Abstract
Objectives:
The purpose of this community-based participatory research was to compare different training sources for adolescents’ menstrual health education.
Methods:
From 15 middle schools in Tehran, through quota random sampling, 1823 female students were selected proportionally and allocated randomly to three groups (parent trained, schools’ health trainers trained, and control). Following a two-year training program, the adolescents’ menstrual health was compared.
Results:
In the present study, the school health trainers trained group showed a better feeling for menarche, compared to the two other groups (P < 0.001). The need for adolescent health training was emphasized by 82% of the participants; they also believed that the appropriate age for such empowerment courses was about 12 years. In the school health trainers trained group, the offered age was significantly lower than in other groups (P < 0.001). The adolescents trained by the school health trainers had a better practice of habits related to menstrual and hygiene practices, like having a bath during menstruation and the use of sanitary pads or cotton, compared to their counterpart groups (P > 0.05).
Conclusion:
It is suggested that school-based health training leads to better menstrual health promotion and healthy puberty transition, and school health trainers play a key role in this regard.
Keywords: Adolescents, health, menstrual
INTRODUCTION
Adolescence is a transitional stage with major physical and psychological changes. It is estimated that there are 1.2 billion adolescents in the world today.[1] In Iran more than 27% of the population is composed of the age group between 10 and 15 years, which certainly has an important role in the future of the country's development.[2] Although, adolescents involve in special problems that threaten their health, a national study in Iran showed that a few interventional programs were conducted on the adolescents’ health.[3] Unfortunately, myths, irrational beliefs, and cultural taboos form barriers for adolescent reproductive health. Some studies in developing countries, proposed that reproductive health educational programs should be considered as the best route to take, to meet adolescent knowledge needs.[4,5] In one study, 84% of the participants expressed that adolescents should be given reproductive training, whereas, only 48.3% of them had received any. They supposed that this educational program should be carried out in schools through reliable sources.[6,7] In Iranian girls, the puberty stage begins at around 10 years, with a median age of menarche at 13 years.[8] If adolescents have not received the proper required training at the appropriate time, it is possible that menarche could lead to some critical situations such as stress, anxiety, or unhealthy behavior. A study showed that 72% of the adolescents required to be trained particularly on reproductive health subjects. The most interesting subjects discussed were questionable topics of reproductive physiology and reproductive health.[9] Therefore, according to the perceptible needs and scientific suggestions, school-based training programs should be considered as the most effective adolescent health promotion approaches.[10]
Parents, especially mothers, and health trainers of schools have a unique practical position, with the highest degree of influence, for providing safe and affective adolescent health training services. From this perspective, they are an available and reliable resource for health-related notifications that should be responsible for a fundamental role in the promotion of healthy behavior. In this regard, the American Medical Association aims to improve adolescent compatibility based on puberty, and precautionary strategies have been attended to, for parents’ empowerment in the assessment of adolescents’ needs.[11]
Complementary plans are the essential requirements for adolescent health promotion, which could be realized through; community partnership, health training development, capacity building, safe and supportive environment, and appropriate and accessible health counseling services.[12]
Considering the above, we conducted an interventional participatory study in partnership with the adolescents’ mothers and health trainers of target middle schools. This article aimed to compare the effects of these different training methods on the adolescents’ reproductive health promotion for designing and implementing the most proper reproductive health training program.
METHODS
This community-based health education intervention was implemented by a multidisciplinary approach under the supervision of the Deputy of Research and Technology, Ministry of Health and Medical Education, Tehran, Iran.
By considering a confidence interval of 95% and alpha 0.5, the sample size was calculated as 1800. In the first year of study, 95250 female students had trained in Tehran's middle schools. The participants were recruited through quota random sampling. Among five regions of Tehran; north, south, east, west, and the central part, 15 middle schools had been selected randomly and then according to the size of the school population, 1823 female students, 11 to 15 years of age, were selected proportionally from the middle school students for final analysis of the training interventional results. For the inclusion criteria we considered the teens that were interested in research participation and were studying in middle school from the start of study. Students who entered school after the start of the study were excluded from the final assessment. Also, adolescents with a history of being diagnosed with a disease were excluded.
As it was a vast multidimensional study on various aspects of adolescent health, this article consists of the comparison of the roles of parents and health trainers of schools in adolescent reproductive health promotion, at the end of study.
At first we conducted a survey on the menstrual health of the participants. After that the participants were randomly divided into three groups. The first group was considered as the control group, without any intervention. The second group was trained by the school health trainers, who were themselves trained by project experts; and the third group received designed training through their parents. It is mentioned that only for the third group their parents were trained by project experts, with emphasis on puberty health. Following the interventional health training plan, the adolescents’ knowledge of puberty and menstrual health was assessed.
Participation in this survey was voluntary and self-administered questionnaires were filled anonymously, after explanation of the objectives of the study to every participant, and a verbal consent obtained.
The questionnaire was designed by the scientific committee, based on the related literature and goals of the study. The main questionnaire included 93 closed questions on various aspects of adolescent health, including demographic data, nutritional habits, exercise, communication and interpersonal relationship, mental and spiritual health, and adolescent health, with an emphasis on menstrual health.
In this article, we focused on 34 menstrual health-related questions, which were analyzed to compare the knowledge of puberty and menstrual health in the three groups. The extracted data have been reviewed in the following five topics.
Menarche experience: Good feeling at the moment of menarche (happy or proud and thankful); Appropriate actions (being informed and prepared by her mother, grandmother, doctor).
Menstrual information: Information resource; attitude about adolescent health education requirements.
Menstrual and hygiene practices: Proper menstrual hygiene (bathing and washing during the period of menstruation after each urination and defecation, and use of sanitary pad or cotton).
Menstrual pain: The right action to recover (refer to the doctor). In the pilot study, reliability and validity of instruments were conceptualized .The validity of the questionnaire was confirmed through the peer-reviewed literature by ten experts and its reliability was established with the test–retest
In the final evaluation after three years, we evaluated about a 5% loss to follow-up .The main reason was changing the school from the selected schools during the study and in rare cases being busy on the day of the final assessment. Overall, among the final completed questionnaires, the response rate was 95%. Among some questions of menstrual health, the response rate depended on having the menarche experience. For that reason, the number of respondents in different subjects was different.
Data analyses were processed by the use of the SPSS software version 16 (Chicago IL USA). Descriptive statistics with the chi-squared (χ2) test and ANOVA was used for analysis. Statistical significance level was set at P < 0 / 05 (two tailed).
RESULTS
Following a two-year intervention, information on 1231 female adolescents was included for assessment. The mean age of the students in the control group was 11.8 ± 1.3 (Mean ± SD) and in the adolescent groups trained by school health trainers and by parents, the mean age was 11.65 ± 0.51 and 11.62 ± 0.59 (Mean ± SE), respectively.
More than 80% of the participants in each group had one sister or brother. Most of the students’ parents had a high school diploma and only about 30% of the fathers and 20% of the mothers had graduated from university. Mothers’ and fathers’ highest educational levels were significantly correlated (r = 0.68, P < 0.001).
ANOVA with P < 0.05 showed that there was no significant difference between Weight, Height, BMI, and around the wrist in the three groups.
This study finding showed that 52.7% of the participants had experienced menarche at the last evaluation phase of intervention. In this regard, there was no significant difference between the groups (iIn control, trained by school health trainers, and trained by parents groups, respectively, it was 52.5, 52.1, and 53.5%), but the T-test showed that the girls who had experienced menarche had more BMI than the others (19.84 kg / m2 vs. 18.13 kg / m2, P < 0.0001).
In 73.5% of the participant students, the first menstruation had occurred at home, whereas overall, 52.8% of them had experienced a scared and bad feeling. The Chi Square Test showed a significant difference between the feelings of the respondents at the menarche (P < 0.001).
Table 1 shows that there was an uncomfortable, scared, and confused feeling in the control group and a good feeling in the school health trainers trained group were happened more than other groups (P < 0.001). In the trained groups, the appropriate actions at the time of the first menstrual bleeding were more than in the control group, but the difference was not statistically significant (Trained group by school health trainers 38.5% and trained group by parents 34% vs. control group 27.5%). The need for adolescent health training was emphasized by 82% of the participants; they also believed that the appropriate age for such empowerment courses should be about 12 years. ANOVA Test with P < 0.05 showed, based on the view point of the group trained by the school health trainers, that the mean appropriate age for adolescent health education was significantly lower than other groups (11.9 years vs. 12.4 and 12.05 years).
Table 1.
Menstrual experience

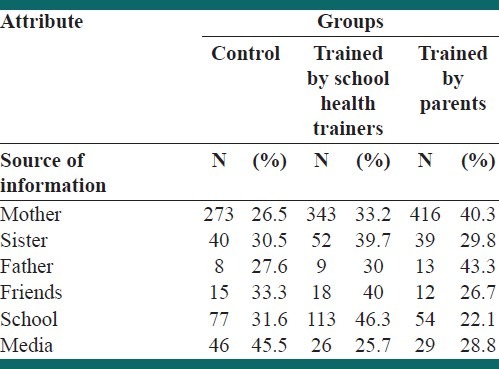
Mothers were introduced as the most proper resource for information. As shown in Table 2, in adolescents trained by school health trainers and parents, respectively, the “school” and “mother” have recommended more than other information resource.
Table 2.
Menstrual information
Related to menstrual and hygiene practices [Table 3], 71.7% of the participants had a bath during menstruation. The reasons for not having a bath were relatives′ recommendation (43.5%), fear of pain (28.7%), fear of sickness (22.7%), and unavailable bathroom (5.1%). In the trained groups, especially in the adolescents trained by school health trainers, bathing during menstruation was more frequent than others; 71.9% of the adolescents usually washed themselves after each urination and defecation, and this habit was higher in educated groups than in the control group (P > 0.05).
Table 3.
Menstrual and hygiene practices

Data analysis revealed that the use of sanitary pad or cotton during menstruation was higher in the trained groups when compared with the other groups (P > 0.05).
It is worth mentioning that emotional change (27.5%), appetite change (24.6%), digestive disorders (3.6%) and headache, dizziness, and vomiting (44.3%) were seen among adolescents. Menstrual pain was reported in 68.1% of the respondents. Referring to the doctor as the right action to recover from the pain was mentioned by 24.5% of the participants, of whom 69.7% were in the trained groups.
Exercising during menstruation was reported by 36.4% of the participants, and most of them were in the school health trainers trained group (P < 0.05).
DISCUSSION
Adolescents experience significant physical and emotional changes around menstruation. Poor information about menstrual health leads them to inappropriate reactions to menarche. Menarche is an important milestone in a woman's life that can be a traumatic and uncomfortable experience. Menstrual health education can be presented by different and varied sources such as parents or friends; school health trainers aim for adolescent health promotion.[5,13]
Design and conduction of different approaches to the practical procedure of adolescent health promotion was realized through community-based interventional studies.[12]
In the present study, we benefited from having parents and school health trainers as mobilizers and key stakeholders in the participation of this community-based interventional program. Similarly in other related had emphasized on the effective role of other stakeholders participation in health promotion programs. They have also suggested that through such a targeted and coherent partnership synergistic capacities lead to more successful results in health implementation.[6]
Regarding the menarche experience, our study showed that 52.8% of our participants had experienced scared and bad feelings at the time of first menstruation. Similarly, another study described 51.4% anxiety and 26.6% shame at menarche.[14]
In the present study we have concluded that menstrual health training through parents and school health trainers leads to better experience of menarche. Eighty-two percent of our participants believe that adolescent health training should be given the highest priority; meanwhile the appropriate age for such capacity building is 12 years. Regarding the above, a study demonstrated that menstrual education before menarche leads to a positive attitude regarding menarche in adolescents.[15] In many societies, menstruation is considered a very private subject and is not discussed openly in a family.[16] A study showed that 48.8% of the adolescents felt their menstruation was a secret.[17] This is more attention able point in menstrual hygiene training in schools.
Our study revealed that the use of sanitary pad or cotton during menstruation was higher in the trained groups compared tot he control group. In similar studies, research knowledge promotion regarding menstruation and menstrual hygiene, after educational intervention, led to better practice.[4]
Dysmenorrhea is an important and disturbing problem, which needs the right guidance to recover from the pain. The right action in this situation was seen more in the educated groups. Although menstrual pain is a common problem, in a Chinese study, only 5.9% of the adolescents received medical advice and most of them were offered traditional Chinese medications.[18]
In another subsequent study, the influence of menstruation on emotions (74.8%), daily life (73.1%), schoolwork (61.6%), and social interaction (50.1%) were highlighted more than in our study.[19]
There are many limitations in our study, which are as follows; there were little missing values in the data, especially for questions that were dependent on the experience of menarche. There were also limitations to the school-based approach. The school calendar generally contains nine months, which is less than the minimum of 12 months of mentoring recommended by those in the mentoring field. Lack of possibility of controlling the received information, which we were getting from other peripheral sources, was the latest limitation.
Adolescent health is important for normal transition from childhood to adulthood. Since conducting the interventional study and opening new opportunities for evaluating various situations and assessing the results, it was revealed why health-related messages were not as effective as expected among adolescents. The comparison of various adolescent health promotional methods helped to develop effective interventions. Appropriate health education, evidence-based policies, and parental and social support, helped to implement effective interventions.[10,20,21]
It is concluded that school health trainers play an essential role in knowledge transfer, attitude promotion, and practice betterment of female adolescents. Considering our experience, we conclude that school-based interventional programs provide the best situation for adolescents’ health promotion, but there is no doubt that more effective school-based health promotional programs are needed, to reduce the risk and improve adolescents’ health outcomes.
ACKNOWLEDGMENT
This project was led by the Deputy of Research and Technology, Ministry of Health and Medical Education of IR.IRAN, and supported by the United Nation Population Fund (UNFPA). The authors thank all participants for their cooperation and for sharing this experience.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Geneva: World Health Organization; 2010. [Last accessed on 2011 Jan 26]. Adolescence. Available from: http://www.who.int/child_adolescent_health/topics/prevention_care/adolescent/en/index.html . [Google Scholar]
- 2.Why do we need to invest in the health and development of adolescents? [Last accessed on 2010 Apr 02]. Available from: http://www.who.int/child_adolescent_health/topics/prevention_care/adolescent/en/index.html .
- 3.Reproductive Health Research Center. Ministry of Health and Medical Education. 2005. The study of conducted project among youth health promotion. Department of Research and Technology. [Google Scholar]
- 4.Peacock A, Alvi NS, Mushtaq T. Period problems: Disorders of menstruation in adolescents. Arch Dis Child. 2012;97:554–60. doi: 10.1136/adc.2009.160853. [DOI] [PubMed] [Google Scholar]
- 5.Sharma P, Malhotra C, Taneja DK, Saha R. Problems related to menstruation amongst adolescent girls. Indian J Pediatr. 2008;75:125–9. doi: 10.1007/s12098-008-0018-5. [DOI] [PubMed] [Google Scholar]
- 6.Adeokun LA, Ricketts OL, Ajuwon AJ, Ladipo OA. Sexual and reproductive health knowledge, behaviour and education needs of in-school adolescents in northern Nigeria. Afr J Reprod Health. 2009;13:37–49. [PubMed] [Google Scholar]
- 7.Groft JN, Hagen B, Miller NK, Cooper N, Brown S. Adolescent health: A rural community's approach. Rural Remote Health. 2005;5:366. [PubMed] [Google Scholar]
- 8.Kashani HH, Kavosh MS, Keshteli AH, Montazer M, Rostampour N, Kelishadi R, et al. Age of puberty in a representative sample of Iranian girls. World J Pediatr. 2009;5:132–5. doi: 10.1007/s12519-009-0026-1. [DOI] [PubMed] [Google Scholar]
- 9.Ryan SA, Millstein SG, Irwin CE. Puberty questions asked by early adolescents: What do they want to know? J Adolesc Health. 1996;19:145–52. doi: 10.1016/1054-139X(95)00326-N. [DOI] [PubMed] [Google Scholar]
- 10.Acharya DR, Van Teijlingen ER, Simkhada P. Opportunities and challenges in school-based sex and sexual health education in Nepal. Kathmandu Univ Med J (KUMJ) 2009;7:445–53. doi: 10.3126/kumj.v7i4.2773. [DOI] [PubMed] [Google Scholar]
- 11.American Medical Association. Guide lines for adolescent preventive services (GAPS) 1995. [Last accessed on 2011 Sep 20]. Available from: http://www.ama-assn.org/adolhlth/recommend/monogrfl.htm .
- 12.Brug J, Oenema A, Ferreira I. Theory, evidence and Intervention Mapping to improve behavior nutrition and physical activity interventions. Int J Behav Nutr Phys Act. 2005;2:2. doi: 10.1186/1479-5868-2-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chang YT, Chen YC, Hayter M, Lin ML. Menstrual and menarche experience among pubescent female students in Taiwan: implications for health education and promotion practice. J Clin Nurs. 2009;18:2040–8. doi: 10.1111/j.1365-2702.2008.02545.x. [DOI] [PubMed] [Google Scholar]
- 14.Mohammadzadeh Z, Allame Z, Shahroki S, Oriezi HR, Marasi MR. Puberty Health Education in Iranian Teenagers: Self -Learning or Lecture and Discussion Panel? Iran J Med Educ. 2002;4:3. [Google Scholar]
- 15.Skandhan KP, Pandya AK, Skandhan S, Mehta YB. Menarche: Prior knowledge and experience. Adolescence. 1988;23:149–54. [PubMed] [Google Scholar]
- 16.Aniebue U, Aniebue PN, Nwankwo TO. The impact of pre-menarcheal training on menstrual practices and hygiene of Nigerian school girls. Pan Afr Med J. 2009;2:29. [PMC free article] [PubMed] [Google Scholar]
- 17.Walker SP, Grantham-McGregor SM, Himes JH, Williams S, Duff EM. School performance in adolescent Jamaican girls: Associations with health, social and behavioral characteristics, and risk factors for drop out. J Adolesc. 1998;21:109–22. doi: 10.1006/jado.1997.0133. [DOI] [PubMed] [Google Scholar]
- 18.Agarwal A, Venkat A. Questionnaire study on menstrual disorders in adolescent girls in Singapore. J Pediatr Adolesc Gynecol. 2009;22:365–71. doi: 10.1016/j.jpag.2009.02.005. [DOI] [PubMed] [Google Scholar]
- 19.Chang YT, Chen YC. Menstrual health care behavior and associated factors among female elementary students in the Hualien region. J Nurs Res. 2008;16:8–16. doi: 10.1097/01.jnr.0000387285.23065.2d. [DOI] [PubMed] [Google Scholar]
- 20.Peykari N, Ramezani Tehrani F, Malekafzali H, Hashemi Z, Djalalinia Sh. An Experience of Peer Education Model among Medical Science University Students in Iran. Iran J Public Health. 2011;40:57–62. [PMC free article] [PubMed] [Google Scholar]
- 21.Peykari N, Tehrani FR, Baradaran Eftekhari MB, Malekafzali H, Dejman M, Neot R, et al. A peer-based study on adolescence nutritional health: A lesson learned from Iran. J Pak Med Assoc. 2011;61:549–54. [PubMed] [Google Scholar]


