOI] [PubMed] [Google Scholar]
- 16. Light K, Nuzik S, Personius W, Barstrom A. Low-load prolonged stretch vs high-load brief stretch in treating knee contractures. Phys Ther. 1984;64(3):330-333 [DOI] [PubMed] [Google Scholar]
- 17. McClure P, Blackburn L, Dusold C. The use of splints in the treatment of joint stiffness: biologic rationale and an algorithm for making clinical decisions. Phys Ther. 1994;74:1101-1107 [DOI] [PubMed] [Google Scholar]
- 18. McDowell M, Fryar C, Ogden C, Flegal K. Anthropometric Reference Data for Children and Adults: United States, 2003-2006. Hyattsville, MD: National Center for Health Statistics; 2008. Report No. 10 [PubMed] [Google Scholar]
- 19. Moseley A, Herbert R, Nightingale E, et al. Passive stretching does not enhance outcomes in patients with plantarflexion contracture after cast immobilization for ankle fracture: a randomized controlled trial. Arch Phys Med Rehabil. 2005;86:1118-1126 [DOI] [PubMed] [Google Scholar]
- 20. Neviaser J. Adhesive capsulitis of the shoulder: a study of the pathological findings in periarthritis of the shoulder. J Bone Joint Surg Am. 1945;27:211-222 [Google Scholar]
- 21. Pouliart N, Somers K, Eid S, Gagey O. Variations in the superior capsuloligamentous complex and description of a new ligament. J Shoulder Elbow Surg. 2007;16:821-836 [DOI] [PubMed] [Google Scholar]
- 22. Prosser R. Splinting in the management of proximal interphalangeal joint flexion contracture. J Hand Ther. 1996;9:378-386 [DOI] [PubMed] [Google Scholar]
- 23. Steffen T, Mollinger L. Low-load, prolonged stretch in the treatment of knee flexion contractures in nursing home residents. Phys Ther. 1995;75:886-897 [DOI] [PubMed] [Google Scholar]
- 24. Stephenson J, Quimbo R, Gu T. Knee-attributable medical costs and risk of re-surgery among patients utilizing non-surgical treatment options for knee arthrofibrosis in a managed care population. Curr Med Res Opin. 2010;26(5):1109-1118 [DOI] [PubMed] [Google Scholar]
- 25. Uhl T, Jacobs C. Torque measures of common therapies for the treatment of flexion contractures. J Arthroplasty. 2011;26(2):328-334 [DOI] [PubMed] [Google Scholar]
- 26. Uhthoff H, Boileau P. Primary frozen shoulder: a global capsular stiffness versus localized contracture. Clin Orthop Relat Res. 2007;456:79-84 [DOI] [PubMed] [Google Scholar]
- 27. Unterhauser F, Bosch U, Zeichen J, Weiler A. α-Smooth muscle actin containing contractile fibroblastic cells in human knee arthrofibrosis tissue. Arch Orthop Trauma Surg. 2004;124:585-591 [DOI] [PubMed] [Google Scholar]
- 28. van Grinsven S, van Cingel R, Holla C, van Loon C. Evidence-based rehabilitation following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2010;18:1128-1144 [DOI] [PubMed] [Google Scholar]
- 29. Wilk K, Macrina L, Reinhold M. Rehabilitation following microfracture of the knee. Cartilage. 2010;1(2):96-107 [DOI] [PMC free article] [PubMed] [Google Scholar]


