Abstract
Hydrothorax as a result of pleuroperitoneal communication (PPC) is an uncommon but a well-known complication of continuous ambulatory peritoneal dialysis (CAPD). In this paper, we present a 60-year old man with diabetic renal failure who underwent CAPD. Two weeks after starting CAPD, chest radiographs showed a right-sided hydrothorax. Radioscintigraphy was performed and PPC was diagnosed. Eight days after the diagnosis, thoracoscopic surgery was performed. The leakage points were closed by direct suturing with absorbable polyglycolic acid felt and fibrin glue. The patient resumed CAPD 2 weeks later, and there was no recurrence of the right hydrothorax. Video-assisted thoracic surgery with direct suturing represents a feasible method for treating PPC with confirmed fistulae.
Keywords: Pleuroperitoneal communication, Continuous ambulatory peritoneal dialysis, Video-assisted thoracic surgery
INTRODUCTION
Hydrothorax is a well-known complication associated with continuous ambulatory peritoneal dialysis (CAPD), reportedly occurring in ∼2% of all patients undergoing CAPD in Japan [1]. Hydrothorax in these cases is caused by pleuroperitoneal communication (PPC), a so-called porous diaphragm syndrome, and requires early treatment; otherwise, CAPD should be converted to haemodialysis. We present here a surgically treated case of PPC that continued to undergo CAPD after surgery.
CASE
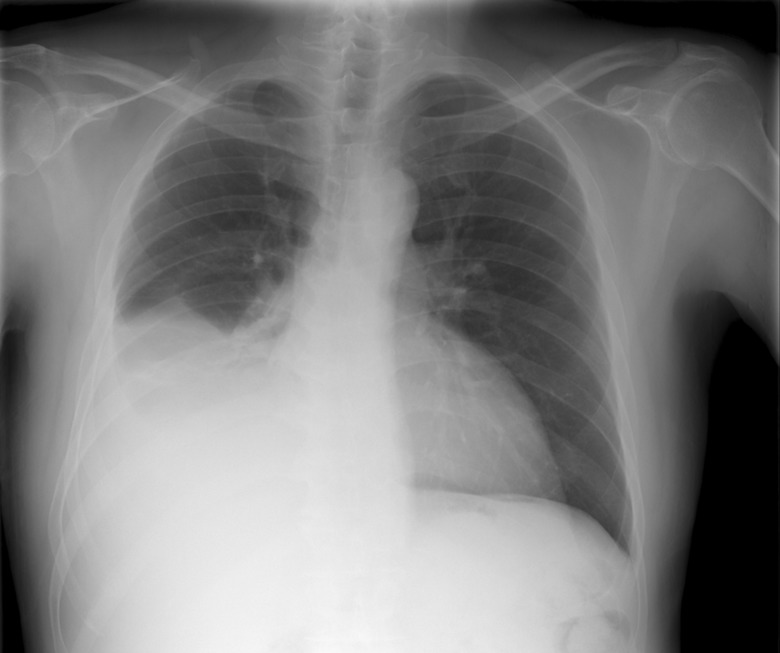
A 60-year old man with diabetic renal failure underwent CAPD in April 2011. Two weeks after starting CAPD, his chest radiographs showed a right-sided hydrothorax (Fig. 1). PPC was suspected, and radioscintigraphy was performed for diagnosis. 99mTc-macro-aggregated albumin was administered into the peritoneal cavity with a dialysate, and 15 min later, a leakage of the dialysate into the right pleural cavity was detected, confirming the presence of PPC. Thoracoscopic surgery was performed under general anaesthesia 8 days after the diagnosis. A volume of 2000 ml of dialysis solution containing 10 ml of indocyanine green (ICG) was injected into the abdominal cavity through the CAPD catheter just before the beginning of the surgery. The patient was positioned in a left-sided lateral decubitus position with separate lung ventilation. Three thoracoports were inserted, and the entire thoracic cavity was carefully inspected thoracoscopically. The preexisting pleural effusion gradually turned green and solid, and a small, thin membranous lesion was detected at the central tendon of the diaphragm by green staining (Fig. 2). The lesion was treated with a 3-0 absorbable monofilament suture in a mattress pattern. After treatment, the leakage of the ICG solution could not be detected. A sheet of absorbable polyglycolic acid felt (Neoveil) was fixed with fibrin glue onto the sutured lesion. The patient resumed CAPD 2 weeks later with the same volume of dialysate as previously used; however, there was no recurrence of the hydrothorax for >4 months.
Figure 1:
Chest radiograph shows a right-sided hydrothorax.
Figure 2:
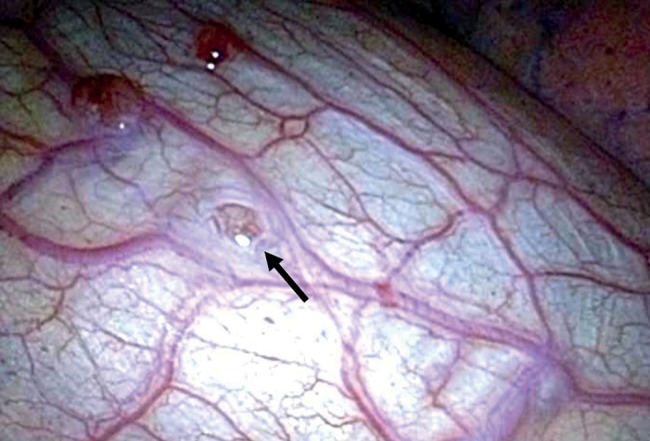
Thoracoscopic findings. A small pore was detected at the central tendon of the diaphragm (arrow). This site was stained with green gradually.
DISCUSSION
PPC occurs in 1.6–1.9% of patients who undergo CAPD, and approximately half of these patients are forced to permanently exchange CAPD for haemodialysis [1, 2]. Hydrothorax is usually right-sided and more prevalent in women, and involves cough, chest pain and dyspnoea, but it is sometimes asymptomatic [3]. Diagnosis is usually not difficult because of the close relationship between the increase in the pleural effusion and CAPD performance. A high level of glucose in the pleural effusion, which suggests the leakage of dialysis solutions that contain a high level of glucose, is one of the diagnostic markers. The definitive diagnosis involves proving the presence of PPC. The appearance of fistulae differs in cases with small defects and bleb-like or even thin walls. The detection of the leakage of the dialysis solution containing dyes or contrast materials is usually performed. Radioactive isotope examination, as performed in our case, may also contribute to the decisive evaluation of the disease.
Either a nonsurgical or a surgical approach is taken for the treatment of the disease. A decreased injection volume of dialysate or temporal cessation of CAPD may lead to the spontaneous healing of diaphragmatic fistulae. Pleurodesis with agents such as autologous blood, fibrin glue, minomycin, talc powder, Nocardia rubra cell-wall skeleton and OK-432 is reportedly effective for the protection against hydrothorax, prompting pleural adhesion. However, nonsurgical treatment reportedly fails to achieve a radical cure in about 50% of patients [3]. On the other hand, surgical treatment has the same advantage as that of nonsurgical treatment in terms of the possible direct closure of the fistula. In 1984, Pattison et al. reported the first case of surgical treatment using a Teflon patch for the fistula closure. In 1996, Di Bisceglie et al. [4] reported the usefulness of video-assisted thoracic surgery (VATS). VATS has become the standard procedure for the disease since then, with a curative rate of ∼90% to date [2]. Several surgical techniques have been reported, including direct suturing, resection with a stapler, mechanical pleurodesis with absorbable sheets or mesh, chemical pleurodesis with talc or other agents, ablation and so forth. These techniques are used either singly or combined with others. However, the recurrence rate is relatively high in cases in which the fistula is not detected during the operation. Shishido et al. [3] reviewed 24 Japanese cases of PPC complicating CAPD treated by VATS, and we summarized 29 cases of PPC, adding 5 cases from our institute, including the present case. The treatment success rate was 72%. According to the detection of fistulae in VATS, the success rate was 89% in 21 fistula-confirmed cases, but only 38% in 8 cases in which fistulae were not confirmed. A direct closure was performed in 20 cases; of which, 13 involved direct suturing and 7 involved stapling. Cerfolio and Bryant [5] report the usefulness of talc powdering by VATS in patients with a hepatic hydrothorax, with a success rate of >80% (33 of 41patients), when it is combined with repeat talc slurry through the chest tube. But definitive openings in the diaphragm were seen in only 12% (5 of 41patients).
Talc powder was not applied to the Japanese cases because talc is not commonly used in Japan. The lack of the use of talc may contribute to the low success rate in Japanese cases in which fistulae were not confirmed. Talc powdering by VATS may be more effective than suturing or stapling, particularly in cases in which the leakage is not confirmed during the operation.
CONCLUSIONS
VATS with direct suturing represents a feasible method for treating PPC with confirmed fistulae. The therapeutic effect can be determined intraoperatively, and peritoneal dialysis can be resumed early. If a fistula is not confirmed during the operation, talc powdering should be performed.
Conflict of interest: none declared.
REFERENCES
- 1.Nomoto Y, Suga T, Nakajima K, Sakai H, Osawa G, Ota K, et al. Acute hydrothorax in continuous ambulatory peritoneal dialysis – a collaborative study of 161 centers. Am J Nephrol. 1989;9:363–7. doi: 10.1159/000167997. [DOI] [PubMed] [Google Scholar]
- 2.Chow KM, Szeto CC, Li PK. Management options for hydrothorax complicating peritoneal dialysis. Semin Dial. 2003;16:389–94. doi: 10.1046/j.1525-139x.2003.16080.x. [DOI] [PubMed] [Google Scholar]
- 3.Shishido T, Ryuzaki M, Takimoto C, Kobayashi E, Handa M, Yamamoto T, et al. A case of recurrent hydrothorax complicating continuous ambulatory peritoneal dialysis after video-assisted thoracoscopic surgery. J Jpn Soc Dial Ther. 2010;43:873–9. [Google Scholar]
- 4.Di Bisceglie M, Paladini P, Voltolini L, Garosi G, Ghiribelli C, Di Paolo N, et al. Videothoracoscopic obliteration of pleuroperitoneal fistula in continuous ambulatory peritoneal dialysis. Ann Thorac Surg. 1996;62:1509–10. doi: 10.1016/0003-4975(96)00544-9. [DOI] [PubMed] [Google Scholar]
- 5.Cerfolio RJ, Bryant AS. Efficacy of vido-assisted thoracoscopic surgery with talc pleurodesis for porous diaphragm syndrome in patients with refractory hepatic hydrothorax. Ann Thorac Surg. 2006;82:457–9. doi: 10.1016/j.athoracsur.2006.03.057. [DOI] [PubMed] [Google Scholar]