Abstract
Lymphorrhea is a rare but potentially serious complication following various surgical procedures. Uncontrolled lymph drainage may lead to infection and prolonged hospital stay. Currently, there is no standard effective treatment. Early management usually involves bed rest, drainage and pressure dressings. These methods are associated with prolonged recovery and high recurrence rates. We report a case of lymphorrhea from the groin wound after an aortic valve replacement. The patient presented with significant lymph drainage from the postoperative inguinal wound. Lymphorrhea was successfully treated with a long-acting somatostatin analogue, lanreotide. No recurrence was observed after 1 and 6 months of patient follow-up. This case report demonstrates the successful use of lanreotide in the control of lymphorrhea following groin dissection for vascular access.
Keywords: Aortic valve replacement, Lymphorrhea, Somatostatin analogues, Lanreotide
INTRODUCTION
Lymphorrhea is an abnormal flow of lymph that drains externally from disrupted lymphatic vessels or is retained within a wound. Lymphorrhea is an uncommon but potentially serious complication following a surgical dissection and inadequate closure of lymphatic vessels after surgery. Untreated lymphorrhea may lead to lymphatic complications and infections. Currently, the treatment is not standardized.
Beneficial effects of a somatostatin analogue, octreotide, in the treatment of postoperative lymphorrhea have been previously reported [1–3]. Here, we report the successful use of a long-acting somatostatin analogue, lanreotide, as a new treatment of lymphorrhea following an aortic valve replacement.
CASE REPORT
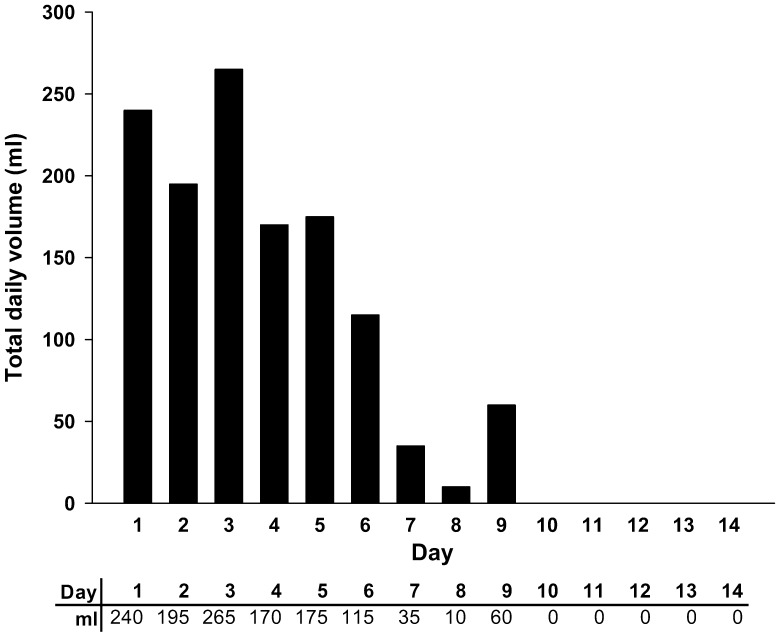
A 67-year old Caucasian man underwent an aortic valve replacement due to an aortic root aneurysm. He had previously suffered from hypertension, treated with bisoprolol (Isoten™), furosemide (Lasix™) and potassium canrenoate (Canrenol™), and atrial fibrillation, treated with acenocoumarol (Sintrom™), amiodarone (Cordarone™) and digoxin (Lanoxin™). He had also been suffering for many years from rheumatoid arthritis, treated with low-dose methylprednisolone (Medrol™, 4 mg) both pre- and postoperatively. Twelve weeks after the surgery, the patient presented in our hospital with continuous significant lymph leakage from the wound at the site of inguinal incision. A swab taken from the wound tested negative for infection. To target lymphorrhea, we chose lanreotide Autogel™ (Somatuline Autogel Injectable™ 120 mg, Ipsen), as it is administered once a month deeply subcutaneously and its action begins the day of injection. Draining lymph was collected in a Urinocol™ bag (B.Braun, France). The volume of collected lymph was measured each day starting one day after the lanreotide Autogel™ injection. On the first day of recording, the total amount of fluid was 240 ml. Over the next 8 days, the lymphorrhea persisted, but gradually reduced to half the initial lymph volume (115 ml) 6 days after the injection, before dropping to 10 and 60 ml, on Days 8 and 9, respectively. Ten days after the lanreotide Autogel™ administration, the leakage stopped; no further lymph collection was recorded over the next 4 days (Fig. 1). Over the 7 following days the leakage did not relapse and the Urinocol™ bag was removed. Patient follow-up 1 and 6 months after the surgery revealed no recurrence of lymphorrhea.
Figure 1:
Total daily volume of lymph (ml) collected from the patient 1–14 days after the administration of lanreotide Autogel™.
DISCUSSION
The incidence of postoperative lymphorrhea varies depending on the type of surgical procedure and site of incision. Uncontrolled lymphorrhea may lead to the subcutaneous collection of lymphatic fluid (lymphocele) or to a draining lymphatic fistula. Such lymphatic complications delay wound healing, increasing the incidence of wound infections and postoperative morbidity. Until now there has been no consensus on the most effective treatment of lymphorrhea. A standard approach involves bed rest, leg elevation, prophylactic antibiotics and simple drainage with or without pressure dressings. However, these methods entail a high recurrence rate and often fail to control the lymphatic leak, leading to prolonged hospital stays, increased risk of infection and thus, increased costs [2, 3]. More invasive procedures such as repeated aspiration or injection of sclerosing agents may be painful and further increase the risk of infection. If these fail, surgical interventions are sometimes considered, but are associated with risk of bleeding, infection, increased morbidity and surgery failure. Despite these current treatment options, lymphorrhea remains difficult to manage and may result in more severe lymphatic complications and, consequently, prolonged hospital stays and decreased quality of life [2, 3].
Here, we report the successful use of the synthetic somatostatin analogue, lanreotide, in the management of a patient with postoperative lymphorrhea. Following lanreotide Autogel™ administration, the volume of draining lymph was markedly reduced within 7 days, and abolished by Day 10. To our knowledge, there has been one previous report of the use of lanreotide in the treatment of para-aortic lymphocele after pelvic lymphadenectomy [4]. In this previous case report, the lymph flow from the patient's postoperative wound dropped dramatically from 300 to 90 ml one day after lanreotide injection and decreased gradually over the next 3 days. Lanreotide Autogel™ is currently used for the treatment of acromegaly and symptoms associated with carcinoid syndrome. The main side effects include gastrointestinal disturbances, gallstone formation and hyperglycaemia. However, no side effects were observed in the previous or this case report.
Another synthetic somatostatin analogue, octreotide, has been used in the successful management of lymphatic leaks after axillary [1] and pelvic [2] lymph node dissection or renal transplantation [3]. Beneficial effects of octreotide in the treatment of lymphorrhea after axillary lymph node dissection in breast cancer patients were demonstrated in a randomized controlled clinical trial [1]. In this previous study, significantly lower amounts and shorter duration of lymphorrhea were observed in patients treated with octreotide compared with patients treated using conservative methods (control group). Similar effects of octreotide have been observed in the treatment of lymphorrhea after pelvic lymph node dissection and after renal transplantation [2, 3]. The mean duration of lymphorrhea or lymph drainage (until lymphorrhea was <50 ml/day) in these studies varied between 7.1 and 8.9 days in patients treated with octreotide, and between 12.1 and 16.7 days in the control groups [1–3]. The mean length of hospital stay was also reported to be shorter in treated groups [2, 3], with Kim et al. [2] reporting 9.9 (±3.1) and 14.9 (±3.9) days in treated and control groups, respectively (specific data were not provided by Capocasale et al. [3]). Additionally, one of these studies showed a trend for a lower rate of postoperative complications in the treated group than in the control group [1]. The nature of these studies and the treatment doses differ, making comparisons between them difficult. The reduced volume and duration of lymph drainage, however are in line with those observed in our patient.
The precise mechanism by which somatostatin analogues affect lymphorrhea is unknown. Somatostatin, a tetrapeptide hormone, is widely distributed within the nervous and the gastroentero-pancreatic system. To date, a direct effect of somatostatin on the lymph flow has only been observed in the gastrointestinal track [1]. However, somatostatin receptors have been found in lymphatic tissues, within and outside of the gastrointestinal track. Therefore, it is possible that these drugs exert a direct effect on lymphatic vessels to reduce lymph production [5].
CONCLUSIONS
Our report supports the use of lanreotide Autogel™ as an effective first-line therapy in the management of postoperative lymphorrhea. Potential benefits include not only reduction of the volume and duration of lymphorrhea, improving the patient's quality of life, but also reduced cost, shorter hospital stays and decreased surgery-related morbidity.
Funding
Medical writing services were funded by Ipsen.
Conflict of interest: none declared.
ACKNOWLEDGEMENTS
We thank Vincent de Ruyter and Sybille Virgule (Ipsen) for their support in developing this case study report. We also thank Urszula Miecielica (XPE Pharma & Science) and Juliette Gray, PhD (XPE Pharma & Science) who provided medical writing services on behalf of Ipsen.
REFERENCES
- 1.Carcoforo P, Soliani G, Maestroni U, Donini A, Inderbitzin D, Hui TT, et al. Octreotide in the treatment of lymphorrhea after axillary node dissection: a prospective randomized controlled trial. J Am Coll Surg. 2003;196:365–9. doi: 10.1016/S1072-7515(02)01757-X. [DOI] [PubMed] [Google Scholar]
- 2.Kim WT, Ham WS, Koo KC, Choi YD. Efficacy of octreotide for management of lymphorrhea after pelvic lymph node dissection in radical prostatectomy. Urology. 2010;76:398–401. doi: 10.1016/j.urology.2009.04.104. [DOI] [PubMed] [Google Scholar]
- 3.Capocasale E, Busi N, Valle RD, Mazzoni MP, Bignardi L, Maggiore U, et al. Octreotide in the treatment of lymphorrhea after renal transplantation: a preliminary experience. Transplant Proc. 2006;38:1047–8. doi: 10.1016/j.transproceed.2006.03.040. [DOI] [PubMed] [Google Scholar]
- 4.Kapella M, Gana J, Decroisette E, Aubard Y. Para-aortic lymphocele treated with an injection of somatostatine analog (lanreotide) Eur J Obstet Gynecol Reprod Biol. 2008;141:89–90. doi: 10.1016/j.ejogrb.2008.06.005. [DOI] [PubMed] [Google Scholar]
- 5.Frati A, Antoine M, Rodenas A, Gligorov J, Rouzier R, Chéreau E. Somatostatin in breast cancer. Ann Biol Clin (Paris) 2011;69:385–91. doi: 10.1684/abc.2011.0588. [DOI] [PubMed] [Google Scholar]