Abstract
Background
The population of persons seeking medical care is linguistically diverse in the United States. Language barriers can adversely affect a patient’s ability to explain their symptoms. Among hospitalized patients, these barriers may lead to higher readmission rates and longer hospitalizations. Trained interpreters help overcome communication barriers; however, interpreter usage among patients is suboptimal.
Objective
To investigate differences among patients with limited English proficiency (LEP) in their length of stay (LOS) and 30-day readmission rate associated with their receiving professional interpretation at admission or discharge.
Design
We analyzed the rates of interpretation at admission and discharge of all LEP patients admitted to a tertiary care hospital over a three-year period. We calculated length of stay in days and as log of LOS. We also examined 30-day readmission. Using multivariable regression models, we explored differences among patients who received interpretation at admission, discharge, or both, controlling for patient characteristics, including age, illness severity, language, and gender.
Participants
All LEP patients admitted between May 1, 2004 and April 30, 2007.
Main Measures
Length of hospital stay as related to use of professional interpreters; readmission to the hospital within 30 days.
Key Results
Of the 3071 patients included in the study, 39 % received language interpretation on both admission and discharge date. Patients who did not receive professional interpretation at admission or both admission/discharge had an increase in their LOS of between 0.75 and 1.47 days, compared to patients who had an interpreter on both day of admission and discharge (P < 0.02). Patients receiving interpretation at admission and/or discharge were less likely than patients receiving no interpretation to be readmitted with 30 days.
Conclusions
The length of a hospital stay for LEP patients was significantly longer when professional interpreters were not used at admission or both admission/discharge.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-012-2041-5) contains supplementary material, which is available to authorized users.
Key Words: low English proficient (LEP), interpreters, length of stay (LOS)
People living in the United States speak over 300 different languages according to the 2008 US census estimates and over 24 million individuals speak English less than very well, representing 8.6 % of the US population.1 Low English proficient (LEP) patients seeking medical care often have a difficult time explaining their illness and understanding their doctor’s instructions and treatment plan. Language problems impact multiple aspects of health care including access, patient-physician communication, satisfaction with care and patient safety.2 This results in LEP patients being more likely to experience adverse medical events of a serious nature and having difficulty adhering to their treatment plan.3 LEP patients receiving care without qualified interpreters have a poor self-reported understanding of their diagnosis and treatment plan and frequently wish their doctors had explained things better.4
To avoid these problems, it is imperative that LEP patients be provided with qualified, professional interpreters to help them navigate our health care system. Kaliner et al. described a professional interpreter as one who is paid by a hospital or health system to interpreter.5 Training can vary between institutions. Research has shown that the use of untrained, ad hoc interpreters or family members can result in disastrous mistakes. Ad hoc interpreters can misinterpret or omit up to half of physicians’ questions, are more likely to commit errors with clinical significance, have a higher risk of not mentioning medication side effects, and may ignore embarrassing issues (especially when children are used to interpret).3,6,7
From an economical standpoint, it has been found that LEP patients stay in the hospital between 0.7 and 4.3 days longer than English speaking patients with similar conditions.8 In addition non-English speaking patient have a higher 30-day readmission rate compared to their English speaking counterparts.9 This research did not address the use of professional interpreters though and its effect on LOS or readmission. More recently it’s been shown that providing LEP inpatients with trained medical interpreters throughout their hospital stay can reduce their LOS by almost a day.10
Our objective was to examine hospital length of stay (LOS) and 30-day readmission rates among LEP patients and compare those rates with a patient’s access to professional interpretation. We tried to determine if the timing of interpretation, at admission, discharge or some other time during a patient’s stay was associated was LOS and readmission.
Methods
Study Design
This study is a retrospective analysis of length of stay and 30-day readmission rates among patients who were admitted to a tertiary care, university hospital. We examined patterns of language interpretation during each patient’s hospital stay. We then compared these patterns with hospital registration information that documents patients’ preferred language and their need for interpretation with records kept by the hospital’s department of interpreter services documenting all interpretations done for hospitalized patients.
Participants
At the hospitals that this study took place, after being assessed for being bilingual in oral and written language, all professional interpreters are required to attend a 90-hour interpreter training that includes 45 hours of class didactics and 45 hours of clinical practicum. The study dataset includes three sources of data: admission/registration information, medical records, and language service encounter data. Using administrative records collected and maintained by the hospital that record patients’ interpretation needs, we abstracted data from hospital admission records for all patients that included an indicator that patients both spoke a language other than English and requested an interpreter. We obtained diagnostic and procedure hospital records for all adult (aged 18 and older) LEP patients who were admitted between 1 May 2004 and 30 April 2007. Our study population includes all patient admissions that had at least one interpretation event during their hospital stay. Initially, 3127 patients were included in the study. Of these the following admissions were excluded from the analysis: 54 patients who were not admitted into the hospital (i.e., a LOS of 0) and two patient admissions who had extremely long stays in the hospital of 153 and 289 days, respectively. The study population includes 3071 admissions with a LOS between 1 and 85 days.
Main Measures
Hospital administrative data contained several patient characteristics, including age, gender, and length of stay. As a measure of severity of illness, we used the hospital’s diagnoses cost weight that accounts for differences in patients’ illness burden. Among the 3071 patients in the study population these weights ranged from 0.28 to 20.04, where higher weights indicate more severe illness. Using the primary diagnosis recorded in hospital administrative records, we created an additional major diagnosis category to distinguish patients admitted for cardiovascular conditions. We also used administrative data to obtain patient’s preferred language. A description of the study measures is presented in the Appendix (available online).
We merged encounter data collected by the language services department with administrative data containing patient characteristics and pertinent clinical information, including diagnoses and a measure of clinical severity. Using encounter data to assess whether or not interpretation occurred at admission and discharge, we compared date of interpretation with admission and discharge dates. For each patient, we created a single categorical indicator that defined four possible conditions between hospital dates and encounter with an interpreter—0, no interpreter either on day of admission or on day of discharge; 1, interpreter on admission, but not discharge; 2, interpreter on discharge day, but not admission; and 3, interpreter on day of admission and day of discharge.
Using date of admission and discharge we calculated length of stay (LOS) in days for all patients. Patient LOS in days is skewed such that about 75 % of patients were hospitalized less than 6 days. Hence, we conducted sensitivity analysis by examining the log of length of stay as an outcome variable, see online appendix.
We used analysis of variance (ANOVA) to assess differences in age and severity of illness among patients with no interpreter at admission/discharge, admission only, discharge only, and interpreter encounter on both admission and discharge date. All patients had at least one interpreter encounter. We also compared patterns of interpretation by patient’s language for the five main language groups.
To examine patterns of interpretation and patients’ length of hospital stay, we used multivariable models that controlled for patient characteristics, including age, gender, language, primary diagnosis, and illness severity. To account for effects of patients repeated hospital stays, we conducted mixed model regression with a random effect for patient. To explore the effects of patient age and severity of illness on the LOS, we fit a number of linear models including main effects and various 2-way interactions. These models were fit by mixed model regression using SPSS (IBM SPSS Advanced Statistics 18, Chicago, IL). To examine whether or not the association of age and severity with LOS was non-linear, we added a quadratic function (i.e., age squared and severity squared) to provide the best fit of the association. As length of stay is a skewed outcome measure, we transformed length of stay using a log of LOS to “normalize” the distribution. Results of this sensitivity analysis using log of LOS as the dependent variable are presented in the online appendix. We report the final model that contains independent variables listed as follows: language, gender, age, severity, primary diagnosis, and pattern of interpretation (no interpreter on either admission or discharge, interpreter on admission only, interpreter on discharge only, and interpreter on both admission and discharge (reference category).
We also examined patient characteristics, including interpretation, associated with patients being readmitted to the hospital within 30 days. According to Benbassat & Taragin,11 “most preventable readmissions have been reported to occur early, within one month of discharge . . . ”. We used the same patient characteristics included in models examining length of stay in logistic regression models with readmission within 30 days as the dependent variable. In addition, since length of stay (LOS) is associated with readmission within 30 days,12 we also included LOS as an additional covariate in the logistic regression model.
This study was reviewed, approved, and monitored by the University of Massachusetts Medical School Institutional Review Board. It received an exemption from requiring informed consents.
Results
Of LEP patients in the study sample, 90 % spoke 1 of 5 languages. Spanish and Portuguese were the most commonly interpreted languages, but. 65 different languages comprised the “other” languages Table 1. Table 2 shows that 39 % of hospitalized LEP patients had language interpretation services on both day of admission and day of discharge, while 14 % had interpreters neither on day of admission or day of discharge. Spanish and Portuguese speaking patients were most likely to have interpreters on admission and discharge. Patients speaking less prevalent languages were most likely to not have interpretation services on both admission and discharge.
Table 1.
Characteristics of Patients with Limited English Proficiency Who Were Admitted for One or More Days
| Patient Characteristic | % (n) |
|---|---|
| Patient’s Preferred Language | |
| Spanish | 65.4 (2007) |
| Portuguese | 10.2 (313) |
| Vietnamese | 6.0 (183) |
| Albanian | 5.7 (174) |
| Russian | 2.9 (89) |
| Other | 9.9 (305) |
| Gender | |
| Female | 56.5 (1735) |
| Male | 43.5 (1336) |
| Primary Diagnosis | |
| Cardiovascular disease | 12.6 (386) |
| Lung disease (asthma, COPD, etc.) | 9.2 (284) |
| Gastrointestinal disorder | 13.0 (398) |
| Diabetes | 2.2 (68) |
| Age in Years | |
| 18–21 | 1.3 (39) |
| 22–45 | 21.7 (666) |
| 46–65 | 38.5 (1181) |
| > = 66 | 38.1 (1171) |
| Length of Stay in Days | |
| 1 | 17.7 (554) |
| 2 | 23.7 (729) |
| 3 | 15.2 (468) |
| 4 | 11.0 (38) |
| 5 | 8.1 (250) |
| 6 or more | 24.2 (742) |
aMay not sum to 100 % due to missing data
Table 2.
Patient Language and Presence of Interpreter on Day of Admission or Discharge from Hospital
| Encounter with Interpreter | All LEP Patients | Spanish | Portuguese | Vietnamese | Albanian | Russian | Other |
|---|---|---|---|---|---|---|---|
| % (n) | % (n) | % (n) | % (n) | % (n) | % (n) | ||
| Neither day of admission nor day of discharge | 13.8 (423) | 12.4 (247) | 6.7 (21) | 12.8 (23) | 9.2 (16) | 25.8 (23) | 30.5 (93) |
| Admission, but not on discharge | 30.8 (963) | 30.8 (616) | 34.5 (108) | 36.1 (65) | 33.9 (59) | 30.3 (27) | 28.9 (88) |
| Discharge, but not on admission | 15.8 (482) | 16.0 (320) | 6.1 (19) | 17.2 (31) | 17.8 (31) | 21.3 (19) | 20.3 (62) |
| Both day of admission & discharge | 39.0 (1192) | 40.8 (816) | 52.7 (165) | 33.9 (61) | 39.1 (68) | 22.5 (20) | 20.3 (62) |
| TOTAL | 100 % | 100 % | 100 % | 100 % | 100 % | 100 % | 100 % |
Chi-square = 168.3, df = 15, P < 0.001
Table 3 shows that patients who did not have an interpreter present on admission and discharge were older and had the highest average cost weight (1.98), which was the highest of all four language interpretation groups. These two characteristics were included in multivariable regression models to control for severity and age effects on length of stay. Their associations were nonlinear and the best fit was using a quadratic function for both severity and age.
Table 3.
Patient Age and Severity of Illness with Presence of Interpreter on Day of Admission or Discharge from Hospital
| Encounter with Interpreter | n | Mean Severity Weight (S.E.) | Median Severity | Mean Age in Years (S.E.) | Median Age |
|---|---|---|---|---|---|
| Neither on admission nor discharge | 423 | 1.98 (0.13) | 1.18 | 63.1 (0.81) | 64.8 |
| Admission, but not on discharge | 963 | 1.56 (0.05) | 1.10 | 57.2 (0.54) | 58.8 |
| Discharge, but not on admission | 482 | 1.36 (0.08) | 1.00 | 59.9 (0.80) | 62.8 |
| Both day of admission and discharge | 1192 | 1.34 (0.03) | 1.03 | 56.5 (0.48) | 58.6 |
Statistically significant differences in mean patient age and severity of illness among patients with encounters with interpreters, ANOVA, P < 0.001
Table 4 shows the results of a mixed-model regression for length of stay in days (LOS) with a random effect for patients that accounts for the association of repeat hospitalization on differences among patients. Adjusted for all patient characteristics (i.e., age, gender, illness severity, and main primary diagnoses), no statistically significant differences in length of stay were observed among the different language groups. In general, men were in the hospital slightly longer than women, a little over one-half of a day (regression coefficient = 0.69). Patients with a primary diagnosis other than cardiovascular disease were hospitalized shorter than other patients (β = -2.07, SE = 0.33).
Table 4.
Regression Results for Patient Characteristics Associated with Length of Stay (in days)
| Regression coefficient (Standard Error) | P | Regression coefficient (Standard Error) | P | |
|---|---|---|---|---|
| Intercept | 3.98 (0.20) | 3.58 (1.14) | < 0.01 | |
| Presence of an Interpreter | ||||
| Neither admission nor discharge | 2.31 (0.53) | <0.001 | 1.49 (0.46) | < 0.01 |
| Discharge, but not admission | 0.87 (0.36) | 0.016 | 0.76 (0.32) | 0.02 |
| Admission, but not discharge | 0.74 (0.29) | 0.011 | 0.25 (0.25) | 0.33 |
| Both admission and discharge | Reference | Reference | ||
| Patient’s Preferred Language | ||||
| Spanish | –0.48 (0.38) | 0.21 | ||
| Portuguese | –0.63 (0.51) | 0.22 | ||
| Vietnamese | –0.27 (0.57) | 0.64 | ||
| Albanian | –0.50 (0.59) | 0.39 | ||
| Russian | 0.13 (0.75) | 0.86 | ||
| Other | Reference | |||
| Gender | ||||
| Male | 0.69 (0.23) | < 0.01 | ||
| Female | Reference | |||
| Diagnosis of Cardiovascular Disease | ||||
| Not Cardiovascular disease | –2.07 (0.33) | < 0.001 | ||
| Cardiovascular disease | Reference | |||
| Age | ||||
| Age in years | –0.09 (0.04) | 0.02 | ||
| Age in years squared | 0.001 (0.001) | 0.01 | ||
| Illness Severity | ||||
| Severity weight | 2.30 (0.14) | <0.01 | ||
| Severity weight squared | –0.02 (0.01) | 0.01 | ||
The regression model used to adjust for patient characteristics used a quadratic function to account for non-linear effects of age and illness severity. Younger patients are hospitalized longer with a decline in length of stay among middle-aged patients with increasing length of stay for older patients. The severity of illness coefficients for severity and severity squared (β = 2.30, SE = 0.14 and β = –0.02, SE = 0.01, respectively) indicate a steep increase in length of stay associated with severity that flattens out among the oldest patients.
Patients who did not have an interpreter present on both admission and discharge days were in the hospital about 1.5 days longer than patients who had interpreters on both days (β = 1.49, SE = 0.46). In addition, patients who had interpreter present on discharge but not admission days had longer LOS (β = 0.87, SE = 0.36).
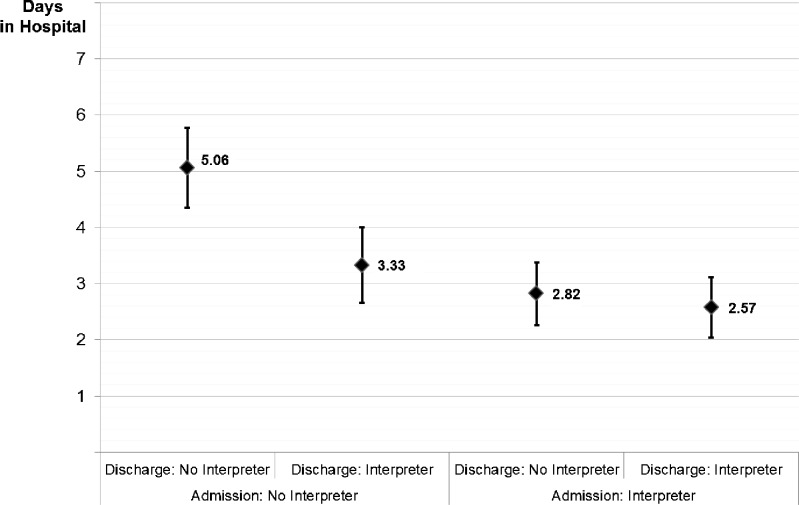
Figure 1 shows the mean adjusted LOS for the four interpretation conditions, controlling for age, illness severity and other patient characteristics. Means shown in the figure are for a female, 60-year-old patient with a severity index of 1.05. Patients who received interpreters on both admission and discharge days had a mean LOS of 2.57, whereas patients who received interpretation neither on admission nor discharge days had a mean adjusted LOS of 5.06 days, significantly longer, P < 0.001. The figure shows that the lower limit for no admission/discharge interpretation is 4.35 days and the upper limit for both conditions for having an interpreter on day of admission (i.e., interpreter at admission and not discharge; interpreter at both admission/discharge day) are less than 4.35 (3.38 and 3.11, respectively). Hence, those patients who had no interpreter on admission and discharge were in statistically significantly longer than patients who had an interpreter at admission, regardless of whether or not they had an interpreter present on discharge day.
Figure 1.
Adjusted length of hospital stay among patients who requested interpreter services and presence of interpreter on day of admission or discharge from hospital. Source: Adjusted means from mixed model regression with patient characteristics (age, illness severity, gender, major diagnosis, and language) and a random effect for patient, assuming a mean age of 60 and a mean severity weight of 1.05.
Of the 3060 patient admissions we examined for readmission, 529 (17.3 %) were readmission events within 30 days of discharge. The 30-day readmission rates for four patterns of interpretation are as follows: 24.3 % (103) of the 423 patient admissions who did not have an interpreter present either at admission and discharge were readmitted within 30 days, compared to 16.9 % (163/963) of patients with an interpreter at admission only, 17.6 % (85/482) of those with an interpreter at discharge only, and 14.9 % (178/1192) with an interpreter at both admission and discharge day (Chi-square = 19.5, df = 3, P < 0.001). Table 5 shows that the logistic regression model predicting readmission that included patient age, gender, severity of illness, language, length of hospital stay in days, and receipt of interpretation as independent variables was not statistically significant (Hosmer & Lemeshow Test Chi-square = 8.10, df = 8, P = 0.42). However, adjusted for age, severity, LOS, and language, patients who received interpretation at admission and/or at discharge were less likely to be readmitted with 30 days than patients who received no interpretation.
Table 5.
Patient Characteristics Associated with Hospital Readmission within 30 days
| B (S.E.) | P | Odds Ratio | |
|---|---|---|---|
| Intercept | –1.37 (0.51) | 0.01 | 0.25 |
| Presence of an Interpreter | |||
| Both admission and discharge | –0.39 (0.15) | <0.01 | 0.67 |
| Discharge, but not admission | –0.36 (0.17) | 0.03 | 0.69 |
| Admission, but not discharge | –0.53 (0.15) | <0.01 | 0.59 |
| Neither admission nor discharge | Reference | ||
| Patient’s Preferred Language | |||
| Spanish | 0.09 (0.17) | 0.59 | 1.09 |
| Portuguese | –0.08 (0.23) | 0.73 | 0.92 |
| Vietnamese | 0.21 (0.24) | 0.38 | 1.24 |
| Albanian | 0.30 (0.24) | 0.22 | 1.35 |
| Russian | 0.10 (0.31) | 0.75 | 1.11 |
| Other | Reference | ||
| Gender | |||
| Male | 0.25 (0.010) | 0.01 | 1.28 |
| Female | Reference | ||
| Diagnosis of Cardiovascular Disease | |||
| Not Cardiovascular disease | –0.04 (0.15) | 0.81 | 0.96 |
| Cardiovascular disease | Reference | ||
| Length of Hospital Stay (in days) | 0.02 (0.01) | 0.01 | 1.02 |
| Age | |||
| Age in years | –0.01 (0.02) | 0.62 | 0.99 |
| Age in years squared | 0.0001 (0.0001) | 0.51 | 1.00 |
| Illness Severity | |||
| Severity weight | 0.03 (0.07) | 0.69 | 1.03 |
| Severity weight squared | –0.01 (0.01) | 0.21 | 0.99 |
Homer & Lemenshow test: chi-square = 8.10, df = 8, P = 0.42
Discussion
Our research shows that LEP patients who did not receive professional interpretation on date of admission and discharge experienced a more lengthy hospitalization with an average of 1.5 days longer than LEP patients who received these services. Specifically, a patient’s access to professional interpretation at admission seems to have had the greatest effect on LOS. In addition, patients who do not have access to interpretation at admission or discharge are more likely to be readmitted within 30 days.
We controlled for variables that were most likely to affect LOS including age, gender, severity of illness, primary language spoken and major type of illness. There are still a few limitations to the study, though. The first is our lack of a calculated LOS for an English-speaking comparison group. Despite this omission, we were able to show a statistically significant difference in LOS within our group of LEP patients. The other unknown information concerns how often family members or untrained staff are providing interpretation or whether bilingual providers were able to speak directly with patients during provision of care. This may explain why some patients received professional interpretation and others did not. Research has shown a negative effect of using family members to interpret, with more confusion as a result.6 One might hypothesize that this is more likely to adversely affect LOS. In comparison, bilingual providers have a positive impact on patient satisfaction and understanding of their illness.4,13 Thus, they may be more likely to shorten LOS potentially decreasing the patterns of LOS we observed in our analysis. These types of “untrained” interpreters may also explain why some patients did not receive qualified interpretation at various times during their admission. In addition to unqualified interpretation use, it may be that a qualified interpreter was used in the emergency room, but the admission day wasn’t recorded until the following day when the patient was formally admitted to the hospital. Our data does not include time of admission, which may have clarified this situation. Hypothetically, this situation would more likely positively influence LOS. Finally, it has been shown that often interpreters are not called because of inadequate access to professional interpretation and time constraints, but in her 2011 study on resident use of interpretation, Diamond et al. found that time and access are not the only issues, but the reasons are more complex with residents often just feeling they can “get by” without an interpreter.14 At the time that this study took place, very little phone interpretation was being used in our hospital system, so providers relied upon on site professional interpreters.
Another limitation includes that the study took place within one institution and may not be entirely applicable to other hospitals. Socioeconomic status of our patients was not collected and may affect a patient’s ability to advocate for interpretation. Our patients were from diverse ethnic backgrounds; however, they all had limited English proficiency that may have similarly impacted their length of stay. We also do not have data on the mental health and alertness of the patients. If a patient was unable to communicate because of decreased mental capacity, and his family all spoke English, an interpreter may have been less likely to be called. Of note, we did not include patients that were admitted for purely mental health reasons. In addition, a patient’s language preference is entered into the hospital’s registration system any time a patient is seen within the system, so even if language preference is not able to be collected at admission the data may already be recorded from a previous visit to the system, or would be obtained from a patient’s health care proxy. Although mental status would certainly affect LOS, it would also be accounted for in a patient’s illness severity, which we did control for in our analysis.
Another potential limitation of our analysis could result from an admission that was very brief (i.e., one to two days). Moreover, analyzing other indicators of interpretation status, such as the number of interpretations per day might be artificially high as potentially they could receive just one interpretation that counts for both admission and discharge. We did run our analysis with and without these brief admissions and found no differences in the conclusions.
In summary, this study supports an argument for the use of professional interpreters by reducing length of stay and 30-day readmission rates for LEP patients. The impact on a hospital that cares for a large proportion of LEP patients could be significant. Best practices are still being developed to help institutions determine when telephonic interpretation is equally appropriate as on-site interpreters as this method can sometimes help alleviate some of the financial burden of providing interpretation. Interpretation at admission seems to be especially important as it has the greatest impact on LOS. This intuitively makes sense since a patient’s history accounts for approximately 70 % of the necessary information to formulate a correct diagnosis. Further research could be directed at controlled studies that target LEP patients to receive professional interpretation at admission as compared to LEP patients who may or may not receive these services. The likelihood of a patient being admitted within 30 days of discharge seems to be associated with having an interpreter at either admission or discharge. As more research is done on the economic impact of inadequate interpretation for LEP patients, the business case for providing interpretation will be established and offer support for a model in which providing professional interpreters makes good medical and economic sense.
Electronic Supplementary Material
(DOC 116 kb)
Acknowledgements
Connie Camelo, Director of Interpreter Services, UMass Memorial Health Care.
This study was partially supported through a grant from Commonwealth Medicine, the health care consulting division of University of Massachusetts Medical School.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Poster presentation at North American Primary Care Research Group Annual meeting (NAPCRG) October 20-23, 2007 Vancouver, British Columbia; Oral presentation at NAPCRG 2009 Annual meeting November 15-18, 2009, Montreal, Quebec; Oral presentation at 2010 International Medical Interpreters Assoc., annual meeting 9/4/2010, Boston, MA
References
- 1.U.S. Census Bureau. Language use and English speaking ability. 2008.
- 2.Flores G. The impact of medical interpreter services on the quality of health care: a systematic review. Med Care Res Rev. 2005;62(3):255–299. doi: 10.1177/1077558705275416. [DOI] [PubMed] [Google Scholar]
- 3.David R, Rhee M. The impact of language as a barrier to effective health care in an underserved urban Hispanic community. Mt Sinai J Med. 1998;65:393–97. [PubMed] [Google Scholar]
- 4.Baker D, Parker R, Williams M, Coates W, Pitkin K. Use and effectiveness of interpreters in an emergency department. JAMA. 1996;275:783–88. doi: 10.1001/jama.1996.03530340047028. [DOI] [PubMed] [Google Scholar]
- 5.Karliner L, Jacobs E, Chen A, Mutham S. Do professional interpreters improve clinical care? A systematic review of the literature. Heal Serv Res. 2007;42(2):727–754. doi: 10.1111/j.1475-6773.2006.00629.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ebden P, Bhatt A, Carey O, Harrison B. The bilingual consultation. Lancet. 1988;331(8581):347. doi: 10.1016/S0140-6736(88)91133-6. [DOI] [PubMed] [Google Scholar]
- 7.Flores G, Laws M, Mayo S, et al. Errors in medical interpretation and their potential clinical consequences in pediatric encounters. Pediatrics. 2003;111(1):6–14. doi: 10.1542/peds.111.1.6. [DOI] [PubMed] [Google Scholar]
- 8.John-Baptiste A, Naglie G, Tomlinson G, et al. The effect of English language proficiency on length of stay and in-hospital mortality. J Gen Inter Med. 2004;19:221–228. doi: 10.1111/j.1525-1497.2004.21205.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Karliner LS, Kim SE, Meltzer DO, Auerbach AD. Influence of language barriers on outcomes of hospital care for general medicine inpatients. J Hosp Med. 2010;5(5):276–282. doi: 10.1002/jhm.658. [DOI] [PubMed] [Google Scholar]
- 10.Jacobs E, Sadowski L, Rathouz P. The impact of an enhanced interpreter service intervention on hospital costs and patient satisfaction. J Gen Inter Med. 2007;22(Suppl 2):306–11. doi: 10.1007/s11606-007-0357-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Benbassat J, Taragin M. Hospital readmissions as a measure of quality of health care: Advantages and limitations. Arch Intern Med. 2000;160:1074–1081. doi: 10.1001/archinte.160.8.1074. [DOI] [PubMed] [Google Scholar]
- 12.García-Pérez L, Linertová R, Lorenzo-Riera A, Vázquez-Díaz JR, Duque-González B, Sarría-Santamera A. Risk factors for hospital readmissions in elderly patients: a systematic review. QJM. 2011;104(8):639–651. doi: 10.1093/qjmed/hcr070. [DOI] [PubMed] [Google Scholar]
- 13.Baker D, Hayes R, Fortier J. Interpreter use and satisfaction with interpersonal aspects of care for Spanish-speaking patients. Med Care Res Rev. 1998;36:1461–70. doi: 10.1097/00005650-199810000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Diamond L, Schenker Y, Curry L, Bradley E, Fernandez A. Getting by: Underuse of interpreters by resident physicians. J Gen Inter Med. 2008;24(2):256–62. doi: 10.1007/s11606-008-0875-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC 116 kb)