Abstract
Background:
Hamstring muscle strains represent a common and disabling athletic injury with variable recurrence rates and prolonged recovery times.
Objectives:
To present the outcomes of a novel rehabilitation protocol for the treatment of proximal hamstring strains in an intercollegiate sporting population and to determine any significant differences in the rate of reinjury and time to return to sport based on patient and injury characteristics.
Study Design:
Retrospective case series.
Methods:
A retrospective review was performed of 48 consecutive hamstring strains in intercollegiate athletes. The rehabilitation protocol consisted of early mobilization, with flexible progression through supervised drills. Athletes were allowed to return to sport after return of symmetrical strength and range of motion with no pain during sprinting. Primary outcomes included time to return to sport and reinjury rates.
Results:
All patients returned to their sports, and 3 sustained repeat hamstring strains (6.2% reinjury rate) after a minimum follow-up of 6 months. The average number of days missed from sport was 11.9 (range, 5-23 days). There was no statistically significant difference for time to return to sport between first-time and recurrent injuries and between first- and second-degree injuries (P > 0.05).
Conclusions:
Grade I and II hamstring strains may be aggressively treated with a protocol of brief immobilization followed by early initiation of running and isokinetic exercises—with an average expected return to sport of approximately 2 weeks and with a relatively low reinjury rate regardless of injury grade (I or II), injury characteristics (including first-time and recurrent injuries), or athlete characteristics.
Keywords: hamstring muscle, injury, athletes, rehabilitation, return to sports
Hamstring strains are the most common muscle strains associated with competitive sports.5,10,12 Accounting for 13% of injuries in Australian Rules football,9 they are the second-most-common injury sustained during National Football League training camp.11 In addition to rugby and football players, athletes in soccer, track, and dancing are prone to hamstring injuries.3,5,9-11 Unfortunately, hamstring strains pose a significant challenge not only because of their high incidence but also because of their traditionally slow healing rate, persistence of symptoms, and high incidence of recurrence.14
Hamstring strains generally occur while sprinting or jumping. The semimembranosus and semitendinosus muscles are typically injured during the late swing phase while they eccentrically contract to slow knee extension.12,21 Injury to the biceps femoris, the most commonly injured hamstring muscle, occurs more often in early toe-off.3
Many aspects of hamstring rehabilitation are still debated—from the time of immobilization, if any, to the appropriate timing and mixture of concentric, eccentric, and isometric exercise.6,14,20 The present rehabilitation program emphasizes early motion and a sustained static elevated stretch technique, with a return to sport based in part on pain-free completion of a specific running drill.
Methods
After institutional review board approval, a review was performed of existing data from all patients who sustained a hamstring strain from 2006 to 2008. All athletes in the study presented within 24 hours of the onset of posterior thigh pain while playing a sport, usually involving high-speed running. A diagnosis of a hamstring strain was based on sudden posterior thigh pain while running or jumping, physical disability, pain with resisted prone knee flexion, and tenderness to palpation of the muscle-tendon unit of the hamstring.6,14 The injury was graded according to injury severity. Grade I injuries are mild, grade II moderate, and grade III severe8 (Table 1). Grade I and II injuries were classified by the amount of pain, loss of motion, and manual strength testing on presentation and during physical examination. The specific hamstring muscle injured (semimembranosus, semitendinosus, biceps) was determined on manual muscle testing during the physical examination. Additionally, the athlete identified which muscle was most tender on palpation.
Table 1.
Muscle injury classification system.
| Grade | Pathophysiology | Signs and Symptoms |
|---|---|---|
| I | Tearing of only a few muscle or tendon fibers | Minor swelling and discomfort with no or minimal loss of strength |
| II | More severe partial tear without complete disruption of the musculotendinous unit | Clear loss of strength with more discomfort |
| III | Complete rupture of the musculotendinous unit | A total lack of muscle function and commonly with massive hematoma |
After initial diagnosis, the athlete had a 5-in. foam pad placed over the posterior thigh, secured in place by an Ace wrap, providing compression to both the injured muscle and the surrounding tissue. The athlete was then placed in a knee immobilizer locked in extension and could bear weight as tolerated. The knee immobilizer was initially used to prevent the athlete from “toe walking” and then as an attempt to limit muscle spasms. The knee immobilizer was removed after 24 hours (day 2), but the pad and Ace wrap were kept in place. Rest, ice, compression, and elevation were strictly adhered to for the first 24 hours. Additionally, no nonsteroidal anti-inflammatory drugs were used for the first 48 hours, with acetaminophen (Tylenol) as needed for pain control. With the knee immobilizer removed on day 2, the athlete was allowed to go for a self-paced run until fatigued, typically 1 mile, with ice applied to the posterior thigh at the completion of exercise for approximately 40 minutes (the athlete was allowed to walk to class with ice bag in place). All athletes, regardless of grade of injury (I or II), followed the same rehabilitation protocol.
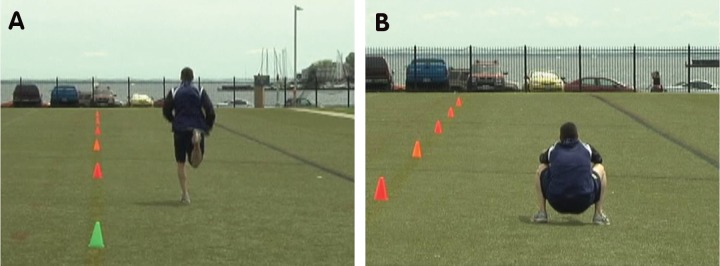
On day 3, the athlete initiated the run protocol (Table 2), which included plyometric exercises such as “butt kickers” and tuck jumps (Figure 1). All other plyometric exercises were closed chain exercises, including single-leg hops, “kangaroo hops,” and tuck jumps. The athletic trainer explained and demonstrated the drills and told the athletes that they should not experience any sharp pains during the drills (pain factor of 1 or 2 of 10). If they did feel a sharp pain, the intensity was decreased, although the activity was not terminated. Drills included retro running (running backward) utilizing 6-in. orange agility cones placed at 10-yd intervals. The athlete was given rest periods between each drill until normal breathing was recovered, which varied per each athlete’s level of fitness. While pain was a limiting factor, it was important to keep the athletes active and drive them to their full potential. All drills and exercises were monitored with direct daily supervision. The athlete’s progress through the flexible protocol was not based on time but on pain-free completion of drills.
Table 2.
Hamstring rehabilitation protocol.
| Time | Details |
|---|---|
| Immediately postinjury | Place 5-in. foam pad over site and snug Ace wrap, knee immobilizer for 24-hour period |
| Day 2 | Leave Ace wrap and pad in place, go for jog until fatigued (approx 1 mile), ice bag × 40 minutes |
| Day 3 | Start run protocol |
| Bike warm-up × 5 minutes | |
| Butt kickers: down and back to 50-yd cone | |
| Carioca run: down and back to 50-yd cone | |
| Cone drills (retro runs): Sprint backward to each cone, jog home Sprint backward to each cone, sprint home Sprint backward, clap hand, 180° turn, sprint to each cone, jog home Arm wave drills—forward/backward/lateral sprints (quick transition) Cones done in sequence No sharp pains—pain factor of 1 or 2 out of 10 |
|
| Jumps: tuck/kangaroo hops | |
| Stair-bounding drills: affected leg only, single steps | |
| Bounding drills (plyometrics): interspersed between backward sprints, affected leg only | |
| Extra drills: Stool = secretary stool; pull with affected leg to cone 5, turnaround, and pull back to home × 2; minimum of 40 yd each way (own pace) | |
| Eccentric exercises: 3× per week starting after day 7; two sets of 10 each | |
| Isokinetics: starting after day 7; 300/300 degrees per second × 90-second run, rest—then power/speed: 90/90, 180/180, 240/240, 120/120 degrees per second (15 seconds each), 300 degrees per second until burnout; continue for 2 more weeks postrehabilitation to power up | |
| Run: At 1-2 weeks postinjury; plastic-wrap the hamstring (spica type) over underwear; athlete can do 4 to 6 rolling start sprints (100 yd) at 90% to 95% effort; then ice bag postexercise for 40 minutes | |
| Exercise | Details |
| Cone drills | Place cones at start, 10, 20, 30, 40, and 50 yd; always face instructor Sprint 1: All retro runs—backward to each cone in succession, jog home Sprint 2: Sprint backward, quick stop, sprint home—no rest between Sprint 3: Sprint backward toward first cone, instructor claps hand—athlete must do 180° turn to finish cone; each cone is done in succession Sprint 4: Arm wave drill—just like football drills; fast transition between forward/lateral/backward (mix it up) Stretch before each sprint |
| Butt kickers | Jog at own pace with heels hitting butt each step |
| Jumps | Tuck jumps: Jump out as far as one can, land in full squat to absorb impact, rise slowly to full standing position, continue 8 down and 8 back |
| Kangaroo hops | Short hops to simulate a kangaroo, uninterrupted, 15 down and 15 return home |
| Bounding drill | Just as track athletes do, affected leg only; 8-15 steps down and back |
| Hamstring stretch | Important: Minimum height is 48 to 60+ in. (progressive daily) from the floor, holding the stretch 60 to 90 seconds; do this between each drill; release from stretch slowly in stages to prevent a rubber band effect—pain-free |
| Rest | Athlete gets a rest period to recover normal breathing as needed; keep the athlete active; drive him or her to full potential |
Figure 1.
Plyometric exercises: A, “butt kickers”—the athlete jogs at one’s own pace, with heels hitting butt each step; B, tuck jumps—athlete jumps out as far as he or she can, lands in full squat to absorb impact, rises slowly to full standing position, then repeats.
A progressive static elevated stretching technique was also initiated on postinjury day 2, starting approximately 48 in. from the floor, adjusting for the athlete’s height and flexibility as needed. A handrail in stadium bleachers was used to stretch (Figure 2). We believe that, in contrast to a traditional toe-touch stretch, performing an elevated stretch prevents the hips from flexing, allowing a simultaneous effect on the muscle origin and insertion. The elevated stretch should be maintained for 60 to 90 seconds, usually after each drill or exercise. The stretch was progressively increased to ≥ 60 in. (from the floor), if possible, by the end of the protocol. During the stretch, the foot was rotated so that the heel pointed to the involved muscle (eg, biceps femoris—heel points laterally), forcing healing tissue to elongate adjacent to the muscle fiber.6
Figure 2.

Static elevated hamstring stretch technique.
Eccentric exercises were started on postinjury day 6 and performed 3 times per week. With the athlete prone on the training table, knees slightly off the edge, 2 sets of resisted extension were performed, 10 repetitions each: the first set acting as a learning curve, the second set providing the desired level of activity (3 sets result in too much soreness to participate the next day).
Isokinetic rehabilitation was also started on postinjury day 6 using 2 exercise techniques:
High speed: 300/300 degrees per second for a 90-second run, then rest for 90 seconds
Power/speed: 90/90, 180/180, 240/240, 120/120 degrees per second (15 seconds each), then 300/300 degrees per second to burnout (determined strictly by fatigue)
Isokinetics were maintained for a 2-week period post-rehabilitation until strength testing was equivalent between injured and uninjured legs and the athlete was able to do full sprints with no residual soreness.
Rolling start sprints were initiated when the athlete was completing drills at a full sprint and felt that he or she was performing at 90% speed. This unique running drill has a 10-yd buildup to speed and a 10-yd coast to a jog. Athletes typically started on postinjury day 7. This was used to determine if the athlete could return to sports. Sprints were performed at a 90% to 95% effort. After all sessions of training, the athlete iced the posterior thigh for 40 minutes.
Athletes returned to sports when they perceived equivalent hamstring function and strength between injured and uninjured legs (Cybex II + Isokinetic Dynamometer, Ronkonkoma, New York) and remained pain-free during all drills, including rolling sprints. On return to respective sports, athletes were monitored with a software tracking system (Sportsware Injury Tracking Software, CSMi, Stoughton, Massachusetts) for recurrence. All recurrent injuries were confirmed by repeat examination.
Days to return to sport were compared on the basis of injury location (biceps vs semimembranosus), injury type (primary vs recurrent), age, sex, sport, side, and degree of injury. Mean and median time to return to sport were calculated using the Kaplan-Meier method and compared using log rank tests. Cox proportional hazard regression was used to identify independent associations with time to return to sport, after adjusting for other variables.
Results
Data were available for review from 48 athletes, from 14 sports, with acute hamstring strains. Athletes participated in levels of sport ranging from recreational to division I collegiate. All participants were division I athletes; however, some of the sports they were participating in at time of injury were recreational. Most of the injuries came from track and football (16 and 12, respectively). There were 40 men and 8 women. Twenty-six injuries were left-sided and 22 injuries were right-sided. Of note, there were no semitendinosus strains identified (Table 3).
Table 3.
Time to return to sports (first-time and recurrent injuries).
| Athletes, No. | Return to Sports, Mean (SE) | Pa | |
|---|---|---|---|
| Site | |||
| Biceps | 25 | 12.24 (0.69) | 0.77 |
| Semimembranosus | 20 | 11.50 (0.78) | |
| Not specified | 3 | ||
| Degree | |||
| First | 30 | 11.23 (0.64) | 0.32 |
| Second | 18 | 13.06 (0.79) | |
| Sport | |||
| Football | 12 | 11.83 (0.82) | 0.16 |
| Lacrosse | 7 | 14.29 (1.71) | |
| Rugby | 9 | 9.89 (1.20) | |
| Track | 16 | 11.69 (0.86) | |
| Other | 4 | 13.50 (0.65) | |
| Side | |||
| Right | 22 | 11.46 (0.58) | 0.09 |
| Left | 26 | 12.31 (0.80) | |
| Sex | |||
| Male | 40 | 11.93 (0.58) | 0.98 |
| Female | 8 | 11.88 (1.08) | |
| Recurrent | |||
| Primary | 25 | 12.17 (0.58) | 0.78 |
| Recurrent | 23 | 11.57 (0.88) | |
| Age, y | |||
| 18-20 | 30 | 11.37 (0.58) | 0.35 |
| 21-25 | 17 | 12.59 (0.96) | |
Log rank test.
There was an even distribution of first-time and recurrent injuries, with 23 recurrent and 25 first-time injuries. The degree of injury was limited to 30 first- and 18 second-degree strains. All patients returned to their sports, and 3 of the 48 athletes in the study experienced reinjury (6.2%); minimum follow-up was 6 months. All 3 reinjuries were to the biceps, and 2 of 3 reinjuries followed a primary injury. The average number of days from injury to return to competition was 11.9 (range, 5-23 days). Range of motion postrehabilitation for the injured leg showed an average increase of 21.3° (range, 0°-43°).
There was no statistically significant difference between time to return to sport between first-time injuries and recurrent injuries or by injury location (biceps vs semimembranosus), injury type (primary vs recurrent), age, sex, sport, side, or degree of injury (P > 0.05; Table 3). None of the variables were significantly associated with time to return to sport in a Cox regression model that included all 7 variables.
Discussion
The goal of any hamstring rehabilitation is to return the athlete to sport at the previous level of performance while attempting to minimize the rate of injury recurrence. This rehabilitation protocol allows for early mobilization after initial injury, with a combination of drills and stretches that are supervised to ensure that the athletes progress but only while experiencing minimal pain. The timeline is flexible, and the criteria for return to play are multifactorial. Previous studies showed that despite knee and hip flexion strength of more than 90%, athletes were not ready to return to sports.2 The combination of strength and flexibility, in addition to completion of pain-free rolling start sprints, was successful in this population.
These patients missed similar time from sports (5-23 days) compared with previous data (8-25 days).4 The most striking difference seen in this study was the relatively low reinjury rate, 6.2%, at 6-month follow-up. Previous series had reinjury rates of 30.6% within 2 weeks of return to sports.22 A prospective randomized trial23 of progressive agility drills with static strengthening and stretching alone showed a lower reinjury rate for the agility group (7.7% vs 70%). One major difference with that agility program was the initial limitation of early range of motion.
Immobilization immediately postinjury has 2 distinct advantages. The pad and Ace wrap serve to limit capillary bleeding.1 The knee immobilizer prevents the slight knee flexion and toe walk caused by protective muscle spasm so often seen in hamstring strains, thereby helping to limit disability. Additionally, placing the injured extremity at rest immediately posttrauma prevents further retraction of the ruptured muscle stumps and reduces the size of the hematoma and, subsequently, the size of the connective tissue.20 Immobilization also appears to provide the new granulation tissue with the needed tensile strength to withstand the forces created by muscle contraction.16-18,20
While a brief period of immobilization is beneficial, prolonged immobilization can be detrimental to the recovery process. Research has shown that early mobilization induces rapid and intense capillary ingrowth, regeneration of muscle fibers, and parallel orientation of regenerating myofibers in comparison with immobilization.16-18,20 Active movement after a short period of immobilization enhances the penetration of muscle fibers through connective tissue, limits permanent scarring, and facilitates alignment and strength of regenerating muscle fibers.16-18,20
Scar tissue matrix formation starts20 at day 2 or 3 and is fully developed by day 7. At day 10, it is no longer the weakest link; muscle is, when loaded to failure.16-18,20 Initiating static elevated stretching early encourages elongation of the maturing scar while it is still plastic, after it has developed strength to prevent retraction of the muscle.13,20 During the remodeling phase of rehabilitation, stretching determines the stress lines along which collagen will be oriented.7,20 If tensile strength is not regained, prolonged pain, limited function, and increased susceptibility to tissue injury can be expected.7
Early concentric, eccentric, and isokinetic exercise starting postinjury (day 2) helps prevent reduction in strength and muscle imbalances without adversely affecting the healing tissue.23 The incorporation of plyometrics and agility drills increases hamstring peak torque and improves hamstring:quadriceps ratios.7,15
While there is no clearly defined length of initial immobilization, most agree that it should be limited to no more than 1 week,19 with a graduated return to strengthening exercise.24 This protocol uses a brief period of immobilization (24 hours), with return to isokinetic strengthening by day 6 and initiation of rolling start sprints by day 7 (on average).
An inherent weakness of the study is that there is no control rehabilitation program. Another weakness is the lack of imaging to confirm hamstring injury and severity.6 And another is the applicability to only grade I and II hamstring strains. Certainly the intensity and timing of the protocol will have to be adjusted when treating a grade III strain.
Conclusions
The combination of 24 hours of immobilization with early initiation of a sustained static elevated stretch technique, with progression to on-the-field drills for concentric, eccentric, and isometric loading of the injured muscle, allows for a fast rate of recovery and maintenance of muscle strength in this athletic cohort with grade I and II hamstring strains. Rolling sprints are a critical factor in ensuring that the athlete meets functional criteria to return to play. This protocol may be an effective means to return athletes with primary or recurrent grade I and II biceps and semimembranosus strains to play in less than 2 weeks with a low risk for injury recurrence.
Footnotes
The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Department of the Army, the Department of the Navy, Department of Defense, or the US government.
References
- 1. Aronen JG, Garrick JG, Chronister RD, McDevitt ER. Quadriceps contusions: clinical results of immediate immobilization in 120 degrees of knee flexion. Clin J Sport Med. 2006;16:383-387 [DOI] [PubMed] [Google Scholar]
- 2. Askling C, Saartok T, Thorstensson A. Type of acute hamstring strain affects flexibility, strength, and time to return to pre-injury level. Br J Sports Med. 2006;40:40-44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Askling CM, Tengvar M, Saartok T, Thorstensson A. Acute first-time hamstring strains during high-speed running: a longitudinal study including clinical and magnetic resonance imaging findings. Am J Sports Med. 2007;35:197-206 [DOI] [PubMed] [Google Scholar]
- 4. Brooks JH, Fuller CW, Kemp SP, Reddin DB. Incidence, risk, and prevention of hamstring muscle injuries in professional rugby union. Am J Sports Med. 2006;34:1297-1306 [DOI] [PubMed] [Google Scholar]
- 5. Brubaker CE, James SL. Injuries to runners. J Sports Med. 1974;2:189-198 [DOI] [PubMed] [Google Scholar]
- 6. Clanton TO, Coupe KJ. Hamstring strains in athletes: diagnosis and treatment. J Am Acad Orthop Surg. 1998;6:237-248 [DOI] [PubMed] [Google Scholar]
- 7. Comfort P, Green CM, Matthews MJ. Training considerations after hamstring injury in athletes. Strength Cond J. 2009;31:68-73 [Google Scholar]
- 8. Craig T, ed. Comments in Sports Medicine. Chicago, IL: American Medical Association; 1973 [Google Scholar]
- 9. Dadebo B, White J, George KP. A survey of flexibility training protocols and hamstring strains in professional football clubs in England. Br J Sports Med. 2004;38:388-394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ekstrand J, Gillquist J. Soccer injuries and their mechanisms: a prospective study. Med Sci Sports Exerc. 1983;15:267-270 [DOI] [PubMed] [Google Scholar]
- 11. Feeley BT, Kennelly S, Barnes RP, et al. Epidemiology of National Football League training camp injuries from 1998 to 2007. Am J Sports Med. 2008;36:1597-1603 [DOI] [PubMed] [Google Scholar]
- 12. Garrett WE., Jr. Muscle strain injuries. Am J Sports Med. 1996;24(6)(suppl):S2-S8 [PubMed] [Google Scholar]
- 13. Goldspink G. Changes in muscle mass and phenotype and the expression of autocrine and systemic growth factors by muscle in response to stretch and overload. J Anat. 1999;194(pt 3):323-334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Heiderscheit BC, Sherry MA, Silder A, Chumanov ES, Thelen DG. Hamstring strain injuries: recommendations for diagnosis, rehabilitation, and injury prevention. J Orthop Sports Phys Ther. 2010;40:67-81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Heidt RS, Jr, Sweeterman LM, Carlonas RL, Traub JA, Tekulve FX. Avoidance of soccer injuries with preseason conditioning. Am J Sports Med. 2000;28:659-662 [DOI] [PubMed] [Google Scholar]
- 16. Jarvinen M. Healing of a crush injury in rat striated muscle: 2. A histological study of the effect of early mobilization and immobilization on the repair processes. Acta Pathol Microbiol Scand A. 1975;83:269-282 [PubMed] [Google Scholar]
- 17. Jarvinen M. Healing of a crush injury in rat striated muscle: 3. A micro-angiographical study of the effect of early mobilization and immobilization on capillary ingrowth. Acta Pathol Microbiol Scand A. 1976;84:85-94 [PubMed] [Google Scholar]
- 18. Jarvinen M. Healing of a crush injury in rat striated muscle: 4. Effect of early mobilization and immobilization on the tensile properties of gastrocnemius muscle. Acta Chir Scand. 1976;142:47-56 [PubMed] [Google Scholar]
- 19. Jarvinen MJ, Lehto MU. The effects of early mobilisation and immobilisation on the healing process following muscle injuries. Sports Med. 1993; 15:78-89 [DOI] [PubMed] [Google Scholar]
- 20. Jarvinen TA, Jarvinen TL, Kaariainen M, Kalimo H, Jarvinen M. Muscle injuries: biology and treatment. Am J Sports Med. 2005;33:745-764 [DOI] [PubMed] [Google Scholar]
- 21. Orchard J. Biomechanics of muscle strain. New Zealand J Sports Med. 2002;30:92-98 [Google Scholar]
- 22. Orchard J, Best TM. The management of muscle strain injuries: an early return versus the risk of recurrence. Clin J Sport Med. 2002;12:3-5 [DOI] [PubMed] [Google Scholar]
- 23. Sherry MA, Best TM. A comparison of 2 rehabilitation programs in the treatment of acute hamstring strains. J Orthop Sports Phys Ther. 2004;34:116-125 [DOI] [PubMed] [Google Scholar]
- 24. Worrell TW. Factors associated with hamstring injuries: an approach to treatment and preventative measures. Sports Med. 1994;17:338-345 [DOI] [PubMed] [Google Scholar]