Abstract
Objectives: Web-based applications have been developed that allow patients to enter their own information into secure personal health records. These applications are being promoted as a means of providing patients and providers with universal access to updated medical information. The authors evaluated the functionality and utility of a selection of personal health records.
Design: A targeted search strategy was used to identify eleven Web sites promoting different personal health records. Specific criteria related to the entry and display of data elements were developed to evaluate the functionality of each PHR. Information abstracted from an actual case was used to create a series of representative PHRs. Output generated for review was evaluated to assess the accuracy and completeness of clinical information related to the diagnosis and treatment of specific disorders.
Results: The PHRs selected for review employed data entry methods that limited the range and content of patient-entered information related to medical history, medications, laboratory tests, diagnostic studies, and immunizations. Representative PHRs created with information abstracted from an actual case displayed varying amounts of information at basic and comprehensive levels of representation.
Conclusions: Currently available PHRs demonstrate limited functionality. The data entry, validation, and information display methods they employ may limit their utility as representations of medical information.
Consumer advocates have raised concerns about the extent to which decentralization of health care has led to the dispersal of personal medical information.1–3 Recognizing that increased mobility and managed care restrictions may drive patients to seek care from different providers, some advocates have recommended that patients adopt a proactive stance toward collecting and organizing their own medical information.4,5 Until recently, efforts directed at providing patients with approaches to this task have promoted document organization systems and specialized software applications. Document organization systems provide patients with templates and binders to store copies of medical records.6 Software applications allow patients to enter information abstracted from medical records into files stored on personal computers.7
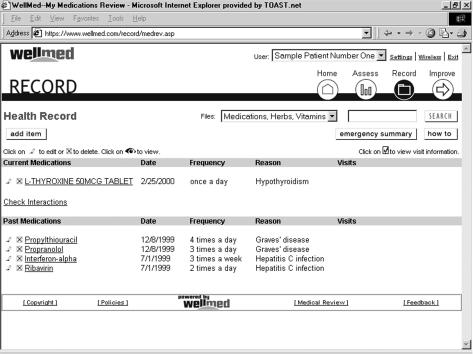
Recently, a number of Web-based applications have been developed as resources to provide patients with secure access to personal medical information.8–10 Configured along the lines of standard provider-entered records, these personal health records (PHRs) allow patients to directly enter information about their own diagnoses, medications, laboratory tests, diagnostic studies, and immunizations. Host sites use this information to generate records that can be displayed for review or transmitted to authorized receivers (Figure 1▶).
Figure 1 .
WellMed Personal Health Record screen displaying current and past medication information
Versions of these records are being promoted by a number of different consumer health care Web sites. Although a few have been set up by nonprofit organizations, most have been developed as commercial ventures. While initial revenue models were based on sales of advertising, current business strategies aim to use PHRs to provide laboratory, prescription, and billing information to designated providers.11 One prominent commercial site recently reported enrollment of 10,000 active users based in the United States.12
Most PHRs in current use are designed to serve as static repositories for personal medical information. Advertisements depict hypothetical situations in which access to a centralized record might help patients relate accurate histories during clinical encounters, check for drug interactions when filling new prescriptions, or avoid unnecessary duplication of laboratory tests and diagnostic studies.13 Promotional materials place a particular emphasis on the potential use of PHRs in emergency situations.14 In circumstances in which a patient might be incapacitated or unable to provide a history, providers could access an updated PHR to obtain critical information about allergies, medications, and diagnoses.15 A few PHRs are being promoted as resources to guide self-monitoring and disease management.16,17
To date, there have not been any studies evaluating the accuracy or utility of medical records generated using patient-entered information.12 One pilot study focused on evaluating the performance of a Web-based application designed to collect verifiable patient-entered information detailing family health histories.18 A few studies have evaluated the utility of patient-held summaries of institutional records, documenting significant improvements in levels of compliance with monitoring protocols and immunization schedules.19–22 A number of recent initiatives have focused on the development of resources targeted to provide patients with direct online access to their own institutional records.23–25 One recent study reviewed a selection of PHRs with a specific focus on features that might affect their utility as resources for critical care, noting significant problems with provisions for emergency access and storage of digitized images.26
In an effort to carry out an assessment of these untested resources, we adopted a systematic approach to evaluate the functionality and clinical utility of a selection of currently available PHRs.
Methods
Our assessment was carried out in three phases. The first phase focused on the identification and selection of candidate PHRs. The second phase focused on the development of criteria related to the entry and display of data elements that would need to be met for PHRs to serve as adequate representations of information. These criteria were used to evaluate the functionality and utility of a selected group of PHRs during the third phase of our assessment.
Identification and Selection of Candidate Personal Health Records
We performed a search to identify sites promoting PHRs. Entered search terms included combinations of the words “patient,” “own,” “online,” “personal,” “health,” “medical,” and “record.” We explored identified sites in detail, following links from articles, specialty guides, commercial sites, and personal Web pages to locate sites providing access to PHRs. We identified 19 independent sites promoting different versions of PHRs. We excluded four of these sites from consideration because of their narrow focus on specific diseases. We excluded two additional sites because of their connections to disease management programs. We also excluded a site that provided access to a hospital information system. Twelve remaining sites were selected for review (Table 1▶). During the course of our evaluation, we opted to exclude one of these sites because of recurrent problems encountered while trying to establish and maintain access.
Table 1 .
Personal Health Records
| Web Site | Record | URL |
|---|---|---|
| Dr. I-Net | My Medical Record | www.aboutmyhealth.com |
| HealthCompass | Lifelong Health Record | www.healthcompassnet.com |
| MedicalEdge | Medical Registry | www.medicaledge.com |
| MedicalRecord.com | Your Medical Record | www.medicalrecord.com |
| MedicData | MedicData | www.medicdata.com |
| Medscape AboutMyHealth | Personal Health Record | www.aboutmyhealth.com |
| myhealthnotes.com | Personal Health Manager | www.myhealthnotes.com |
| PersonalMD | My Medical Records | www.personalmd.com |
| TheDailyApple | Health Records | www.thedailyapple.com |
| VistaLink | Health Profile | www.vistalink.com |
| WebMD | My Health Record | www.webmd.com |
| WellMed | Health Record | www.wellmed.com |
Development of Criteria
We identified five prospective functions of PHRs, based on our survey of aggregate claims appearing in advertising and promotional materials (Table 2▶). To establish a basis for systematic evaluation, we identified specific criteria that would need to be met for a given PHR to perform each of these functions. Given the lack of professional oversight in the creation of PHRs, most of these criteria outlined requirements for accurate entry of information and verification of reported test and study results. Other criteria outlined requirements for the provision of different routes of access, links to consumer health care information, functions to process and interpret information, and functions to provide secure communication between patients and providers. We identified specific data elements that would need to be included in a PHR to fulfill each of these requirements.
Table 2 .
Criteria for Evaluation of Functionality
| Function | Requirements |
|---|---|
| Providing Web-based access to personal medical information | ▪ Secure password-protected patient access ▪ Capacity to provide authorized provider access ▪ Capacity to provide directed emergency access |
| Providing an organized summary of personal medical information for presentation to health care providers | ▪ Accurate entry of past and current medical conditions, including information about diagnosis and treatment ▪ Accurate entry of past and current medications, including information about indication, dose, frequency, and duration ▪ Verification of laboratory test results ▪ Verification of diagnostic study results ▪ Verification of immunizations, including information about dates and sequences |
| Serving as a portal to patient-specific consumer-level health care information | ▪ Accurate entry of medical conditions ▪ Accurate entry of medications ▪ Capacity to provide links to consumer health care information |
| Providing interpretive information about laboratory test and diagnostic study results | ▪ Accurate entry of medical conditions ▪ Accurate entry of medications ▪ Verification of laboratory test results ▪ Verification of diagnostic study results ▪ Capacity to interpret laboratory test and diagnostic study results |
| Serving as a database of information for patient-specific self-monitoring and disease management | ▪ Accurate entry of medical conditions ▪ Accurate entry of medications ▪ Verification of monitoring study results ▪ Capacity to interpret monitoring study results ▪ Capacity to provide evaluation and treatment recommendations ▪ Capacity to provide secure communication between patients and providers |
Evaluation of Functionality and Utility
Our evaluation of the functionality of each PHR focused on testing different routes of access while documenting and characterizing representations of specific data elements in each category of required information (Table 3▶). To evaluate the functionality of each site, we generated representative PHRs using a standard profile of information. We identified six categories of required information that fell under general headings of personal information, medical history, medications, laboratory tests, diagnostic studies, and immunizations. We entered requested information without any truncation or omission, documenting the data-entry methods used to enter each type of information. Completed PHRs were printed for review. If a summary version was available for electronic transmission, it was relayed and printed for review.
Table 3 .
Functionality of Personal Health Records
| Web Site* | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Access: | |||||||||||
| Password-protected patient access | X | X | X | X | X | X | X | X | X | X | X |
| Authorized provider access | X | X | X | X | |||||||
| Directed emergency access | X | X | X | X | X | X | |||||
| Medical conditions: | |||||||||||
| Verification | X | ||||||||||
| Distinction between past and current | X | X | X | ||||||||
| Diagnosis | X | X | X | X | X | X | X | X | |||
| Treatment | X | X | X | X | X | ||||||
| Links | X | ||||||||||
| Medications: | |||||||||||
| Verification | |||||||||||
| Distinction between past and current | X | X | X | X | |||||||
| Indication | X | X | X | ||||||||
| Dose | X | X | X | X | X | X | X | X | |||
| Frequency | X | X | X | X | X | X | |||||
| Duration | X | X | X | X | X | ||||||
| Links | X | ||||||||||
| Laboratory tests: | |||||||||||
| Verification | X | X | X | ||||||||
| Results | X | X | X | X | X | X | X | X | X | ||
| Interpretation | X | ||||||||||
| Links | X | X | |||||||||
| Diagnostic tests: | |||||||||||
| Verification | X | X | |||||||||
| Results | X | X | X | X | X | X | |||||
| Interpretation | |||||||||||
| Links | X | ||||||||||
| Immunizations: | |||||||||||
| Verification | |||||||||||
| Results | X | X | X | X | X | X | X | X | X | ||
| Interpretation | X | X | X | ||||||||
| Links | X | ||||||||||
*De-identified from listing in Table 1▶.
To evaluate the clinical utility of the PHRs selected for review, we used objective information abstracted from an actual test case to generate a series of representative PHRs. We reviewed the output of each PHR to document the extent to which it accurately and completely presented diagnostic and therapeutic information.
The case selected for this purpose represented a patient seen in consultation for a thyroid condition. The initial referral had been prompted by identification of possible hyperthyroidism ascribed to Graves' disease. Subsequent evaluation revealed an extensive history incorporating a prior diagnosis of hepatitis C infection, immunization against hepatitis A and hepatitis B, treatment with ribavirin and interferon-alpha, development of autoimmune thyroiditis precipitated by interferon-alpha, and eventual progression to a state of persistent hypothyroidism.27,28
This case presented a number of considerations that would test the limits of any representation of medical information. Each diagnosis represented a chronic condition requiring specific treatment with an oral or subcutaneously injected medication. Clinical evaluation was based on a range of laboratory tests and radiographic studies used to establish diagnoses and monitor treatments. Specific indices reflected a transition from a hyperfunctioning condition to a hypofunctioning condition, prompting a change in diagnosis with alteration of therapy. Treatment of one of the conditions included specific immunizations, one of which was administered as a series of injections.
Outpatient chart records related to this case covered a span of 19 months. After reviewing these records, we abstracted relevant data elements from clinic notes and test reports to generate a standard profile of information. This information was entered along with a profile of anonymous personal information to generate a series of representative PHRs. In the course of entering medical history information, we elected to use the term “Graves' disease” in place of “autoimmune thyroiditis,” since Graves' disease was more likely to appear on pick lists of diagnoses. The PHRs that were generated were checked for accuracy before completed versions were printed for review.
Our evaluation of the utility of each PHR focused on a stratified assessment of output presented for display from a clinical perspective. In an effort to establish rigorous criteria for evaluation, we opted to review this output from the standpoint of different providers who might be presented with a PHR as a summary of a patient's medical history. To provide a balanced view with regard to different levels of complexity, we elected to evaluate each PHR at two distinct levels of representation.
At a basic level, we reviewed the output of each PHR to see if it provided the minimum amount of information a primary care provider would need to manage a simple problem based on the results of objective laboratory tests. Our evaluation at this level focused on the identification of essential data elements related to the diagnosis and treatment of persistent hypothyroidism (Table 4▶). At a more comprehensive level, we reviewed the output of each PHR to see whether it provided the minimum amount of information a consulting subspecialist would need to accurately trace the course of events contributing to a complete clinical history. Our evaluation at this level focused on the identification of essential data elements related to the diagnosis of hepatitis C infection, subsequent treatment with interferonalpha, and the emergence of complications associated with the development of autoimmune thyroiditis (Table 4▶). To set reasonable limits, we excluded additional tests that might be indicated to eliminate different causes of hepatitis. We also excluded quantitative hepatitis C RNA results that might be used to guide the treatment of hepatitis C infection, as documented values were not available at the time the PHRs were generated.29
Table 4 .
Clinical Utility of Personal Health Records
| Web Site* | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Basic level: | |||||||||||
| Diagnostic elevated TSH and low T4 | X | X | X | X | X | ||||||
| Decline in TSH indicating response to therapy | X | X | X | X | |||||||
| Current levothyroxine dose | X | * | X | † | X | X | X | X | X | ||
| Comprehensive level: | |||||||||||
| Diagnosis of hepatitis C infection | |||||||||||
| Elevated transaminases | X | X | X | X | X | ||||||
| Hepatitis C antibodies | X | X | X | X | X | ||||||
| Treatment with interferon-alpha | |||||||||||
| Liver biopsy results | X | X | X | X | X | ||||||
| Interferon-alpha regimen | X | X | X | † | X | X | |||||
| Hepatitis A immunization | X | † | X | X | X | X | X | X | |||
| Hepatitis B immunization | ‡ | † | ‡ | X | X | ‡ | X | ‡ | |||
| Diagnosis of interferon-alpha-associated autoimmune thyroiditis | |||||||||||
| Suppressed TSH, elevated T4 | X | X | X | X | X | ||||||
| Thyroid scan results | X | X | X | X | X | ||||||
| Timing relative to treatment | X | ||||||||||
* Unable to specify dose of levothyroxine in micrograms or fractions of milligrams.
† Unable to display entered information
‡ Unable to specify series.
Results
Functionality
Access
Each of the 11 sites displayed explicitly stated privacy and security policies at the point of registration. Each site provided password-protected access to entered information, with one requiring entry of an additional identification phrase. Four sites provided authorized physicians with password-protected access to viewable summaries of entered information.
Seven sites provided emergency access to patients' information. Three of these sites allowed patients to create a wallet card listing a URL along with an identification phrase. In an emergency situation in which a patient might be incapacitated or unable to relate a history, providers would be able to use the information on this card to access a viewable summary of a patient's PHR. Two sites allowed patients to transmit a printable summary of a PHR to a designated fax number, although neither elaborated a mechanism that would enable providers to receive this information if a patient were completely incapacitated.
Personal Information
Each site allowed patients to enter personal contact information that typically included a current home address, home phone number, work phone number, cellular phone number, fax number, and e-mail address. Each site also allowed patients to enter information for an individual designated as a primary emergency contact, with seven sites allowing patients to enter information for a secondary emergency contact.
Each site allowed patients to enter contact information for a designated primary physician, with nine sites allowing patients to enter contact information for other physicians. Ten sites allowed patients to enter insurance coverage information.
Medical History
Each site used a different method to guide patients through the process of entering information related to medical conditions. Eight sites directed patients to select conditions from categorized lists. These lists varied widely in content and organization. Most included examples of nonspecific symptoms, general systemic disorders, and specific etiologic diagnoses. In most cases, entry was limited to simple identification, although there were a few notable examples. One site generated an extensive list of subcategories for each condition based on a keyword search using a metathesaurus. Two sites prompted the entry of condition-specific information related to associated symptoms, etiology, diagnosis, and treatment. Sites that did not make use of lists relied on free-text entry.
The range of descriptive information requested for each medical condition was limited. Eight sites asked patients to enter the date of onset of each medical condition, four asked about the physician or provider responsible for treating each condition, and three asked about the actual treatment prescribed for each condition.
Medications
Three sites directed patients to select medications from lists, with two generating listings based on keyword searches. Sites that did not make use of lists relied on free-text entry. A wide range of descriptive information was requested for each medication. Ten sites asked patients to enter the prescribed dose for each medication, seven asked about the frequency of administration, and five asked about starting dates for each medication. Four sites asked about the pharmacy that issued each medication, four asked about the provider responsible for prescribing each medication, and three asked whether each medication was a past or current prescription.
Laboratory Tests
Nine sites allowed patients to enter information about laboratory tests. Two sites were set up to import results from outside sources, although only one was fully functional at the time of review. Six sites directed patients to select laboratory tests from lists. Sites that did not make use of lists relied on free-text entry. A limited range of descriptive information was requested for each laboratory test. Six sites asked patients to enter a date and result for each test. Results were entered as free text without quantification of units or reference ranges. Only one site asked patients to identify the provider responsible for ordering each test.
Diagnostic Studies
Four sites allowed patients to enter information about diagnostic studies. One site directed patients to select diagnostic studies from a list, whereas the others relied on free-text entry. All four sites asked patients to enter a date and result for each study. Results were entered as free text. Only one site asked patients to identify the provider responsible for ordering each study.
Immunizations
Each site allowed patients to enter information related to immunizations. Seven sites directed patients to select different types of immunizations from lists, whereas the others relied on free-text entry. Nine sites asked patients to enter a date for each immunization. Three sites allowed patients to indicate whether a specific dose was part of a series. Three sites asked patients to identify the provider responsible for administering each immunization. None of the sites requested any information about specific antibody titers.
Utility
At a basic level of representation, 5 of the 11 PHRs selected for review incorporated all the data elements needed to manage a simple problem based on the results of objective laboratory tests. Two of these sites were plagued by technical problems that hampered the display of medication information. One was unable to express doses of prescribed medications in micrograms or fractions of milligrams, whereas the other failed to display any values at all. One PHR that relied on the importation of laboratory test results from an outside source was unable to display the full range of results entered in its profile. Four of the remaining PHRs presented accurate medication information without any associated test results. One PHR failed to incorporate any of the essential data elements.
At a more comprehensive level of representation, only 1 of the 11 PHRs selected for review incorporated all the elements needed to provide a complete clinical history. Each of the others was missing at least one critical element. The most uniformly represented elements were listings of immunizations that appeared in designated profiles. Nine PHRs included listings that reported hepatitis A and hepatitis B immunizations, although only four allowed for specification of doses in a series. Five PHRs incorporated complete sets of laboratory test and diagnostic study results, including scanned or entered summaries of biopsy and radiographic study reports. Six PHRs documented a history of treatment with interferon-alpha. Only one PHR included temporal information that linked treatment with interferon-alpha to the development of autoimmune thyroiditis.
Discussion
Overall, the patient-entered PHRs we selected for evaluation demonstrated limited functionality. At a basic level, each site did manage to provide Web-based access to personal medical information. A minority of these sites extended this capacity to provide access to information in emergency situations. This finding was surprising in light of the emphasis placed on this mode of access in the promotion of these applications.
Many of the functions we evaluated were compromised by limitations related to the process of data entry and validation. Each site required patients to select entries from lists or to type information into text fields without much in the way of guidance or explanation. There were no mechanisms to direct patients through the process of selecting appropriate diagnoses. None of the sites provided any directions to help guide patients through the process of abstracting relevant information from prescription labels or test reports. Even simple functions that might ensure greater accuracy, such as spell-checking typed entries or identifying normal dose and reference ranges, were notably lacking. With few exceptions, there were no systems to verify information abstracted from test and study reports. Limited ranges of descriptive information further compromised entries that might be called into question.
Evaluation from a clinical perspective using the example of a test case demonstrated that the PHRs we selected for review provided varying representations of information at increasing levels of complexity. Given the range of information that could be entered, it was surprising that most of these records failed to include the basic data elements needed to manage one of the simpler problems encountered in outpatient medicine. Evaluation at a comprehensive level demonstrated that any inherent deficiencies of representation became magnified in proportion to the number of data elements included in a clinical history. Those PHRs that included listings of information kept different elements segregated in discrete sections without problem-based integration. Actual use of information in clinical practice would require abstraction and rearrangement of elements to provide context for analysis.
The criteria for evaluation outlined in this review set high standards for accuracy and validation. Questions might arise as to whether patient-oriented applications need to be this exacting. Although PHRs may primarily be viewed as an extension of the technologic capacity of the Internet, in truth they appear to embody a new representation of medical information. Despite claims that point to their potential for use in tracking and guiding personal health care, their status as an informational resource is yet to be defined.
When held to the rigorous standards of provider-entered records, PHRs reveal deficiencies and limitations that cast doubt on whether they will ever be able serve as effective primary resources. Of principal concern is the fact that the entire process of data entry assumes that individuals can accurately categorize and prioritize their own medical information. No documented studies have examined the question of whether this strategy is feasible or efficacious.
Additional concerns may be raised by the potential for misrepresentation of patient-entered information. Most currently available PHRs are organized along the lines of standard provider-entered charts. Lists presented for selection use standard medical terminology to describe diagnoses, medications, and laboratory tests. Printed summaries convey an air of medical sophistication. In many respects they appear to be indistinguishable from standardized records used by service agencies and chronic care facilities. There are no signifiers that indicate that the information presented is entirely patient-entered. This lack of distinction raises the serious issue of whether printed summaries of PHRs may be mistaken for provider-entered records.
Strategies to improve performance may vary, depending on the intended uses of future applications. If PHRs are scaled back to provide limited medical history and prescription information, efforts might focus on methods of registering information. At one extreme, providers might be asked to work with patients to supervise the creation of individual profiles. Other approaches might focus on abstraction of information from billing records or pharmacy databases. If PHRs continue to be promoted as entities that mirror the full content of standard institutional records, challenges for refinement will be much greater. At a basic level, patients will need to be guided through the process of sorting through information to determine which elements warrant inclusion. Methods will need to be developed to verify the accuracy of entered information. Logical approaches might focus on optimizing user interfaces to increase accuracy.
The approach we adopted in completing this assessment had certain limitations. Our evaluation of clinical utility was based on a single test case that focused on specialized domains of endocrinology and hepatology. In an effort to overcome the limitations of this approach, output was stratified and analyzed at different levels of representation to reflect the concerns of primary care providers and medical subspecialists.
Questions might arise as to whether information entry performed by a clinically experienced operator provided a realistic simulation of the prospective use of these applications by real patients. Our goal in adopting this approach was directed toward optimizing the accuracy and efficiency of information entry to provide a reliable standard for comparison of representations of data elements. This may have led to overestimation of the functionality of these applications, since the accuracy of information entered by real patients would probably vary to a greater extent with differing levels of knowledge and experience.
Further research should focus on the evaluation of test cases explicitly limited to the entry of data elements that patients are likely to be able to self-report with acceptable degrees of accuracy. It remains to be seen whether PHRs generated by real patients can provide enough reliable information to serve as basic representations of medical information.
Conclusion
The data entry, validation, and information display methods employed by currently available PHRs may limit their ability to serve as adequate representations of medical information for use in clinical practice. Future development of PHRs should be guided by patient-oriented research targeted to evaluate the performance and usability of evolving applications.
References
- 1.Spragins E. Get it in writing. Newsweek. Aug 24, 1998:62. [PubMed]
- 2.Personal and Family Health History. AMA Health Insight Web site. 1997. Available at: http://www.ama-assn.org/insight/yourhlth/per_hlth/per_hlth.htm. Accessed Jul 2000.
- 3.Maintaining a treasure chest: your health record. University of Nebraska Cooperative Extension Web site. 1999. Available at: http://www.ianr.unl.edu/pubs/consumered/hef481.htm. Accessed Jul 2000.
- 4.Savard M. The Savard Health Record: A Six-Step System for Managing Your Healthcare. Alexandria, Va.: Time-Life, 2000.
- 5.Ryan MA. Maintain your medical records. Today's Chemist at Work. 1999;8(8):49–50, 52–53. [Google Scholar]
- 6.MyBodyBook.com Web site. Available at: http://www.mybodybook.com. Accessed Sep 2000.
- 7.CancerOption.com Web site. Available at: http://www.canceroption.com/capmed/index.asp. Accessed September 2000.
- 8.Putting patients at the center. Internet Health Care Web site. 2000. Available at: http://www.internethealthcaremag.com/html/current/050100_1.htm. Accessed Jul 2000.
- 9.Winters R. Your vital signs online. Time. Feb 28, 2000:G4.
- 10.Rashbass J. The patient-owned, population-based electronic medical record: a revolutionary resource for clinical medicine. JAMA. 200;285(13):1765. [PubMed] [Google Scholar]
- 11.Personal communication with Nelson Hazeltine, iVista Group. Oct 24, 2000.
- 12.Waegermann CP. Consumer-driven health care records [lecture]. Presented at: TEPR 2001; Boston, Mass.; May 11, 2001.
- 13.Permanent record: allowing patients to post their own medical records on the Internet is becoming big business. American Medical News Web Site. 1999. Available at: http://www.ama-assn.org/sci-pubs/amnews/pick_99/biza1108.htm. Accessed Feb 2001.
- 14.Online Consumer Health Records: Revolution or Confusion? Journal of AHIMA Web site. 2000. Available at: http://www.ahima.org/journal/features/feature.0003.2.html. Accessed Sep 2000. [PubMed]
- 15.California emergency physicians medical group and PersonalMD introduce online medical records to state's emergency departments. PersonalMD, Inc. Web site. 2001. Available at: http://www.personalmd.com/pressCEP_article.shtml. Accessed Mar 2001.
- 16.Can the Web save disease management? Healthcare Informatics Online Web site. 2000. Available at: http://www.healthcareinformatics.com/issues/2000/03_00/cover.htm. Accessed Sep 2000. [PubMed]
- 17.Tsai CC, Starren J. Patient participation in electronic medical records. JAMA. 2001;285(13):1765. [PubMed] [Google Scholar]
- 18.Cohn W. PM Health Heritage: development and evaluation of a family health history collection and assessment tool [lecture]. Presented at: TEPR 2001; Boston, Mass.; May 11, 2001.
- 19.Hertz CG, Bernheim JW, Perloff TN. Patient participation in the problem-oriented system: a health care plan. Med Care. 1976;14(1):77–9. [DOI] [PubMed] [Google Scholar]
- 20.Hetzel MR, Williams IP, Shakespeare RM. Can patients keep their own peak-flow records reliably? Lancet. 1979;1(8116): 597–9. [DOI] [PubMed] [Google Scholar]
- 21.Miller SA. A trial of parent held child health records in the armed forces. BMJ. 1990;300(6731):1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dickey LL, Petitti D. A patient-held minirecord to promote adult preventive care. J Fam Pract. 199;34(4):457–63. [PubMed] [Google Scholar]
- 23.Cimino JJ, Li J, Mendonca EA, Sengupta S, Patel VL, Kushniruk AW. An evaluation of patient access to their electronic medical records via the World Wide Web. Proc AMIA Symp. 2000:151–5. [PMC free article] [PubMed]
- 24.Jones R, Pearson J, McGregor S, et al. Randomised trial of personalised computer based information for cancer patients. BMJ. 1999;319(7219):1241–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Masys DR, Baker DB. Patient-Centered Access to Secure Systems Online (PCASSO): a secure approach to clinical data access via the World Wide Web. Proc AMIA Annu Fall Symp. 1997:340–3. [PMC free article] [PubMed]
- 26.Schneider JH. Online personal medical records: Are they reliable for acute/critical care? Crit Care Med. 2001;29(8 suppl):196–201. [DOI] [PubMed] [Google Scholar]
- 27.Koh LK, Greenspan FS, Yeo PP. Interferon-alpha induced thyroid dysfunction: three clinical presentations and a review of the literature. Thyroid. 1997;7(6):891–6. [DOI] [PubMed] [Google Scholar]
- 28.Fernandez-Soto L, Gonzalez A, et al. Increased risk of autoimmune thyroid disease in hepatitis C vs. hepatitis B before, during, and after discontinuing interferon therapy. Arch Intern Med. 1998;158(13):1445–8. [DOI] [PubMed] [Google Scholar]
- 29.Pianko S, McHutchison JG. Treatment of hepatitis C with interferon and ribavirin. J Gastroenterol Hepatol. 2000;15(6): 581–6. [DOI] [PubMed] [Google Scholar]