Abstract
In the present study, we present a 60-year-old woman of American Indian descent with a life-long history of bleeding diathesis. She had a history of recurrent and prolonged bleeding such as mild epistaxis, gingival bleeding and microscopic hematurias. She also experienced a severe bleeding event after surgery. The patient had a large family with a history of a tendency of bleeding, severe in some cases. Hemostatic screening studies revealed no abnormalities, which could explain the bleeding tendency. Clot formation of sodium-citrated blood was analyzed by thromboelastography, which suggested a low platelet count or plasminogen activator inhibitor-1 (PAI-1) deficiency. However, her platelet count was slightly elevated. Subsequent sequencing of the PAI-1 gene revealed a heterozygous Ala15Thr mutation in the signal peptide. This type of deficiency is related to dynamics of PAI-1 secretion rather than its low levels or activity. We concluded that the PAI-1 mutation was likely the etiology of the bleeding diathesis in this patient.
Keywords: plasminogen activator inhibitor, PAI-1 deficiency, heterozygous mutation A15T
Introduction
Hereditary plasminogen activator inhibitor-1 (PAI-1) deficiency is considered an extremely rare disorder characterized by hyperfibrinolysis due to decreased PAI-1 activity that results in frequent bleeding episodes. Five variants of PAI-1 polymorphisms have been identified: two common polymorphisms −765 4G/5G and −844 A>G in the promoter; and three less common, Ala15Thr, Val17Ile at the signal peptide and Asn195Ile (1). To date, only two types of mutations are clearly associated with PAI-1 deficiency. One is the Ala15Thr mutation (2), and the second is the frame-shift mutation in exon 4 of the PAI-1 gene, which results in complete PAI-1 deficiency (3). In this study, we present the case of a woman with PAI-1 functional deficiency having a heterozygous Ala15Thr mutation.
Materials and methods
All blood work was routinely carried out by different hospital laboratories.
Analysis of plasma clot formation with thromboelastography
Thromboelastography (TEG) not only allows for the measurement of the global coagulation profile, but also yields data on the kinetics and dynamics of clot formation and clot lysis in whole blood or in plasma (4,5). The critical part of this instrument is a pin hanging on a torsion wire suspended in a cup holding a sample (360 μl). When plasma changes viscosity during clot formation the pin motion is progressively restrained by the clot and the cup. The strength of the clot determines the degree of force on the pin. Sodium-citrated blood was used for TEG assays by mixing 1 ml of blood with 20 μl of kaolin (Haemoscope Co., Neils, IL) to which a constant amount of tPA was added [10 μl of tPA (2.1 mg/ml in 0.4 M HEPES, 0.1 M NaCl, pH 7.4)] as a fibrinolytic agent (6,7) to measure proteolysis under controlled conditions (5,8,9). Subsequently, 320 μl of the mixture was transferred to each TEG cup containing 20 μl of CaCl2 (0.2 M) and an activity assay buffer (50 mM HEPES, 150 mM NaCl, 1% human serum albumin, 0.05% Tween-20 buffer, pH 6.6) with i) VLHL PAI-1 to prevent lysis by tPA, or ii) VLHL PAI-1 plus the tested compound to check its inhibitory action demonstrated by lysis of the clot when tPA is unopposed by PAI-1 activity.
DNA sequencing
The PAI-1 gene was analyzed by PCR, and sequencing of both DNA strands of the entire coding region and the highly conserved exon-intron splice junction was carried out. Analysis was carried out by Centrogen GmbH, Rostock, Germany.
Results
We report the case of a 60-year-old woman of American Indian descent with a bleeding diathesis. She had a life-long history of recurrent and prolonged bleeding such as mild epistaxis, gingival bleeding and microscopic hematuria. Prior to this study, she experienced severe bleeding after surgery. The patient had a large family with a history of bleeding tendency including menorrhagia in several female family members. She describes one case of severe bleeding lasting for three months while the female patient was in a coma and treated with multiple transfusions. The bleeding tendency was related to her mother's side of the family.
Her symptoms and family history suggested a hereditary bleeding disorder. Therefore, she insisted on multiple blood analyses, which were performed over the years to eliminate common bleeding conditions. Screening studies revealed no abnormalities that could explain the bleeding tendency: hematocrit, 37.8–41.4% (range 34.0–46.0%); hemoglobin levels, 12.9–13.5 gm/dl (range 11.5–15.0 gm/dl); an elevated platelet count in some blood work, 381–470×103/μl (range 150–400×103/μl).
Coagulation tests were conducted as well: prothrombin time, 17 sec (range 16–23 sec); fibrinogen levels, 3.26–3.51 g/l (range 1.70–4.50 g/l); factor VIII coagulant activity, 84–87% (range 50–150%); von Willebrand factor levels, 65–70% (range 46–155%); ristocetin cofactor activity, 81% (range 50–150%); factor IX, 110%, (range 50–150%); factor XI, 163% (range 50–150%); factor XIII, 196% (range 57–192%). Euglobulin clot lysis time test was carried out twice; the first for 45 min and the second for >60 min (normal >60 min). α2-antiplasmin was 120% (range 85–156%) and PAI-1 antigen, 8.9–14.7 ng/ml (range 4.0–43.0 ng/ml). Tests of PAI-1 activity were carried out; these were the most controversial due to the lack of standardized and uniform methods. PAI-1 activity tested by amidolytic assays was determined as <6 IU/ml (range 15.0–40.7 IU/ml). Using ELISA based on binding active PAI-1 to immobilized uPA was determined as 5.2 U/ml [range 1–15 U/ml (10) or 0–36.7 U/ml (11)] clearly being on the lower end of the normal range.
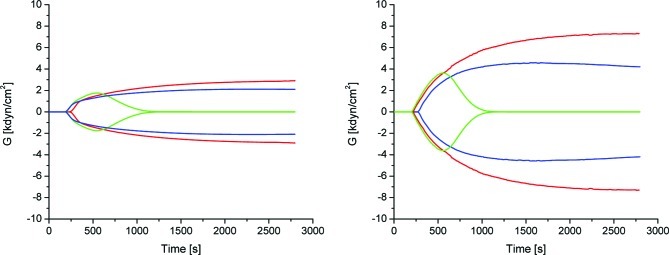
Clot formation of sodium-citrated blood was analyzed by TEG, which allows for the measurement of the overall coagulation profile. TEG also yields data on the kinetics and dynamics of clot formation and clot lysis in whole blood. Most of the parameters were within the normal range with the exception of A (amplitude), which was used to derive the elastic modulus strength: G = [5000A/(100-A)]/1000). As shown in Fig. 1 and Table I, the mean of G of 2.2±0.4 dyn/cm2 was almost 2-fold less than the reported normal range (4.6–10.9 dyn/cm2) (12). A similar pattern was observed for TEG of PAI-1-deficient and normal mouse blood (13).
Figure 1.
Clotting was induced by addition of CaCl2. (A) Thromboelastogram of the patient. Blood: red, control; green, blood treated with tPA; blue, blood treated with tPA and PAI-1. (B) For comparison a thromboelastogram of blood from an individual not affected with the PAI-1 deficiency is shown. Red, control; green, blood treated with tPA; blue, treated with tPA andPAI-1.
Table I.
Thromboelastogram parameters of the blood of the studied patient.
| R (min) | K (min) | An (°) | MA (mm) | MG (dyn/cm2) | LY30 (min) | |
|---|---|---|---|---|---|---|
| Normal | 2–8 | 1–3 | 55–78 | 51–69 | 4.6–10.9 | 0–8 |
| Control | 4.2±0.1 | 3.0±0.2 | 65.6±1.2 | 34.7±1.3 | 2.7±0.2 | 0 |
| tPA | 3.4±0.1 | 2.1±0.4 | 69.0±2.8 | 27.6±2.3 | 1.9±0.2 | 86.4±0.8 |
| tPA+PAI-1 | 3.3±0.1 | 4.2±0.6 | 70.5±5.2 | 29.3±1.6 | 2.1±0.2 | 0 |
The critical parameters of blood clotting measured by TEG are as follows: R is the time from the start of the reaction until a measurable clot is detected, K is the time from the R point until a certain clot firmness is achieved, An is the maximum angle that represents kinetics of clotting, LY 30 represents clot lysis 30 min after MA (maximum amplitude); G (elastic modulus strength) is derived from A (amplitude) by the formula G = [5000A/(100-A)]/1000. It measures actual clot strength in dyn/cm2, presented here as kdyn/cm2; MG is G at maximum amplitude.
Therefore, the PAI-1 gene was sequenced for possible mutations. PAI-1 gene sequencing revealed that the patient had a heterozygous mutation G to A at nucleotide position 4497 in exon 2, resulting in the replacement of alanine 15 (GCC) to threonine (ACC) at the signal peptide.
Discussion
PAI-1 deficiency was first reported in 1989, when undetectable PAI-1 activity and antigen levels were noted in a 76-year-old man with a life-long bleeding tendency (14,15). At that time this condition was considered extremely rare. Since then, more cases have been reported in the literature (2,3,14). PAI-1 deficiency seems to be more common than previously thought, possibly due to misdiagnosis or lack of awareness of this condition by primary physicians.
Initially, PAI-1 deficiency and its related bleeding diathesis was defined as a very low PAI-1 antigen (less than 4 ng/ml) or activity (lower than 1 IU/ml) (3,16). However, hereditary PAI-1 deficiency and severe menorrhagia have been reported in patients with a PAI-1 antigen level of 11.4 ng/ml (4.0–43 ng/ml) and PAI-1 activity less than 5 AU/ml (5–37 AU/ml) (17). The levels of PAI-1 in our reported case were similar, which initially challenged our assumption of PAI-1 deficiency. The TEG analysis revealed weak blood clotting, which indicated a low platelet count contradicting PAI-1 deficiency. However, her platelet count was slightly elevated. For this reason sequencing of the PAI-1 gene was carried out. A mutation found in the signal peptide strongly suggested that this type of deficiency was related to the secretory dynamics of PAI-1 secretion rather than to its low levels or activity as originally suggested by Zhang at el, who described the first case of an Ala15Thr mutation (2).
To conclude, we considered the PAI-1 mutation to be the likely etiology of the bleeding diathesis in this patient.
Acknowledgments
We thank Dr R. Hart (President, PharmaIP LLC, Greenwich, CT, USA) for the helpful remarks, discussions and support. This work was supported, in part, by grants from PharmaIP LLC and the Frank D. Stranahan Endowment Fund for Oncological Research. Special thanks to the patient for her extraordinary involvement and willingness to provide multiple samples of her blood.
References
- 1.Lopes C, Dina C, Durand E, Froguel P. PAI-1 polymorphisms modulate phenotypes associated with the metabolic syndrome in obese and diabetic Caucasian population. Diabetologia. 2003;46:1284–1290. doi: 10.1007/s00125-003-1170-0. [DOI] [PubMed] [Google Scholar]
- 2.Zhang ZY, Wang ZY, Dong NZ, Bai X, Zhang W, Ruan CG. A case of deficiency of plasma plasminogen activator inhibitor-1 related to Ala15Thr mutation in its signal peptide. Blood Coagul Fibrinolysis. 2005;16:79–84. doi: 10.1097/00001721-200501000-00013. [DOI] [PubMed] [Google Scholar]
- 3.Fay WP, Parker AC, Condrey LR, Shapiro AD. Human plasminogen activator inhibitor-1 (PAI-1) deficiency: characterization of a large kindred with a null mutation in the PAI-1 gene. Blood. 1997;90:204–208. [PubMed] [Google Scholar]
- 4.Evans PA, Hawkins K, Lawrence M, Barrow MS, Williams PR, Williams RL. Studies of whole blood coagulation by oscillatory shear, thromboelastography and free oscillation rheometry. Clin Hemorheol Microcirc. 2008;38:267–277. [PubMed] [Google Scholar]
- 5.Gallimore MJ, Harris SL, Tappenden KA, Winter M, Jones DW. Urokinase induced fibrinolysis in thromboelastography: a model for studying fibrinolysis and coagulation in whole blood. J Thromb Haemost. 2005;3:2506–2513. doi: 10.1111/j.1538-7836.2005.01615.x. [DOI] [PubMed] [Google Scholar]
- 6.Carr ME, Jr, Krishnamurti C, Alving BM. Effect of plasminogen activator inhibitor-1 on tissue-type plasminogen activator-induced fibrinolysis. Thromb Haemost. 1992;67:106–110. [PubMed] [Google Scholar]
- 7.Sugiki M, Maruyama M, Yoshida E, Mihara H, Kamiguti AS, Theakston DG. Enhancement of plasma fibrinolysis in vitro by jararhagin, the main haemorrhagic metalloproteinase in Bothrops jararaca venom. Toxicon. 1995;33:1605–1617. doi: 10.1016/0041-0101(95)00102-6. [DOI] [PubMed] [Google Scholar]
- 8.Jankun J, Aleem AM, Selman SH, et al. Highly stable plasminogen activator inhibitor type one (VLHL PAI-1) protects fibrin clots from tissue plasminogen activator-mediated fibrinolysis. Int J Mol Med. 2007;20:683–687. [PubMed] [Google Scholar]
- 9.Kohro S, Yamakage M, Omote T, Namiki A. In vitro effects of propofol on blood coagulability and fibrinolysis by the use of thromboelastograph technique. Acta Anaesthesiol Scand. 1999;43:217–219. doi: 10.1034/j.1399-6576.1999.430217.x. [DOI] [PubMed] [Google Scholar]
- 10.Agren A, Wiman B, Schulman S. Laboratory evidence of hyperfibrinolysis in association with low plasminogen activator inhibitor type 1 activity. Blood Coagul Fibrinolysis. 2007;18:657–660. doi: 10.1097/MBC.0b013e3282dded21. [DOI] [PubMed] [Google Scholar]
- 11.Perkowska A, Elhasade A, Durlik M, et al. The effect of chronic allograft rejection on plasma regulators of fibrinolysis. Ann Transplant. 2002;7:44–51. [PubMed] [Google Scholar]
- 12. TEG 5000 User's Manual Version 4.2 Software. Haemoscope Corporation 2006.
- 13.Jankun J, Aleem AM, Struniawski R, Lysiak-Szydlowska W, Selman SH, Skrzypczak-Jankun E. Accelerated thrombus lysis in the blood of plasminogen activator inhibitor deficient mice is inhibited by PAI-1 with a very long half-life. Pharmacol Rep. 2009;61:673–680. doi: 10.1016/s1734-1140(09)70119-7. [DOI] [PubMed] [Google Scholar]
- 14.Mehta R, Shapiro AD. Plasminogen activator inhibitor type 1 deficiency. Haemophilia. 2008;14:1255–1260. doi: 10.1111/j.1365-2516.2008.01834.x. [DOI] [PubMed] [Google Scholar]
- 15.Schleef RR, Higgins DL, Pillemer E, Levitt LJ. Bleeding diathesis due to decreased functional activity of type 1 plasminogen activator inhibitor. J Clin Invest. 1989;83:1747–1752. doi: 10.1172/JCI114076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jankun J, Skrzypczak-Jankun E. Yin and yang of the plasminogen activator inhibitor. Pol Arch Med Wewn. 2009;119:410–417. [PubMed] [Google Scholar]
- 17.Repine T, Osswald M. Menorrhagia due to a qualitative deficiency of plasminogen activator inhibitor-1: case report and literature review. Clin Appl Thromb Hemost. 2004;10:293–296. doi: 10.1177/107602960401000316. [DOI] [PubMed] [Google Scholar]