Abstract
Context:
Low back pain (LBP) is a prevalent condition imposing a large socioeconomic burden. Despite intensive research aimed at the efficacy of various therapies for patients with LBP, most evidence has failed to identify a superior treatment approach. One proposed solution to this dilemma is to identify subgroups of patients with LBP and match them with targeted therapies. Among the subgrouping approaches, the system of treatment-based classification (TBC) is promoted as a means of increasing the effectiveness of conservative interventions for patients with LBP.
Evidence acquisition:
MEDLINE and PubMed databases were searched from 1985 through 2010, along with the references of selected articles.
Results:
TBC uses a standardized approach to categorize patients into 1 of 4 subgroups: spinal manipulation, stabilization exercise, end-range loading exercise, and traction. Although the TBC subgroups are in various stages of development, recent research lends support to the effectiveness of this approach.
Conclusions:
While additional research is required to better elucidate this method, the TBC approach enhances clinical decision making, as evidenced by the improved clinical outcomes experienced by patients with LBP.
Keywords: low back pain, classification, decision making, exercise, manual therapy
Low back pain (LBP) is a common and costly complaint, with the point prevalence ranging from 12% to 33%, the 1-year prevalence from 22% to 65%, and the lifetime prevalence from 11% to 84%.113 Estimates of the economic costs in different countries vary greatly but must be considered a substantial burden on society.31 In the United Kingdom each year, the National Health Service physiotherapy and hospital costs directly related to LBP are £150.6 million and £512 million, respectively.94 Thirteen percent of all unemployed people reported that LBP was the reason that they were not working.36 In the United States, $26 billion per year in health care expenses were directly attributable to treating LBP. Individuals with LBP incur health care expenditures about 60% higher than those without back pain.83 In Australia, the estimated direct and indirect cost of LBP in 2001 was A$9.17 billion.114
Chronic LBP is a disabling condition and is particularly costly to individuals and the community.30 In the majority of those presenting with acute LBP, the cause of pain is thought to be nonspecific and possibly caused by a variety of etiologies.74 Serious underlying conditions are rare.72 While risk factors for LBP are multidimensional, with physical attributes, socioeconomic status, general medical health, psychological status, and environmental factors all contributing.99
Clinical experience often leads health care providers to believe that manual, exercise, and traction therapies are effective for patients with LBP. Unfortunately, evidence for the effectiveness of these therapies remains suboptimal. While studies have described benefit from a broad range of physical and pharmacologic interventions when compared with natural history or placebo therapies, these benefits have small effect sizes, with only small differences in outcome observed when alternative therapies are compared.24,101,111,112 This understanding can lead to the mistaken impression among clinicians and policy makers that there are no effective or efficient treatment options for patients with LBP. The objective of this review is to discuss the elements of current research that may partly explain why this is so and to summarize and update one approach to LBP classification.
Subgrouping Strategies and Treatment-Based Classification
The apparent lack of treatment effect mentioned above may be partly due to the tendency of researchers to treat nonspecific LBP as one homogenous condition, rather than a heterogeneous collection of differing conditions that may preferentially respond to different treatments.58 Many different methods of subgrouping patients have been developed over the past century. Traditional subgrouping strategies are based on pathoanatomy and have failed to establish relationships between pathology and symptoms.1,37 An alternative approach is to classify patients into clinically relevant subgroups.15,63 One method of classification involves the identification of unique patient attributes that allow patients to be matched to the most appropriate therapeutic approach.35,89,92,115 This review focuses on one of these approaches: the system of treatment-based classification (TBC), as first described by Delitto et al.35,48,61
The TBC approach involves a stepwise process of clinical decision making (Figure 1). Patients with LBP are first screened for signs of serious pathology and the presence of biopsychosocial “yellow flags.” Next, information from their history and physical examination is used to match their clinical presentation to the most appropriate therapy, by placing them into a treatment subgroup named for the primary therapy employed: spinal manipulation, stabilization exercise, end-range loading exercise, and traction.
Figure 1.
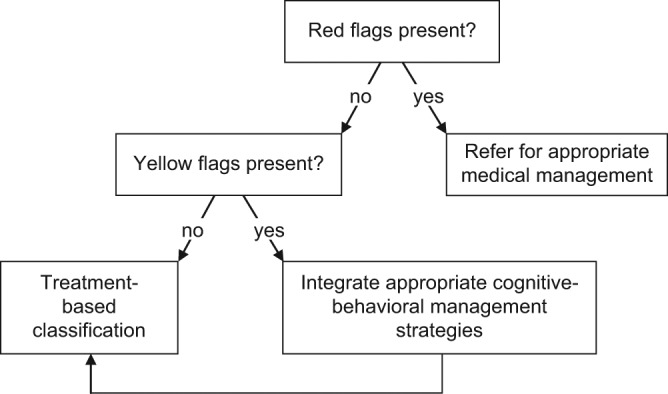
Stepwise decision-making process for patients with low back pain assessed using treatment-based classification.
Treatment Subgroups
Spinal Manipulation Subgroup
Spinal manipulation has been used for centuries and remains one of the most common treatments for LBP.43 As spinal manipulation can result in rapid clinical benefit in some individuals23,44 and can be applied very quickly with little to no equipment, its use in athletes is especially appealing. The safety of spinal manipulation has generated a great deal of discussion and inquiry. Benign, self-limiting adverse events such as short-term soreness following spinal manipulation are common8,21,81; however, serious adverse events are rare.5,57 Therefore, spinal manipulation is considered a safe therapeutic option for the patient with LBP.100
The mechanism by which spinal manipulation exerts its clinical effects has also been the subject of much debate and investigation.12,14,39 Traditional theory has emphasized the restoration of joint motion and/or correction of biomechanical misalignment.56,85,90 More recent evidence suggests a primarily neurophysiologic effect on pain perception and muscle function.12,13,77
Evidence for the efficacy of spinal manipulation for LBP has been mixed. While multiple trials and systematic reviews support its efficacy,18,19,112 others do not.6,40 The conflicting results and small effect sizes found in many trials may stem from the treatment of heterogeneous back pain as though it arises from a common cause.34 In other words, while spinal manipulation may be an effective treatment option for some patients with LBP, not all patients will benefit from this therapy.
Initially, the spinal manipulation subgroup was identified by proponents of TBC using a traditional biomechanical paradigm in which manipulation was indicated in the presence of lumbosacral asymmetries and/or “capsular patterns” of facet joint motion restriction.35 To more objectively define this subgroup, Flynn et al44 derived a clinical prediction rule (CPR) that identifies people likely to experience clinical success from spinal manipulation. Two sessions of lumbopelvic manipulation (Figure 2) were applied to 71 consecutive patients with nonradicular low back pain. Clinical success was defined as a 50% improvement in Oswestry Disability Index score, which reflects a significant improvement in clinical status.50 Five factors from the history and physical examination predicted clinical success at 1 week (Table 1). Overall, just under half the patients experienced clinical success with spinal manipulation. However, the probability of experiencing clinical success increased to 95% when patients met at least 4 of 5 criteria from the history and physical examination.
Figure 2.

Supine lumbopelvic spinal manipulation technique.
Table 1.
Treatment-based classification subgroups with identification criteria and treatment approaches for patients with low back pain.a
| Subgroup Criteria | Treatment Approach |
|---|---|
| Manipulation subgroup | |
| No symptoms distal to knee Duration of symptoms < 16 days Lumbar hypomobility FABQW < 19 Hip internal rotation ROM > 35° |
Manipulation techniques for the lumbopelvic region Active lumbar ROM exercises |
| Stabilization subgroup | |
| Age (< 40 years) Average SLR ROM (> 91°) Aberrant movement present FABQW < 19 Positive prone instability test |
Exercises to strengthen large spinal muscles (eg, erector spinae, oblique abdominals) Exercises to promote contraction of deep spinal muscles (eg, lumbar multifidus, transversus abdominis) |
| End-range loading exercise subgroup | |
| Extension | |
| Symptoms distal to the buttock Symptoms centralize with lumbar extension Symptoms peripheralize with lumbar flexion Directional preference for extension |
End-range extension exercises Mobilization to promote extension Avoidance of flexion activities |
| Flexion | |
| Older age (> 50 years) Directional preference for flexion Imaging evidence of lumbar spine stenosis |
End-range flexion exercises Mobilization or manipulation of the spine and/or lower extremities Exercise to address impairments of strength or flexibility Body weight–supported ambulation |
| Traction subgroup | |
| Symptoms extend distal to the buttock(s) Signs of nerve root compression are present Peripheralization with extension movement OR positive crossed SLR test is present |
Prone mechanical traction Extension specific exercise activities |
FABQW, Fear-Avoidance Beliefs Questionnaire–Work subscale; ROM, range of motion; SLR, straight-leg raise. Adapted with permission from Hebert et al.61
Subsequent work has supported the validity of the CPR. A multicenter randomized controlled trial23 found that patients who were positive on the CPR and received spinal manipulation and stabilization exercise were more likely to experience clinical success than patients who were CPR positive and received stabilization exercise only or were CPR negative and received stabilization exercise with or without spinal manipulation. The clinical benefit of receiving matched treatment (ie, spinal manipulation and CPR positive) persisted for 6 months. This suggests that the CPR criteria can identify those individuals with LBP who benefit from spinal manipulation, not just those patients who have a favorable prognostic course. Therefore, the utilization of this CPR appears to enhance clinical decision making for patients with LBP.
Subsequent research has examined the generalizability of the CPR to the use of other manual therapy approaches. These studies suggest that this subgroup of patients respond equally well to other manipulative thrust techniques (Figure 3)27,106 but not to nonthrust mobilization techniques.27,59
Figure 3.

Side-lying lumbopelvic spinal manipulation technique.
All together, these studies suggest that (1) the identification of the proper patient subgroup is more important to a successful outcome than choosing the right manipulative technique and (2) the application of spinal manipulation based solely on a paradigm of biomechanical faults and/or spinal misalignments is inappropriate.
Stabilization Subgroup
Spinal instability is a theorized mechanism of LBP used to justify therapies from exercise to surgical fusion.53,93,103 Recent research into lumbar spine stability has emphasized the morphology and function of the trunk musculature. In asymptomatic individuals, some trunk muscles (eg, transversus abdominis, lumbar multifidus) contract in anticipation of extremity movement.3,70,86 This feedforward behavior is disturbed in individuals with LBP, with delayed transversus abdominis and lumbar multifidus muscle activation.69,71,73,84 Additionally, fatty infiltration76,91 and atrophy7,33,116 of the lumbar multifidus are associated with LBP.
Stabilization exercise can normalize the timing of trunk muscle activation.108,109 Moreover, improved trunk muscle function following a stabilization exercise program is associated with enhanced clinical outcomes.42 It is not known if stabilization exercises can influence the distribution of intramuscular fat within the paraspinal musculature; however, evidence suggests that such programs can reverse lumbar multifidus atrophy among athletic and nonathletic populations.66-68
Research examining the efficacy of stabilization exercise programs for patients with LBP have provided conflicting results.22,29,41,55,65,79 Additionally, there is much debate on the most effective method of stabilization exercise. One method stresses the importance of retraining specific muscles, such as the transversus abdominis and lumbar multifidus,98 while other methods emphasize the general restoration of the strength and endurance of trunk muscles.87
Clinical trials comparing the efficacy of these approaches have reported conflicting results supporting the motor control41,45 and general stabilization approaches.79 Additional research is needed to further elucidate the optimal approach to lumbar stabilization exercise. Despite this, stabilization exercise programs are effective for some patients,55,65,79,95 and the observed treatment effect may be more pronounced with consideration of the proper subgroup of individuals with LBP.64
Hicks and colleagues64 derived a CPR that sought to identify those with LBP most likely to achieve clinical success with an 8-week stabilization exercise program. Four variables relating to clinical outcome were identified (Tables 1 and 2). When 3 variables were present, the probability of achieving clinical success improved from 33% (among unclassified patients) to 67%.
Table 2.
Special examination procedures identifying the stabilization exercise subgroup
| Criterion: Definition of Positive |
|---|
| Aberrant movements |
| The presence of one or more of the following during standing trunk flexion testing: Instability catch: Movement other than in the sagittal plane (eg, lumbar spine rotation or lateral flexion) or a sudden acceleration or deceleration of trunk movement Gower sign: The patient uses his or her hands to push upon the thighs or other surface to assist with the attainment of an erect posture from a flexed posture. Reversal of lumbopelvic rhythm: The patient returns to an erect posture from a flexed position by flexing the knees and translating the pelvis anteriorly. Painful arc of motion: Increased discomfort is experienced during lumbar spine flexion or return from flexion that occurs at a specific point or range and is not present before or after this point. |
| Prone instability test |
| The patient lies prone with his or her trunk on the table and feet on the floor. The clinician manually applies posterior-to-anterior pressure to each lumbar spinous process that results in pain. The patient is then asked to lift his or her feet from the floor, and the process is repeated with the pain relieved at the respective lumbar segment. |
These predictive criteria have yet to undergo validation through the rigors of a randomized trial. However, the construct validity of these variables has been supported through their relationship with lumbar segmental kinematics (aberrant segmental structural integrity, segmental stiffness, and altered neuromuscular control during lumbar spine movement)107 and lower levels of lumbar multifidus activation.62
End-Range Loading Exercise Subgroup
Popularized by McKenzie’s system of mechanical diagnosis and therapy,89 end-range loading exercises are often prescribed for patients with radicular low back pain whose symptoms benefit from end-range postures or movements (eg, lumbar flexion, extension, lateral translation, or combined movements). The prescribed direction of treatment depends on a patient’s response, especially the presence or absence of directional preference or centralization phenomena.
Directional preference describes the clinical situation where movement in one direction improves pain or range of motion and where movement in the opposite direction may cause symptoms to worsen.75 Patients can have a directional preference for flexion, extension, or lateral translation, although extension is the most common.82 While end-range loading exercises may be prescribed in the direction of a patient’s directional preference, advocates of TBC have emphasized the related concept of centralization (Table 1).
Centralization describes the clinical situation where a movement or position results in the migration of symptoms from a more distal/lateral location in the buttocks and/or lower extremity to a more proximal location, closer to the midline of the spine.2 Advocates of TBC have expanded this definition to include the abolishment of distal pain and/or paresthesias.48 Therefore, patients who demonstrate centralization would be considered to have a directional preference, but not all patients that have a directional preference experience centralization.48,119 As with directional preference, treatment recommendations can be dictated by the presence of centralization. For example, patients who centralize with extension may be advised to perform the prone press-up exercise (Figure 4) frequently throughout the day. Additionally, this treatment is often accompanied by manual spinal mobilization into lumbosacral extension (Figure 5) and temporary avoidance of flexion activities (eg, improper bending, slumped sitting) (Table 1).
Figure 4.

Example of an end-range loading exercise into extension: the prone press-up.
Figure 5.

Posterior to anterior mobilization to promote lumbosacral extension.
Centralization is of prognostic importance for patients with LBP.10,54,105,117,118 Moreover, centralization appears to identify the subgroup of patients that require end-range loading exercises. Browder et al20 found that patients with LBP whose symptoms centralized with lumbar extension experienced better clinical outcomes when prescribed extension end-range loading exercises and mobilizations as compared with patients randomized to receive lumbar stabilization exercises. A recent systematic review of the centralization phenomenon concluded with the recommendation that centralization be routinely monitored and used to guide treatment strategies in patients with spinal pain.2
Additional evidence suggests that the directional preference and centralization phenomena may identify the presence of spinal pathology.9,38,80,122 Beattie et al9 investigated the effect of extension-based end-range loading exercises and mobilizations on L5-S1 intervertebral disc hydration among a subgroup of patients with LBP who demonstrated a directional preference for extension. They reported that participants who experienced immediate reductions in LBP following extension exercise (ie, exercise responders) demonstrated increased water diffusion in the L5-S1 intervertebral disc, while nonresponders demonstrated decreased diffusion.
While extension responders form the largest proportion of the end-range loading exercise subgroup, some patients appear to benefit from flexion end-range loading exercises. These patients are often assumed to have spinal stenosis28,46 and improve when flexion exercises are incorporated into a multimodal treatment program.121
The possible associations between centralization, direction preference, and spinal pathoanatomy are an emerging area of study; however, additional research is required to understand these relationships. Nonetheless, it appears that centralization and directional preference are important factors in the evaluation and management of this subgroup of patients with LBP. Current understanding presumes that centralization and/or a directional preference for extension may help to identify patients experiencing discogenic pain, while centralization and/or a directional preference for flexion is most likely associated with spinal stenosis.
Traction
The use of mechanical spinal traction for LBP and other disorders of the lumbar spine has a long history in medicine and continues to be used by clinicians today.104 Yet, clinical trials examining heterogenous populations of individuals with LBP11,16,110,120 have failed to demonstrate the efficacy of mechanical traction, and current treatment guidelines do not support its use.25,102 Most clinicians who recommend traction do so using criteria to identify a more selective group of patients with LBP. Traditionally, these criteria have focused on the presence of sciatica or signs of nerve root compression.60
To better identify these patients, a recent clinical trial examined the characteristics of patients with LBP and sciatica who experienced a favorable clinical response with mechanical traction and extension end-range loading exercises.51 Radicular leg pain and signs of lumbar nerve root compression did not adequately identify this subgroup of patients. Two additional factors were related to clinical outcome: peripheralization with extension movement and a positive crossed straight-leg raise test (Table 1). Peripheralization occurs when a movement or posture causes distal migration of symptoms (eg, lumbar extension causes posterior thigh pain to extend to the dorsal aspect of the foot).61 The crossed straight-leg raise test is deemed positive when the patient’s familiar lower extremity symptoms are reproduced upon passive flexion of the contralateral leg while the knee is fully extended.78 When either factor is present along with radicular leg pain and signs of nerve root compression, patients are more likely to benefit from traction therapy and end-range loading exercises into lumbar extension when compared to extension exercises alone. Ongoing research may well provide additional clarification to these preliminary findings.52
Clinicians use a variety of lumbar traction approaches (or spinal decompression32 approaches). However, no generally accepted traction protocol is available.26 When identifying a traction protocol for the individual patient, clinicians need to consider various factors, including patient positioning (eg, prone or supine), maximal force and force progression, duration of force application, and the inclusion of additional therapies (eg, end-range loading exercise). The protocol used to identify the traction subgroup within TBC involves the static application of high-force traction (between 40% and 60% of body weight) with the patient in the prone position.51
Limitations and Implementation of the Current Model
The subgroups defining the TBC approach were identified through a combination of clinical knowledge and research activity, including the development of CPRs (also known as clinical decision rules). These tools are designed to assist with clinical decision making by statistically combining historical, clinical, laboratory, and/or imaging findings to improve diagnostic accuracy, prognostic understanding, or prediction of therapeutic response.88,96 Within the realm of rehabilitation, CPRs are most commonly used to predict a patient’s treatment response. Specifically, CPRs can be used to identify discrete subgroups of patients who are likely to respond to a particular therapy that would otherwise fall into a broad, homogenous diagnostic category such as LBP.47
The development of CPRs occurs in 3 stages: derivation, validation, and impact analysis.88 CPR derivation studies seek to identify variables with predictive power that may aid clinicians when making decisions about their patients. Validation studies examine the predictive criteria for evidence of reproducible accuracy, while impact analyses investigate the ability of a CPR to change clinician behavior, improve clinical outcomes, and/or cost effectiveness. While it is appropriate for clinicians to use data from derivation studies to inform clinical decision making, CPRs must undergo the rigors of validation prior to confident implementation.88
As we have discussed, the TBC subgroups are each in various stages of development, with corresponding differences in their levels of evidence. This fact requires our attention, as lower levels of evidence are more subject to the dangers of bias and confounding.97 Traditional wisdom tells us that strong evidence of clinical and cost-effectiveness should inform clinical practice. While only one of the treatment subgroups (manipulation) has been validated, the TBC approach as a whole has demonstrated some degree of clinical effectiveness. Fritz et al49 performed a clinical trial comparing the effectiveness of TBC to therapy based on the Agency for Health Policy and Research guidelines for patients with acute LBP. Classified patients experienced greater short-term improvements in LBP-related disability and return-to-work status. Similarly, Brennan and colleagues17 examined the clinical outcomes of patients with LBP who received treatment that was either matched or unmatched according to the TBC subgroups. Patients receiving matched treatment experienced greater improvements in short- and long-term LBP-related disability. Ongoing research efforts should help to inform the cost implications of TBC-informed clinical decision making.4
Conclusions
Subgrouping patients with LBP using the TBC criteria allows for improved identification of those who are most likely to experience clinical success with spinal manipulation, stabilization exercise, end-range loading exercise, and traction therapies. Although each of the 4 TBC subgroups are in various stages of development and validation, current evidence suggests that TBC-informed clinical decision making improves the effectiveness of care provided to patients with LBP. Therefore, TBC can be recommended as an approach for matching patients to the most appropriate therapeutic intervention.
Acknowledgments
We thank Dr Keith Simpson for reviewing a draft of this article. The opinions or assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the US Department of the Army or US Department of Defense
References
- 1. Abenhaim L, Rossignol M, Gobeille D, Bonvalot Y, Fines P, Scott S. The prognostic consequences in the making of the initial medical diagnosis of work-related back injuries. Spine. 1995;20(7):791-795 [DOI] [PubMed] [Google Scholar]
- 2. Aina A, May S, Clare H. The centralization phenomenon of spinal symptoms: a systematic review. ~Man Ther. 2004;9(3):134-143 [DOI] [PubMed] [Google Scholar]
- 3. Allison GT, Morris SL, Lay B. Feedforward responses of transversus abdominis are directionally specific and act asymmetrically: implications for core stability theories. J Orthop Sports Phys Ther. 2008;38(5):228-237 [DOI] [PubMed] [Google Scholar]
- 4. Apeldoorn AT, Ostelo RW, van Helvoirt H, Fritz JM, de Vet HC, van Tulder MW. The cost-effectiveness of a treatment-based classification system for low back pain: design of a randomised controlled trial and economic evaluation. BMC Musculoskelet Disord. 2010;11(1):58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Assendelft WJ, Bouter LM, Knipschild PG. Complications of spinal manipulation: a comprehensive review of the literature. J Fam Pract. 1996;42(5):475-480 [PubMed] [Google Scholar]
- 6. Assendelft WJ, Morton SC, Yu EI, Suttorp MJ, Shekelle PG. Spinal manipulative therapy for low back pain. Cochrane Database Syst Rev. 2004(1):CD000447 [DOI] [PubMed] [Google Scholar]
- 7. Barker KL, Shamley DR, Jackson D. Changes in the cross-sectional area of multifidus and psoas in patients with unilateral back pain: the relationship to pain and disability. Spine. 2004;29(22):E515-E519 [DOI] [PubMed] [Google Scholar]
- 8. Barrett AJ, Breen AC. Adverse effects of spinal manipulation. J R Soc Med. 2000;93(5):258-259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Beattie PF, Arnot CF, Donley JW, Noda H, Bailey L. The immediate reduction in low back pain intensity following lumbar joint mobilization and prone press-ups is associated with increased diffusion of water in the L5-S1 intervertebral disc. J Orthop Sports Phys Ther. 2010;40(5):256-264 [DOI] [PubMed] [Google Scholar]
- 10. Berthelot J, Delecrin J, Maugars Y, Passuti N. Contribution of centralization phenomenon to the diagnosis, prognosis, and treatment of diskogenic low back pain. Joint Bone Spine. 2007;74(4):319-323 [DOI] [PubMed] [Google Scholar]
- 11. Beurskens AJ, De Vet HC, Koke AJ, et al. Efficacy of traction for nonspecific low back pain. 12-week and 6-month results of a randomized clinical trial. Spine. 1997;22:2756-2762 [DOI] [PubMed] [Google Scholar]
- 12. Bialosky J, Bishop M, Price D, Robinson M, George S. The mechanisms of manual therapy in the treatment of musculoskeletal pain: a comprehensive model. Man Ther. 2009;14(5):531-538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bialosky J, Bishop M, Robinson M, Zeppieri GJ, George S. Spinal manipulative therapy has an immediate effect on thermal pain sensitivity in people with low back pain: a randomized controlled trial. Phys Ther. 2009;89(12):1292-1303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bialosky JE, George SZ, Bishop MD. How spinal manipulative therapy works: why ask why? J Orthop Sports Phys Ther. 2008;38(6):293-295 [DOI] [PubMed] [Google Scholar]
- 15. Borkan JM, Koes B, Reis S, Cherkin DC. A report from the second international forum for primary care research on low back pain: reexamining priorities. Spine. 1998;23(18):1992-1996 [DOI] [PubMed] [Google Scholar]
- 16. Borman P, Keskin D, Bodur H. The efficacy of lumbar traction in the management of patients with low back pain. Rheumatol Int. 2003;23:82-86 [DOI] [PubMed] [Google Scholar]
- 17. Brennan GP, Fritz JM, Hunter SJ, Thackeray A, Delitto A, Erhard RE. Identifying subgroups of patients with acute/subacute “nonspecific” low back pain: results of a randomized clinical trial. Spine. 2006;31(6):623-631 [DOI] [PubMed] [Google Scholar]
- 18. Bronfort G, Haas M, Evans R, Kawchuk G, Dagenais S. Evidence-informed management of chronic low back pain with spinal manipulation and mobilization. Spine J. 2008;8(1):213-225 [DOI] [PubMed] [Google Scholar]
- 19. Bronfort G, Haas M, Evans RL, Bouter LM. Efficacy of spinal manipulation and mobilization for low back pain and neck pain: a systematic review and best evidence synthesis. Spine J. 2004;4(3):335-356 [DOI] [PubMed] [Google Scholar]
- 20. Browder D, Childs J, Cleland J, Fritz J. Effectiveness of an extension-oriented treatment approach in a subgroup of subjects with low back pain: a randomized clinical trial. Phys Ther. 2007;87(12):1608-1618 [DOI] [PubMed] [Google Scholar]
- 21. Cagnie B, Vinck E, Beernaert A, Cambier D. How common are side effects of spinal manipulation and can these side effects be predicted? Man Ther. 2004;9(3):151-156 [DOI] [PubMed] [Google Scholar]
- 22. Cairns MC, Foster NE, Wright C. Randomized controlled trial of specific spinal stabilization exercises and conventional physiotherapy for recurrent low back pain. Spine. 2006;31(19):E670-E681 [DOI] [PubMed] [Google Scholar]
- 23. Childs JD, Fritz JM, Flynn TW, et al. A clinical prediction rule to identify patients with low back pain most likely to benefit from spinal manipulation: a validation study. Ann Intern Med. 2004;141(12):920-928 [DOI] [PubMed] [Google Scholar]
- 24. Chou R, Huffman LH. Nonpharmacologic therapies for acute and chronic low back pain: a review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline. Ann Intern Med. 2007;147(7):492-504 [DOI] [PubMed] [Google Scholar]
- 25. Chou R, Qaseem A, Snow V, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147(7):478-491 [DOI] [PubMed] [Google Scholar]
- 26. Clarke JA, van Tulder MW, Blomberg SE, et al. Traction for low-back pain with or without sciatica. Cochrane Database Syst Rev. 2007;2:CD003010 [DOI] [PubMed] [Google Scholar]
- 27. Cleland JA, Fritz JM, Kulig K, et al. Comparison of the effectiveness of three manual physical therapy techniques in a subgroup of patients with low back pain who satisfy a clinical prediction rule: a randomized clinical trial. Spine (Phila Pa 1976). 2009;34(25):2720-2729 [DOI] [PubMed] [Google Scholar]
- 28. Comer C, Redmond A, Bird H, Conaghan P. Assessment and management of neurogenic claudication associated with lumbar spinal stenosis in a UK primary care musculoskeletal service: a survey of current practice among physiotherapists. BMC Musculoskelet Disord. 2009;10:121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Costa LO, Maher CG, Latimer J, et al. Motor control exercise for chronic low back pain: a randomized placebo-controlled trial. Phys Ther. 2009;89(12):1275-1286 [DOI] [PubMed] [Google Scholar]
- 30. Costa Lda C, Maher CG, McAuley JH, et al. Prognosis for patients with chronic low back pain: inception cohort study. BMJ. 2009;339:b3829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Dagenais S, Caro J, Haldeman S. A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J. 2008;8(1):8-20 [DOI] [PubMed] [Google Scholar]
- 32. Daniel DM. Non-surgical spinal decompression therapy: does the scientific literature support efficacy claims made in the advertising media? Chiropr Osteopat. 2007;15:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Danneels LA, Vanderstraeten GG, Cambier DC, Witvrouw EE, De Cuyper HJ. CT imaging of trunk muscles in chronic low back pain patients and healthy control subjects. Eur Spine J. 2000;9(4):266-272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Delitto A. Research in low back pain: time to stop seeking the elusive “magic bullet.” Phys Ther. 2005;85:206-208 [PubMed] [Google Scholar]
- 35. Delitto A, Erhard RE, Bowling RW. A treatment-based classification approach to low back syndrome: identifying and staging patients for conservative management. Phys Ther. 1995;75:470-489 [DOI] [PubMed] [Google Scholar]
- 36. Department of Health The Prevalence of Back Pain in Great Britain in 1998. London: Government Statistical Service; 1999 [Google Scholar]
- 37. Deyo RA, Rainville J, Kent DL. What can the history and physical examination tell us about low back pain? JAMA. 1992;268(6):760-765 [PubMed] [Google Scholar]
- 38. Donelson R, Aprill C, Medcalf R, Grant W. A prospective study of centralization of lumbar and referred pain. A predictor of symptomatic discs and anular competence. Spine (Phila Pa 1976). 1997;22(10):1115-1122 [DOI] [PubMed] [Google Scholar]
- 39. Evans DW. Mechanisms and effects of spinal high-velocity, low-amplitude thrust manipulation: previous theories. J Manipulative Physiol Ther. 2002;25(4):251-262 [DOI] [PubMed] [Google Scholar]
- 40. Ferreira M, Ferreira P, Latimer J, Herbert R, Maher C. Does spinal manipulative therapy help people with chronic low back pain? Aust J Physiother. 2002;48(4):277-284 [DOI] [PubMed] [Google Scholar]
- 41. Ferreira ML, Ferreira PH, Latimer J, et al. Comparison of general exercise, motor control exercise and spinal manipulative therapy for chronic low back pain: a randomized trial. Pain. 2007;131(1-2):31-37 [DOI] [PubMed] [Google Scholar]
- 42. Ferreira P, Ferreira M, Maher C, Refshauge K, Herbert R, Hodges P. Changes in recruitment of transversus abdominis correlate with disability in people with chronic low back pain. Br J Sports Med. 2010;44(16):1166-1172 [DOI] [PubMed] [Google Scholar]
- 43. Feuerstein M, Marcus SC, Huang GD. National trends in nonoperative care for nonspecific back pain. Spine J. 2004;4(1):56-63 [DOI] [PubMed] [Google Scholar]
- 44. Flynn T, Fritz J, Whitman J, et al. A clinical prediction rule for classifying patients with low back pain who demonstrate short-term improvement with spinal manipulation. Spine. 2002;27(24):2835-2843 [DOI] [PubMed] [Google Scholar]
- 45. Franca FR, Burke TN, Hanada ES, Marques AP. Segmental stabilization and muscular strengthening in chronic low back pain: a comparative study. Clinics (Sao Paulo). 2010;65(10):1013-1017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Fritz J, Delitto A, Welch W, Erhard R. Lumbar spinal stenosis: a review of current concepts in evaluation, management, and outcome measurements. Arch Phys Med Rehabil. 1998;79(6):700-708 [DOI] [PubMed] [Google Scholar]
- 47. Fritz JM. Clinical prediction rules in physical therapy: coming of age? J Orthop Sports Phys Ther. 2009;39(3):159-161 [DOI] [PubMed] [Google Scholar]
- 48. Fritz JM, Cleland JA, Childs JD. Subgrouping patients with low back pain: evolution of a classification approach to physical therapy. J Orthop Sports Phys Ther. 2007;37(6):290-302 [DOI] [PubMed] [Google Scholar]
- 49. Fritz JM, Delitto A, Erhard RE. Comparison of classification-based physical therapy with therapy based on clinical practice guidelines for patients with acute low back pain: a randomized clinical trial. Spine. 2003;28(13):1363-1371 [DOI] [PubMed] [Google Scholar]
- 50. Fritz JM, Hebert J, Koppenhaver S, Parent E. Beyond minimally important change: defining a successful outcome of physical therapy for patients with low back pain. Spine (Phila Pa 1976). 2009;34(25):2803-2809 [DOI] [PubMed] [Google Scholar]
- 51. Fritz JM, Lindsay W, Matheson JW, et al. Is there a subgroup of patients with low back pain likely to benefit from mechanical traction? Results of a randomized clinical trial and subgrouping analysis. Spine. 2007;32(26):E793-E800 [DOI] [PubMed] [Google Scholar]
- 52. Fritz JM, Thackeray A, Childs JD, Brennan GP. A randomized clinical trial of the effectiveness of mechanical traction for sub-groups of patients with low back pain: study methods and rationale. BMC Musculoskelet Disord. 2010;11:81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Frymoyer JW, Selby DK. Segmental instability: rationale for treatment. Spine. 1985;10(3):280-286 [DOI] [PubMed] [Google Scholar]
- 54. George S, Bialosky J, Donald D. The centralization phenomenon and fear-avoidance beliefs as prognostic factors for acute low back pain: a preliminary investigation involving patients classified for specific exercise. J Orthop Sports Phys Ther. 2005;35(9):580-588 [DOI] [PubMed] [Google Scholar]
- 55. Goldby LJ, Moore AP, Doust J, Trew ME. A randomized controlled trial investigating the efficiency of musculoskeletal physiotherapy on chronic low back disorder. Spine. 2006;31(10):1083-1093 [DOI] [PubMed] [Google Scholar]
- 56. Greenman PE. Principles of Manual Medicine. 2nd ed. Baltimore, MD: Williams & Wilkins; 1996 [Google Scholar]
- 57. Haldeman S, Rubinstein SM. Cauda equina syndrome in patients undergoing manipulation of the lumbar spine. Spine (Phila Pa 1976). 1992;17(12):1469-1473 [DOI] [PubMed] [Google Scholar]
- 58. Hancock M, Herbert RD, Maher CG. A guide to interpretation of studies investigating subgroups of responders to physical therapy interventions. Phys Ther. 2009;89(7):698-704 [DOI] [PubMed] [Google Scholar]
- 59. Hancock M, Maher C, Latimer J, Herbert R, McAuley J. Independent evaluation of a clinical prediction rule for spinal manipulative therapy: a randomised controlled trial. Eur Spine J. 2008;17(7):936-943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Harte AA, Gracey JH, Baxter GD. Current use of lumbar traction in the management of low back pain: results of a survey of physiotherapists in the United Kingdom. Arch Phys Med Rehabil. 2005;86:1164-1169 [DOI] [PubMed] [Google Scholar]
- 61. Hebert J, Koppenhaver S, Fritz J, Parent E. Clinical prediction for success of interventions for managing low back pain. Clin Sports Med. 2008;27(3):463-479 [DOI] [PubMed] [Google Scholar]
- 62. Hebert JJ, Koppenhaver SL, Magel JS, Fritz JM. The relationship of transversus abdominis and lumbar multifidus activation and prognostic factors for clinical success with a stabilization exercise program: a cross-sectional study. Arch Phys Med Rehabil. 2010;91(1):78-85 [DOI] [PubMed] [Google Scholar]
- 63. Henschke N, Maher CG, Refshauge KM, Das A, McAuley JH. Low back pain research priorities: a survey of primary care practitioners. BMC Fam Pract. 2007;8:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Hicks GE, Fritz JM, Delitto A, McGill SM. Preliminary development of a clinical prediction rule for determining which patients with low back pain will respond to a stabilization exercise program. Arch Phys Med Rehabil. 2005;86(9):1753-1762 [DOI] [PubMed] [Google Scholar]
- 65. Hides JA, Jull GA, Richardson CA. Long-term effects of specific stabilizing exercises for first-episode low back pain. Spine. 2001;26(11):E243-E248 [DOI] [PubMed] [Google Scholar]
- 66. Hides JA, Lambrecht G, Richardson CA, et al. The effects of rehabilitation on the muscles of the trunk following prolonged bed rest. Eur Spine J. 2011;20(5):808-818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Hides JA, Richardson CA, Jull GA. Multifidus muscle recovery is not automatic after resolution of acute, first-episode low back pain. Spine. 1996;21(23):2763-2769 [DOI] [PubMed] [Google Scholar]
- 68. Hides JA, Stanton WR, McMahon S, Sims K, Richardson CA. Effect of stabilization training on multifidus muscle cross-sectional area among young elite cricketers with low back pain. J Orthop Sports Phys Ther. 2008;38(3):101-108 [DOI] [PubMed] [Google Scholar]
- 69. Hodges PW, Richardson CA. Altered trunk muscle recruitment in people with low back pain with upper limb movement at different speeds. Arch Phys Med Rehabil. 1999;80(9):1005-1012 [DOI] [PubMed] [Google Scholar]
- 70. Hodges PW, Richardson CA. Feedforward contraction of transversus abdominis is not influenced by the direction of arm movement. Exp Brain Res. 1997;114(2):362-370 [DOI] [PubMed] [Google Scholar]
- 71. Hodges PW, Richardson CA. Inefficient muscular stabilization of the lumbar spine associated with low back pain: a motor control evaluation of transversus abdominis. Spine. 1996;21(22):2640-2650 [DOI] [PubMed] [Google Scholar]
- 72. Hollingworth W, Todd CJ, King H, et al. Primary care referrals for lumbar spine radiography: diagnostic yield and clinical guidelines. Br J Gen Pract. 2002;52(479):475-480 [PMC free article] [PubMed] [Google Scholar]
- 73. Hungerford B, Gilleard W, Hodges P. Evidence of altered lumbopelvic muscle recruitment in the presence of sacroiliac joint pain. Spine. 2003;28(14):1593-1600 [PubMed] [Google Scholar]
- 74. Kent P, Keating J. Do primary-care clinicians think that nonspecific low back pain is one condition? Spine (Phila Pa 1976). 2004;29(9):1022-1031 [DOI] [PubMed] [Google Scholar]
- 75. Kilpikoski S, Airaksinen O, Kankaanpaa M, Leminen P, Videman T, Alen M. Interexaminer reliability of low back pain assessment using the McKenzie method. Spine. 2002;27(8):E207-E214 [DOI] [PubMed] [Google Scholar]
- 76. Kjaer P, Bendix T, Sorensen JS, Korsholm L, Leboeuf-Yde C. Are MRI-defined fat infiltrations in the multifidus muscles associated with low back pain? BMC Med. 2007;5:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Koppenhaver SL, Fritz JM, Hebert JJ, et al. Association between changes in abdominal and lumbar multifidus muscle function and clinical improvement after spinal manipulation. J Orthop Sports Phys Ther. Accepted for publication [DOI] [PubMed] [Google Scholar]
- 78. Kosteljanetz M, Bang F, Schmidt-Olsen S. The clinical significance of straight-leg raising (Lasegue’s sign) in the diagnosis of prolapsed lumbar disc: interobserver variation and correlation with surgical finding. Spine. 1988;13(4):393-395 [DOI] [PubMed] [Google Scholar]
- 79. Koumantakis GA, Watson PJ, Oldham JA. Trunk muscle stabilization training plus general exercise versus general exercise only: randomized controlled trial of patients with recurrent low back pain. Phys Ther. 2005;85(3):209-225 [PubMed] [Google Scholar]
- 80. Laslett M, Oberg B, Aprill C, McDonald B. Centralization as a predictor of provocation discography results in chronic low back pain, and the influence of disability and distress on diagnostic power. Spine J. 2005;5(4):370-380 [DOI] [PubMed] [Google Scholar]
- 81. Leboeuf-Yde C, Hennius B, Rudberg E, Leufvenmark P, Thunman M. Side effects of chiropractic treatment: a prospective study. J Manipulative Physiol Ther. 1997;20:511-515 [PubMed] [Google Scholar]
- 82. Long A, Donelson R, Fung T. Does it matter which exercise? A randomized control trial of exercise for low back pain. Spine (Phila Pa 1976). 2004;29(23):2593-2602 [DOI] [PubMed] [Google Scholar]
- 83. Luo X, Pietrobon R, Sun SX, Liu GG, Hey L. Estimates and patterns of direct health care expenditures among individuals with back pain in the United States. Spine (Phila Pa 1976). 2004;29(1):79-86 [DOI] [PubMed] [Google Scholar]
- 84. MacDonald D, Moseley GL, Hodges PW. Why do some patients keep hurting their back? Evidence of ongoing back muscle dysfunction during remission from recurrent back pain. Pain. 2009;142(3):183-188 [DOI] [PubMed] [Google Scholar]
- 85. Maitland GD. Vertebral Manipulation. 5th ed. Oxford, England: Butterworth Heinemann; 1986 [Google Scholar]
- 86. Mannion AF, Pulkovski N, Schenk P, et al. A new method for the noninvasive determination of abdominal muscle feedforward activity based on tissue velocity information from tissue Doppler imaging. J Appl Physiol. 2008;104(4):1192-1201 [DOI] [PubMed] [Google Scholar]
- 87. McGill S. Low Back Disorders: Evidence-Based Prevention and Rehabilitation. 2nd ed. Champaign, IL: Human Kinetics; 2007 [Google Scholar]
- 88. McGinn TG, Guyatt GH, Wyer PC, Naylor CD, Stiell IG, Richardson WS. Users’ guide to the medical literature XXII: how to use articles about clinical decision rules. JAMA. 2000;284:79-84 [DOI] [PubMed] [Google Scholar]
- 89. McKenzie R, May S. The Lumbar Spine: Mechanical Diagnosis and Therapy. Raumati Beach, New Zealand: Spinal Publications; 2003 [Google Scholar]
- 90. Meeker WC, Haldeman S. Chiropractic: a profession at the crossroads of mainstream and alternative medicine. Ann Intern Med. 2002;136(3):216-227 [DOI] [PubMed] [Google Scholar]
- 91. Mengiardi B, Schmid MR, Boos N, et al. Fat content of lumbar paraspinal muscles in patients with chronic low back pain and in asymptomatic volunteers: quantification with MR spectroscopy. Radiology. 2006;240(3):786-792 [DOI] [PubMed] [Google Scholar]
- 92. Murphy DR, Hurwitz EL. A theoretical model for the development of a diagnosis-based clinical decision rule for the management of patients with spinal pain. BMC Musculoskelet Disord. 2007;8:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Nachemson A. Lumbar spine instability: a critical update and symposium summary. Spine. 1985;10(3):290-291 [PubMed] [Google Scholar]
- 94. Palmer KT, Walsh K, Bendall H, Cooper C, Coggon D. Back pain in Britain: comparison of two prevalence surveys at an interval of 10 years. BMJ. 2000;320(7249):1577-1578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Rackwitz B, de Bie R, Limm H, von Garnier K, Ewert T, Stucki G. Segmental stabilizing exercises and low back pain: what is the evidence? A systematic review of randomized controlled trials. Clin Rehabil. 2006;20(7):553-567 [DOI] [PubMed] [Google Scholar]
- 96. Randolph AG, Guyatt GH, Carlet J. Understanding articles comparing outcomes among intensive care units to rate quality of care. Evidence Based Medicine in Critical Care Group. Crit Care Med. 1998;26(4):773-781 [DOI] [PubMed] [Google Scholar]
- 97. Reeves BC, Deeks JJ, Higgins JPT, Wells GA. Including non-randomized studies. In: Higgins JPT, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.0.2. http://www.cochrane-handbook.org Updated September 2009
- 98. Richardson C, Hodges P, Hides J. Therapeutic Exercise for Lumbopelvic Stabilization: A Motor Control Approach for the Treatment and Prevention of Low Back Pain. 2nd ed. London, England: Churchill Livingstone; 2004 [Google Scholar]
- 99. Rubin DI. Epidemiology and risk factors for spine pain. Neurol Clin. 2007;25(2):353-371 [DOI] [PubMed] [Google Scholar]
- 100. Rubinstein SM. Adverse events following chiropractic care for subjects with neck or low-back pain: do the benefits outweigh the risks? J Manipulative Physiol Ther. 2008;31(6):461-464 [DOI] [PubMed] [Google Scholar]
- 101. Rubinstein SM, van Middelkoop M, Kuijpers T, et al. A systematic review on the effectiveness of complementary and alternative medicine for chronic non-specific low-back pain. Eur Spine J. 2010;19(8):1213-1228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Savigny P, Watson P, Underwood M. Early management of persistent non-specific low back pain: summary of NICE guidance. BMJ. 2009;338:b1805. [DOI] [PubMed] [Google Scholar]
- 103. Shaughnessy M, Caulfield B. A pilot study to investigate the effect of lumbar stabilisation exercise training on functional ability and quality of life in patients with chronic low back pain. Int J Rehabil Res. 2004;27(4):297-301 [DOI] [PubMed] [Google Scholar]
- 104. Silver J. The history of modern spinal traction with particular reference to neural disorders. Spinal Cord. 1997;35(10):710-711 [DOI] [PubMed] [Google Scholar]
- 105. Skytte L, May S, Petersen P. Centralization: its prognostic value in patients with referred symptoms and sciatica. Spine (Phila Pa 1976). 2005;30(11):E293-E299 [DOI] [PubMed] [Google Scholar]
- 106. Sutlive T, Mabry L, Easterling E, et al. Comparison of short-term response to two spinal manipulation techniques for patients with low back pain in a military beneficiary population. Mil Med. 2009;174(7):750-756 [DOI] [PubMed] [Google Scholar]
- 107. Teyhen DS, Flynn TW, Childs JD, Abraham LD. Arthrokinematics in a subgroup of patients likely to benefit from a lumbar stabilization exercise program. Phys Ther. 2007;87(3):313-325 [DOI] [PubMed] [Google Scholar]
- 108. Tsao H, Hodges PW. Immediate changes in feedforward postural adjustments following voluntary motor training. Exp Brain Res. 2007;181(4):537-546 [DOI] [PubMed] [Google Scholar]
- 109. Tsao H, Hodges PW. Persistence of improvements in postural strategies following motor control training in people with recurrent low back pain. J Electromyogr Kinesiol. 2008;18(4):559-567 [DOI] [PubMed] [Google Scholar]
- 110. van der Heijden GJ, Beurskens AJ, Koes BW, Assendelft WJ, De Vet HC, Bouter LM. The efficacy of traction for back and neck pain: a systematic, blinded review of randomized clinical trial methods. Phys Ther. 1995;75:93-104 [DOI] [PubMed] [Google Scholar]
- 111. van Middelkoop M, Rubinstein SM, Kuijpers T, et al. A systematic review on the effectiveness of physical and rehabilitation interventions for chronic non-specific low back pain. Eur Spine J. 2011;20(1):19-39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. van Tulder MW, Koes B, Malmivaara A. Outcome of non-invasive treatment modalities on back pain: an evidence-based review. Eur Spine J. 2006;15:S64-S81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Walker BF. The prevalence of low back pain: a systematic review of the literature from 1966 to 1998. J Spinal Disord. 2000;13(3):205-217 [DOI] [PubMed] [Google Scholar]
- 114. Walker BF, Muller R, Grant WD. Low back pain in Australian adults: the economic burden. Asia Pac J Public Health. 2003;15(2):79-87 [DOI] [PubMed] [Google Scholar]
- 115. Walker BF, Williamson OD. Mechanical or inflammatory low back pain: what are the potential signs and symptoms? Man Ther. 2009;14(3):314-320 [DOI] [PubMed] [Google Scholar]
- 116. Wallwork TL, Stanton WR, Freke M, Hides JA. The effect of chronic low back pain on size and contraction of the lumbar multifidus muscle. Man Ther. 2009;14(5):496-500 [DOI] [PubMed] [Google Scholar]
- 117. Werneke M, Hart D, George S, Stratford P, Matheson J, Reyes A. Clinical outcomes for patients classified by fear-avoidance beliefs and centralization phenomenon. Arch Phys Med Rehabil. 2009;90(5):768-777 [DOI] [PubMed] [Google Scholar]
- 118. Werneke M, Hart D, Resnik L, Stratford P, Reyes A. Centralization: prevalence and effect on treatment outcomes using a standardized operational definition and measurement method. J Orthop Sports Phys Ther. 2008;38(3):116-125 [DOI] [PubMed] [Google Scholar]
- 119. Werneke MW. “Centralization” and “directional preference” are not synonymous. J Orthop Sports Phys Ther. 2009;39(11):827. [DOI] [PubMed] [Google Scholar]
- 120. Werners R, Pynsent PB, Bulstrode CJK. Randomized trial comparing interferential therapy with motorized lumbar traction and massage in the management of low back pain in a primary care setting. Spine. 1999;24:1579-1584 [DOI] [PubMed] [Google Scholar]
- 121. Whitman J, Flynn T, Childs J, et al. A comparison between two physical therapy treatment programs for patients with lumbar spinal stenosis: a randomized clinical trial. Spine. 2006;31(22):2541-2549 [DOI] [PubMed] [Google Scholar]
- 122. Young S, Aprill C, Laslett M. Correlation of clinical examination characteristics with three sources of chronic low back pain. Spine J. 2003;3(6):460-465 [DOI] [PubMed] [Google Scholar]


