Abstract
Context:
Overuse injuries of the musculoskeletal system in immature athletes are commonly seen in medical practice.
Evidence Acquisition:
An analysis of published clinical, outcome, and biomechanical studies of adolescent epiphyseal and overuse injuries was performed through 2008 to increase recognition and provide treatment recommendations.
Results:
Adolescent athletes can sustain physeal and bony stress injuries. Recovery and return to play occur more swiftly if such injuries are diagnosed early and immobilized until the patient is pain-free, typically about 4 weeks for apophyseal and epiphyseal overuse injuries. Certain epiphyseal injuries have prolonged symptoms with delayed treatment, including those involving the bones in the hand, elbow, and foot. If such injuries are missed, prolonged healing and significant restrictions in athletic pursuits may occur.
Conclusion:
Some of these injuries are common to all weightbearing sports and are therefore widely recognized. Several are common in gymnastics but are rarely seen in other athletes. Early recognition and treatment of these conditions lead to quicker recovery and so may prevent season-ending, even career-ending, events from occurring.
Keywords: apophysitis, epiphysitis, epihyseolysis, adolescent athletes, overuse
Skeletally immature athletes can sustain all the same injuries that mature athletes sustain: fractures, dislocations, sprains, and tendonitis. Immature athletes differ from mature athletes because of their open growth plates. Physes provide multiple additional sites for injury not seen in a mature skeleton. They are frequently injured during a discrete traumatic event, and they are commonly affected by the repeated stress of sports and so may present insidiously. Apophysitis15,20,22,35 is a tuberosity stressed in traction, whereas epiphysitis11 is a compression or shear injury; epiphyseolysis5,37,64 is the widening of a growth plate under stress.
These injuries may continue to be symptomatic over a long period. Inadequate treatment of these overuse injuries may prolong healing. Neglect may result in permanent deformity (Osgood-Schlatter disease) or, in rare cases, avulsion requiring operative fixation. Early diagnosis and treatment can prevent the more serious sequela of these injuries.
The Physis
During adolescent growth spurts, the cartilage cells of the physis not only become more active but apparently become more prone to injury.9 Hypertrophy and weakening of the hypertrophic zone of cartilage are thought to be the cause. The female skeleton generally grows and fully matures (ie, growth plate fusion) before the male skeleton.32 Therefore, male athletes tend to manifest physeal injuries 1 to 2 years later than female athletes. Gymnasts and ballet dancers often show delayed skeletal maturity71 and so may experience these injuries at a much later chronologic age than that of participants in other sports.
Until recently, growth plate injuries were thought to always involve the cartilaginous physis. Ogden et al52 recently demonstrated that these injuries may be fractures of the metaphyseal bone adjacent to the physis. The principles of treating stress fractures elsewhere in the body should therefore be applied: relief of daily and pathologic stresses by activity modification, casting, modified weightbearing, and bracing.
In most long bones, the epiphysis is at least partially ossified at an early age and therefore visible with plain radiographs. In certain areas of the body (eg, ischial tuberosity, iliac crest, base of the fifth metatarsal), the epiphysis may not become ossified until the near end of the final growth spurt. Given that these are not ossified at an early age, they are not visible on plain radiographs. Therefore, one must understand that despite the lack of a visible physis on plain radiographs, these areas may still have peri-epiphyseal injuries and so must be treated as such.
Physical Exam
Peri-epiphyseal injuries all have one feature in common: tenderness to direct palpation. Some growth plates are in superficial areas with scant subcutaneous tissue, such as the calcaneus and the distal radius, and are thus easily palpated. Some deeper areas, such as the ischial tuberosity, may not be palpable in heavily muscled or obese persons. When easy access is not possible, indirect methods may be used to elicit tenderness. Hamstrings stretching may produce ischial tuberosity pain. The Ober test for iliotibial band tightness is done with the patient lying on the unaffected side. The affected hip is extended and adducted with the knee at a 90° angle. A tight iliotibial band will not allow enough hip adduction so that the knee on the affected side can touch the examination table. This test stresses the physis of the iliac crest, which may result in pain. Resisting joint motion may also produce pain or elicit weakness: knee extension for Osgood-Schlatter disease or hip abduction for the iliac crest.
Soft tissue swelling may be seen in more severe cases where the physis is superficial, such as at the distal radius and tibial tuberosity.
Distal Radial Epiphysitis
Distal radial epiphyseal injuries are most common in male and female gymnasts17,63,75 but occasionally happen in other sports.26 The patients describe the gradual onset of wrist pain made worse by weightbearing activities while the wrist is in extension, as in tumbling, vaulting, and back walkovers.
Physical examination often reveals normal range of motion and swelling of the distal radius.14 Tenderness is frequently found over the dorsal-radial growth plate. Tenderness may also be elicited on the volar-radial physis as well. Snuff box tenderness is usually absent. Range of motion of the wrist is usually normal.
Radial physes appear at the age of 12 to 18 months and fuse by 15 to 18 years.32 The growth plate is most vulnerable to injury during the adolescent growth spurt.30 Competitive gymnasts frequently demonstrate delayed skeletal maturity and so may manifest these developments 1 to 2 years later than athletes in other sports.
Radiographic findings depend on the stage of the disease (Figure 1). Sclerosis may occur on both sides of the growth plate, but it is usually more prominent on the metaphyseal side.17 Widening of the physis may be observed on both anteroposterior and lateral radiographic projections, but it is most common on the radial and volar aspects of the epiphysis. Similar changes may occur in the ulnar growth plate.17,75
Figure 1.
Anteroposterior and lateral radiographs of a 14-year-old female gymnast with distal radius epiphysitis, demonstrating widening of epiphysis (more pronounced volarly and radially). The patient had resolution of symptoms after immobilization in a short arm cast for 4 weeks. Repeat radiographs at 1 year show interval improvement in the physeal widening.
The frequency of distal radius pathology varies with age and competitive level. In a survey of 60 club gymnasts aged 9 to 17 years and of varying levels, Caine et al13 found only 5 with radiographic changes of the radius. Auberge et al,4 however, found those changes in 83% of 105 gymnasts in the 1980 European gymnastics championships. In more severe cases, beaking of the volar and radial epiphysis may occur with cystic changes in the distal metaphysis.
As healing occurs, these radiographic findings reverse in most patients. However, permanent bone changes may occur in highly competitive high-level gymnasts. In college male gymnasts, Mandelbaum et al45 found significant shortening of the radius resulting in positive ulnar variance. Severe growth disturbance (Madelung’s deformity) has also been reported in gymnasts.72
Although these injuries are usually confined to the distal forearm, the carpus can be involved. Epiphyseolitis of the radius, combined with a stress fracture of the scaphoid, has been reported.37 Patients may simultaneously present with distal radial and snuff box tenderness with painful passive extension of the wrist. Radiographs of the carpus are usually negative, analogous to bony stress injuries in the foot and elbow. MRI, however, may reveal extensive stress reaction in the scaphoid and other bones of the wrist, which may represent an impending stress fracture of the carpus and thus be a more serious injury than distal radial epiphysitis, requiring immediate treatment.
Bone scans have not been helpful in diagnosing radial epiphysitis. Two studies63,75 have shown bilaterally symmetrical uptake in patients with unilateral symptoms. Bone scans may show increased uptake near the physis owing to the high bone turnover in this area; therefore, the clinical presentation (rather than the bone scans) is the key to establishing the diagnosis. Treatment begins with cessation of the activities that require weightbearing, the use of dowel grips, or excessive traction on the extended wrist.75
Time to healing is dependent on the stage of the disease and the radiographic findings. When radiographs are negative, 4 weeks of rest usually allow for healing and return to activities. Immobilization in a cast is the mainstay of treatment. Athletes are under pressure from coaches, parents, and themselves to continue participation, often removing a splint to “just do some handstands and see how it feels.” Casting removes the athlete from these pressures and allows complete rest of the injured wrist. Those involved must understand that when this injury is severe, it is the slowest of all the physeal injuries to heal. Six months or more may be required for those patients with severe involvement.63
Elbow Overuse Injuries
Adolescent baseball players, gymnasts, and weightlifters are susceptible to medial, lateral, and posterior elbow overuse injuries from the repetitive microtrauma of throwing and axial loading.
The term Little League elbow has been used to describe injuries to the medial side of the elbow,10 such as epicondyle apophysitis, epicondyle avulsion fractures, and ulnar collateral ligament injuries. The high valgus torque of throwing generates tensile and shearing stresses at the medial elbow. During adolescence, the medial epicondyle apophyseal cartilage is vulnerable to the repetitive microtrauma of throwing; it is the weak link.12
Patients with medial epicondyle apophysitis will typically present with medial pain, claiming that their throwing distance has decreased. Common findings include point tenderness over the medial epicondyle and epicondylar hypertrophy.29 Radiographs may reveal widening of the apophysis or fragmentation of the ossification center.1
Treatment begins with rest for 4 to 6 weeks. Immobilization is necessary only for severe or refractory cases. If a patient is pain-free after a period of rest, a gradual return to throwing may be allowed. Avoidance of aggravating pitches, high pitch counts, and pitching mechanics modification may be needed. Avulsion injuries may occur with continued throwing in untreated elbows and so may require operative reduction and fixation.
The lateral elbow is also susceptible to overuse injury. Osteochondritis dissecans of the elbow most commonly involves the capitellum (Figure 2). Causes include repetitive forces applied to the radiocapitellar joint12,39,74 from valgus compression and shearing during throwing or axial loading (in gymnasts). These forces can alter the subchondral blood supply, thereby leading to a focal subchondral bone lesion, which can collapse. An early radiographic finding is the flattening of subchondral bone.70 The natural progression leads to new bone formation over the flattened subchondral bone. If this occurs, repetitive forces can produce an unstable fragment, which may displace. Presenting symptoms include poorly localized activity-related elbow pain, aching at rest, or mechanical symptoms of catching or locking. An elbow effusion and/or tenderness of the radiocapitellar joint may be present. Loss of elbow motion and flexion contractures are common. MRI may identify loose bodies and help determine the size of the lesion and the condition of the articular cartilage.
Figure 2.

Sagittal MRI of the elbow in a 14-year-old gymnast with lateral elbow pain. Note the signal alteration in the capitellum, representing early osteochondritis dissecans. The symptoms resolved with appropriate nonoperative treatment. This osteochondritis dissecans lesion was never visible on plain radiographs.
Osteochondritis dissecans should be differentiated from osteochondrosis of the capitellum (Panner’s disease).40 Panner’s disease is a self-limited condition of the capitellum, typically seen in children younger than 10 years old. Radiographs of Panner’s disease demonstrate involvement of the entire capitellar epiphysis. It has a benign course that usually resolves with rest and activity modifications. Treatment for an osteochondritis dissecans lesion is guided by the stage of the lesion. Arthroscopic and radiographic classification systems have been proposed.6,69 Radiographic stage 1 lesions have localized capitellar flattening or radiolucency; stage 2 lesions have nondisplaced fragments; and stage 3 lesions have displaced fragments. Patients with stable lesions can be treated nonoperatively if they do not have mechanical symptoms. The treatment begins with an extended period of elbow rest and splinting (if symptoms are significant). Mihara et al49 found that throwing could resume at 4 months (for open physes) and 8 months (for closed physes). Patients with open physes and stage 1 lesions tend to have a better outcome69 and are good candidates for nonoperative treatment. Worse outcomes are seen in those who continue to stress the elbow.49 Surgical treatment should be considered for closed growth plates or for stage 2 or 3 lesions with mechanical symptoms or loose bodies. Surgical options include open or arthroscopic excision of loose bodies, debridement, drilling and in situ fixation, excision and chondral resurfacing, or bone grafting.12,49,69 Simple excision should be limited to lesions less than 50% of capitellar width.69 In situ fixation of loose capitellar lesions is not recommended, owing to poor outcomes.12,39
Due to the frequent weightbearing activities of gymnasts, osteochondritis dissecans is a common injury. Unlike pitchers, gymnasts stress the elbow daily, and once symptoms occur, the lesion can progress quickly. Once fragmentation of the capitellum has occurred, gymnasts are rarely able to return to competition. For this reason, early diagnosis is paramount, thus justifying an early MRI in a gymnast with radial-sided elbow pain. Extensive stress reaction in the capitellum, which is not visible on plain radiographs, may be seen in early stages. Cessation of weightbearing activities relieves symptoms and prevents progression to a fragmented capitellum, which has a much poorer prognosis.49
Olecranon apophysitis is commonly seen in adolescent throwers and in gymnasts.22,35,44 Typical symptoms include localized tenderness over the olecranon, as well as pain with resisted elbow extension. Radiographs may show widening or fragmentation of the apophysis (Figure 3). Avoidance of throwing for 4 to 6 weeks is advised, with a gradual return allowed when the patient is pain-free. The radiographs may not show complete consolidation at the resolution of symptoms; it may take up to 10 months.35
Figure 3.

Lateral radiograph of an elbow in a 12-year-old gymnast with olecranon apophysitis. Note the fragmentation of the olecranon.
Proximal Humeral Epiphysitis (Little Leaguer’s Shoulder)
Little Leaguer’s shoulder was first described in 1953 by Dotter.23 It is also known as osteochondritis, epiphysitis, and epiphyseolysis of the proximal humeral epiphysis. The term Little Leaguer’s shoulder may be a misnomer because it is more common in adolescents who are older than 12 and beyond Little League years.
The proximal humerus ossifies from 4 ossification centers: humeral head, greater tuberosity, lesser tuberosity, and humeral shaft.32 The ossification center for the humeral head is usually evident (radiographically) within the first year of life, whereas the greater tuberosity appears at age 3 and the lesser tuberosity at age 5. The humeral head and tuberosity unite around age 6 to form a large proximal humeral epiphysis, which unites with the shaft around age 20. This cone-shaped growth center is responsible for approximately 80% of the longitudinal growth of the humerus.59
Injury to the proximal humeral epiphysis usually occurs because of 2 mechanisms in throwers: distraction and torsion. During ball release, a distracting force is acting across the physis as the rotator cuff muscles contract to center the humeral head on the glenoid.11 The resulting distractive force may reach one-half body weight.64 In addition, throwing generates significant rotational stresses at the proximal humerus (18 N·m), particularly during the late cocking phase.16,64 Repetitive microtrauma to the physis can result in a fatigue fracture or a local inflammatory reaction. These injuries occur just before the peak incidence of Little Leaguer’s shoulder (at 13 years) and present with the loss of glenohumeral motion in adolescent pitchers.47 This decrease in glenohumeral motion may result in increased stress at the physis during throwing.
Patients describe pain localized to the proximal humerus during both throwing and resisted shoulder strength testing. It is most common in baseball pitchers, although it may be seen in any throwing athlete. Examination demonstrates focal tenderness over the proximal humerus, whereas swelling is usually absent.
The differential diagnosis of shoulder pain in adolescent throwing athletes includes glenohumeral instability, rotator cuff tendinopathy, impingement, and proximal humerus physeal fracture.
Radiographs characteristically show widening of the proximal humeral physis (Figure 4). Metaphyseal sclerosis5 and demineralization or fragmentation of the epiphysis2 may also be present.
Figure 4.

Anteroposterior radiograph of the shoulder in a 13-year-old pitcher with shoulder pain. Note the dramatic widening of the proximal humerus physis.
Treatment includes cessation of throwing until (1) the patient has pain-free range of motion of the shoulder and (2) radiographs return to normal, which may take up to 1 year.16 Immobilization is not recommended, owing to the risk of stiffness of both the shoulder and the elbow. When the patient is asymptomatic and has normal radiographs, gradual throwing may resume and increase as tolerated and as based on pitch count monitoring. Complications of proximal humerus epiphysitis include premature closure of the physis and salter-harris fracture.16
Skeletally Immature Spine
Gymnasts frequently sustain low back injuries secondary to hyperextension of the spine during vaulting, walkovers, and dismounts. Goldstein28 found that 25% of pre-elite gymnasts, 43% of elite gymnasts, and 63% of Olympic gymnasts had MRI abnormalities of the spine, including spondylolysis, spondylolisthesis, and disc disease.
Spondylolysis, a stress fracture of the pars interarticularis, frequently heals with rest and bracing if treated early.51 Chronic defects may not heal and so may progress to spondylolisthesis,36 a forward or anterior displacement of one vertebral body over another. Regular monitoring for progression with physical examination and standing lateral radiographs should be done at 6- to 9-month intervals until skeletal maturity (ie, some may require lumbar fusion).18
Spinous process epiphysitis (SPE)46 may mimic the symptoms of spondylolysis. It is usually nonprogressive and self-limiting, and it is often seen in female gymnasts. Diffuse low back pain is produced with hyperextension maneuvers, but it is not localized on one side or the other. Accurate diagnosis is paramount and may allow an athlete to continue training or competing.
Side bending causes pain on the side of a spondylolytic defect, whereas this maneuver causes little or no pain in SPE. Forward flexion is not painful or limited in SPE, although spondylolysis may cause hamstrings spasm,19 thus limiting forward bending. In SPE, resisted extension from a flexed position may cause pain from traction stress on the dorsal spinous processes in SPE. Also, in SPE there is tenderness exclusively at the spinous process, but in spondylolysis the pain is usually in the paraspinal area.
Radiographs are usually unremarkable in SPE and early spondylolysis. Standing posteroanterior, lateral, and supine oblique radiographs are indicated to evaluate the lumbar spine and to grade spondylolisthesis.18 Bone or SPECT (single-photon emission computed tomography) scans may be necessary to differentiate SPE from spondylolysis (Figure 5).
Figure 5.
Posteroanterior, lateral, and axial SPECT images demonstrate increased uptake of radioactive marker in 2 lumbar spinous processes of a 14-year-old patient with spinous process epiphysitis.
Treatment of SPE consists of avoiding hyperextension maneuvers, such as those based on back walkovers, dismounts, vaults, and uneven bars. Forceful extension from a flexed position places traction on the spinous process and so prolongs healing. Most patients are placed in an elastic lumbar corset with a moldable plastic insert. General conditioning such as jogging and stretching are allowed when pain-free. For a return to full activity, 4 to 6 weeks of rest and immobilization are usually required.
Pelvic Overuse Injuries
The iliac apophysis appears at an average age of 13 in girls and 15 in boys, with ossification beginning laterally and anteriorly and advancing posteriorly. The time from radiographic appearance of ossification until fusion to the crest may vary from 7 months to 3 years,61 although it typically takes 1 year. Fusion to the crest occurs at an average age of 16 in boys and 14 in girls.61 Anatomically, the anterior third of the iliac crest is the origin of the external oblique, transversus abdominis, and tensor fascia lata muscles (Figure 6).34 The posterior iliac crest is the origin of latissimus dorsi, lumbodorsal fascia, and quadratus lumborum. The anterior superior iliac spine is the site of insertion of the sartorius, tensor fascia lata muscle, and the inguinal ligament.
Figure 6.
Illustrations demonstrating iliac crest anatomy with muscular attachments.
Iliac apophysitis was described by Clancy and Foltz.20 The proposed pathophysiology is similar to that of other repetitive traction injuries, such as Osgood-Schlatter disease or Sever’s disease. It is likely a result of an inflammatory reaction, a repetitive muscle contraction, or a subclinical stress fracture at the unfused iliac apophysis.20 Although it more commonly affects the anterior crest, it may occur posteriorly.20 Frequently seen in long-distance runners and gymnasts, it has also been reported in wrestlers,68 dancers, lacrosse players, and football players. Patients often present with 2 to 8 weeks of gradual activity-related pain.20 They may have pain with coughing or sneezing, due to muscle traction at the apophysis. Physical examination typically reveals tenderness over the iliac crest, along with tightness in the iliotibial band, hip flexor, or rectus femoris. With the patient lying on the unaffected side, resisted hip abduction will produce pain at the iliac crest.
The radiographs of the pelvis may show widening of the affected portion of the iliac apophysis20 or discontinuity between the anterior one third of the apophysis and the posterior two thirds (Figure 7).43
Figure 7.

Anteroposterior radiograph of the iliac crest shows widening and fragmentation of the anterior iliac apophysis in a 15-year-old soccer player with iliac apophysitis.
The differential diagnosis includes avulsion fractures of the iliac apophysis or anterosuperior iliac spine, hip pointers (a contusion to the iliac crest and surrounding soft tissues), hernias, abdominal muscular strains, stress fractures of the femoral neck, slipped capital femoral epiphysis, and intra-articular hip pathology.
Treatment recommendations for iliac apophysitis include restricted weightbearing, limited activities, and rest for at least 4 weeks. When pain-free, the patient can start a lateral abdominal and hip abductor stretching and strengthening rehabilitation program. If sprinting or running is allowed too early, there is a risk of anterosuperior iliac spine avulsion, which may require repair.58 Local injection of a corticosteroid does not appear to provide relief in patients. Complete relief of symptoms without recurrence can result from 3 to 4 weeks of activity modification and rest.20
The ischial apophysis, the origin of the hamstrings muscle, may also be injured in adolescent athletes. The apophysis appears between the ages of 13 and 15 and fuses to the pelvis between 16 and 25.8 Eccentric contractions of the hamstrings with the hip flexed and the knee extended can result in apophysitis or avulsion fractures.56 Avulsion fractures of the ischial tuberosity are the most common site of pelvic avulsions in athletes,66 especially in soccer and female gymnasts.62 A pop is often heard during an acute injury; after which, athletes hold their hip in an extended position, allowing minimal hamstrings tension.57 Ecchymosis, swelling, tenderness, and a palpable lump at the ischium are often present, and radiographs will show a displaced ischial tuberosity (Figure 8). There are little data regarding treatment decisions between an operative and nonoperative approach for ischial avulsions.3 Surgical treatment may be needed if the displacement is greater than 1 cm or if a painful fibrous nonunion occurs.42,56
Figure 8.

Anteroposterior radiograph of the pelvis demonstrates an ischial avulsion fracture in a 14-year-old gymnast.
Adolescents with apophysitis will present with an insidious onset of ischial pain. These injuries are often misdiagnosed as bursitis or tendonitis of the hamstrings.42 Examination demonstrates tenderness over the ischium with pain worsened by straight leg raising. Treatment includes 4 weeks of protected weightbearing with crutches or until the patient is pain-free, at which time a gentle hamstrings stretching program can begin. Return to sport activities should be delayed until restoration of full strength and motion. Noncompliance or delay in treatment can lead to avulsion of the tuberosity.
Tibial Tubercle Apophysitis (Osgood-Schlatter Disease)
The most common overuse injury in adolescent athletes is apophysitis of the tibial tubercle, or Osgood-Schlatter disease.55,65 The tibial tubercle apophysis appears radiographically at 9 years in girls and 11 years in boys.41 There are 4 radiographic stages of maturation: cartilaginous, 0-11 years; apophyseal, 11-14 years; epiphyseal, 14-18 years, during which the epiphysis and apophysis coalesce; and bony, > 18 years.24 Osgood-Schlatter disease most commonly occurs during the apophyseal phase of the adolescent growth spurt. It is seen with activities requiring repeated forced knee extension. The extensor mechanism causes repetitive tensile microtrauma at the tibial tubercle apophysis. The patellar tendon inserts at the unossified distal portion of the tibial tubercle apophysis via fibrocartilage. When this weak secondary ossification center is unable to withstand the repetitive tensile forces, bony or cartilaginous separation occurs, usually during the preossification or ossification phase; bone formation between the fragments follows.53 Osgood-Schlatter disease may be related to lower limb malalignments: pronated feet, genu valgum, patella alta, and torsional abnormalities.27
More common in boys than girls50 and bilateral in 17.6% to 56.0% of cases,41 Osgood-Schlatter disease usually presents at age 13 in boys and age 12 in girls. A gradual onset of pain, swelling, tenderness, or prominence at the tibial tuberosity region is common, while worsening with jumping or running. Duration of symptoms may be up to 28 months.24
Lateral radiographs may show anterior soft tissue swelling, widening, or fragmentation of the tibial tubercle apophysis (Figure 9) and, in later stages, bony ossicles within the patellar tendon insertion. MRI of Osgood-Schlatter disease can demonstrate cartilaginous detail not visible on radiograph.33 Ultrasound may reveal pretibial edema, thickening of the patellar tendon, and fragmentation of the ossification center.7
Figure 9.

Lateral radiograph of the proximal tibia in a 14-year-old cross-country runner with Osgood-Schlatter disease. Note widening of the physis and fragmentation of the tibial tubercle.
The standard treatment for Osgood-Schlatter disease is nonoperative while the tubercle apophysis is still open. Activity modification, ice, and immobilization may be initially needed for 4 to 6 weeks, followed by stretching and strengthening exercises as pain subsides.50 Adherence to the treatment regimen may minimize the risk of tubercle enlargement and ossicle formation. The use of local injection of corticosteroids should be avoided because of their catabolic side effects.41 Surgical treatment rarely becomes necessary for refractory cases with an open apophysis. Drilling across the apophysis can expedite fusion.54 After apophyseal fusion, removal of ununited ossicles within the patellar tendon may reduce discomfort.25,50
Apophysitis of the Os Calcis (Sever’s Disease)
The calcaneal apophysis appears radiographically at 4 to 7 years in girls and 4 to 10 in boys,31 and it fuses at an average age of 16 years.48,67 This ossification center is oriented perpendicular to the axis of the calcaneal tuberosity. The Achilles tendon inserts onto the posterior aspect, and the plantar fascia originates at the medial calcaneal tuberosity.
Heel pain associated with athletic activity in an adolescent with an unfused apophysis may represent apophysitis.48 Male athletes are affected more often (75%), and 61% of cases are bilateral.48 On physical examination, there is usually posterior calcaneal tenderness with mediolateral compression anterior to the Achilles tendon insertion.48,67 Ankle dorsiflexion may aggravate the pain due to tight heel cords.48 It is associated with forefoot pronation.48,67
Radiographically, the apophysis may appear thickened67 and fragmented73 (Figure 10), reflective of the mechanical demands. Growth disturbances and bone density changes are not typical. The diagnosis is usually based on sport involvement, timing of the growth spurt, physical exam findings, and decreased flexibility, thereby obviating the need for an initial radiograph.48
Figure 10.

Lateral radiograph of the calcaneus demonstrates fragmentation and sclerosis of the calcaneal apophysis in a 13-year-old long-distance runner with Sever’s disease.
MRI on 14 patients with Sever’s disease found bone edema in the metaphysis adjacent to the apophysis, suggesting metaphyseal stress fractures.53 The edema resolved when patients were asymptomatic after immobilization for 3 to 4 weeks.
The differential diagnosis for calcaneal apophysitis includes tarsal coalition, osteomyelitis, retrocalcaneal bursitis, and neurologic disorders.48 CT scan can identify coalitions, whereas MRI can localize infection or stress injuries in the tarsal bones. The diagnosis of calcaneal apophysitis should be reconsidered if the apophysis has already fused. Gymnasts often describe nonspecific heel pain with associated ankle and midfoot discomfort. As with the wrist, stress injuries of the foot may quickly progress to more serious problems. Foot pain in an adolescent athlete is not always due to apophyseal injury (eg, navicular stress injury in Figure 11).
Figure 11.

Sagittal MRI of a foot demonstrates a navicular stress injury in a 14-year-old runner with midfoot pain.
Nonoperative treatment options include gastrocnemius-soleus stretching, dorsiflexion strengthening, and discontinuation of running sports,48 as well as viscoelastic heel cups, soft plastizote orthotics, heel wedges, or a rubber heel lift.67
Stretching exercises and orthotics may be slow to resolve symptoms because young athletes are often noncompliant. Immobilization in a short leg cast may provide the quickest resolutions of symptoms, generally in about 4 weeks.
Apophysitis of the Proximal Fifth Metatarsal (Iselin’s Disease)
The apophysis of the proximal fifth metatarsal appears radiographically at about age 10 in girls and age 12 in boys15 and fuses approximately 2 years later. The peroneus brevis and peroneus tertius insert proximally on the fifth metatarsal near the attachment of the plantar and dorsal metatarsal ligaments as well as the plantar fascia (Figure 12). The secondary ossification center is within the insertion site of the peroneus brevis on the dorsolateral aspect of the tuberosity.21
Figure 12.
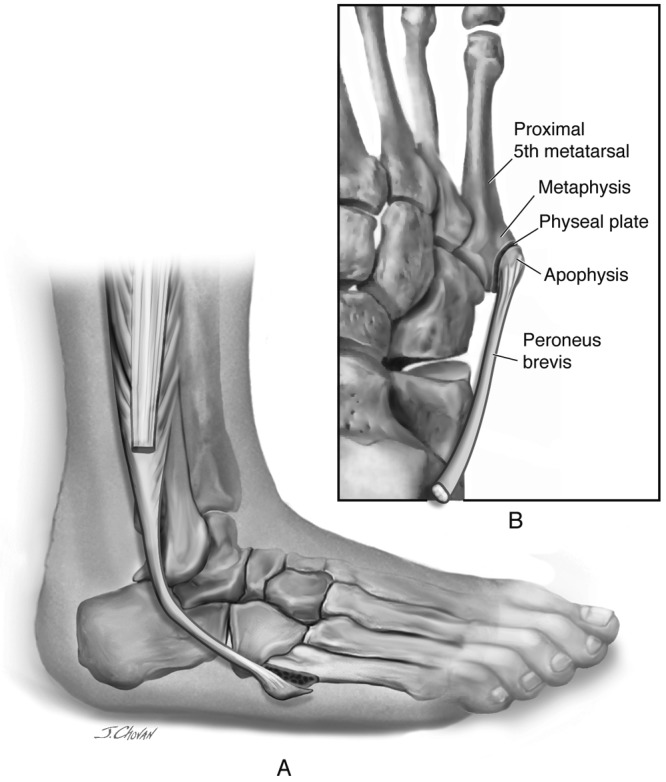
Illustration of the foot showing the peroneus brevis attachment and its relationship to the proximal fifth metatarsal apophysis.
Repetitive microtrauma from the pull of the peroneus brevis on the weak apophyseal cartilage60 causes traction apophysitis38 during rapid growth in adolescents. Inversion injuries to the foot may also lead to this condition.15
Lateral midfoot pain during weightbearing may be aggravated by running, jumping, cutting, and inversion. Pressure on the fifth metatarsal tuberosity from shoe wear may increase symptoms. Tenderness at the proximal fifth metatarsal insertion of the peroneus brevis tendon, soft tissue edema, hyperkeratosis, or mild erythema may be present on examination. Resisted eversion and extreme plantarflexion and dorsiflexion elicit pain.15 Symptoms generally resolve when fusion of the apophysis to the metaphysis occurs.
Radiographically, the secondary ossification center is best seen with an oblique view: a small fleck of bone, slightly oblique to the long axis of the metatarsal shaft along the plantar-lateral aspect of the tuberosity.21 Enlargement of the apophysis, fragmentation, or widening of the chondro-osseous junction may also be seen.15
Differential diagnosis includes fracture of the proximal fifth metatarsal, avulsion fracture of the peroneus brevis, and os vesalianum.15 The apophysis is oriented slightly oblique to the long axis of the metatarsal shaft, whereas fractures of tuberosity are more transverse. Avulsions of the peroneus brevis are most commonly seen with inversion ankle sprains and may be difficult to differentiate radiographically from apophysitis. The os vesalianum is an accessory bone found proximal to the base of the fifth metatarsal within the peroneus brevis tendon.21 Its smooth and sclerotic appearance may help to differentiate from a recent fracture. Dameron21 found these in only 1 of 1000 foot radiographs.
Treatment includes activity modifications, crutch weightbearing, nonsteroidal anti-inflammatories, stretching and strengthening exercises, bracing, and immobilization. In a case report by Ralph et al,60 a patient developed a nonunion of the apophysis, which led to excision of the proximal bony fragment.
A short leg cast may provide the quickest resolution of symptoms, and it may resolve the issue of compliance with adolescents. After 4 weeks of immobilization, a program of peroneal stretching and strengthening can begin.
Conclusion
Adolescents can sustain physeal, apophyseal, and bony stress injuries. The clinician must be aware that not all overuse injuries in children are to the growth plate. Many times, recovery is quickest if the injury is immobilized until the patient is pain-free, typically about 4 weeks. Early diagnosis will lead to a quicker recovery and return to sporting activity. The clinician must be aware that not all overuse injuries are to the growth plate. Injuries of the bones in the hand, elbow, and foot, when diagnosed early, respond to rest and treatment. If diagnosis is delayed, prolonged healing is expected.
Footnotes
No potential conflict of interest declared.
References
- 1. Adams JE. Injury to the throwing arm: a study of traumatic changes in the elbow joints of boy baseball players. Calif Med. 1965;102:127-132 [PMC free article] [PubMed] [Google Scholar]
- 2. Adams JE. Little League shoulder: osteochondrosis of the proximal humeral epiphysis in boy baseball pitchers. Calif Med. 1966;105:22-25 [PMC free article] [PubMed] [Google Scholar]
- 3. Anderson K, Strickland SM, Warren R. Hip and groin injuries in athletes. Am J Sports Med. 2001;29:521-533 [DOI] [PubMed] [Google Scholar]
- 4. Auberge T, Zenny JC, Duvallet A, Godefroy D, Horreard P, Chevrot A. Bone maturation and osteoarticular lesions in top level sportsmen: apropos of 105 cases [in French]. J Radiol. 1984;65:555-561 [PubMed] [Google Scholar]
- 5. Barnett LS. Little League shoulder syndrome: proximal humeral epiphyseolysis in adolescent baseball pitchers: a case report. J Bone Joint Surg Am. 1985;67:495-496 [PubMed] [Google Scholar]
- 6. Baumgarten TE, Andrews JR, Satterwhite YE. The arthroscopic classification and treatment of osteochondritis dissecans of the capitellum. Am J Sports Med. 1998;26:520-523 [DOI] [PubMed] [Google Scholar]
- 7. Blankstein A, Cohen I, Heim M, et al. Ultrasonography as a diagnostic modality in Osgood-Schlatter disease: a clinical study and review of the literature. Arch Orthop Trauma Surg. 2001;121:536-539 [DOI] [PubMed] [Google Scholar]
- 8. Brandser EA, el-Khoury GY, Kathol MH, Callaghan JJ, Tearse DS. Hamstring injuries: radiographic, conventional tomographic, CT, and MR imaging characteristics. Radiology. 1995;197:257-262 [DOI] [PubMed] [Google Scholar]
- 9. Bright RW, Burstein AH, Elmore SM. Epiphyseal-plate cartilage: a biomechanical and histological analysis of failure modes. J Bone Joint Surg Am. 1974;56:688-703 [PubMed] [Google Scholar]
- 10. Brogdon BG, Crow NE. Little Leaguer’s elbow. Am J Roentgenol. 1960;83:671-675 [PubMed] [Google Scholar]
- 11. Cahill BR, Tullos HS, Fain RH. Little League shoulder: lesions of the proximal humeral epiphyseal plate. J Sports Med. 1974;2:150-152 [DOI] [PubMed] [Google Scholar]
- 12. Cain EL, Jr, Dugas JR, Wolf RS, Andrews JR. Elbow injuries in throwing athletes: a current concepts review. Am J Sports Med. 2003;31:621-635 [DOI] [PubMed] [Google Scholar]
- 13. Caine D, Cochrane B, Caine C, Zemper E. An epidemiologic investigation of injuries affecting young competitive female gymnasts. Am J Sports Med. 1989;17:811-820 [DOI] [PubMed] [Google Scholar]
- 14. Caine D, Roy S, Singer KM, Broekhoff J. Stress changes of the distal radial growth plate: a radiographic survey and review of the literature. Am J Sports Med. 1992;20:290-298 [DOI] [PubMed] [Google Scholar]
- 15. Canale ST, Williams KD. Iselin’s disease. J Pediatr Orthop. 1992;12:90-93 [PubMed] [Google Scholar]
- 16. Carson WG, Gasser SI. Little Leaguer’s shoulder: a report of 23 cases. Am J Sports Med. 1998;26(4):575-580 [DOI] [PubMed] [Google Scholar]
- 17. Carter SR, Aldridge MJ, Fitzgerald R, Davies AM. Stress changes of the wrist in adolescent gymnasts. Br J Sports Med. 1988;61(722):109-112 [DOI] [PubMed] [Google Scholar]
- 18. Cavalier R, Herman MJ, Cheung EV, Pizzutillo PD. Spondylolysis and spondylolisthesis in children and adolescents, I: diagnosis, natural history, and nonsurgical management. J Am Acad Orthop Surg. 2006;14:417-424 [DOI] [PubMed] [Google Scholar]
- 19. Ciulio JV, Jackson DW. Pars interarticularis stress reaction, spondylolysis, and spondylolisthesis in gymnasts. Clin Sports Med. 1985;4:95-110 [PubMed] [Google Scholar]
- 20. Clancy WG, Jr, Foltz AS. Iliac apophysitis and stress fractures in adolescent runners. Am J Sports Med. 1976;4:214-218 [DOI] [PubMed] [Google Scholar]
- 21. Dameron TB., Jr Fractures and anatomical variations of the proximal portion of the fifth metatarsal. J Bone Joint Surg Am. 1975;57:788-792 [PubMed] [Google Scholar]
- 22. Danielsson LG, Hedlund ST, Henricson AS. Apophysitis of the olecranon: a report of four cases. Acta Orthop Scand. 1983;54:777-778 [DOI] [PubMed] [Google Scholar]
- 23. Dotter WE. Little Leaguer’s shoulder: a fracture of the proximal epiphysial cartilage of the humerus due to baseball pitching. Guthrie Clin Bull. 1953;23(1):68-72 [PubMed] [Google Scholar]
- 24. Ehrenborg G, Lagergren C. Roentgenologic changes in the Osgood-Schlatter lesion. Acta Chir Scand. 1961;121:315-327 [PubMed] [Google Scholar]
- 25. Flowers MJ, Bhadreshwar DR. Tibial tuberosity excision for symptomatic Osgood-Schlatter disease. J Pediatr Orthop. 1995;15:292-297 [DOI] [PubMed] [Google Scholar]
- 26. Gerber SD, Griffin PP, Simmons BP. Break dancer’s wrist. J Pediatr Orthop. 1986;6:98-99 [DOI] [PubMed] [Google Scholar]
- 27. Gholve PA, Scher DM, Khakharia S, Widmann RF, Green DW. Osgood Schlatter syndrome. Curr Opin Pediatr. 2007;19:44-50 [DOI] [PubMed] [Google Scholar]
- 28. Goldstein JD, Berger PE, Windler GE, Jackson DW. Spine injuries in gymnasts and swimmers: an epidemiologic investigation. Am J Sports Med. 1991;19:463-468 [DOI] [PubMed] [Google Scholar]
- 29. Hang DW, Chao CM, Hang YS. A clinical and roentgenographic study of Little League elbow. Am J Sports Med. 2004;32:79-84 [DOI] [PubMed] [Google Scholar]
- 30. Harsha WN. Effects of trauma upon epiphyses. Clin Orthop. 1957;10:140-147 [PubMed] [Google Scholar]
- 31. Heneghan MA, Wallace T. Heel pain due to retrocalcaneal bursitis-radiographic diagnosis (with an historical footnote on Sever’s disease). Pediatr Radiol. 1985;15:119-122 [DOI] [PubMed] [Google Scholar]
- 32. Hensinger RN. Standards in Pediatric Orthopedics: Tables, Charts, and Graphs. New York, NY: Raven Press; 1986:295-296 [Google Scholar]
- 33. Hirano A, Fukubayashi T, Ishii T, Ochiai N. Magnetic resonance imaging of Osgood-Schlatter disease: the course of the disease. Skeletal Radiol. 2002;31:334-342 [DOI] [PubMed] [Google Scholar]
- 34. Hoppenfeld S, DeBoer P, Thomas HA. Surgical Exposures in Orthopaedics: The Anatomic Approach. Vol 3 Philadelphia, PA: Lippincott Williams & Wilkins; 2003:345-364 [Google Scholar]
- 35. Hunter LY, O’Connor GA. Traction apophysitis of the olecranon: a case report. Am J Sports Med. 1980;8:51-52 [DOI] [PubMed] [Google Scholar]
- 36. Ikata T, Miyake R, Katoh S, et al. Pathogenesis of sports-related spondylolisthesis in adolescents: radiographic and magnetic resonance imaging study. Am J Sports Med. 1996:24:94-98 [DOI] [PubMed] [Google Scholar]
- 37. Inagaki H, Inoue G. Stress fracture of the scaphoid combined with the distal radial epiphysiolysis. Br J Sports Med. 1997;31:256-257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Iselin H. Wachtumsbeschwerden zur zeit dur knochernen entwicklung der tuberositas metatarsi quint. Deutsch Zeit Chir. 1912;117:529-535 [Google Scholar]
- 39. Klingele KE, Kocher MS. Little League elbow: valgus overload injury in the paediatric athlete. Sports Med. 2002;32:1005-1015 [DOI] [PubMed] [Google Scholar]
- 40. Kobayashi K, Burton KJ, Rodner C, Smith B, Caputo AE. Lateral compression injuries in the pediatric elbow: Panner’s disease and osteochondritis dissecans of the capitellum. J Am Acad Orthop Surg. 2004;12:246-254 [DOI] [PubMed] [Google Scholar]
- 41. Kujala UM, Kvist M, Heinonen O. Osgood-Schlatter’s disease in adolescent athletes: retrospective study of incidence and duration. Am J Sports Med. 1985;13:236-241 [DOI] [PubMed] [Google Scholar]
- 42. Kujala UM, Orava S, Karpakka J, Leppavuori J, Mattila K. Ischial tuberosity apophysitis and avulsion among athletes. Int J Sports Med. 1997;18:149-155 [DOI] [PubMed] [Google Scholar]
- 43. Lombardo SJ, Retting AC, Kerlan RK. Radiographic abnormalities of the iliac apophysis in adolescent athletes. J Bone Joint Surg Am. 1983;65:444-446 [PubMed] [Google Scholar]
- 44. Maffulli N, Chan D, Aldridge MJ. Overuse injuries of the olecranon in young gymnasts. J Bone Joint Surg Br. 1992;74:305-308 [DOI] [PubMed] [Google Scholar]
- 45. Mandelbaum BR, Bartolozzi AR, Davis CA, Teurlings L, Bragonier B. Wrist pain syndrome in the gymnast: pathogenetic, diagnostic, and therapeutic considerations. Am J Sports Med. 1989;17:305-317 [DOI] [PubMed] [Google Scholar]
- 46. Mannor DA, Lindenfeld TN. Spinal process apophysitis mimics spondylolysis: case reports. Am J Sports Med. 2000;28:257-260 [DOI] [PubMed] [Google Scholar]
- 47. Meister K, Day T, Horodyski M, Kaminski TW, Wasik MP, Tillman S. Rotational motion changes in the glenohumeral joint of the adolescent/Little League baseball player. Am J Sports Med. 2005;33:693-698 [DOI] [PubMed] [Google Scholar]
- 48. Micheli LJ, Ireland ML. Prevention and management of calcaneal apophysitis in children: an overuse syndrome. J Pediatr Orthop. 1987;7:34-38 [DOI] [PubMed] [Google Scholar]
- 49. Mihara K, Tsutsui H, Nishinaka N, Yamaguchi K. Nonoperative treatment for osteochondritis dissecans of the capitellum. Am J Sports Med. 2009;37:298-304 [DOI] [PubMed] [Google Scholar]
- 50. Mital MA, Matza RA, Cohen J. The so-called unresolved Osgood-Schlatter lesion: a concept based on fifteen surgically treated lesions. J Bone Joint Surg Am. 1980;62:732-739 [PubMed] [Google Scholar]
- 51. Morita T, Ikata T, Katoh S, et al. Lumbar spondylolysis in children and adolescents. J Bone Joint Surg Br. 1995;77:620-625 [PubMed] [Google Scholar]
- 52. Ogden JA, Ganey TM, Hill JD, Jaakkola JI. Sever’s injury: a stress fracture of the immature calcaneal metaphysis. J Pediatr Orthop. 2004;24:488-492 [DOI] [PubMed] [Google Scholar]
- 53. Ogden JA, Southwick WO. Osgood-Schlatter’s disease and tibial tuberosity development. Clin Orthop Relat Res. 1976;116:180-189 [PubMed] [Google Scholar]
- 54. Orava S, Malinen L, Karpakka J, et al. Results of surgical treatment of unresolved Osgood-Schlatter lesion. Ann Chir Gynaecol. 2000;89:298-302 [PubMed] [Google Scholar]
- 55. Osgood RB. Lesions of the tibial tubercle occuring during adolescence. Boston Med Surg J. 1903;148:114-117 [PubMed] [Google Scholar]
- 56. Paletta GA, Jr, Andrish JT. Injuries about the hip and pelvis in the young athlete. Clin Sports Med. 1995;14:591-628 [PubMed] [Google Scholar]
- 57. Paluska SA. An overview of hip injuries in running. Sports Med. 2005;35:991-1014 [DOI] [PubMed] [Google Scholar]
- 58. Pointinger H, Munk P, Poeschl GP. Avulsion fracture of the anterior superior iliac spine following apophysitis. Br J Sports Med. 2003;37:361-362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Pritchett JW. Growth plate activity in the upper extremity. Clin Orthop Relat Res. 1991;268:235-242 [PubMed] [Google Scholar]
- 60. Ralph BG, Barrett J, Kenyhercz C, DiDomenico LA. Iselin’s disease: a case presentation of nonunion and review of the differential diagnosis. J Foot Ankle Sur. 1999;38:409-416 [DOI] [PubMed] [Google Scholar]
- 61. Risser JC. The Iliac apophysis: an invaluable sign in the management of scoliosis. Clin Orthop. 1958;11:111-119 [PubMed] [Google Scholar]
- 62. Rossi F, Dragoni S. Acute avulsion fractures of the pelvis in adolescent competitive athletes: prevalence, location and sports distribution of 203 cases collected. Skeletal Radiol. 2001;30:127-131 [DOI] [PubMed] [Google Scholar]
- 63. Roy S, Caine D, Singer KM. Stress changes of the distal radial epiphysis in young gymnasts: a report of twenty-one cases and a review of the literature. Am J Sports Med. 1985;13:301-308 [DOI] [PubMed] [Google Scholar]
- 64. Sabick MB, Kim YK, Torry MR, Keirns MA, Hawkins RJ. Biomechanics of the shoulder in youth baseball pitchers: implications for the development of proximal humeral epiphysiolysis and humeral retrotorsion. Am J Sports Med. 2005;33:1716-1722 [DOI] [PubMed] [Google Scholar]
- 65. Schlatter C. Verletzunger des schnabelformigen fortsatzes der oberen tibiaepiphse. Beitr Klin Chir. 1903;38:874-887 [Google Scholar]
- 66. Scopp JM, Moorman CT., III The assessment of athletic hip injury. Clin Sports Med. 2001;20:647-659 [DOI] [PubMed] [Google Scholar]
- 67. Sever JW. Apophysitis of the os calcis. NY Med. 1912;95:1025-1029 [Google Scholar]
- 68. Steerman JG, Reeder MT, Udermann BE, Pettitt RW, Murray SR. Avulsion fracture of the iliac crest apophysis in a collegiate wrestler. Clin J Sports Med. 2008;18:102-103 [DOI] [PubMed] [Google Scholar]
- 69. Takahara M, Mura N, Sasaki J, Harada M, Ogino T. Classification, treatment, and outcome of osteochondritis dissecans of the humeral capitellum. J Bone Joint Surg Am. 2007;89:1205-1214 [DOI] [PubMed] [Google Scholar]
- 70. Takahara M, Ogino T, Takagi M, Tsuchida H, Orui H, Nambu T. Natural progression of osteochondritis dissecans of the humeral capitellum: initial observations. Radiology. 2000;216:207-212 [DOI] [PubMed] [Google Scholar]
- 71. Thomis M, Claessens AL, Lefevre J, Philippaerts R, Beunen GP, Malina RM. Adolescent growth spurts in female gymnasts. J Pediatr. 2005;146:239-244 [DOI] [PubMed] [Google Scholar]
- 72. Vender MI, Watson HK. Acquired Madelung-like deformity in a gymnast. J Hand Surg. 1988;13:19-21 [DOI] [PubMed] [Google Scholar]
- 73. Volpon JB, de Carvalho Filho G. Calcaneal apophysitis: a quantitative radiographic evaluation of the secondary ossification center. Arch Orthop Trauma Surg. 2002;122:338-341 [DOI] [PubMed] [Google Scholar]
- 74. Yadao MA, Field LD, Savoie FH., III Osteochondritis dissecans of the elbow. Instr Course Lect. 2004;53:599-606 [PubMed] [Google Scholar]
- 75. Yong-Hing K, Wedge JH, Bowen CV. Chronic injury to the distal ulnar and radial growth plates in an adolescent gymnast: a case report. J Bone Joint Surg Am. 1988;70:1087-1089 [PubMed] [Google Scholar]





