Abstract
BACKGROUND
Although four-dollar programs ($4 per 30-day supply for selected generic drugs) have become important options for seniors to obtain affordable medications, little is known about access to these programs and the characteristics of those who use them.
OBJECTIVES
We quantify access to $4 programs based on driving distance; evaluate factors affecting the program use and potential cost-savings associated with switching to $4 programs in Medicare.
DESIGN
Observational study.
SETTING
US Medicare Part D data, 5% random sample, 2007
PARTICIPANTS
347,653 elderly beneficiaries without Medicaid coverage or low-income subsidies.
MAIN MEASURES
We evaluated how use of $4 programs was affected by driving distance to the store and the beneficiary’s demographic and socioeconomic status, insurance coverage, health status, comorbidities, and medication use. For those who did not use the $4 programs, we calculated potential savings from switching to $4 generics.
KEY RESULTS
Eighty percent of seniors in Medicare Part D filled prescriptions for generic drugs that were commonly available at $4 programs. Among them, only 16.3% filled drugs through $4 programs. Beneficiaries who lived in poor areas, had less insurance, more co-morbidities, and used more drugs and lived closer to $4 generic retail pharmacies, were more likely to use these programs. Blacks were less likely to use the program relative to Whites (15.0% vs. 16.4%; OR = 0.75, 95% CI 0.71–0.80). While 53.2% of nonusers would save by switching to $4 program after incorporating travelling costs, 58% of those who could save would have net annual out-of-pocket savings of less than $20.
CONCLUSIONS
The take-up rate of $4 programs was low in 2007 among Medicare beneficiaries. As more stores offer $4 programs and increasing numbers of drugs become generic, more beneficiaries could potentially benefit, as could the Medicare program.
Key words: Medicare, low-cost generic drugs, pharmaceuticals
INTRODUCTION
When Wal-Mart initiated the $4 generic drug program ($4 per 30-day supply for selected generic prescription drugs) in October 2006, it created an important low-cost alternative for individuals who use these medications.1 In November 2006, Target followed Wal-Mart’s lead and offered a similar program in several states.2 In 2007, Wal-Mart and Target were the only major national chains offering the $4 programs, with approximately 244 prescriptions with varying dosages in 2007. Since 2008, additional pharmacies have started to offer similar programs, such as Walgreens ($12/3 month supply) and CVS ($9.99/3 month supply).
Through $4 programs, anyone regardless of insurance status or age pays only $4 per 30-day supply (inclusive of dispensing fee); in comparison, patients with private non-Medicare prescription drug coverage often pay $10–$11 per 30-day supply for generics and $25–$27 per 30-day for a preferred brand-name drug.3 Medicare beneficiaries pay $5–$7 copayment for their generic drugs and $28–$42 for a preferred brand-name drug.4
The $4 programs have the potential to save patients and the health care system substantial amounts of money. A recent study found that the total savings to insurance plans and patients would be $3.2 billion if everyone filled their eligible generic prescriptions in a $4 store in 2007.5 The savings would be less for the Medicare population because the smaller difference in copayment in the Medicare plans and $4 programs. However, the $4 programs could still have significant implications for individuals, Medicare and the larger health system because Medicare beneficiaries spend more on medications and are more sensitive to price difference.6
Little is known about access to these $4 programs for Medicare beneficiaries and the characteristics of those who use the program, especially among older adults who could benefit most. In this study, we used 2007 Medicare Part D prescription drug data and locations of stores that offered $4 programs in 2007 to address four key questions related to the use of low-cost generic programs: (1) What proportion of elderly beneficiaries used the $4 programs in 2007 and how does this proportion differ by medication therapeutic class? (2) How far did elderly Medicare beneficiaries live from these $4 programs and how do driving distances affect the use of $4 programs? (3) What other factors were related to the use of these programs? (4) Among non-users of $4 programs, what proportion would save by switching to a $4 program after incorporating the driving costs to the stores?
METHODS
Study Population
Our study population consists of a 5% random sample of elderly Medicare beneficiaries who were enrolled in stand-alone Medicare prescription drug (PDP) plans in 2007. We identified those who used any drug available through the $4 programs in 2007. We excluded those who paid copayments lower than $4 because they would have no financial incentives to use the $4 program. The excluded beneficiaries included those eligible for Medicaid or low-income subsidies, and those who had drug coverage with lower than $4 copayments. We also excluded drugs with plan negotiated prices below $4. Our study population was thus potential users of the $4 programs.
We divided our study population into two groups: those who filled a drug through a $4 program (users) and those who did not (non-users). We identified the drugs as being filled through a $4 program if: 1) the drug was available through a $4 program at $4 per 30-day supply; 2) the gross reported drug cost was $4 per 30-day supply (i.e., the total amount the pharmacy billed); and 3) patients paid $4 or a copayment amount accepted by their Part D plans for prescriptions filled in the $4 programs. In 2007, the options of a $10 per 90-day supply and mail-order use were not available and thus not analyzed.1
Data Sources
We used four different data sources. First, we obtained a 5% random sample of elderly Medicare beneficiaries (aged 65 and over) with full-year enrollment in Part A, B and a stand-alone Part D plan (PDP) in 2007. These data include beneficiary demographics, all outpatient prescription drug events, plan characteristics, enrollment information, and Zip-Code of residence. Second, we used 2000 US census data (2010 US census data are not yet available for these variables) that contained information on household income and education for people aged 65–74 and 75 and older at the Zip-Code level. Third, we obtained the 2002 US 5-Digit Zip-Code Tabulation Area (ZCTA5) National Shapefile which provides information on the latitude and longitude of the center of each Zip-Code. Last, from Wal-Mart and Target, we obtained the list of $4 generic drugs available at the end of 2007 (their drug lists were essentially the same) and the addresses of all Wal-Mart Corporate (including Sam’s Club and neighborhood markets) and Target stores that offered the $4 program in the United States in 2007.
Measures of Interest
Factors Associated with the Use of $4 Programs
From the Medicare Part D data, we obtained individual-level beneficiary information including sex, age (65–69 as reference group, 70–74, 75–79, and ≥80), race/ethnicity, indicator of living in Metropolitan Statistical Area (“MSA”; non–MSA as reference group), type of drug coverage in the gap, total number of $4 drugs filled in any pharmacy, and whether the beneficiary entered Medicare Part D’s coverage gap (where they paid full drug costs) or catastrophic period (where they paid 5% of drug costs). Part D data have an enhanced Research Triangle Institute Race Code verified by first and last name algorithms, including non-Hispanic White (“Whites”), non-Hispanic Blacks, Hispanics, Asian/Pacific Islander (“Asians”), American Indian/Alaska Native (“Native Americans”), and others (missing or unable to determine).7 We excluded the last two categories due to small sample size, and created indicators for Blacks, Hispanics, and Asians relative to Whites.
Using medical data, we calculated the number of Elixhauser comorbidities8 and the Centers for Medicare & Medicaid Services (CMS)’ prescription drug hierarchical condition categories (RxHCC), as proxies for health status.9
Based on the beneficiary’s Zip-Code of residence, we determined median household income (< $25 k as reference group, $25 k–$35 k, $35 k–$45 k, and >$45 k) and the proportion of elderly residents having higher than high-school education.
We calculated the driving distance to the closest store that offered the $4 program in 2007 for each individual in our overall study population using ArcGIS v10 and SAS v9.2. The distance was calculated from the exact store location to the center of the Zip-Code where the beneficiary lived, because the exact home addresses of beneficiaries were not available due to data confidentiality. There are other important aspects of access, such as knowledge, health literacy, and cognitive ability,10 which cannot be observed in the data. Thus, in this paper we only focus on driving distance to the store.
Potential Savings
To determine whether current nonusers would save money by switching to a $4 program, we calculated the difference between potential savings per year if they switched their drugs to $4 generics and the driving costs to the $4 stores per year. Potential savings were defined as difference between the actual costs the beneficiary paid for the drug and the costs of medications if they had filled them in $4 programs. To calculate the driving costs to the closest store, we (1) used the weighted average cost per mile in 2007 for different types of vehicles, $0.1578 per mile;11 (2) counted how many different visits one had to make to the $4 store according to particular dates they filled their prescriptions; and (3) calculated the total driving costs in 2007 for each beneficiary. This calculation gives us the upper bound of travelling costs and therefore the lower bound of net savings. In reality, driving costs will likely be lower than we estimate; for example, individuals may visit these retail stores for other non-drug purchases or individuals may visit the stores on the way home from work.
Statistical Analysis
We identified the proportion of beneficiaries living within the following categories of driving distances to the closest store that offered the program: <2, 2–5, 5–10, and ≥10 miles. We examined this proportion separately for those who resided in MSA vs. non-MSA areas.
To evaluate factors associated with the use of $4 programs, we included the variables discussed previously. We first compared these factors between user and non-user groups using Chi2-tests and Analysis of Variance (ANOVA). Second, we used multivariate logistic regression to model the probability of use of a $4 program among beneficiaries, controlling for all covariates mentioned above.
Finally, we calculated the proportion of non-users whose potential savings would be greater than their travelling costs if they had switched to $4 programs. We reported the distribution of the gross savings and net savings after incorporating travelling costs.
RESULTS
Eighty percent of American seniors enrolled in Medicare Part D (n = 242,691) used at least one generic drug that was commonly available in $4 programs in 2007. Among all prescriptions filled by these individuals (n = 242,691), 7.6% of their prescriptions were eligible drugs in the $4 program in 2007. Among potential users, 39,575 (users) or 16.3% filled at least one of these generic drugs in a $4 program. About 60% of users filled all their drugs in a store providing the $4 program. Table 1 compares the characteristics of users and non-users.
Table 1.
Characteristics of the Study Population in 2007
| Variable | Users | Non Users | P-value |
|---|---|---|---|
| (n = 39,575) | (n = 203,116) | ||
| Female, % | 63.2 | 63.2 | 0.94 |
| Race, % | |||
| Whites | 93.7 | 92.8 | < 0.001 |
| Blacks | 2.9 | 3.2 | |
| Hispanics | 2.1 | 2.1 | |
| Asians | 0.7 | 1.2 | |
| Age, % | |||
| 65–69 | 25.4 | 21.9 | < 0.001 |
| 70–74 | 27.0 | 23.2 | |
| 75–80 | 25.4 | 25.0 | |
| 80+ | 22.2 | 29.8 | |
| Zip-Code median household income, % | |||
| <$25 k | 45.4 | 41.9 | < 0.001 |
| $25 k–$35 k | 34.6 | 32.6 | |
| $35 k–$45 k | 13.4 | 14.6 | |
| >$45 k | 6.2 | 10.1 | |
| Living in metropolitan areas, % | 60.4 | 67.3 | < 0.001 |
| Driving distance to the closest $4 program, mean | 8.81 ± 0.059 | 10.63 ± 0.041 | < 0.001 |
| Driving distance to the closest $4 program, % | |||
| <2 mi | 13.3 | 11.9 | < 0.001 |
| 2– < 5 mi | 35.5 | 35.2 | |
| 5– < 10 mi | 22.7 | 23.7 | |
| ≥10 mi | 28.5 | 29.1 | |
| Prescription drug risk score, mean | 0.90 ± 0.001 | 0.88 ± 0.001 | < 0.001 |
| No. of Elixhauser comorbidities, mean | 2.37 ± 0.010 | 2.29 ± 0.004 | 0.18 |
| No. of Elixhauser comorbidities, % | |||
| ≤1 | 40.0 | 41.1 | < 0.001 |
| 2–4 | 46.5 | 44.9 | |
| ≥5 | 13.5 | 14.0 | |
| Total No. of $4 drugs filled anywhere, mean | 13.9 ± 0.06 | 12.6 ± 0.02 | < 0.001 |
| Gap coverage type, % | |||
| Generic & brand coverage | 1.3 | 1.6 | < 0.001 |
| Generic only coverage | 13.3 | 13.1 | |
| No coverage | 83.8 | 81.7 | |
| Entering the coverage gap, % | 30.8 | 35.6 | < 0.001 |
| Entering the catastrophic period, % | 2.6 | 4.4 | < 0.001 |
plus minus indicate Mean ± SE
The proportion of users varies by drug class: 23.2% of those using an eligible cholesterol drug (lovastatin, pravastatin) filled it in $4 programs, while 19.8% of those using an eligible anti-diabetic drug (chlorpropamide, glimepiride, glipizide, glyburide) and 17.9% of those using an eligible mental health drug (e.g., fluoxetine, haloperidol, thioridazine, doxepin) did so (all these comparisons are significantly different from each other with p-value < 0.001; data not shown).
Driving Distance to a $4 Program
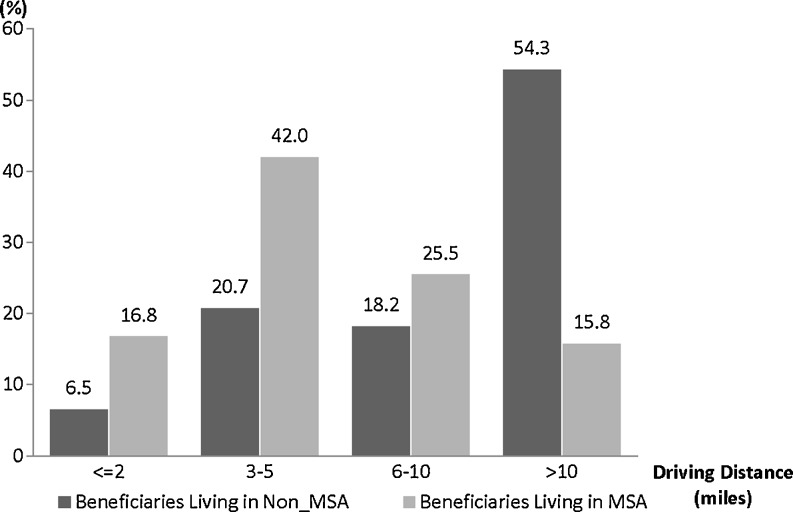
The driving distance to $4 programs differed in MSA and non-MSA areas (Fig. 1). Only 6.5% of non-MSA beneficiaries lived within 2 miles of a store while 54.3% lived 10 miles or more away. In comparison, 16.8% of those in MSA lived within 2 miles from the closest $4 store, while only 15.8% lived 10 miles or more away.
Figure 1.
Distribution of driving distance to nearest retail pharmacy offering $4 generics according to whether beneficiaries resided in rural or metropolitan areas. Abbreviation: MSA Metropolitan Statistical Area.
Factors Associated with the Use of $4 Programs
Table 2 presents factors associated with the use a $4 program among potential users (those who used any eligible drugs). Compared to Whites, Blacks and Asians were less likely to use a $4 program (16.4% vs. 15.0%, and 10%, respectively) (OR = 0.80, 95% CI 0.75–0.85 for Blacks vs. Whites; OR = 0.72, 95% CI 0.63–0.81 for Asians vs. Whites) and Hispanics were more likely to use (OR = 1.10, 95% CI 1.02–1.19). Seniors were less likely to use the programs as they aged. Seniors living in areas with low household income were more likely to use the $4 programs (17.4% users in areas with median household income <$25 K vs. 10.6% users in areas with median household income >$45 K).
Table 2.
Factors Influencing Whether Beneficiaries Used the $4 Program in 2007
| Variable | % of Users | Estimated Odds Ratio | 95% CI Lower Limit | 95% CI Upper Limit | P-value |
|---|---|---|---|---|---|
| Female | 16.3 | 1.00 | 0.98 | 1.03 | 0.86 |
| Race | |||||
| Whites | 16.4 | 1[Reference] | |||
| Blacks | 15.0 | 0.80 | 0.75 | 0.85 | < 0.001 |
| Hispanics | 16.4 | 1.10 | 1.02 | 1.19 | 0.02 |
| Asians | 10.0 | 0.72 | 0.63 | 0.81 | < 0.001 |
| Age | |||||
| 65–69 | 18.4 | 1[Reference] | |||
| 70–74 | 18.5 | 0.99 | 0.96 | 1.02 | 0.62 |
| 75–80 | 16.5 | 0.82 | 0.79 | 0.85 | < 0.001 |
| >80 | 12.7 | 0.61 | 0.59 | 0.63 | < 0.001 |
| Percentage of residence finishing high school* | 1.02 | 1.02 | 1.03 | < 0.001 | |
| Median household income* | |||||
| <$25 k | 17.4 | 1[Reference] | |||
| $25 k–$35 k | 17.1 | 0.94 | 0.91 | 0.97 | < 0.001 |
| $35 k–$45 k | 15.1 | 0.92 | 0.88 | 0.97 | < 0.001 |
| >$45 k | 10.6 | 0.86 | 0.81 | 0.91 | < 0.001 |
| Living in metropolitan area | 14.8 | 0.83 | 0.77 | 0.90 | < 0.001 |
| Driving distance | |||||
| Rural | |||||
| <2 mi | 23.6 | 1[Reference] | |||
| 2– < 5 mi | 22.0 | 0.93 | 0.86 | 1.00 | 0.06 |
| 5– < 10 mi | 20.6 | 0.85 | 0.79 | 0.92 | < 0.001 |
| ≥10 mi | 17.3 | 0.61 | 0.57 | 0.66 | < 0.001 |
| Metropolitan | |||||
| <2 mi | 16.9 | 1[Reference] | |||
| 2– < 5 mi | 15.0 | 0.88 | 0.85 | 0.92 | < 0.001 |
| 5– < 10 mi | 13.9 | 0.77 | 0.74 | 0.81 | < 0.001 |
| ≥10 mi | 13.9 | 0.67 | 0.63 | 0.70 | < 0.001 |
| No. of Elixhauser comorbidities | 1.01 | 1.01 | 1.02 | < 0.001 | |
| Prescription drug risk score | 1.44 | 1.37 | 1.51 | < 0.001 | |
| Total No. of $4 drugs filled anywhere | 1.01 | 1.01 | 1.01 | < 0.001 | |
| Type of coverage in the gap | |||||
| No coverage | 16.6 | 1[Reference] | |||
| Generic & brand coverage | 14.1 | 0.70 | 0.56 | 0.87 | 0.001 |
| Generic only coverage | 16.5 | 1.05 | 1.00 | 1.10 | 0.05 |
*These measures are at the Zip-Code level
Seniors living in MSAs were less likely to use the $4 program compared with those living in rural areas (OR = 0.83, 95% CI 0.77–0.89). The likelihood of using a $4 program decreased with distance; however, distance affected those in MSA more.
Potential Savings and Travelling Costs
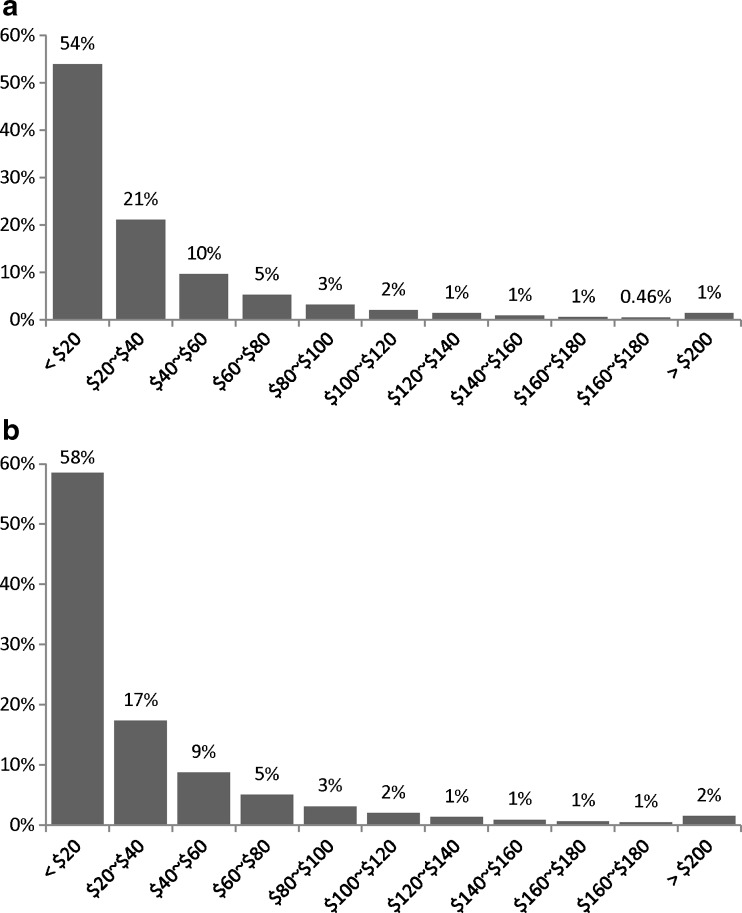
Among non-users, on average beneficiaries would save $33 (s.d. = $46) if they filled their eligible drugs in a $4 program; however, 50% of these non-users would save less than $20 if they switched. Thus, potential savings are highly skewed (Fig. 2 Panel A). After incorporating travelling costs, only 53.2% of non-users would have net savings from switching to a $4 program; that is, their potential savings from switching would be greater than the travelling costs to a $4 store. On average, a potential switcher (if their savings were greater than traveling costs) would have a lower bound of net savings of $32 (s.d. = $48); only 2% would save over $200 (Fig. 2 Panel B).
Figure 2.
Distribution of potential annual savings from switching to $4 programs among potential users. Panel A. Potential gross savings without incorporating the travelling costs among all non-users (n = 203,116). Panel B. Potential net savings after incorporating the travelling costs among those with positive net savings (n = 108,058).
CONCLUSIONS
Today, many stores offer the $4 programs. However, little is known about use of these low-cost generic programs. Our study is the first we are aware of to quantify access to $4 programs and evaluate who used these programs in Medicare.
Our study yields several important findings:
First, in 2007 the use of the $4 program was quite limited. The majority of older Medicare beneficiaries (86%) never filled a prescription for an eligible generic drug at a $4 store. This represents a loss of potential savings for the Medicare program and for patients. However, our findings also point to an important reason for why use of these programs may be low. We estimated, after taking driving costs into consideration, that only 53.2% of nonusers would save. On average, the net savings was $32, and only 2% would save over $200. Thus Medicare and the healthcare system overall could save substantial sums,5 while individual patients are unlikely to see substantial savings. It may be most effective to target the 2% of the Medicare population who could potentially save the most in switching, which is readily done using claims data, as we demonstrate.
Second, driving distance was strongly associated with the use of the program. It stands to reason that improved accessibility could lead to increased use of low-cost generics. As more stores offer $4 programs in subsequent years and some programs begin offering mail-order services for these drugs,1 more Americans can easily access to low-cost drugs.
Third, several beneficiary characteristics were associated with the uptake of the $4 program. Those who had higher risk scores, more co-morbidities, and/or used more $4 drugs, were more likely to use the program. In addition, those beneficiaries at some increased financial risk; i.e. those who had no coverage in the coverage gap and those who lived in Zip-Codes with lower income families were more likely to use the program. These findings are encouraging because they suggest that seniors who could benefit most were using these low-cost alternatives. Asians and Blacks were less likely to use the program than Whites. It would be important to assess why these racial/ethnic differences arise—are they due to access, knowledge, or use of different types of pharmacies?
There are several strengths to our study. We used national Medicare Part D data and believe these data are the best available to study these questions for several reasons. First, our data is a 5% random sample of those enrolled in PDPs, so it is generalizable. Second, CMS considers highly-discounted drugs filled in $4 programs as “usual and customary” and Part D plans adjudicate the $4 claims so we can observe these drugs in the claims data.12 For example, if the beneficiary’s coinsurance is 25% in the initial coverage period, the beneficiary only pays $1 ($4*25%) and the plan pays the rest. Thus, missing claims from $4 programs would be less of a problem among the Medicare population compared to a commercial population.
It is possible that some drugs filled in the $4 program were missing in claims if beneficiaries chose not to present their Medicare Part D plan cards.13 We believe the missing claims would not have significant effects on our results for several reasons. First, the proportion of users estimated in our study is larger than the estimated proportion of users (9%) found in a recent study using 2007 Medical Expenditure Panel Survey data.5 Second, almost all of the users of $4 programs in our sample used the $4 stores in the initial coverage period where they would have financial incentives to present their Medicare cards. They may not present their cards when they were in the coverage gap phase, but because we already captured them in the initial period our results modeling factors affecting users are unlikely to change. Third, even though beneficiaries paid the entire $4, they would have incentives to present their cards, because pharmacies would adjudicate these drugs in the claims so patients’ doctors can monitor patients’ medications. We acknowledge that it is possible that some pharmacies do not report these drugs to the patient’s insurance and we may miss them in our data. We believe the effect is likely small, but we are unable to know for sure using existing data.
There are some additional potential limitations to our study. First, we overestimate travelling costs because people are unlikely to drive to a $4 store solely to pick up their prescriptions. Nevertheless, the ability to calculate the driving distance and travelling costs is an important contribution: driving distance turns out to be a major factor associated with the use of $4 programs and omitting this variable could bias the results. Second, we only examined direct substitution of generics, while a larger potential savings could be realized if individuals were willing to switch their brand-name drugs, and not just their generics, for low-cost generics. Finally, we do not quantify the potential downsides of increased use of $4 generics,13 but we do acknowledge that these downsides are real and important to consider. For example, if prescriptions filed in the $4 program are not reported back to insurance or patients use more than one pharmacy, it may be difficult to monitor drug–drug interactions. Additionally, it is likely that $4 programs were created to attract people to the stores to buy other products, including non-prescription or prescriptions drugs not eligible for the $4 programs, which could potentially be more expensive.
In sum, 80% of American seniors in Medicare filled prescriptions for generic drugs that were commonly available at $4 per 30-day supply in 2007; only 16.3% used a $4 program in 2007. Once incorporating travelling costs, only 53.2% of nonusers would potentially save by switching to the $4 programs and the potential savings focus on a small proportion of beneficiaries. Potential policies could be considered to encourage the use of $4 generic programs among Medicare beneficiaries who have not been using and/or could save the most, including Blacks, those with less drug coverage, those with high prescription drug risk scores and those with easy access to a $4 store. However, because of only modest individual savings associated with switching additional incentives for most patients would likely be required before the Medicare program could experience any savings.
ACKNOWLEDGMENTS
The RAND University of Pittsburgh Health Institute and the Clinical and Translational Science Institute: Translating Research into Practice Program. This project was supported in part by the RAND–University of Pittsburgh Health Institute (RUPHI), a formal collaboration between the RAND Corporation, RAND Health, and the University of Pittsburgh School of the Health Sciences. This publication was made possible by grant UL1 RR024153 from the National Center for Research Resources, a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. During the study period, Dr. Zhang was also supported by NIMH RC1 MH088510 and AHRQ R01 HS018657.
Conflict of Interest
Dr. Gellad has received an honorarium from Vindico Medical Education for preparation of a continuing medical education (CME) activity focused on improving medication adherence. Drs. Zhang and Lave were investigators for a contact (2008–2009) to evaluate the effects of high-deductible health plans funded by Highmark Inc., which sells Part D plans.
References
- 1.Wal-Mart Stores Inc. Affordable prescription program. http://walmartstores.com/healthwellness/8247.aspx. Accessed May 4, 2011.
- 2.Target.com. Target 4 dollar listing. http://sites.target.com/site/en/health/page.jsp?contentId=PRD03-004319. Accessed January 10, 2010.
- 3.Kaiser Family Foundation. Prescription Drug Trends. http://kff.org/rxdrugs/3057.cfm. Accessed February 18, 2010.
- 4.Kaiser Family Foundation. Medicare prescription drug plans in 2010 and key changes over five years: summary of findings. 2010; http://www.kff.org/medicare/upload/8096.pdf. Accessed September 1, 2011.
- 5.Zhang Y, Zhou L, Gellad WF. Potential savings from greater use of $4 generic drugs. Arch Intern Med. 2011;171(5):468–469. doi: 10.1001/archinternmed.2011.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kaiser Family Foundation. Health care on a budget: the financial burden of health spending by Medicare households. http://kff.org/medicare/upload/8171.pdf. Accessed April 26, 2011.
- 7.Bonito A, Bann C, Eicheldinger C, Carpenter L. Creation of New Race-Ethnicity Codes and Socioeconomic Status (SES) Indicators for Medicare Beneficiaries. Final Report. Sub-Task 2. (Prepared by RTI International for the Centers for Medicare and Medicaid Services through an interagency agreement with the Agency for Healthcare Research and Policy, under Contract No. 500-00-0024, Task No. 21). http://www.ahrq.gov/qual/medicareindicators/medicareindicators.pdf. Accessed March 16, 2010.
- 8.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Centers for Medicare & Medicaid Services. Centers for Medicare & Medicaid Services Prescription Drug Hierarchical Condition Category (RxHCC) Model Software. 2010; http://www.cms.hhs.gov/MedicareAdvtgSpecRateStats/06_Risk_adjustment.asp. Accessed February 3, 2010.
- 10.Eisenberg JM, Power EJ. Transforming insurance coverage into quality health care: voltage drops from potential to delivered quality. JAMA. 2000;284(16):2100–2107. doi: 10.1001/jama.284.16.2100. [DOI] [PubMed] [Google Scholar]
- 11.AAA Association Communication. Your driving costs. http://www.aaaexchange.com/Assets/Files/20073261133460.YourDrivingCosts2007.pdf. Accessed April 12, 2011.
- 12.Centers for Medicare & Medicaid Services. Medicare Prescription Drug Benefit Manual, Chapter 14 Coordination of Benefits, Page 19. Baltimore, MD, USA 2008.
- 13.Choudhry NK, Shrank WH. Four-Dollar Generics — Increased Accessibility, Impaired Quality Assurance. N Engl J Med. 2010;363(20):1885–1887. doi: 10.1056/NEJMp1006189. [DOI] [PubMed] [Google Scholar]