Abstract
OBJECTIVES
Sternal dehiscence and mediastinitis are rare but serious complications following cardiac surgery. The aim of this study was to investigate the influence of the number of sternal wires used for chest closure on sternal complications.
METHODS
From May 2003 to April 2007, 4714 adult patients received cardiac surgery in our institute. X-ray images of all patients were reviewed and the used wires were counted. Patients who received another material or longitudinal wiring technique according to Robicsek for chest closure were excluded from this analysis; thus 4466 patients were included into the final analysis. Figure-of-eight wiring was counted as two wires.
RESULTS
Sternal complications occurred in 2.4%, and hospital mortality with or without sternal complications were 2.8 and 2.7%, respectively (P = 0.60). Mean numbers of sternal wires were 7.8 in both patient groups with or without sternal complications (P = 0.79). Multivariate analysis revealed diabetes mellitus [odds ratio (OR) 1.54, 95% CI 1.01–2.34, P = 0.04], chronic obstructive pulmonary disease (OR 1.85, 95% CI 1.12–2.79, P = 0.01) and renal insufficiency (OR 1.70, 95% CI 1.11–2.59, P = 0.001) as significant risk factors for sternal complications. In high-risk patients, the use of less than eight wires was significantly associated with postoperative sternal complications.
CONCLUSIONS
Particularly in high-risk patients, careful haemostasis should be done and eight or more wires should be used to avoid sternal complications.
Keywords: Sternal complications, Sternal closure, Wires
INTRODUCTION
Sternal dehiscence and mediastinitis are rare but serious complications following cardiac surgery. They occur in 0.3–5% of all cases and are associated with a mortality rate of 14–40%, particularly in cases where mediastinitis supervenes [1–4]. It is well known that an inadequate sternal closure leads to a sternal instability [5]. Therefore, diverse techniques have been devised to reduce sternal instability [6–10], but a final solution has not been found yet.
The sternum is closed normally with steel wires and the tension acting on each single wire depends on the total number of wires. Therefore, the total number of wires has an impact on the holding power of the sternum and this fact may be a key to reducing postoperative sternal instability. However, there have been only a few clinical reports studying the relationship between the number of wires and postoperative sternal instability. Indeed, this may not be so relevant in low-risk patients, but could play an important role in a high-risk cohort.
The aims of the present study were (i) to investigate the relationship between the number of wires and the postoperative occurrence of a sternal instability, (ii) to clarify the risk factors for a postoperative sternal instability and (iii) to find a patient cohort who would benefit from more sternal wires.
PATIENTS AND METHODS
From May 2003 to April 2007, 4714 adult patients received cardiac surgery via median sternotomy in our institute. X-ray images of all patients were reviewed and the wires used were counted. Among these patients, those who received another material or a longitudinal wiring technique according to Robicsek for chest closure were excluded from this analysis. Thus, 4466 patients were included in the final analysis. Figure-of-eight wiring was counted as two wires. Medical records that were prospectively collected into an institutional data base were retrospectively reviewed. Re-wiring for sternal instability and/or surgical intervention for mediastinitis was defined as sternal complication. This retrospective study was approved by the institutional ethical board.
Statistical analyses
Results are expressed as mean ± SD. Statistical analysis was performed using the Mann–Whitney U-test for continuous variables or χ2 tests (Fisher's exact tests if n < 5) for categorical variables. Logistic regression was also used for the multivariate analysis of risk factors for mortality. A P-value < 0.05 was considered significant. All statistical analyses were performed using SPSS 16.0 software (SPSS Inc., Chicago, IL, USA).
RESULTS
Demographic description
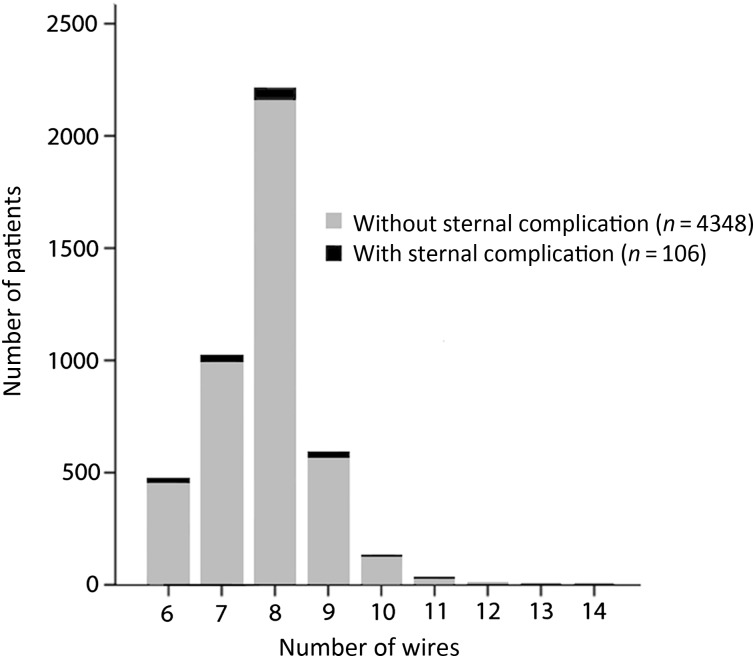
Distribution of the number of used wires is demonstrated in Fig. 1. The mean number of used wires was 7.8 ± 1.0.
Figure 1:
Distribution of number of wires.
Univariate analysis
Among 4466 patients, 106 patients suffered from sternal complications. The results of univariate analyses for sternal complication are listed in Table 1. Among the preoperative parameters, the following were statistically significant factors: male gender, hyperlipidemia, history of smoking, peripheral arterial disease, diabetes mellitus, chronic obstructive pulmonary disease (COPD), preoperative renal insufficiency and regular intake of steroids. Among the intraoperative parameters, the use of a thoracic artery as bypass vessel was the only significant risk factor. Among the postoperative factors, the following were significant: re-thoracotomy for bleeding, postoperative liver insufficiency, postoperative renal failure, postoperative respiratory failure, laparotomy for gastroenterological complications, prolonged ventilation and prolonged intensive care unit (ICU) stay. The number of used wires did not differ between the two groups.
Table 1:
Univariate analyses for sternal complication
| With sternal complication (n = 106) | Without sternal complication (n = 4360) | P-value | |
|---|---|---|---|
| Preoperative patient characteristics | |||
| Age (years) | 67.9 ± 9.4 | 66.5 ± 10.8 | 0.18 |
| Gender (male) | 87 (82.1%) | 3115 (71.4%) | 0.01 |
| Body mass index (kg/m2) | 29.4 ± 4.7 | 28.1 ± 4.3 | 0.11 |
| Hypertension | 99 (93.4%) | 3882 (89.0%) | 0.15 |
| Hyperlipidemia | 86 (81.1%) | 3138 (72.0%) | 0.03 |
| Smoking | 60 (56.6%) | 1957 (45.0%) | 0.02 |
| Pulmonary hypertension | 21 (19.9%) | 909 (21.0%) | 0.78 |
| Re-operation | 5 (4.7%) | 284 (6.5%) | 0.45 |
| Peripheral vascular disease | 27 (25.5%) | 611 (14.0%) | 0.001 |
| Diabetes mellitus | 40 (37.7%) | 1079 (24.7%) | 0.001 |
| Obstructive pulmonary disease | 43 (40.6%) | 1016 (23.3%) | 0.001 |
| Renal insufficiency | 39 (36.8%) | 935 (21.4%) | 0.001 |
| Liver cirrhosis | 3 (2.8%) | 46 (1.1%) | 0.08 |
| Immune suppression | 1 (0.9%) | 54 (1.2%) | 0.78 |
| Steroids | 8 (7.5%) | 161 (3.7%) | 0.04 |
| Emergency | 13 (12.3%) | 771 (17.7%) | 0.14 |
| Body mass index | 29.5 ± 4.69 | 28.14 ± 43.7 | 0.75 |
| NYHA | 3.3 ± 0.7 | 3.2 ± 0.8 | 0.09 |
| Ejection fraction | 45.2 ± 19.0 | 54.7 ± 18.0 | 0.23 |
| Intraoperative parameters | |||
| Duration of OP | 235.3 ± 77.6 | 225.7 ± 81.4 | 0.23 |
| Bypass duration | 110.9 ± 39.1 | 113.8 ± 50.5 | 0.56 |
| Aortic clamp duration | 62.8 ± 24.6 | 64.3 ± 30.5 | 0.63 |
| Core body temperature | 32.3 ± 1.2 | 31.93 ± 2.4 | 0.12 |
| Use of ITA | 64 (60.4%) | 2152 (49.4%) | 0.03 |
| Assist device | 0 (0%) | 9 (0.2%) | 0.63 |
| IABP | 5 (4.7%) | 343 (7.8%) | 0.22 |
| Number of wires | 7.8 ± 1.0 | 7.8 ± 1.0 | 0.73 |
| Postoperative complications | |||
| Re-thoracotomy | 25 (23.6%) | 279 (6.4%) | 0.001 |
| Postoperative psychosis | 19 (17.9%) | 610 (14.0%) | 0.25 |
| Postoperative neurological complications | 2 (1.9%) | 166 (3.8%) | 0.30 |
| Postoperative heart failure | 17 (16.0%) | 595 (13.7%) | 0.48 |
| Postoperative liver failure | 7 (6.6%) | 100 (2.3%) | 0.01 |
| Postoperative renal failure | 14 (13.2%) | 277 (6.4%) | 0.01 |
| Postoperative respiratory insufficiency | 15 (14.2%) | 314 (7.2%) | 0.01 |
| Postoperative immune suppression | 5 (4.7%) | 113 (2.6%) | 0.18 |
| Laparotomy | 5 (4.7%) | 74 (1.7%) | 0.02 |
| Postoperative MI | 7 (6.6%) | 140 (3.2%) | 0.54 |
| Duration of ventilation (hours) | 87.8 ± 248.0 | 48.4 ± 130.0 | 0.01 |
| Intensive care duration (days) | 6.58 ± 11.6 | 3.6 ± 6.9 | 0.001 |
IABP: intra-aortic balloon pumping; OP: operation; ITA: internal thoracic artery; MI: myocardial infarction.
Multivariate analysis for preoperative factors
To identify a high-risk cohort for postoperative sternal instability, a multivariate analysis for preoperative factors was performed and the results are demonstrated in Table 2. Diabetes mellitus, COPD and renal insufficiency were independent risk factors.
Table 2:
Multivariate analysis for preoperative patient characteristics
| OR | 95% CI | P-value | |
|---|---|---|---|
| Diabetes mellitus | 1.54 | 1.01–2.34 | 0.04 |
| COPD | 1.85 | 1.12–2.79 | 0.01 |
| Renal insufficiency | 1.70 | 1.11–2.59 | 0.01 |
COPD: chronic obstructive pulmonary disease.
From the three above-mentioned independent risk factors, the following seven groups were generated for further analyses.
diabetes mellitus only; n = 1119,
COPD only; n = 1059,
renal insufficiency only; n = 974,
diabetes mellitus + COPD; n = 280,
diabetes mellitus + renal insufficiency; n = 354,
COPD + renal insufficiency; n = 304 and
diabetes mellitus + COPD + renal insufficiency; n = 111.
Comparison of the number of wires between groups of high-risk patients with or without a sternal complication
The mean number of used wires was compared between the high-risk patients with or without a sternal complication and the results are demonstrated in Table 3. In the group of patients with diabetes mellitus + COPD (7.24 ± 0.97 with sternal complication vs 7.75 ± 1.04 without sternal complications, P = 0.05) and in the group with diabetes mellitus + COPD + renal insufficiency (7.00 ± 0.94 with sternal complication vs 7.84 ± 0.90 without sternal complications, P = 0.01), the difference was significant.
Table 3:
Comparison of the mean number of wires in different groups of high-risk patients
| Occurrence of sternal complication (%) | Number of wires in patients with sternal complication | Number of wires in patients without sternal complication | P-value | |
|---|---|---|---|---|
| Diabetes mellitus (n = 1119) | 3.6 | 7.50 ± 1.18 | 7.76 ± 1.00 | 0.06 |
| COPD (n = 1059) | 4.0 | 7.63 ± 1.00 | 7.80 ± 0.98 | 0.27 |
| Renal insufficiency (n = 974) | 4.0 | 7.81 ± 1.00 | 7.87 ± 1.10 | 0.70 |
| Diabetes mellitus + COPD (n = 280) | 6.1 | 7.24 ± 0.97 | 7.75 ± 1.04 | 0.05 |
| Diabetes mellitus + renal insufficiency (n = 354) | 5.1 | 7.78 ± 1.40 | 7.80 ± 1.04 | 0.88 |
| COPD + renal insufficiency (n = 304) | 5.9 | 7.50 ± 1.04 | 7.83 ± 0.96 | 0.16 |
| COPD + renal insufficiency + diabetes mellitus (n = 111) | 9.0 | 7.00 ± 0.94 | 7.84 ± 0.90 | 0.01 |
COPD: chronic obstructive pulmonary disease.
Occurrence of sternal complications in high-risk patients receiving seven or more wires
The occurrence of sternal complications in patients who received seven or more wires and in patients who received six wires was compared in each high-risk group and the result is listed in Table 4. The occurrence of sternal complications was significantly lower in patients who received seven or more wires than in patients who received six wires in the group with diabetes mellitus (3.1 vs 7.1%, P = 0.02), in the group with diabetes mellitus + COPD (4.9 vs 14.7%, P = 0.02), in the group with COPD + renal insufficiency (5.1 vs 14.3%, P = 0.05) and in the group with diabetes mellitus + COPD + renal insufficiency (6 vs 36.4%, P = 0.001).
Table 4:
Occurrence of sternal complications in high-risk patients who received equal or more than seven wires
| Wires ≥7 | Wires <7 | P-value | |
|---|---|---|---|
| Diabetes mellitus (n = 1119) | 31/993 patients (3.1%) | 9/126 patients (7.1%) | 0.02 |
| COPD (n = 1059) | 36/951 patients (3.8%) | 7/108 patients (6.5%) | 0.18 |
| Renal insufficiency (n = 974) | 34/873 patients (3.9%) | 5/101 patients (5.0%) | 0.61 |
| Diabetes mellitus + COPD (n = 280) | 12/246 patients (4.9%) | 5/34 patients (14.7%) | 0.02 |
| Diabetes mellitus + renal insufficiency (n = 354) | 14/316 patients (4.4%) | 4/38 patients (10.5%) | 0.10 |
| COPD + renal insufficiency (n = 304) | 14/276 patients (5.1%) | 4/28 patients (14.3%) | 0.05 |
| COPD + renal insufficiency + diabetes mellitus (n = 111) | 6/100 patients (6%) | 4/11 patients (36.4%) | 0.001 |
COPD: chronic obstructive pulmonary disease.
Occurrence of sternal complications in high-risk patients receiving eight or more wires
The occurrence of sternal complications in patients who received eight or more wires and in those who received seven or less wires was compared in each high-risk group and the result is listed in Table 5. The occurrence of sternal complication was significantly lower in patients who received eight or more wires than in those who received seven wires only in the group with diabetes mellitus (2.7 vs 5.1%, P = 0.04).
Table 5:
Occurrence of sternal complications in high-risk patients who received equal or more than eight wires
| Wires ≥8 | Wires <8 | P-value | |
|---|---|---|---|
| Diabetes mellitus (n = 1119) | 20/729 patients (2.7%) | 20/390 patients (5.1%) | 0.04 |
| COPD (n = 1059) | 26/702 patients (3.7%) | 17/357 patients (4.8%) | 0.41 |
| Renal insufficiency (n = 974) | 27/653 patients (4.1%) | 12/321 patients (3.7%) | 0.76 |
| Diabetes mellitus + COPD (n = 280) | 8/178 patients (4.5%) | 9/102 patients (8.8%) | 0.14 |
| Diabetes mellitus + renal insufficiency (n = 354) | 11/235 patients (4.7%) | 7/119 patients (5.9%) | 0.62 |
| COPD + renal insufficiency (n = 304) | 10/204 patients (4.9%) | 8/100 patients (8%) | 0.28 |
| COPD + renal insufficiency + diabetes mellitus (n = 111) | 4/73 patients (5.4%) | 6/38 patients (15.8%) | 0.07 |
COPD: chronic obstructive pulmonary disease.
Occurrence of sternal complications in high-risk patients receiving nine or more wires
The occurrence of sternal complications in patients who received nine or more wires and in patients who received eight or less wires was compared in each high-risk group and the result is listed in Table 6. There was no significant difference in any group.
Table 6:
Occurrence of sternal complications in high-risk patients who received equal or more than nine wires
| Wires ≥9 | Wires <9 | P-value | |
|---|---|---|---|
| Diabetes mellitus (n = 1119) | 6/181 patients (3.3%) | 34/938 patients (3.6%) | 0.83 |
| COPD (n = 1059) | 7/181 patients (3.9%) | 36/878 patients (4.1%) | 0.88 |
| Renal insufficiency (n = 974) | 9/170 patients (5.3%) | 30/804 patients (3.7%) | 0.34 |
| Diabetes mellitus + COPD (n = 278) | 1/45 patients (2.2%) | 16/235 patients (6.8%) | 0.23 |
| Diabetes mellitus + renal insufficiency (n = 354) | 4/61 patients (6.6%) | 14/293 patients (4.8%) | 0.56 |
| COPD + renal insufficiency (n = 304) | 3/54 patients (5.6%) | 15/250 patients (6%) | 0.90 |
| COPD + renal insufficiency + diabetes mellitus (n = 111) | 0/19 patients (0%) | 10/92 patients (10.9%) | 0.13 |
COPD: chronic obstructive pulmonary disease.
DISCUSSION
The crucial findings of the present study were that (i) the number of wires had no influence on sternal complications in the entire patient cohort, (ii) preoperative parameters, diabetes mellitus, COPD and preoperative renal insufficiency were independent risk factors for postoperative sternal complications in our study cohort and that (iii) the number of wires had a significant impact on the frequency of sternal complications in the high-risk patient cohort.
In the present study, a mediastinitis and a sternal instability that needed a surgical re-fixation were both analysed as a ‘sternal complication’ because it turned out to be very complex to retrospectively identify a pure mechanical sternal instability without any infection. In our experience, probably similar to that of others, it is relatively easy to diagnose a mediastinitis with bacteriological evidence, but it is sometimes rather difficult to clarify that there is definitively no infection in a case of a sternal instability. However, sternal instability is a well-known trigger for mediastinitis as pointed out by Robicsek et al. [5] and therefore, the joint analysis of sternal instability and mediastinitis, as performed in the present study may be well justified.
There have been few clinical studies about the relationship between the number of wires and postoperative sternal complications. Friberg et al. [11] reported that among 1012 patients undergoing sternotomy for cardiac surgery, the incidence of deep sternal wound infection was 4.2% in patients with six or fewer wires and 0.4% in patients with seven or more wires (P = 0.001). This is the only work published so far that has focused on the relationship between the number of wires and the rate of sternal complications in a clinical setting.
In contrast to the results reported by Friberg et al. [11], there was no difference in the number of wires between patients with and without sternal complication in our entire study cohort. Sternal complications are relatively rare, as indicated by previous studies [1–5], and this is in line with the rate of 2.4% in our entire patient cohort. Under the requisite of α = 0.05 and β = 0.80, ∼4000 patients will be needed in each arm to detect a significant difference between 2 and 3% according to a simple size power analysis. This may be the reason for our results as obtained for the entire cohort.
For the purpose of the present study, the number of wires was manually counted in X-ray images of 4714 patients in a tedious work. An analysis of the number of sternal wires in 4000 patients in each arm (total 8000 patients) appeared to be unrealistic and therefore, our further analyses were focused on high-risk patients.
In the present study, according to the univariate analysis, the following significant risk factors that are similar to those of previous studies [12–15] were detected: male gender, hyperlipidemia, history of smoking, peripheral arterial disease, diabetes mellitus, COPD, preoperative renal insufficiency, the intake of steroids, the use of a thoracic artery for bypass grafting, re-thoracotomy for bleeding, postoperative liver insufficiency, postoperative renal failure, postoperative respiratory failure, laparotomy for gastroenterological complications, extended duration of ventilation and prolonged ICU stay. Among those factors, only preoperative factors were included in the further multivariate analysis because the intra- and postoperative factors could not have an impact on the wiring technique. Thus, diabetes mellitus, COPD and preoperative renal insufficiency were identified as independent risk factors.
In a high-risk cohort, the number of used wires had a significant impact on the occurrence of sternal complications. In brief, a sternal closure with seven or more wires had an advantage when compared with the use of six or less wires in patients with diabetes mellitus, diabetes mellitus and chronic obstructive pulmonary disease, COPD and renal insufficiency and with diabetes mellitus, COPD and renal insufficiency. A sternal closure with eight or more wires had an advantage over seven or less wires only in patients with diabetes mellitus. A sternal closure with nine or more wires had no more advantage when compared with a closure with eight or less wires. These data indicate that a sternal complication may be reduced with a strategy of using more wires; however, a sternal closure with nine or more wires may bring no additional advantage.
Sternal complications depend on multiple factors. The prevention of a bacterial contamination and other technical influences (the width and tightness of wiring and the accuracy of a midline sternotomy) were not analysed in the present study. In many institutions, a sternotomy and fixation of the sternum are often performed by residents, and the results are not homogeneous in technical aspects. However, the number of wires can be easily controlled. We do not think that a sternal complication could be prevented completely only through the improvement of sternal stability, but the results of the present study suggest that a certain reduction of sternal complications may be expected by an ‘eight wires policy’.
STUDY LIMITATION
In this study, the use of the bilateral internal thoracic arteries was not analysed due to the lack of information on the use of the right internal thoracic artery in our database, which has been extremely rarely used in our institute during the study period of time. The usage of the bilateral internal thoracic arteries is a well-known risk factor for sternal complications [15], and therefore it may be a limitation of the present study. As another study limitation, it should be noted that the occurrence of sternal complications was lower in the present study than in other previously reported series [5, 15]. As described in the Patients and Methods section, only those patients who received a surgical intervention performed in the odds ratio for sternal complications were identified as patients with sternal complications. Therefore, patients with superficial surgical site infection successfully treated with conservative measures were not taken into account.
CONCLUSIONS
In the present study, it was demonstrated that (i) the number of wires had no influence on sternal complications in the entire patient cohort, (ii) the preoperative parameters, diabetes mellitus, COPD and preoperative renal insufficiency were independent risk factors for postoperative sternal complications in our study cohort and that (iii) the number of wires had a significant impact on sternal complications in the high-risk patient cohort. The results of the present study suggest that a certain reduction of sternal complications may be expected with an ‘eight wires policy’.
Conflict of interest: none declared.
REFERENCES
- 1.Losanoff JE, Collier AD, Wagner-Mann CC, Richmann BW, Huff H, Hsieh F, et al. Biomechanical comparison of median sternotomy closures. Ann Thorac Surg. 2004;77:203–9. doi: 10.1016/s0003-4975(03)01468-1. doi:10.1016/S0003-4975(03)01468-1. [DOI] [PubMed] [Google Scholar]
- 2.Losanoff JE, Jones JW, Richmann BW. Primary closure of median sternotomy: techniques and principles. Cardiovasc Surg. 2002;10:102–10. doi: 10.1016/s0967-2109(01)00128-4. doi:10.1016/S0967-2109(01)00128-4. [DOI] [PubMed] [Google Scholar]
- 3.Negri A, Manfredi J, Terrini A, Rodella G, Bisleri G, El Quarra S, et al. Prospective evaluation of a new sternal closure method with thermoreactive clips. Eur J Cardiothorac Surg. 2002;22:571–5. doi: 10.1016/s1010-7940(02)00411-6. doi:10.1016/S1010-7940(02)00411-6. [DOI] [PubMed] [Google Scholar]
- 4.Shih CC, Shih CM, Su YY, Lin SJ. Potential risk of sternal wires. Eur J Cardiothorac Surg. 2004;25:812–8. doi: 10.1016/j.ejcts.2003.11.043. doi:10.1016/j.ejcts.2003.11.043. [DOI] [PubMed] [Google Scholar]
- 5.Robicsek F, Fokin A, Cook J, Bhatia D. Sternal instability after midline sternotomy. Thorac Cardiovasc Surg. 2000;48:1–8. doi: 10.1055/s-2000-9945. doi:10.1055/s-2000-9945. [DOI] [PubMed] [Google Scholar]
- 6.Lee JC, Raman J, Song DH. Primary sternal closure with titanium plate fixation: plastic surgery effecting a paradigm shift. Plast Reconstr Surg. 2010;125:1720–4. doi: 10.1097/PRS.0b013e3181d51292. doi:10.1097/PRS.0b013e3181d51292. [DOI] [PubMed] [Google Scholar]
- 7.Brocki BC, Thorup CB, Andreasen JJ. Precautions related to midline sternotomy in cardiac surgery: a review of mechanical stress factors leading to sternal complications. Eur J Cardiovasc Nurs. 2010;9:77–84. doi: 10.1016/j.ejcnurse.2009.11.009. doi:10.1016/j.ejcnurse.2009.11.009. [DOI] [PubMed] [Google Scholar]
- 8.Schimmer C, Reents W, Berneder S, Eigel P, Sezer O, Scheld H, et al. Prevention of sternal dehiscence and infection in high-risk patients: a prospective randomized multicenter trial. Ann Thorac Surg. 2008;86:1897–904. doi: 10.1016/j.athoracsur.2008.08.071. doi:10.1016/j.athoracsur.2008.08.071. [DOI] [PubMed] [Google Scholar]
- 9.Bhattacharya S, Sau I, Mohan M, Hazari K, Basu R, Kaul A. Sternal bands for closure of midline sternotomy leads to better wound healing. Asian Cardiovasc Thorac Ann. 2007;15:59–63. doi: 10.1177/021849230701500113. [DOI] [PubMed] [Google Scholar]
- 10.Luciani N, Anselmi A, Gandolfo F, Gaudino M, Nasso G, Piscitelli M, et al. Polydioxanone sternal sutures for prevention of sternal dehiscence. J Card Surg. 2006;21:580–4. doi: 10.1111/j.1540-8191.2006.00302.x. doi:10.1111/j.1540-8191.2006.00302.x. [DOI] [PubMed] [Google Scholar]
- 11.Friberg O, Dahlin LG, Söderquist B, Källman J, Svedjeholm R. Influence of more than six sternal fixation wires on the incidence of deep sternal wound infection. Thorac Cardiovasc Surg. 2006;54:468–73. doi: 10.1055/s-2006-924437. doi:10.1055/s-2006-924437. [DOI] [PubMed] [Google Scholar]
- 12.Fowler VG, Jr, O'Brien SM, Muhlbaier LH, Corey GR, Ferguson TB, Peterson ED. Clinical predictors of major infections after cardiac surgery. Circulation. 2005;112(9 Suppl):I358–65. doi: 10.1161/CIRCULATIONAHA.104.525790. [DOI] [PubMed] [Google Scholar]
- 13.Eklund AM, Lyytikäinen O, Klemets P, Huotari K, Anttila VJ, Werkkala KA, et al. Mediastinitis after more than 10,000 cardiac surgical procedures. Ann Thorac Surg. 2006;82:1784–9. doi: 10.1016/j.athoracsur.2006.05.097. doi:10.1016/j.athoracsur.2006.05.097. [DOI] [PubMed] [Google Scholar]
- 14.Risnes I, Abdelnoor M, Almdahl SM, Svennevig JL. Mediastinitis after coronary artery bypass grafting risk factors and long-term survival. Ann Thorac Surg. 2010;89:1502–9. doi: 10.1016/j.athoracsur.2010.02.038. doi:10.1016/j.athoracsur.2010.02.038. [DOI] [PubMed] [Google Scholar]
- 15.Gummert JF, Barten MJ, Hans C, Kluge M, Doll N, Walther T, et al. Mediastinitis and cardiac surgery—an updated risk factor analysis in 10,373 consecutive adult patients. Thorac Cardiovasc Surg. 2002;50:87–91. doi: 10.1055/s-2002-26691. doi:10.1055/s-2002-26691. [DOI] [PubMed] [Google Scholar]