Abstract
Febrile seizures (FS) are the most common form of convulsive phenomena in human being and affect 2% to 14% of children. It is the most common type of seizures that every pediatrician is dealing with. It is the most benign type of all seizures occurring in childhood. There are many debates on how to approach to febrile seizures in pediatric neurology and there are many possible malpractices in this field. Some of the most common frequent queries are
How could we differentiate FS from seizures and fever associated with serious infections involving the central nervous system?
When should we refer the affected child for further investigations such as lumbar puncture, EEG, neuroimaging, and routine biochemical studies?
How should we treat FS in its acute phase?
How could we assess the risk for further recurrences as well as other risks threatening the child's health in future?
How could we select the patients for treatment or prophylaxis?
Which medication(s) should be selected for treatment or prophylaxis?
Trying to answer the above-mentioned questions, this review article will present a four steps algorithmic clinical approach model to a child with febrile seizures based on the current medical literature.
Keywords: Febrile seizures, Febrile convulsions, Clinical Protocol, Algorithms
Introduction
Febrile seizure (FS) is a convulsive event, exclusively occurring in childhood. The International League Against Epilepsy (ILAE) defined FS as "a seizure in association with a febrile illness in the absence of a central nervous system (CNS) infection or acute electrolyte imbalance in children older than 1 month of age without prior afebrile seizures”[1]. The peak incidence is between 18 to 22 months of age. It is the most common form of seizures occurring in human being. It affects 2–4% (US and Europe) to 14% (Guam islands) of general pediatric populationp[2–8]. In which degree of body temperature does a febrile seizure occur? There is no cut-off point regarding this question. In fact, sometimes seizures occur before the fever. But, generally speaking when the body temperature rises over 38 °C rectally, it is considered as fever[9]. Febrile seizures are simple when they are not complex (i.e. multiple, occurring more than once during the febrile illness, prolonged, lasting more than 15 minutes, and focal)[8]. The child's prior neurologic state is not considered as a criterion for classification[1, 11].
Some interesting and yet up to date clinical findings are described by Hippocrates (460–370 BC) when he wrote:[12]
“Children are likely to have convulsions if the fever is high”.
“These may be generalized or partial”.
“This most commonly happens under the age of seven; as they grow up they are no longer likely to be attacked by convulsions in the course of a fever”. (It is interesting point because we do see children with FS older than 5 years in our practice.)
“Particularly likely to occur during the eruption of canines” (perhaps a reference to pain-induced attacks).
“Age of greatest vulnerability between 16 and 20 months”. (On that time there was no registry or epidemiologic data rather than writer's personal experience!)
“A positive family history is important”.
“The brain is the seat of this disease” (insight lost until the late 19th century).
“Those suffering from brain fever (meningitis) have convulsions and some of these die rapidly”.
“Many come through safely but with minor damage” (how interesting).
“Particularly occurs with the warm southerly winds” (a possible reference to malaria in Greece at the time).
Some authors emphasize on the temporal semiology of the febrile seizures and suggest that seizure semiology in febrile seizures deserves closer scrutiny[12].
How to differentiate FS from CNS infections?
This is one of the major concerns of pediatricians who are confronting a child with febrile seizures. Incidence of meningitis in children with FS is about 2% to 5%[6]. Lumbar puncture (LP) is an easy and convenient way to detect NS infection; however it is an invasive method with some serious complications[13, 14]. American Academy of Pediatrics (AAP) suggests LP for infants of less than 12 months and strongly recommends for infants between 12 to 18 months of age, because of the vague symptomatology of meningoencephalitis in this age group[6, 14, 15, 16].
| Key Points |
|---|
| Febrile seizures (FS) are the most common form of childhood seizures. |
| Every pediatrician usually visits these children at routine intervals. |
| There are two major type of FS (i.e. simple and complex) |
| Complex FS is a type of seizure which has one or any combination of the focality, multiplicity, and prolongation. |
Bacterial meningitis presenting as seizure with fever is more commonly seen in children with; a visit for medical care within the previous 48 hours, seizures on arrival to the emergency room, focal seizure, first complex febrile seizure, febrile status, or suspicious findings on physical or neurological examination (eg neck stiffness, petechiae or purpura, prolonged lethargy after the seizure, Kernig and Brudzinsky signs)[17, 18].
So it's quite rational to consider LP for these children. Although, these are practical guidelines for doing LP in a child with FS, we should seek for better indicators of CNS infection, especially in younger children and infants with FS.
| Indications for LP in Children with FS |
|---|
| A visit for medical care within previous 48 hours |
| Seizures on arrival to the emergency room |
| Focal seizure |
| Febrile status |
| Suspicious findings on physical and neurologic examination |
| First complex febrile seizure |
| Prolonged lethargy, or any altered level of consciousness after the seizure |
LP: Lumber puncture/ FS: Febrile Seizure
According to the recommendations of AAP, we should perform LP in a population in which there is only a 3–5% chance of pleocytosis (meningitis)[19, 20].
What other investigations are needed?
No routine laboratory examination [i.e. complete blood count (CBC), blood glucose or electrolytes including serum calcium level] is needed in a child with simple febrile seizure (SFS)[6, 21–24]. If the child has additional signs or symptoms such as vomiting or diarrhea, the relevant exams will be requested. Skull X-ray, brain CT scan, and MRI are not indicated in the simple febrile seizurep[6].
There is some recent information of transient temporal lobe changes such as transient hippocampal edema in brain magnetic resonance imaging (MRI)[12].
But these changes do not have any predictive value. It is also unclear that brain MRI is indicated in the prolonged and/or focal seizures[25, 26, 27]. Electroencephalography (EEG) has a limited value in the work-up of FS. Even if it is abnormal, it is not highly predictive and in fact in the children with complex febrile seizures, EEG may be abnormal in many cases[28, 29]. Even newer neurophysiologic techniques such as magnetoencephalography (MEG) reveals a substantial variety of abnormalities in children with febrile seizures, but like EEG it has a limited predictive value for further recurrences or even epilepsy[30]. Some trace elements (e.g. zinc) maybe decreased in the serum of children with febrile seizures, but there is not enough evidence in the literature to apply this finding to diagnostic as well as therapeutic guidelines in children with FS[31].
| Investigations which are not routinely indicated in SFS |
|---|
| Routine blood count or biochemical lab exams |
| Skull X-rays, brain CT scan and MRI |
| EEG or MEG |
SFS: simple febrile seizure/ MRI: magnetic resonance imaging/ EEG: Electroencephalography/ MEG: magnetoencephalography
How should we treat FS in its acute phase?
Febrile seizures are usually benign and self-limiting attacks (often lasting less than 10 minutes) and protective measures are merely required. Appropriate posturing (lateral recumbent, with head extension), and keeping airways open are the recommended maneuvers for the affected children. Rectal diazepam is a good and reliable way to control seizures outsides of the hospital and even at home[32, 33, 34], but it should be used with great caution and in the hands of well-trained caregivers and/or parents. Parents of children with the history of prolonged and/or multiple FS, and those who are living far from medical care, should be educated and trained to use rectal diazepam. For many parents, the availability of rectal diazepam will relieve their anxiety even though they may never use that[35, 36, 37].
When a child comes to emergency room with seizure, an IV route should be obtained and intravenous diazepam should be administered.
When intravenous access is difficult, rectal diazepam would be an effective alternative choice[32, 34]. If the seizures continue after a sufficient dose of intravenous diazepam, a full status epilepticus treatment protocol should be initiatedp[38, 39].
| Treatment of febrile seizures in its acute phase |
|---|
| Airways open and appropriate positioning |
| Rectal and/or intravenous diazepam |
| If seizures continue, try full status epilepticus treatment protocol |
Four step's model of approach to the children with history of febrile seizure
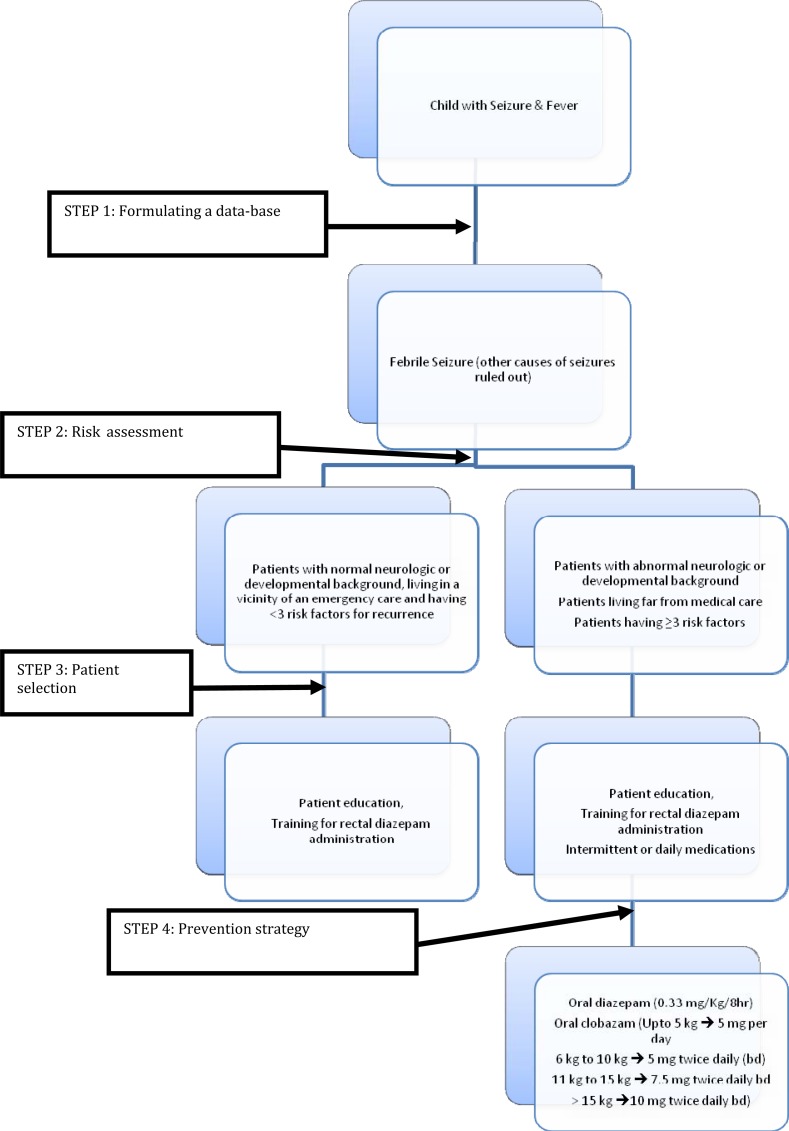
For practical purposes, I have proposed a four steps clinical approach to children with febrile seizures. These steps are; data gathering (i.e. formulating a database), risk assessment, patient selection, selection of treatment strategy.
Step 1: Formulating a database
In this step, physician gathers the clinical as well as the paraclinical relevant information to formulate a robust database.
| 4 Steps Approach in Febrile Seizure |
|---|
|
Following information are mandatory:
Age of the patient
History of febrile seizure in the 1st as well as 2nd degree family
History of any developmental delay History of nursery admission for more than 30 days
Day care attendance
Duration between the beginning of fever and the occurrence of seizure
Complexity (i.e. focal, multiple, and prolonged FS)
Duration of postictal phase
Presence of any neurologic or developmental deficits
Presence of papilledema
Nonspecific and vague symptomatology in infants less than 18 months old (eg agitation, bulging fontanel, excessive cry)
Neck stiffness, Kernig and/or Brudzinsky signs
Petechiae and/or purpura
Step 2: Risk Assessment
Risk assessment is according to the patient's database. What are the risk factors for the first FS, recurrence(s), and epilepsy in children with FS? And how important are these risk factors in our decision-making?
Risk factors in the first febrile seizure: In two independent studies[40, 41], the risk factors associated with the 1st FS are; history of FS in the 1st or 2nd degree family members, nursery stay of more than 30 days, developmental delay, attendance at day-care, high peak temperature. In the second study, there was an inverse association between gastroenteritis, as an underlying disorder, and first attack of febrile seizure. There was a 28% chance of at least one febrile seizure for children with two or more of the above mentioned risk factors[40].
Risk factors in recurrences of febrile seizures: The chance of recurrence of febrile seizures is about one in three regardless of any risk factors[42–45]. The most common consistent risk factors are a family history of FS and age of onset of less than 18 months[42–45]. Two other definite risk factors are peak temperature[43, 44, 46] and duration of the fever before the seizure[2, 47].
The higher the peak temperature, the higher chance for recurrence. It is very important to mention that the peak temperature is not the temperature at the time of seizure or arrival at the emergency department, but it is the peak temperature during the whole febrile illness period. The other related risk factor is the duration of febrile illness before the seizure. The shorter the duration, the higher is the risk of recurrence of further seizures. Children with multiple risk factors have the highest chance for recurrence[43, 47]. A child with two or more risk factors has a greater than 30% chance for recurrence at two years; a child with three or more risk factors has a greater than 60% chance for recurrence[47]. In children with no risk factor, there is a recurrence risk of less than 15% at two years. A recurrent febrile seizure also tends to be prolonged if the first attack was prolonged[10, 44].
Presence of family history of afebrile seizures (epilepsy) is a doubtful risk factor for recurrence of further febrile seizures[43, 44, 48, 49], so I am not going to discuss on or consider it here.
Neurodevelopmental delay, complex FS, sex, and ethnicity are not considered as a risk factor for recurrence of FS[4, 10, 43, 44, 48, 49].
Risk factors for subsequent epilepsy: About 2%–10% of patients with FS will later develop epilepsy[2, 4, 5, 50, 51]. The occurrence of family history of non-febrile seizures as well as the occurrence of complex FS will raise the risk of subsequent epilepsy[2, 4, 5, 50, 51]. In two studies, there was a slightly increased risk in children with multiple FS[2, 51]. One study found an inverse association between the duration of fever before the seizure and occurrence of further epilepsy[51]. That means the shorter the duration between the onset of fever and seizure, the higher the chance of developing further epilepsy. Two studies revealed that the children with very prolonged febrile seizures (ie febrile status) are more prone to develop further epilepsy[2, 51]. The only common risk factor for both recurrence of FS and epilepsy is the duration of fever before the onset of febrile seizure[48, 49, 51].
| 2nd Step; Risk Assessment for FS Recurrences |
|---|
|
|
|
No risk factor; <15% chance of recurrence at two years
2 or more risk factors; >30% chance of recurrence at two years
3 or more risk factors; >60% chance of recurrence at two years
Febrile seizure could be the initial presentation of some malignant childhood epileptic syndromes such as Dravet syndrome or severe myoclonic epilepsy of infancy[52].
Mortality and morbidity: No mortality has been reported with FS according to several studies[3, 4, 53, 54, 55]. Even in a very prolonged FS (febrile status), there is little chance for death[38, 56–61]. There is also no report indicating morbidity such as motor deficit and/or cognitive impairment[3, 4, 53–60]. Even prolonged febrile seizures are not associated with cognitive deficits[55, 59, 62].
Step 3: Patient Selection (who should be treated?)
The 3rd step is patient selection for prophylaxis or treatment. In other words, who should be treated after the risk assessment? As previously mentioned, there is no reported mortality or morbidity after FS. The risk of further occurrence of non-febrile seizures is considerable but there is no way to prevent epilepsy in a child with FS[48, 63–66]. The relationship between FS and temporal lobe sclerosis is yet controversial[25, 67]. Only there are some concerns about prolonged or atypical febrile seizures especially those with a pre-existing temporal or hippocampal pathology [12, 68–74]. Maybe the only strong rational for prophylaxis in children with FS, is preventing the parental awful experience of "feeling dead" when they witness their own child's convulsion[75].
| Who should be treated? |
|---|
| When the patient is pretty far from medical facilities. |
| When the patient has preexisting neurological deficit with prominent temporal semiology. |
| When the patient has three or more risk factors for recurrence of FS (a 60% chance for further recurrences). |
So we prefer to prevent further recurrences of FS in the following cases:
When the patient is pretty far from medical facilities.
When the patient has preexisting neurological deficit with prominent temporal semiology.
When the patient has three or more risk factors for recurrence of FS (a 60% chance for further recurrences).
Step 4: Drug Selection (Treatment Policy)
The best treatment policy is patient (parental) education about the benign nature of FS and the risks and benefits of any medication[76]. Parent's education, regarding how to deal with the convulsing child as well as some simple and clear explanations about febrile seizures and their benign nature and outcome are all that is necessary[75]. Teaching parents how to use rectal diazepam in an emergency condition at home is quite beneficial[32]. So they can administer it whenever their child seizes. Maybe this is the most reliable and convenient type of treatment. There are some evidences that intranasal or intrabuccal administration of midazolam is also effective in cessation of febrile seizures[77, 78].
For long-term treatment, there are mainly two types; intermittent medication at the time of fever, and daily (continuous) medications.
There is not enough evidence that antipyretics would reduce the risk of seizures in a febrile illness[79, 80]. But it is quite rational to use antipyretics in a febrile illness episode because of parental feelings of anxiety and guilt. There are strong evidences that intermittent use of oral or rectal diazepam is effective in preventing the seizures in a febrile episode[42, 81–85]. It is recommended to use oral diazepam in a dose of 0.33 mg/kg/dose every 8 hours from the onset of a febrile illness. But potential side effects of diazepam in such a high dose (i.e. sedation and ataxia) should be considered. There are some studies indicating that intermittent clobozam could be as effective as diazepam in preventing the seizures in a febrile illness, but ataxia is less prominent than with diazepam[86, 87, 88].
Fig. 1.
Four step's model of approach to the children with history of febrile seizure
Intermittent administration of phenobarbital is ineffective in preventing the febrile seizures[89, 90]. Phenobarbital has been used as a daily basis for prevention of further recurrences of FS. Its effectiveness has been proved by some studies in this regard[80, 83, 84, 91–94]. In therapeutic doses, phenobarbital may induce hyperactivity and behavioral disorders[95, 96]. Even in some studies its effectiveness in preventing the further febrile seizures is doubtful[95, 96, 97]. So the use of Phenobarbital is not recommended as a means for prevention of further febrile seizures.
Sodium valproate is also effective in preventing further febrile seizures[84, 93, 94, 98]. However, its use is not indicated because the children who are at highest risk for recurrences are also most vulnerable to idiosyncratic hepatic toxicity as the drug's side-effect[99, 100].
There are some reports indicating that topiramate could protect the blood brain barrier in the experimental model of febrile seizures and may have some protective effect in children with febrile seizures[101, 102, 103]. But there is not enough evidence to use this drug in the practice. There is also no report on newer anticonvulsive agents and their effectiveness as prophylactic measures in febrile seizures.
Conclusions and algorithmic four steps approach to children with FS
Febrile seizures are the most common as well as most benign type of seizures seen in infants and children. Every pediatrician should be familiar with it and adopt a uniform and regular approach to this common phenomenon.
According to the current medical literature the most important role of physicians in this regard is acting as a knowledgeable, trustworthy, sympathetic educator. They should help the parents to know more about the condition and act properly in a convulsive state.
Rectal diazepam is a good treatment modality in acute phase of seizure and parents should be trained to administer it in an emergency condition. Prophylaxis of further attacks by other drugs is not justified in every case. Based on current medical literature, an algorithmic model is proposed, introducing a four steps approach.
CME QUESTIONS
1- What are the main types of febrile seizures?
Simple and atypical
Simple and complex
Complex and atypical
Simple and non‐typical
2- According to the paper which one of the followings is an indication for lumbar puncture in a child with seizure and fever?
Focal seizures
2nd complex febrile seizure
Lethargy after the seizure
Post-ictal sleep
3- You are visiting a 22 months old boy with seizure and fever. He has had diarrhea and fever from yesterday. The seizure was a generalized tonic clonic one lasting for about 5 minutes, without any post-ictal signs. Neurologically he is quietly normal. Which one of the following investigations is indicated?
EEG
Skull x ray
Brain MRI
Serum electrolytes
4- A child who had a simple febrile seizure with a positive family history of febrile seizure (the father). He is 2 years old and the peak temperature was 40 o C. Please assess the risk for further recurrences for febrile seizure(s)?
15%
30%
45%
60%
5- Who should be treated for further recurrences of febrile seizures?
One who had more than one febrile seizure.
One who had multiple FSs in a day.
One who lives far from medical care.
One who is developmentally normal.
Conflict of Interest
None
References
- 1.Commission on Epidemiology and Prognosis. International League Against Epilepsy. Guidelines for epidemiologic studies on epilepsy. Epilepsia. 1993;34(4):592–6. doi: 10.1111/j.1528-1157.1993.tb00433.x. [DOI] [PubMed] [Google Scholar]
- 2.Annegers JF, Hauser WA, Elveback LR, et al. The risk of epilepsy following febrile convulsions. Neurology. 1979;29(3):297–303. doi: 10.1212/wnl.29.3.297. [DOI] [PubMed] [Google Scholar]
- 3.Verity CM, Butler NR, Golding J. Febrile convulsions in a national cohort followed up from birth. I. Prevalence and recurrence in the first 5 years of life. Br Med J. 1985;290(6478):1307–15. doi: 10.1136/bmj.290.6478.1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nelson KB, Ellenberg JH. Prognosis in children with febrile seizures. Pediatrics. 1978;61(5):720–7. [PubMed] [Google Scholar]
- 5.Van der Berg BJ, Yerushalmi J. Studies on convulsive disorders in young children, I. Incidence of febrile and nonfebrile convulsions by age and other factors. Pediatr Res. 1969;3(4):298–304. doi: 10.1203/00006450-196907000-00005. [DOI] [PubMed] [Google Scholar]
- 6.American Academy of Pediatrics: Provisional Committee on Quality Improvement. Practice parameter: the neurodiagnostic evaluation of the child with a simple febrile seizure. Pediatrics. 1996;97(5):769–75. [PubMed] [Google Scholar]
- 7.Berg AT. The epidemiology of seizures and epilepsy in children. In: Shinnar S, Amir N, Branski D, editors. Childhood Seizures. Basel, Switzerland: S Karger; 1995. pp. 1–10. [Google Scholar]
- 8.Stanhope JM, Brody JA, Brink E, Morris CE. Convulsions among the Chamorro people of Guam, Mariana Islands. II. Febrile convulsions. Am J Epidemiol. 1972;95(3):299–304. doi: 10.1093/oxfordjournals.aje.a121397. [DOI] [PubMed] [Google Scholar]
- 9.Medline Plus Medical Encyclopedia. U.S. National Library of Medicine. http://www.nlm.nih.gov/medlineplus/ency/article/003090.htm. Access date: May 20, 2009.
- 10.Berg AT, Shinnar S. Complex febrile seizures. Epilepsia. 1996;37(2):126–33. doi: 10.1111/j.1528-1157.1996.tb00003.x. [DOI] [PubMed] [Google Scholar]
- 11.National Institutes of Health. Bethesda, MD: National Institute of Health; 1980. Febrile seizures: consensus development conference summary. No. 2. [Google Scholar]
- 12.Neville GBR, Gindner D. Febrile seizures – Semiology in humans and animal models: Evidence of focality and heterogeneity. Brain Dev. 2010;32(1):33–6. doi: 10.1016/j.braindev.2009.09.013. [DOI] [PubMed] [Google Scholar]
- 13.Roos KL. Lumbar puncture. Semin Neurol. 2003;23(1):105–14. doi: 10.1055/s-2003-40758. [DOI] [PubMed] [Google Scholar]
- 14.Straus SE, Thorpe KE, Holroyd-Leduc J. How do I perform a lumbar puncture and analyze the results to diagnose bacterial meningitis? JAMA. 2006;296(16):2012–22. doi: 10.1001/jama.296.16.2012. [DOI] [PubMed] [Google Scholar]
- 15.Lorber J, Sunderland R. Lumbar puncture in children with convulsions associated with fever. Lancet. 1980;1(8172):785–6. doi: 10.1016/s0140-6736(80)91290-8. [DOI] [PubMed] [Google Scholar]
- 16.Wears RL, Luten RC, Lyons RG. Which laboratory tests should be performed on children with apparent febrile convulsions? An analysis and review of the literature. Pediatric Emer Care. 1986;2(3):191–6. doi: 10.1097/00006565-198609000-00011. [DOI] [PubMed] [Google Scholar]
- 17.Joffe A, McMcormick M, DeAngelis C. Which children with febrile seizures need lumbar puncture? A decision analysis approach. Am J Dis Child. 1983;137(12):1153–6. doi: 10.1001/archpedi.1983.02140380013005. [DOI] [PubMed] [Google Scholar]
- 18.Riviello JJ, Jr, Ashwal S, Hirtz D, et al. American Academy of Neurology Subcommittee, Practice Committee of the Child Neurology Society. Practice parameter: diagnostic assessment of the child with status epilepticus (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Neurology. 2006;67(9):1542–50. doi: 10.1212/01.wnl.0000243197.05519.3d. [DOI] [PubMed] [Google Scholar]
- 19.Kimia AA, Capraro AJ, Hummel D, et al. Utility of lumbar puncture for first simple febrile seizure among children 6 to 18 months of age. Pediatrics. 2009;123(1):6. doi: 10.1542/peds.2007-3424. [DOI] [PubMed] [Google Scholar]
- 20.Mohammadi M, Ravaghi H. How frequent is the cerebrospinal fluid pleocytosis in infants with febrile seizures? Acta Medica Iranica. 2004;42(1):65–8. [Google Scholar]
- 21.Gerber MA, Berliner BC. The child with a “simple” febrile seizure: appropriate diagnostic evaluation. Am J Dis Child. 1981;135(5):431–3. doi: 10.1001/archpedi.1981.02130290029011. [DOI] [PubMed] [Google Scholar]
- 22.Heijbel J, Blom S, Bergfors PG. Simple febrile convulsions: a prospective incidence study and an evaluation of investigations initially needed. Neuropediatrie. 1980;11(1):5–56. doi: 10.1055/s-2008-1071374. [DOI] [PubMed] [Google Scholar]
- 23.Jaffe M, Bar-Joseph G, Tirosh E. Fever and convulsions-indications for laboratory investigations. Pediatrics. 1981;57(5):729–31. [PubMed] [Google Scholar]
- 24.Rutter N, Smales OR. Role of routine investigations in children presenting with their first febrile convulsion. Arch Dis Child. 1977;52(3):188–91. doi: 10.1136/adc.52.3.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shinnar S. Prolonged febrile seizures and mesial temporal sclerosis. Ann Neurol. 1998;43(4):411–2. doi: 10.1002/ana.410430402. [DOI] [PubMed] [Google Scholar]
- 26.VanLandingham KE, Heinz ER, Cavazos JE, et al. Magnetic resonance imaging evidence of hippocampal injury following prolonged, focal febrile convulsions. Ann Neurol. 1998;43(5):413–26. doi: 10.1002/ana.410430403. [DOI] [PubMed] [Google Scholar]
- 27.Cuestas E. Is routine EEG helpful in the management of complex febrile seizures? Arch Dis Child. 2004;89(3):290. doi: 10.1136/adc.2003.048447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Joshi C, Wawrykow TB, Patrick JC, et al. Do clinical variables predict an abnormal EEG in patients with complex febrile seizures? Seizure. 2005;14(6):429–34. doi: 10.1016/j.seizure.2005.07.006. [DOI] [PubMed] [Google Scholar]
- 29.Stores G. When does an EEG contribute to the management of febrile seizures? Arch Dis Child. 1991;66(4):554–7. doi: 10.1136/adc.66.4.554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Anninos P, Kotini A, Tsalkidis A, et al. Magnetoencephalography evaluation of febrile seizures in young children. J Child Neurol. 2010;25(1):61–6. doi: 10.1177/0883073809336123. [DOI] [PubMed] [Google Scholar]
- 31.Ganesh R, Janakiraman L. Serum zinc levels in children with simple febrile seizure. Clinical Pediatrics. 2008;47(2):164–6. doi: 10.1177/0009922807306165. [DOI] [PubMed] [Google Scholar]
- 32.Camfield CS, Camfield PR, Smith E, et al. Home use of rectal diazepam to prevent status epilepticus in children with convulsive disorders. J Child Neurol. 1989;4(2):125–6. doi: 10.1177/088307388900400210. [DOI] [PubMed] [Google Scholar]
- 33.Knudsen FU. Rectal administration of diazepam in solution in the acute treatment of convulsions in infants and children. Arch Dis Child. 1979;54(11):855–7. doi: 10.1136/adc.54.11.855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Morton LD, Rizkallah E, Pellock JM. New drug therapy for acute seizure management. Semin Pediatr Neurol. 1997;4(1):51–63. doi: 10.1016/s1071-9091(97)80009-5. [DOI] [PubMed] [Google Scholar]
- 35.Knudsen FU. Practical management approaches to simple and complex febrile seizures. In: Baram TZ, Shinnar S, editors. Febrile Seizures. San Diego, CA: Academic Press; 2002. pp. 274–304. [Google Scholar]
- 36.O'Dell C. What do we tell the parent of a child with simple or complex febrile seizures? In: Baram TZ, Shinnar S, editors. Febrile Seizures. San Diego, CA: Academic Press; 2002. pp. 305–16. [Google Scholar]
- 37.O'Dell C, Shinnar S, Ballaban.Gil K, et al. Home use of rectal diazepam gel (Diastat) Epilepsia. 2000;41(suppl 7):246. [Google Scholar]
- 38.Dodson WE, DeLorenzo RJ, Pedley TA, et al. The treatment of convulsive status epilepticus: recommendations of the Epilepsy Foundation of America's working group on status epilepticus. JAMA. 1993;270(7):854–9. [PubMed] [Google Scholar]
- 39.Maytal J, Shinnar S. Status epilepticus in children. In: Shinnar S, Amir N, Branski D, editors. Childhood Seizures. Basel, Switzerland: S Karger; 1995. pp. 111–22. [Google Scholar]
- 40.Bethune P, Gordon K, Dooley J, et al. Which child will have a febrile seizure? Am J Dis Child. 1993;147(1):35–9. doi: 10.1001/archpedi.1993.02160250037013. [DOI] [PubMed] [Google Scholar]
- 41.Berg AT, Shinnar S, Shapiro ED, et al. Risk factors for a first febrile seizure: a matched case-control study. Epilepsia. 1995;36(4):334–41. doi: 10.1111/j.1528-1157.1995.tb01006.x. [DOI] [PubMed] [Google Scholar]
- 42.Knudsen FU. Recurrence risk after first febrile seizure and effect of short. term diazepam prophylaxis. Arch Dis Child. 1985;60(11):1045–9. doi: 10.1136/adc.60.11.1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Offringa M, Bossuyt PMM, Lubsen J, et al. Risk factors for seizure recurrence in children with febrile seizures: a pooled analysis of individual patient data from five studies. J Pediatr. 1994;124(4):574–84. doi: 10.1016/s0022-3476(05)83136-1. [DOI] [PubMed] [Google Scholar]
- 44.Offringa M, Derksen-Lubsen G, Bossuyt PM, et al. Seizure recurrence after a first febrile seizure: a multivariate approach. Dev Med Child Neurol. 1992;34(1):15–24. doi: 10.1111/j.1469-8749.1992.tb08559.x. [DOI] [PubMed] [Google Scholar]
- 45.Van den Berg BJ. Studies on convulsive disorders in young children. 3. Recurrence of febrile convulsions. Epilepsia. 1974;15(2):177–90. doi: 10.1111/j.1528-1157.1974.tb04940.x. [DOI] [PubMed] [Google Scholar]
- 46.El-Rahdi AS, Banajeh S. Effect of fever on recurrence rate of febrile convulsions. Arch Dis Child. 1989;64(6):869–70. doi: 10.1136/adc.64.6.869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Annegers JF, Blakley SA, Hauser WA, et al. Recurrence of febrile convulsions in a population-based cohort. Epilepsy Res. 1990;5(3):209–16. doi: 10.1016/0920-1211(90)90040-3. [DOI] [PubMed] [Google Scholar]
- 48.Berg AT, Shinnar S, Darefsky AS, et al. Predictors of recurrent febrile seizures. Arch Ped Adolesc Med. 1997;151(4):371–8. doi: 10.1001/archpedi.1997.02170410045006. [DOI] [PubMed] [Google Scholar]
- 49.Berg AT, Shinnar S, Hauser WA, et al. Predictors of recurrent febrile seizures: a prospective study of the circumstances surrounding the initial febrile seizure. N Engl J Med. 1992;327:1122–7. doi: 10.1056/NEJM199210153271603. [DOI] [PubMed] [Google Scholar]
- 50.Verity CM, Golding J. Risk of epilepsy after febrile convulsions: a national cohort study. Br Med J. 1991;303(6814):1373–6. doi: 10.1136/bmj.303.6814.1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Berg AT, Shinnar S. Unprovoked seizures in children with febrile seizures: short term outcome. Neurology. 1996;47(2):562–8. doi: 10.1212/wnl.47.2.562. [DOI] [PubMed] [Google Scholar]
- 52.Dravet C, Bureau M, Guerrini R, Roger J. Severe myoclonic epilepsy in infants. In: Bureau M, Dravet C, editors. Epileptic Syndromes in Infancy, Childhood and Adolescence. 2nd ed. London; John Libbey; 1992. pp. 75–88. [Google Scholar]
- 53.Nelson KB, Ellenberg JH. Predictors of epilepsy in children who have experienced febrile seizures. N Engl J Med. 1976;295(19):1029–33. doi: 10.1056/NEJM197611042951901. [DOI] [PubMed] [Google Scholar]
- 54.Verity CM, Butler NR, Golding J. Febrile convulsions in a national cohort followed up from birth. II. Medical history and intellectual ability at 5 years of age. Br Med J. 1985;290(6478):1311–5. doi: 10.1136/bmj.290.6478.1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Verity CM, Ross EM, Golding J. Outcome of childhood status epilepticus and lengthy febrile convulsions: findings of national cohort study. Br Med J. 1993;307(6898):225–8. doi: 10.1136/bmj.307.6898.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.DeLorenzo RJ, Hauser WA, Towne AR, et al. A prospective population- based epidemiological study of status epilepticus in Richmond, Virginia. Neurology. 1996;46(4):1029–35. doi: 10.1212/wnl.46.4.1029. [DOI] [PubMed] [Google Scholar]
- 57.Dunn WD. Status epilepticus in children: etiology, clinical features and outcome. J Child Neurol. 1988;3(3):167–73. doi: 10.1177/088307388800300303. [DOI] [PubMed] [Google Scholar]
- 58.Maytal J, Shinnar S, Moshe SL, Alvarez LA. Low morbidity and mortality of status epilepticus in children. Pediatrics. 1989;83(3):323–31. [PubMed] [Google Scholar]
- 59.Shinnar S, Pellock JM, Berg AT, et al. Short-term outcomes of children with febrile status epilepticus. Epilepsia. 2001;42(1):47–53. doi: 10.1046/j.1528-1157.2001.10000.x. [DOI] [PubMed] [Google Scholar]
- 60.Towne AR, Pellock JM, Ko D, et al. Determinants of mortality in status epilepticus. Epilepsia. 1994;35(1):27–34. doi: 10.1111/j.1528-1157.1994.tb02908.x. [DOI] [PubMed] [Google Scholar]
- 61.Maytal J, Shinnar S. Febrile status epilepticus. Pediatrics. 1990;86(4):611–6. [PubMed] [Google Scholar]
- 62.Ellenberg JH, Nelson KB. Febrile seizures and later intellectual performance. Arch Neurol. 1978;35(1):17–21. doi: 10.1001/archneur.1978.00500250021004. [DOI] [PubMed] [Google Scholar]
- 63.Knudsen FU, Paerregaard A, Andersen R, et al. Long term outcome of prophylaxis for febrile convulsions. Arch Dis Child. 1996;74(1):13–8. doi: 10.1136/adc.74.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wolf SM, Forsythe A. Epilepsy and mental retardation following febrile seizures in childhood. Acta Paediatr Scand. 1989;78(2):291–5. doi: 10.1111/j.1651-2227.1989.tb11072.x. [DOI] [PubMed] [Google Scholar]
- 65.Rosman NP, Labazzo JL, Colton T. Factors predisposing to afebrile seizures after febrile convulsions and preventive treatment. Ann Neurol. 1993;34:452. [Google Scholar]
- 66.Shinnar S, Berg AT. Does antiepileptic drug therapy prevent the development of chronic” epilepsy? Epilepsia. 1996;37(8):701–8. doi: 10.1111/j.1528-1157.1996.tb00639.x. [DOI] [PubMed] [Google Scholar]
- 67.Shinnar S, Babb TL. Long term sequelae of status epilepticus. In: Engel J Jr, Pedley TA, editors. Epilepsy: A Comprehensive Text. Lippincot-Raven: Philadelphia; 1997. pp. 755–63. [Google Scholar]
- 68.Abou-Khalil B, Andermann E, Andermann F, et al. Temporal lobe epilepsy after prolonged febrile convulsions: excellent outcome after surgical treatment. Epilepsia. 1993;34(5):878–83. doi: 10.1111/j.1528-1157.1993.tb02105.x. [DOI] [PubMed] [Google Scholar]
- 69.Bruton CJ. The neuropathology of temporal lobe epilepsy. New York: Oxford University Press; 1988. [Google Scholar]
- 70.Cendes F, Andermann F, Dubeau F, et al. Early childhood prolonged febrile convulsions, atrophy and sclerosis of mesial structures, and temporal lobe epilepsy: an MRI volumetric study. Neurology. 1993;4396:1083–7. doi: 10.1212/wnl.43.6.1083. [DOI] [PubMed] [Google Scholar]
- 71.Cendes F, Andermann F, Gloor P, et al. Atrophy of mesial structures in patients with temporal lobe epilepsy: cases or consequence of repeated seizures. Ann Neurol. 1993;34(6):795–801. doi: 10.1002/ana.410340607. [DOI] [PubMed] [Google Scholar]
- 72.French JA, Williamson PD, Thadani VM, et al. Characteristics of medial temporal lobe epilepsy: I. Results of history and physical examination. Ann Neurol. 1993;34(6):774–80. doi: 10.1002/ana.410340604. [DOI] [PubMed] [Google Scholar]
- 73.Sagar HJ, Oxbury JM. Hippocampal neuron loss in temporal lobe epilepsy: correlation with early childhood convulsions. Ann Neurol. 1987;22(3):334–40. doi: 10.1002/ana.410220309. [DOI] [PubMed] [Google Scholar]
- 74.Taylor DC, Ounsted C. Biological mechanisms influencing the outcome of seizures in response to fever. Epilepsia. 1971;12(1):33–45. doi: 10.1111/j.1528-1157.1971.tb03913.x. [DOI] [PubMed] [Google Scholar]
- 75.Baumer JH, David TJ, Valentine SJ, et al. Many parents think their child is dying when having a first febrile convulsion. Dev Med Child Neurol. 1981;23(4):462–4. doi: 10.1111/j.1469-8749.1981.tb02019.x. [DOI] [PubMed] [Google Scholar]
- 76.Shinnar S, O'Dell C. Treating childhood seizures: when and for how long. In: Shinnar S, Amir N, Branski D, editors. Childhood Seizures. S Karger: Basel; 1995. pp. 100–10. [Google Scholar]
- 77.Rutter N, Metcalfe DH. Febrile convulsions: What do parents do? Br Med J. 1978;2(6148):1345–6. doi: 10.1136/bmj.2.6148.1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Camfield PR, Camfield CS, Shapiro S, et al. The first febrile seizure--antipyretic instruction plus either phenobarbital or placebo to prevent a recurrence. J Pediatr. 1980;97(1):16–21. doi: 10.1016/s0022-3476(80)80122-3. [DOI] [PubMed] [Google Scholar]
- 79.Autret E, Billard C, Bertrand P, et al. Double.blind randomized trial of diazepam versus placebo for prevention of recurrence of febrile seizures. J Pediatr. 1990;117(3):490–5. doi: 10.1016/s0022-3476(05)81104-7. [DOI] [PubMed] [Google Scholar]
- 80.Knudsen FU. Effective short-term diazepam prophylaxis in febrile convulsions. J Pediatr. 1985;106(3):487–90. doi: 10.1016/s0022-3476(85)80688-0. [DOI] [PubMed] [Google Scholar]
- 81.Knudsen FU, Vestermark S. Prophylactic diazepam or phenobarbitone in febrile convulsions: a prospective, controlled study. Arch Dis Child. 1978;53(8):660–3. doi: 10.1136/adc.53.8.660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.McKinlay I, Newton R. Intention to treat febrile convulsions with rectal diazepam, valproate or phenobarbitone. Dev Med Child Neurol. 1989;31(5):617–25. doi: 10.1111/j.1469-8749.1989.tb04047.x. [DOI] [PubMed] [Google Scholar]
- 83.Rosman NP, Colton T, Labazzo J, et al. A controlled trial of diazepam administered during febrile illnesses to prevent recurrence of febrile seizures. N Engl J Med. 1993;329(2):79–84. doi: 10.1056/NEJM199307083290202. [DOI] [PubMed] [Google Scholar]
- 84.Rose W, Kirubakaran C, Scott JX. Intermittent clobazam therapy in febrile seizures. Indian J Pediatr. 2005;72(1):31–3. doi: 10.1007/BF02760577. [DOI] [PubMed] [Google Scholar]
- 85.Manreza ML, Gherpelli JL, Machado-Haertel LR, et al. Treatment of febrile seizures with intermittent clobazam. Arq Neuropsiquiatr. 1997;55(4):757–61. doi: 10.1590/s0004-282x1997000500012. [DOI] [PubMed] [Google Scholar]
- 86.Tondi M, Carboni F, Deriu A, et al. Intermittent therapy with clobazam for simple febrile convulsions. Dev Med Child Neurol. 1987;29(6):830–1. [PubMed] [Google Scholar]
- 87.Wassner E, Morris B, Fernando L, et al. Intranasal midazolam for treating febrile seizures in children. Buccal midazolam for childhood seizures at home preferred to rectal diazepam. BMJ. 2001;322(7278):108. [PubMed] [Google Scholar]
- 88.Scott RC, Besag FM, Neville BG. Intranasal midazolam for treating febrile seizures in children. Buccal midazolam should be preferred to nasal midazolam. BMJ. 2001;322(7278):107. [PubMed] [Google Scholar]
- 89.Pearce JL, Sharman JR, Forster RM. Phenobarbital in the acute management of febrile seizures. Pediatrics. 1977;60(4 pt2):569–72. [PubMed] [Google Scholar]
- 90.Wolf SM, Carr A, Davis DC, et al. The value of phenobarbital in the child who has had a single febrile seizure: a controlled prospective study. Pediatrics. 1977;59(3):378–85. [PubMed] [Google Scholar]
- 91.Antony JH, Hawke SH. Phenobarbital compared with carbamazepine in prevention of recurrent febrile convulsions. Am J Dis Child. 1983;137(9):892–5. doi: 10.1001/archpedi.1983.02140350066016. [DOI] [PubMed] [Google Scholar]
- 92.Bacon C, Mucklow J, Rawlins M, et al. Placebo-controlled study of phenobarbital and phenytoin in the prophylaxis of febrile convulsions. Lancet. 1981;11(8247):600–3. doi: 10.1016/s0140-6736(81)92742-2. [DOI] [PubMed] [Google Scholar]
- 93.Herranz JL, Armijo JA, Arteaga R. Effectiveness and toxicity of phenobarbital, primidone, and sodium valproate in the prevention of febrile convulsions, controlled by plasma levels. Epilepsia. 1984;25(1):89–95. doi: 10.1111/j.1528-1157.1984.tb04160.x. [DOI] [PubMed] [Google Scholar]
- 94.Newton RW. Randomized controlled trials of phenobarbitone and valproate in febrile convulsions. Arch Dis Child. 1988;63(10):1189–92. doi: 10.1136/adc.63.10.1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.American Academy of Pediatrics: Committee on Drugs. Behavioral and cognitive effects of anticonvulsant therapy. Pediatrics. 1995;96(3 pt 1):538–40. [PubMed] [Google Scholar]
- 96.Camfield CS, Chaplin S, Doyle AB, et al. Side effects of phenobarbital in toddlers: behavioral and cognitive aspects. J Pediatr. 1979;95(3):361–5. doi: 10.1016/s0022-3476(79)80507-7. [DOI] [PubMed] [Google Scholar]
- 97.Farwell J, Lee YJ, Hirtz DG, et al. Phenobarbital for febrile seizures: effects on intelligence and on seizure recurrence. N Engl J Med. 1990;322(6):364–9. doi: 10.1056/NEJM199002083220604. [DOI] [PubMed] [Google Scholar]
- 98.Olson JE, Scher MS, Holtzman D. Effects of anticonvulsants on hyperthermia-induced seizures in the rat pup. Epilepsia. 1984;25(1):96–9. doi: 10.1111/j.1528-1157.1984.tb04161.x. [DOI] [PubMed] [Google Scholar]
- 99.Dreifuss FE, Langer DH, Moline KA, et al. Valproic acid hepatic fatalities. II. U.S. experience since 1984. Neurology. 1989;39(2 pt1):201–7. doi: 10.1212/wnl.39.2.201. [DOI] [PubMed] [Google Scholar]
- 100.Dreifuss FE, Santilli N, Langer DH, et al. Valproic acid hepatic fatalities: a retrospective review. Neurology. 1987;37(3):379–85. doi: 10.1212/wnl.37.3.379. [DOI] [PubMed] [Google Scholar]
- 101.Lotowska JM, Sobaniec-Lotowska ME, Sobaniec W. Ultrastructural features of astrocytes in the cortex of the hippocampal gyrus and in the neocortex of the temporal lobe in an experimental model of febrile seizures and with the use of topiramate. Folia Neuropathol. 2009;47(3):268–77. [PubMed] [Google Scholar]
- 102.Lotowska JM, Sobaniec-Lotowska ME, Sendrowski K, et al. Ultrastructure of the blood-brain barrier of the gyrus hippocampal cortex in an experimental model of febrile seizures and with the use of a new generation antiepileptic drug-topiramate. Folia Neuropathol. 2008;46(1):57–68. [PubMed] [Google Scholar]
- 103.Sendrowski K, Sobaniec W, Sobaniec.Lotowska ME, Artemowicz B. Topiramate as a neuroprotectant in the experimental model of febrile seizures. Adv Med Sci. 2007;52(Suppl 1):161–5. [PubMed] [Google Scholar]