Abstract
The authors developed a novel feature in their clinical information systems, which allows clinicians to request notification about laboratory results. Clinicians who are expecting a particular laboratory result for a particular patient can request a report of the result via an alphanumeric pager as soon as the result is filed into the patient database. This feature has gained popularity and is heavily used in both inpatient and outpatient settings, at a rate of about 2,300 times per month. This event-monitor-based feature illustrates one way that information technology can be applied to improve communication in health care.
Clinicians rely heavily on laboratory data to make medical decisions in various settings. However, the lag between the time when laboratory data become available and when clinicians review and act on them is considerable.1 While certain clinical situations permit such delays, many do not. For example, a patient who has had gastrointestinal bleeding should have further units of blood cross-matched if it is clear the hematocrit has not responded to previous blood transfusions. The conscientious clinician who keeps checking the hospital laboratory information system for pending results can waste a lot of time doing so, and yet not checking may lead to unacceptable delays in patient care.
Several groups, including ours, have developed applications that notify physicians when certain conditions apply.1–10 For example, our group has developed an application that alerts physicians when life-threatening results are present, and that application has been shown to decrease the time it takes for a physician to act on such results.1
Previously described applications, however, were all designed to identify results that somehow are unusual or indicate gross deviation in a patient's status from expected norms. In clinical practice, however, many results, including normal ones, may be important for decision making11 and may warrant rapid notification of physicians. Furthermore, given the variety of user preferences12 and the uniqueness of each clinical scenario, it may be difficult, at least with laboratory results in non-life-threatening cases, for an information system to predict whether a particular result merits urgent notification of a particular user.
We designed an application—called “Result Notification via Alphanumeric Pagers,” or ReNAP—that allows clinicians to make this choice. Using this application, a clinician can indicate that he or she wants to be notified about a particular result for a particular patient, regardless of whether the result is abnormal. In this paper, we report the implementation methods, use statistics, and the results of a user satisfaction survey.
Methods
Setting
This study was performed at the Brigham and Women's Hospital (BWH), a 720-bed tertiary-care academic medical center in Boston, Massachusetts, and a member of the Partners Healthcare System. Computing services at BWH are provided by the Brigham Integrated Computing System (BICS), which supports the clinical information needs of the inpatient services and a large number of outpatient clinics.
Relevant features of BICS at the time of this project included a database of laboratory results, an alphanumeric paging system interface, an event-monitoring infrastructure that had been developed for a critical-result alerting application,1 and an e-mail application (Microsoft Exchange) interface.
Design of ReNAP
ReNAP allows any BWH clinician who is expecting a particular laboratory result for a particular patient to have the result automatically reported via an alphanumeric pager at the time the result is filed into the hospital's patient database.
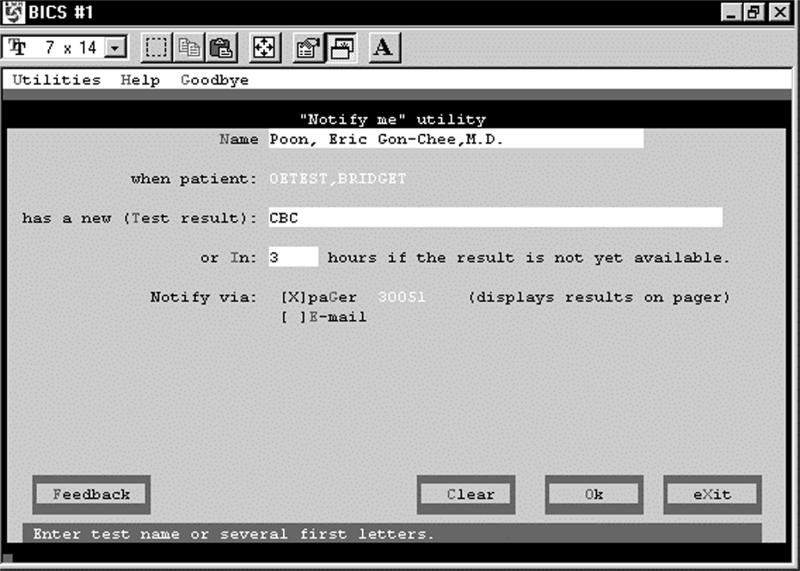
When a clinician decides that a particular laboratory result or set of results warrants rapid notification, he or she accesses the Lab Notification Request screen of ReNAP (Figure 1▶). The clinician specifies the person who should be notified when the laboratory result becomes available. The currently logged-in user will be notified by default, although it is possible to name another clinician.
Figure 1 .
Laboratory Notification Request screen.
The clinician then specifies the individual test (e.g., hematocrit) or test panel (e.g., complete blood count) about which he or she wants to be notified. A test dictionary is accessed to provide matches to the test name the clinician has typed in. Requests can be made on laboratory specimens that are in process (“pending”) or yet to be obtained.
The clinician has the option of asking the system to notify him or her if the result does not become available within a specified time (because the phlebotomist is unable to obtain the blood sample, for example). By changing the notification options on the Lab Notification Request screen, the clinician can choose to be notified by electronic mail instead of (or in addition to) alphanumeric pager.
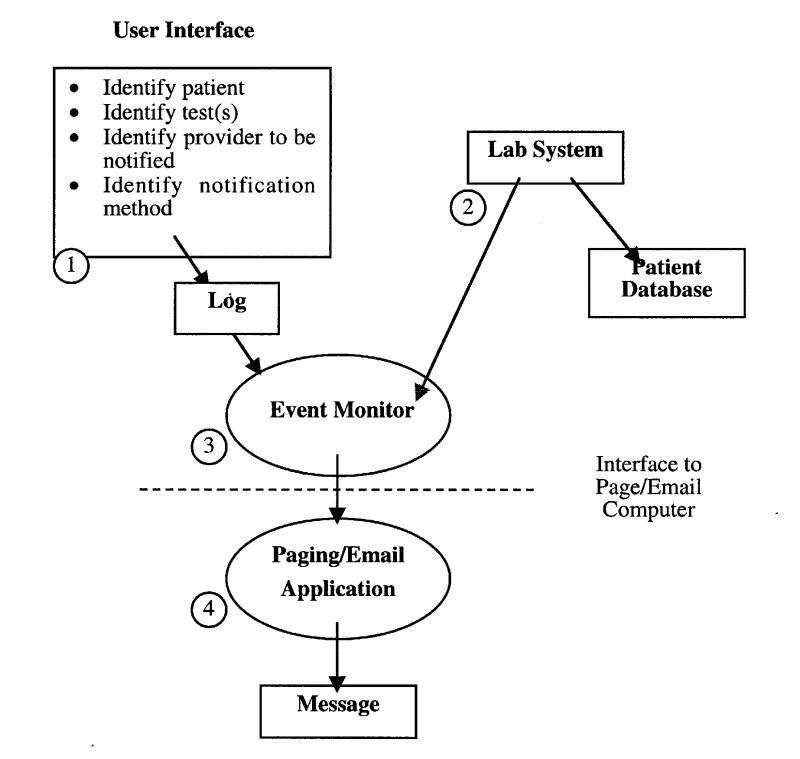
Figure 2▶ shows the architecture of ReNAP. When a new laboratory result is filed in the BICS database, a copy of the data is sent to an event monitor. If the event monitor determines that a notification request has been logged for this kind of laboratory result for this patient, an alphanumeric text page is sent to the appropriate clinician, in the format patient name, medical record number, test, test result(s). For example:
Figure 2 .
Architecture of the ReNAP application. 1) The clinician identifies the patient, the test results, the provider to be notified, and desired method of notification (alphanumeric pager or e-mail). These data are stored in a log. 2) As new results are filed by the laboratory system, a copy is sent to the event monitor. 3) The event monitor examines these results to determine whether any provider wants to be notified about a particular result. 4) If a provider does want to be notified, the information about the result and the name of the person to be notified are sent across an interface to the paging system or the e-mail application.
Test, Bridget (05487033) HCT 31.2
When requested laboratory results fail to become available within a specified time, ReNAP activates, at the time the request is made, a tickler that will go off at the end of the specified time. When the tickler goes off, a special event is sent to the event monitor. If the event monitor determines that the laboratory result has already been sent, no action is taken. Otherwise, a message is sent to the clinician's pager, stating that the result has not been made available in the specified time. For example:
HCT has not been filed for Patient Test, Bridget (05487033)
If a clinician who is to be notified about test results has signed his or her pager out to a covering physician, the system will forward the results to the covering physician.
The current implementation of this feature supports notification of chemistry, hematology, coagulation, and urinalysis results. Notification of microbiology and radiology data is not yet supported, although our intent is to add these domains.
Results
Usage Patterns
ReNAP was released into general use in March 1999, when an e-mail announcement describing the new feature was sent to all house staff and attending physicians. Access was provided via two of the main BICS menus—the inpatient order entry menu, for use by inpatient physicians, and the ambulatory record menu, for use by clinic physicians. Use of ReNAP is entirely voluntary.
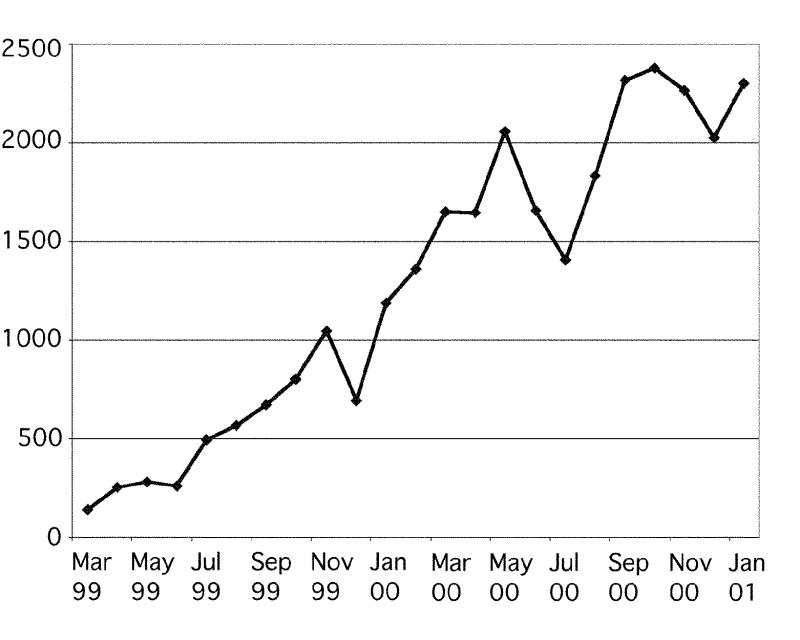
Since its release in March 1999, ReNAP has gained tremendous popularity at the Brigham and Women's Hospital. In the first 24 months of its release, the usage rate has steadily climbed, and as of January 2001, this feature is used about 2,300 times per month (Figure 3▶). During the 12-month period between February 2000 and January 2001, 780 different clinicians used this feature. The top 50 users made 52.5 percent of requests, and the top 100 users made 74.9 percent of requests*.
Figure 3 .
Laboratory notification requests per month (March 1999 to January 2001).
Of the 22,775 requests made between February 2000 and January 2001, 75 percent (17,204 requests) were made for hospitalized patients, and 24 percent (5,352 requests) were made for patients seen in the ambulatory setting (Figure 4▶). The vast majority of users (99.2 percent) preferred notification by alphanumeric pager to notification by e-mail.
Figure 4 .
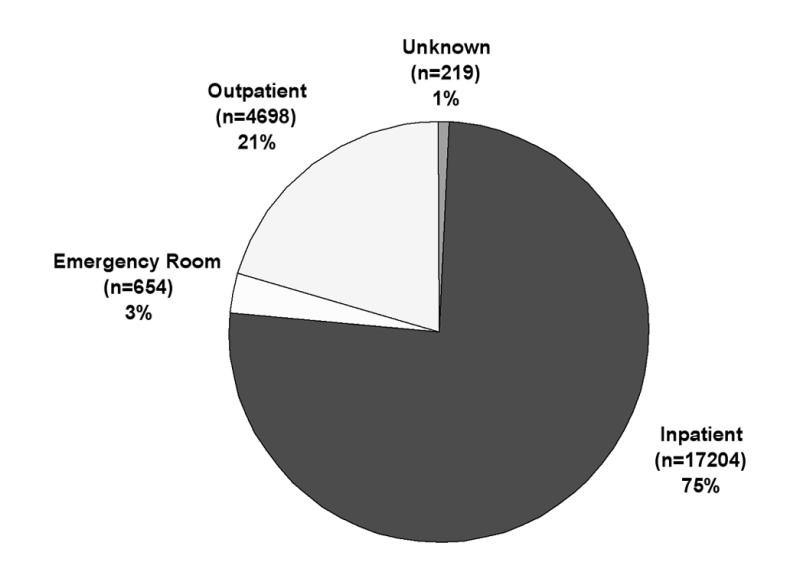
Laboratory notification requests by patient location (22,775 total requests; February 2000 to January 2001).
Figure 5▶ shows the different categories of tests requested for notification with this feature. Data shown again reflect the 12-month period between February 2000 and January 2001. Of all requests in this time period, the combination of electrolytes, complete blood count, and coagulation accounted for 78 percent (17,766 requests).
Figure 5 .
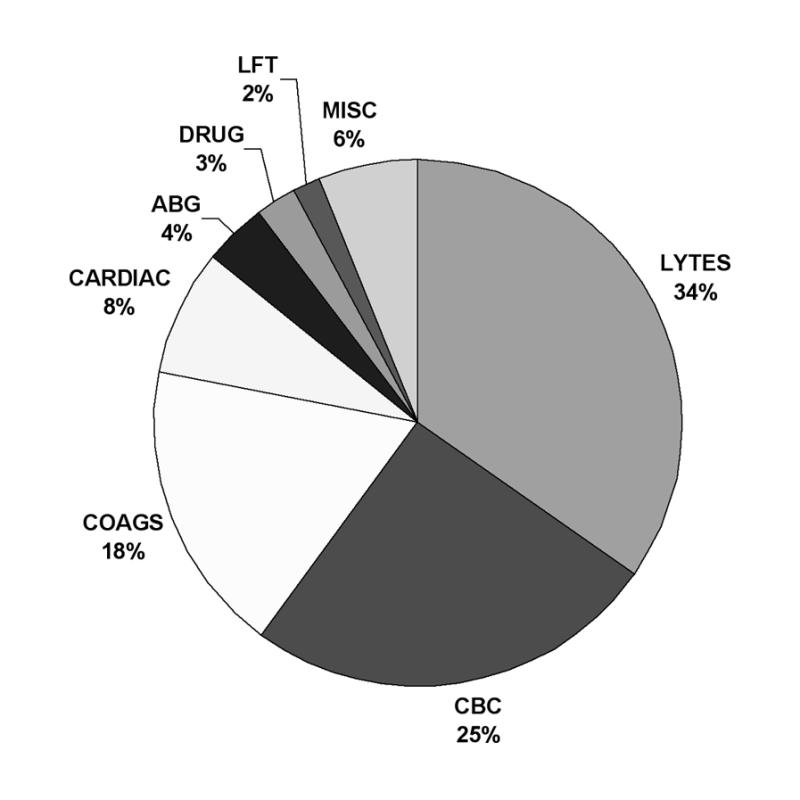
Laboratory notification requests by test category (22,775 total requests; February 2000 to January 2001).
The Departments of Medicine and Surgery were the top users of this feature, accounting for 84 percent of requests. The Departments of Emergency Medicine and Obstetrics–Gynecology ranked third and fourth in usage. Overall, 96.9 percent of all notification requests were made by house staff.
We assessed the effects of training level on the usage of ReNAP. Over a 6-month period (August 2000 to January 2001), 84.4 percent of the 90 medicine and surgery interns (PGY1) used the system at least once a month, compared with 57.8 percent of 135 medicine and surgical residents (PGY2–3 for medicine and PGY2–5 for surgery; chi-square test, p<0.001). Medicine interns were more likely to use ReNAP than medicine residents—73 medicine interns, or 84.9 percent, used ReNAP, compared with 105 residents, or 58.1 percent (chi-square test, p=0.0001). A similar trend was observed with surgery interns—17 interns, or 82.3 percent used ReNAP compared with 30 residents, or 56.7 percent (chi-square test, p=0.074). These data suggest that supervising residents are less likely to use ReNAP than interns, who are primarily responsible for reviewing laboratory data. Other departments were not studied because of relatively small sample sizes.
We also assessed the difference in ReNAP usage between the medicine and surgery house staff. The percentage of house staff who used ReNAP at least once a month was not statistically different between medicine and surgery—73 medicine interns, or 84.9 percent, compared with 17 surgery interns, or 82.3 percent (chi-square test, p=0.79); and 105 medicine residents, or 58.1 percent, compared with 30 surgery residents, or 56.7 percent (chi-square test, p=0.89). We also sampled 50 requests each from medicine and surgery to assess the usage of ReNAP for patients in the intensive care units (ICUs) compared with patients on the wards. After adjusting for the higher proportion of ICU patients in the surgery department, we found that surgery house staff were not statistically more likely than medicine house staff to use ReNAP on ICU patients (weighted ICU usage rate, 18.3 percent medicine compared with 23.5 percent surgery; chi-square test, p=0.53).
User Satisfaction
A user satisfaction survey was sent to users of ReNAP. Users were asked to grade the reliability, ease of use, and helpfulness of ReNAP on a scale of 1 (best) to 4 (worst). Users were also asked to suggest changes to the feature and to report problems encountered when using ReNAP.
Altogether, 150 e-mail surveys were distributed to recent and unique users of ReNAP. Findings based on the 47 responses received (31 percent) showed that users were most satisfied with the helpfulness of ReNAP, although ease of use and reliability also received high scores (Table 1▶).
Table 1 .
User Satisfaction Scores
| Response Score |
|||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | Mean Score | |
| Best | Worst | ||||
| Reliability | 27 (57%) | 18 (38%) | 2 (4%) | 0 (0%) | 1.48 |
| Ease of use | 37 (79%) | 9 (19%) | 1 (2%) | 0 (0%) | 1.23 |
| Helpfulness | 42 (89%) | 4 (9%) | 1 (2%) | 0 (0%) | 1.13 |
The comments, in general, were very positive. These comments include “works great,” “has significantly improved the quality of life for interns,” and “an excellent feature that more people should know about.” Other user comments have prompted us to improve the display of messages on the pager screen and to expand our test name dictionary.
Users were also asked on the satisfaction survey to describe some typical scenarios in which they had used this feature. Responses to this question include:
Awaiting cardiac troponin results for patients in the emergency room, before deciding on their disposition
Awaiting final creatine kinase results before sending a patient to the cardiac exercise treadmill test
Forwarding pending laboratory results to cross-covering house staff (who are often busy admitting patients) so that they do not need to look up individual laboratory results
Receiving the latest laboratory results even when away from a computer terminal (e.g., during attending rounds).
Discussion
Benefits
Many clinical decisions are based on laboratory results. For example, decisions about whether chemotherapy should be given, whether anticoagulant dosages should be adjusted, and whether further studies in critically ill patients should be obtained often depend on test results. Applications such as ReNAP can provide clinicians with added value and are likely to reduce delays, which are all too common in medicine and cause substantial patient dissatisfaction. Indeed, a recent Institute of Medicine report14 suggests that reducing delays should be one of the four cornerstones of health care quality improvement.
ReNAP has offered our clinicians new opportunities to reduce unnecessary delays in patient care. Clinicians who use ReNAP to receive laboratory results do so without any undue delays. Although the current study has not demonstrated the direct effects of ReNAP on overall quality of care, its widespread use and positive user feedback are direct evidence of its utility.
ReNAP may have the potential to enhance patient safety. By obviating the need for clinicians to repeatedly look up pending laboratory results, ReNAP may reduce errors of omission.15 For example, a prior study we performed suggested that patients had a five-fold higher risk of an adverse event when being cross-covered.16 The use of ReNAP by house staff to ensure that their busy cross-covering colleagues receive pending laboratory results illustrates how ReNAP might reduce such adverse events.
Clinical medicine is a communication-intensive activity. Parker and Coiera17 have noted that synchronous channels of communication are interruptive and often not effective. They argue that communication in medicine could be made more effective by increased use of asynchronous channels, such as email. Although we agree with their conclusion, we also think that judicious use of interruptive communication (especially when under the clinician's direct control, such as the system we have developed here) can be used effectively to improve care.
Implementation Considerations
The system we have described here was relatively simple to design, since we already had an event monitor in place as part of our critical laboratory result alerting application. The software already examined new laboratory data to determine whether they met critical results rules. It was thus straightforward to have the monitor determine whether a request for notification for this kind of result for this patient had been entered. We also leveraged interfaces from our hospital information system to our paging and e-mail systems.
When clinicians specify tests for result notification, they naturally want to do so in ways that are familiar to them. However, when ReNAP processes new test results from the laboratory, the test identifiers are based on the laboratory system's own test dictionary, which is not easy for clinicians to use. We have addressed this in ReNAP by allowing clinicians to identify the tests for result notification using the order-entry test dictionary, a dictionary with which they are familiar through everyday use of the order-entry system. We can then use mapping that is already in place to translate between the order-entry dictionary and the laboratory system dictionary. The absence of such mapping in radiology and microbiology is one reason that we have not extended this feature to include studies in these domains.
User Education
During the first 24 months of use, users have generally learned about ReNAP by word of mouth, since no formal instruction beyond the first and only mass e-mail sent in March 1999 was provided. In December 1999 and December 2000, there were noticeable drops in ReNAP usage. This fluctuation coincides with the influx of house staff who were previously rotating in hospitals where ReNAP was not available, to cover colleagues on vacation. This underscores the importance of continuing user instruction, especially since new users of BICS arrive periodically. To that end, we have included a short tutorial on ReNAP usage during house staff orientation this year.
Limitation
This study has several limitations. The ReNAP feature has been released in an academic hospital with house staff, and its usage pattern may not be generalizable to other medical settings. Also, the response rate to our user satisfaction survey was relatively low, and findings from the survey may therefore be biased. Finally, we have not directly measured the effects of this feature on clinical outcomes.
Future Work
Several enhancements of ReNAP are planned. We plan to extend its functionality by allowing clinicians to request notification of radiology and microbiology test results. We also plan to incorporate ReNAP into our outpatient test result tracking system so that clinicians can receive and act on specific test results with minimal delay. Finally, we plan to study whether we can reduce the length of stay for patients in our emergency department if all laboratory results are sent to the clinicians taking care of them as soon as the results become available.
Conclusions
We have described a newly developed feature, ReNAP, that was designed to improve communication between our clinical information system and the clinician. It complements other notification systems in that it allows end users to exert maximal control over the results about which they want to be notified.
This feature has been heavily used by clinicians at our hospital and may reduce delays in patient care. Although further evaluation is needed to measure the direct effects of ReNAP on outcome, its popularity suggests that other clinical information systems should consider implementing a similar feature.
Acknowledgments
The authors thank E. John Orav, PhD, for suggestions on statistical calculations, and Sam Wang, MD, PhD, for editorial comments.
Footnotes
Usage by the authors was excluded from all analyses reported in this paper.
References
- 1.Kuperman GJ, Teich JM, Bates DW, et al. Detecting alerts, notifying the physician, and offering action items: a comprehensive alerting system. Proc AMIA Annu Fall Symp. 1996:704–8. [PMC free article] [PubMed]
- 2.Kuperman GJ, Teich JM, Tanasijevic MJ, et al. Improving response to critical laboratory results with automation: results of a randomized controlled trial. J Am Med Inform Assoc. 1999;6(6):512–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rind DM, Safran C, Phillips RS, et al. Effect of computer-based alerts on the treatment and outcomes of hospitalized events. Arch Intern Med. 1994;154:1511–7. [PubMed] [Google Scholar]
- 4.Butte AJ, Weinstein DA, Kohane IS. Enrolling patients into clinical trials faster using RealTime recruiting. Proc AMIA Annu Symp. 2000;111–5. [PMC free article] [PubMed]
- 5.Tate KE, Gardner RM, Weaver LK. A computerized laboratory alerting system. MD Comput. 1990;7(5):296–301. [PubMed] [Google Scholar]
- 6.Jha AK, Kuperman GJ, Teich JM, et al. Identifying adverse drug events: development of a computer-based monitor and comparison with chart review and stimulated voluntary report. J Am Med Inform Assoc. 1998;5(3):305–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Evans RS, Larsen RA, Burke JP, et al. Computer surveillance of hospital-acquired infections and antibiotic use. JAMA. 1986; 256(8):1007–11. [PubMed] [Google Scholar]
- 8.Hripcsak G. Monitoring the monitor: automated statistical tracking of a clinical event monitor. Comput Biomed Res. 1993;26(5):449–66. [DOI] [PubMed] [Google Scholar]
- 9.Shabot MM, LoBue M, Chen J. Wireless clinical alerts for physiologic, laboratory and medication data. Proc AMIA Annu Symp. 2000:789–93. [DOI] [PMC free article] [PubMed]
- 10.Wagner MM, Tsui F-C, Pike J, Pike L. Design of a clinical notification system. Proc AMIA Annu Symp. 1999:989–93. [PMC free article] [PubMed]
- 11.Hogan WR, Wagner, MM. Optimal use of communication channels in clinical event monitoring. Proc AMIA Annu Symp. 1998: 617–21. [PMC free article] [PubMed]
- 12.Wagner MM, Eisenstadt SA, Hogan WR, Pankaskie MC. Preferences of interns and residents for e-mail, paging, or traditional methods for the delivery of different types of clinical information. Proc AMIA Annu Symp. 1998:140–4. [PMC free article] [PubMed]
- 13.Tsui F-C, Wagner MM, Wilbright WA. A feasibility study of two methods for end-user configuration of a clinical event monitor. Proc AMIA Annu Symp. 1999:975–8. [PMC free article] [PubMed]
- 14.Hurtado MP, Swift EK, Corrigan JM (eds). Envisioning the National Health Care Quality Report. Institute of Medicine, Committee on the National Quality Report on Health Care Delivery. Washington, DC: National Academy Press, 2001. [PubMed]
- 15.Bates DW, et al. Reducing the frequency of errors in medicine using information technology. J Am Med Inform Assoc. 2001; 8(4):299–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Petersen LA, Brennan TA, O'Neil AC, Cook EF, Lee TH. Does housestaff discontinuity of care increase the risk of preventable adverse events? Ann Intern Med. 1994;121(11):866–72. [DOI] [PubMed] [Google Scholar]
- 17.Parker J, Coiera E. Improving clinical communication: a view from psychology. J Am Med Inform Assoc. 20007(5):453–61. [DOI] [PMC free article] [PubMed] [Google Scholar]