Abstract
Objective
Hepatitis C virus (HCV) is an etiological agent responsible for occurrence of post-transfusion hepatitis in thalassemic patients. This study identified hepatitis C genotypes in pediatric and adolescent thalassemic patients and their correlation with age, blood transfusion, HCV RNA viral titer and liver function.
Methods
This study considers cross-sectional data from the Center for Thalassemia in Zahedan (Iran) carried out between August 2005 and September 2007. Twenty multitransfused patients suffering from β-thalassemia major and chronic HCV infection (13 males, 7 females) were included in the study. Patients were considered eligible for the study if they were seropositive for HCV RNA polymerase chain reaction (PCR) before initiation of evaluation. Blood sample was taken for HCV genotype and viral titer as well as biochemical markers. Type specific primer and real-time RT-PCR HCV were used for determination of viral genotype and HCV-RNA titer.
Findings
There was a significant positive correlation between serum HCV RNA titer and genotypes (P<0001). Serum HCV RNA levels were found higher in genotype 3a than in others. The most prevalent genotype in thalassemic patients was genotype 3a (40%) followed by 1b (25%), unclassified (20%) and la (15%). There was no meaningful relationship between genotype, Alanine aminotranferease, ferritin and alkaline phosphatase. Age, serum HCV RNA titer and number of transfusions were the only significant factors associated with genotypes (P<015, P<0.0001 and P<0.001 respectively).
Conclusion
This study showed that HCV genotype and viral titer are related to the number of blood transfusions received by thalassemic patients. Screening donated blood in blood banks would prevent the occurrence of hepatitis C in this high-risk group.
Keywords: Hepatitis C, Virus Titer, Viral Load, Liver Function Tests, Thalassemia, Iran
Introduction
Chronic hepatitis C (HCV) infection is a serious threat to public health especially among children and adolescents. HCV affects nearly 200 million people worldwide and is responsible for at least 90% of the transfusion-associated cases of non-A non-B hepatitis[1]. Multitransfused β–thalas-semic patients constitute a population with high prevalence of HCV infection. Screening blood donors with new tests has reduced the risk of transfusion-transmitted HCV to approximately 1 in 2 million blood units[2]. Therefore, the survival of thalassemic patients has improved due to better blood transfusion protocols and chelation therapy[3]. As life expectancy of these patients prolongs, the consequences of chronic liver disease are likely to increase. The main causes of liver injury among this group are HCV infection and hepatic iron overload, both secondary to the regular transfusion regimen[4]. New treatments such as ribavirin plus interferon can improve response rates in children with chronic hepatitis C[5, 6]. In addition, early initiation of antiviral treatment is associated with a sustained response rate independent of treatment type. Regular follow-up of this at risk children should assist in the early diagnosis[7].
In Iran, according to the latest data, it was estimated that between 0.12-0.89 percent of general population acquire anti-hepatitis C virus antibodies, which corresponds to about 0.5 million chronic carriers[8, 9]. A research in Iran showed that more than 60% of multitransfused patients with major thalassemia are infected by the virus[10]. However, another report selected from five provinces of Iran showed that the prevalence of HCV infection is 19% among Iranian β-thalassemic patients[11]. In addition, a report on seroprevalence of hepatitis B, C and human immunodeficiency virus (HIV) antibodies among thalassaemic children in Iran revealed that HCV is the current major problem in multitransfused patients with thalassaemia[12]. Therefore, more careful pretransfusion screening of blood for anti-HCV must be introduced in Iranian blood banks.
HCV has high genetic heterogeneity and is classified into various genotypes[13]. Regional differences appear to exist in distribution of HCV genotypes. Determination of HCV genotypes may have important implications for prognosis and treatment[14]. Moreover, the geographic distribution and diversity of HCV genotypes may provide clues about the historical origin of HCV[15].
HCV genotyping in thalassemia is mainly useful for the clinical management of the patients and for facilitating decisions on therapy[16]. Some studies showed that both HCV RNA level and genotype could predict response to interferon[17]. Also reports revealed that the HCV genotype was related to HCV RNA in serum, the stage of liver disease and cirrhosis[18]. There is little data about HCV genotypes in children with thalassemia in Iran. Thus, the aim of the present study was to identify the genotypes that are prevalent in this region and to correlate these with age, number of blood transfusions, HCV RNA viral titer and liver tests.
Subjects and Methods
Patients: A cross-sectional study between August 2005 and September 2007 took place on patients attending the Center for Special Diseases in Ali-Asghar Hospital, Zahedan (Iran). There were 560 patients with β-thalassemia major who received regular transfusions of packed erythrocytes at 3-4 week intervals in order to maintain the hemoglobin level above 10 g/dl. In addition, they received iron chelation by daily subcutaneous administration of deferoxamine, or by oral administration of deferiprone. All of patients in this center were checked for HBsAg, HCV Ab and HIV routinely. HCV Ab was tested in all patients after 1997. Thirty samples were positive for HCV Ab (tested by ELISA II). Performing Qualitative HCV RNA polymerase chain reaction (PCR) in these samples demonstrated 20 cases (13 males, 7 females). None of patients received anti-viral therapy for HCV. All subjects were vaccinated against hepatitis B. None of them was HBs Ag or HIV positive. Patients with seropositivity for HCV antibody and qualitative HCV RNA PCR were included in the study.
Definition of chronic HCV infection includes the presence of HCV RNA in serum. All reverse transcription PCR assays and biochemical markers were performed in a single laboratory.
Data collected for each subject included: age, gender, and number of blood transfusions, HCV RNA viral titer, and liver enzyms, alanine aminotranferease (ALT) and aspartate aminotransferase (AST), alkaline phosphatase (ALP) and Ferritin. The Ethical Committee of Zahedan University of Medical Sciences approved the study. Informed consent to participate was obtained from all patients.
HCV genotype and viral load: For genotyping, we used HCV type-specific primers designed by Okamoto et al[19]. Checking genotype needs three steps; at first, we extracted RNA virus by Tripure Method (Roche, Germany), then RNA was converted to cDNA by random Hexamer and MMLV enzyme (Promega, USA). Finaly, cDNA was amplified by allele specific PCR method. For each patient 2 vials containing primer specific for 1a/1b and 2 and 3a were used.
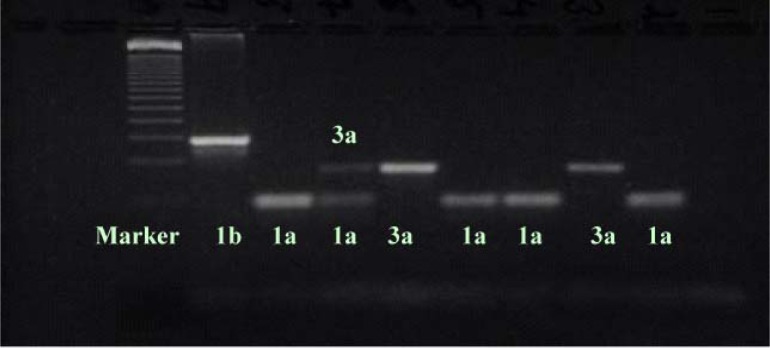
The PCR program was 96C 6min 1 cycle, 95C 1min, 60C 1min, 72C 1min for 40 cycles and final extension 72C for 10min 1 cycle. Positive control for each genotype was supplied by kit manufacture. In addition, HCV viral load was determined using the Artus Real Art Kit. We used real time (light cycler Roche) for assays. The slope of reaction was between 3.2-3.4 and error less than 0.002 in each experiment. All results of quantitative HCV viremia were expressed as log, copies/ml. Detection of different HCV genotypes is shown in Fig. 1.
Fig. 1.
Detection of different hepatitis C virus genotypes
Biochemical markers: Serum ferritin, alanine aminotransferase (ALT), aspartate aminotransferase (AST) and alkaline phosphatase (ALP) were measured at six monthly intervals, and mean values in two-year period were recorded before this evaluation. Biochemical markers were determined by autoanalysis (Normal range: ALT 0-37 mg/dl, AST 0-41 mg/dl, ALP 64-306 mg/dl, Ferritin 20- 220 mg/ dl).
Statistical analysis: Regarding inequality in groups and small sample size, we used non- parametric tests (Kruskal–Wallis) at first, then Scheffe post hoc and ANOVA tests for determining association between genotype and dependent variables. Also, Pearson correlation was used for finding relationship between ALT, AST, ALP, ferritin, viral load and number of transfusions. Statistical tests were conducted at the P<0.05 significance level.
Findings
Demographic, biochemical and virological data of participants in this study are presented in table 1. Twenty patients were evaluated (median age 13.7 yr, range 8-18 yr). Median age at diagnosis of thalassemia was 7.5 months, with 83% being under 1 year. There were 13 males and 7 females in this study. They had received regular transfusions for a median of 13 years (range 3 months to 18 years). All of patients had received blood transfusion before 1996. Unfortunately, we were not able to check HCV serology since three years ago in this part of Iran. Three (15.8%) patients had undergone splenectomy in the past. There was a positive significant correlation between serum HCV RNA titer and genotypes (P<0001), (Table 2). Serum HCV RNA levels were found to be significantly higher in genotype 3a than in others. The most prevalent genotype in thalassemic patients was genotype 3a (40%) followed by 1b (25%), unclassified (20%) and la (15%). Results of Pearson correlation revealed correlation between ALT and AST and ferritin (P<0.01, r=0.6), age and ALT (P=0.04, r= -0.48), ALT and AST (P=0.001, r= 0.97).
Table 1.
Demographic, biochemical and virological data of participants
| Parameter | Mean (SD*) |
|---|---|
| Age(year) | 13.47 (3.92) |
| Aspartate aminotransferase (AST) (mg/dl) | 110.11 (56.37) |
| Alanine aminotranferease (ALT) (mg/dl) | 126.05 (69.06) |
| Alkaline phosphatase (mg/dl) | 497.28 (237.32) |
| Ferritin (mg/dl) | 2464 (915.75) |
| Amount of transfusion (ml) | 98125 (49844) |
| Number of transfusions received prior to diagnosis (times) | 204 (90) |
| Duration of transfusion therapy (year) | 13.4 (3.1) |
SD: Standard Deviation
Table 2.
Association of different genotypes with dependent variables [Mean (SD)]
| Genotype | 3a (No=8) | Undetectable (No=4) | 1b (No=5) | 1a (No=3) | P. value |
|---|---|---|---|---|---|
| Viral Titer (log, copies/ml) | 6.4 (0.81) | 2.9 (1.2) | 5.3 (0.82) | 6.2 (0.33) | 0.0001 |
| ALT (mg/dl) | 113.6 (45.5) | 143 (132.9) | 87 (39.6) | 206 (13.3) | 0.09 |
| Ferritin (mg/dl) | 2234.2 (890.1) | 2836.6 (1955.7) | 2579.8 (486.7) | 2511 (137.5) | 0.8 |
| ALP (mg/dl) | 480.5 (161.7) | 672.6 (277.2) | 432.4 (338.7) | 463.5 (208.5) | 0.5 |
| Number of blood transfusions | 152.2 (34.1) | 259 (77) | 341.8 (78.1) | 138.9 (52.5) | 0.001 |
| Age (yr) | 12.3 (2.5) | 15.7 (1.8) | 15.9 (2) | 11.1 (3) | 0.015 |
ALT: alanine aminotranferease/ AST: Aspartate aminotransferase/ ALP: alkaline phosphatase
In this data set, all of patients had abnormal levels of ALT and AST except one patient infected with HCV type 1b. ALT is more specific than AST for evaluation of liver function. Therefore, for association of variables we use only ALT. Age, Serum HCV RNA levels and number of transfusions were the only significant factors associated with genotypes (P=0.015, P<0.0001 and P<0.001 respectively). Subjects infected with HCV type 1a were younger than others.
Scheffe post hoc showed that the differences between viral titers are due to undetectable genotypes.
Discussion
Using regular transfusion and attention to screen transfused blood in children and adolescents with thalassemia may improve survival of these patients beyond the third decade[20]. However, multitransfused β-thalassaemic patients are still at a risk of acquiring hepatitis C through administration of HCV-infected blood collected during the seronegative window period[21].
Low pretreatment serum HCV-RNA level and HCV genotype plus interferon treatment are the main determinants for the induction of a virological primary response in chronic hepatitis C[17, 22], although the prognostic value of these factors is of limited value in individual cases[23]. However, Characterization of HCV types and subtypes is likely to facilitate and contribute to the development of an effective vaccine against infection with HCV. Differences among HCV genotypes in geographic distributions have provided investigators with an epidemiologic marker that can be used to find the source of HCV infection in a given population. The most prevalent genotype in our study was genotype 3a (40%) followed by 1b (25%), unclassified (20%) and la (15%).
A new research for investigation of HCV genotypes in Iranian patients showed that Genotype 1 and 3 are the most frequently detected type in subjects with thalassemia[24]. Another study on frequency of HCV genotypes in 2231 Iranians with hepatitis C indicated type 1a as the most frequent type in patients followed by genotype 3a and 1b[25]. HCV genotypes among thalassemic patients reported from Greece and Italy was predominantly type 4 followed by 1, although one report from India showed preponderance of genotypes 3 and 1[26–28]. It is known that genotype 3a is commonly encountered in young males, especially young intravenous drug users[29]. We found that genotype 3a was predominant in our patients. Some studies have shown that genotype 3a is associated with a more favorable response to interferon therapy than genotype 1[30]. Further-more, studies have reported an association of subtype 1b with advanced liver disease, higher viral load, histological activity, severe iron overload and more need for splenectomy[31, 32, 24]. Since our analysis was based on cross-sectional data with low sample size, further studies are needed to clarify that.
The results obtained in this study revealed an association between all different genotypes and viral titer except in unclassified group.
Researches showed that low serum HCV RNA and genotypes other than genotype 1 are related to sustained response[17, 33]. These results indicated that HCV genotypes and pretreatment levels of HCV RNA in serum, influence response to interferon. In this study, we investigated 20 subjects with major thalassemia. Although this rate is not as high as the rate reported in other studies[10, 11], it is still far higher than the rate in healthy donors[8, 9]. Therefore, screening of donated blood would prevent serious problems in future.
The results of correlation between seropositivity for HCV studies and age at transfusion or total number of blood transfusions have yielded controversial data [34, 35]. Only three patients in present study were below 13 years old which emphasize on good screening blood at Zahedan. Unfortunately, screening of blood donors in this region of Iran has started in 1997. In addition, our study showed significant correlation between HCV RNA titer and the number of blood transfusions. More studies are needed to find these relations.
We also observed an association between the presence of HCV RNA PCR and abnormal liver tests. The findings are consistent with a new study in thalassemic patients of Tonekabon which demonstrated close association between elevated ALT with iron overload, transfusion index, age, and anti-HCV positivity[35]. The long-term follow-up of these patients have shown that aminotransferase flares are frequent among thalassemics, even in the absence of HCV infection[36]. In this study, level of AST, ALT and ferritin had significantly altered in patients and there was a correlation between ALT and AST, and feritin and age and ALT. Some studies have shown that beta-thalassemia major, older age, long duration of transfusion and higher serum ferritin level were significantly associated with a higher prevalence of HCV[11].
Conclusion
This study showed that HCV genotype and viral titer are related to number of blood transfusions received by children and adolescent with thalassemia. The blood policy followed by blood banks for providing safe blood along with better screening method of donated blood in blood banks would bring down the incidence of hepatitis C in such high-risk group.
Acknowledgment
Our thanks go to all who participated actively in this project especially Zahedan Blood Transfusion Center. The authors want to thank from Dr. Sanie at Iranian Blood Transfusion Center and Research Center for Children and Adolescences Health for their invaluable help.
Conflict of Interest
There were not any conflicts of interest.
References
- 1.Sarbah SA, Younossi ZM. Hepatitis C: an update on the silent epidemic. J Clin Gastroenterol. 2000;30(2):125–43. doi: 10.1097/00004836-200003000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Stramer SL, Glynn SA, Kleinman SH, et al. Detection of HIV-1 and HCV infections among antibody-negative blood donors by nucleic acid-amplification testing. N Engl J Med. 2004;351(8):760–8. doi: 10.1056/NEJMoa040085. [DOI] [PubMed] [Google Scholar]
- 3.Ladis V, Chouliaras G, Berdousi H, et al. Longitudinal study of survival and causes of death in patients with thalassemia major in Greece. Ann N Y Acad Sci. 2005;1054:445–50. doi: 10.1196/annals.1345.067. [DOI] [PubMed] [Google Scholar]
- 4.Prati D. Benefits and complications of regular blood transfusion in patients with beta-thalassaemia major. Vox Sang. 2000;79(3):129–37. doi: 10.1159/000031230. [DOI] [PubMed] [Google Scholar]
- 5.Süoğlu D, Elkabes B, Sökücü S, Saner G. Does interferon and ribavirin combination therapy increase the rate of treatment response in children with hepatitis C? J Pediatr Gastroenterol Nutr. 2002;34(2):199–206. doi: 10.1097/00005176-200202000-00018. [DOI] [PubMed] [Google Scholar]
- 6.Wirth S, Lang T, Gehring S, Gerner P. Recombinant alfa-interferon plus ribavirin therapy in children and adolescents with chronic hepatitis C. Hepatology. 2002;36(5):1280–4. doi: 10.1053/jhep.2002.36495. [DOI] [PubMed] [Google Scholar]
- 7.Hartman C, Berkowitz D, Rimon N, Shamir R. The effect of early treatment in children with chronic hepatitis. J Pediatr Gastro-enterol Nutr. 2003;37(3):252–7. doi: 10.1097/00005176-200309000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Ghavanini AA, Sabri MR. Hepatitis B surface antigen and anti-hepatitis C antibodies among blood donors in the Islamic Republic of Iran. East Mediterr Health J. 2000;6(5–6):1114–6. [PubMed] [Google Scholar]
- 9.Alavian SM, Gholami B, Masarrat S. Hepatitis C risk factors in Iranian volunteer blood donors: a case-control study. J Gastroenterol Hepatol. 2002;17(10):1092–97. doi: 10.1046/j.1440-1746.2002.02843.x. [DOI] [PubMed] [Google Scholar]
- 10.Ansar MM, Kooloobandi A. Prevalence of hepatitis C virus infection in thalassemia and haemodialysis patients in north Iran-Rasht. J Viral Hepat. 2002;9(5):390–2. doi: 10.1046/j.1365-2893.2002.00368.x. [DOI] [PubMed] [Google Scholar]
- 11.Mirmomen S, Alavian SM, Hajarizadeh B, et al. Epidemiology of hepatitis B, hepatitis C, and human immunodeficiency virus infections in patients with beta-thalassemia in Iran: a multicenter study. Arch Iran Med. 2006;9(4):319–23. [PubMed] [Google Scholar]
- 12.Karimi M, Ghavanini AA, Seroprevalence of hepatitis B. hepatitis C and human immunodeficiency virus antibodies among multitransfused thalassaemic children in Shiraz, Iran. J Paediatr Child Health. 2001;37(6):564–6. doi: 10.1046/j.1440-1754.2001.00709.x. [DOI] [PubMed] [Google Scholar]
- 13.Zein NN, Persing DH. Hepatitis C genotypes: current trends and future implications. Mayo Clin Proc. 1996;71(5):458–62. doi: 10.4065/71.5.458. [DOI] [PubMed] [Google Scholar]
- 14.Smith DB, Simmonds P. Review: molecular epidemiology of hepatitis C virus. J Gastroenterol Hepatol. 1997;12(7):522–7. doi: 10.1111/j.1440-1746.1997.tb00477.x. [DOI] [PubMed] [Google Scholar]
- 15.Zein NN. Clinical significance of hepatitis C virus genotypes. Clin Microbiol Rev. 2000;13(2):223–35. doi: 10.1128/cmr.13.2.223-235.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Izopet J, Payen JL, Alric L, et al. Baseline level and early suppression of serum HCV RNA for predicting sustained complete response to alpha-interferon therapy. J Med Virol. 1998;54(2):86–91. doi: 10.1002/(sici)1096-9071(199802)54:2<86::aid-jmv3>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 17.Hosogaya S, Ozaki Y, Enomoto N, Akahane Y. Analysis of prognostic factors in therapeutic responses to interferon in patients with chronic hepatitis C. Transl Res. 2006;148(2):79–86. doi: 10.1016/j.trsl.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 18.Gervais A, Martinot M, Boyer N, et al. Quantitation of hepatic hepatitis C virus RNA in patients with chronic hepatitis C. Relationship with severity of disease, viral genotype and response to treatment. J Hepatol. 2001;35(3):399–405. doi: 10.1016/s0168-8278(01)00138-6. [DOI] [PubMed] [Google Scholar]
- 19.Okamoto H, Sugiyama Y, Okada S, et al. Typing hepatitis C virus by polymerase chain reaction with type-specific primers: application to clinical surveys and tracing infectious sources. J Gen Virol. 1992;73(pt 3):673–9. doi: 10.1099/0022-1317-73-3-673. [DOI] [PubMed] [Google Scholar]
- 20.Roudbari M, Soltani-Rad M, Roudbari S. The survival analysis of beta thalassemia major patients in South East of Iran. Saudi Med J. 2008;29(7):1031–5. [PubMed] [Google Scholar]
- 21.Vrielink H, van der Poel CL, Reesink HW, et al. Transmission of hepatitis C virus by anti HCV-negative blood transfusion. Case report. Vox Sang. 1995;68(1):55–6. doi: 10.1111/j.1423-0410.1995.tb02546.x. [DOI] [PubMed] [Google Scholar]
- 22.Manesis EK, Papaioannou C, Gioustozi A, et al. Biochemical and virological outcome of patients with chronic hepatitis C treated with interferon alfa-2b for 6 or 12 months: a 4-year follow-up of 211 patients. Hepatology. 1997;26(3):734–9. doi: 10.1002/hep.510260327. [DOI] [PubMed] [Google Scholar]
- 23.Conjeevaram HS, Everhart JE, Hoofnagle JH. Predictors of a sustained beneficial response to interferon alfa therapy in chronic hepatitis C. Hepatology. 1995;22(4 pt 1):1326–9. doi: 10.1016/0270-9139(95)90646-0. [DOI] [PubMed] [Google Scholar]
- 24.Alavian SM, Miri SM, Keshvari M, et al. Distribution of hepatitis C virus genotype in Iranian multiply transfused patients with thalassemia. Transfusion. 2009;49(10):2195–9. doi: 10.1111/j.1537-2995.2009.02252.x. [DOI] [PubMed] [Google Scholar]
- 25.Keyvani H, Alizadeh AH, Alavian SM, et al. Distribution frequency of hepatitis C virus genotypes in 2231 patients in Iran. Hepatol Res. 2007;37(2):101–3. doi: 10.1111/j.1872-034X.2007.00015.x. [DOI] [PubMed] [Google Scholar]
- 26.Siagris D, Giannakoulas N, Christofidou M, et al. Virological, immunological and histological aspects in adult beta-thalassemic patients with chronic hepatitis C virus infection. Liver Int. 2004;24(3):204–9. doi: 10.1111/j.1478-3231.2004.0919.x. [DOI] [PubMed] [Google Scholar]
- 27.Di Marco V, Lo Iacono O, Almasio P, et al. Long-term efficacy of alpha-interferon in beta-thalassemics with chronic hepatitis C. Blood. 1997;90(6):2207–12. [PubMed] [Google Scholar]
- 28.Chakravarti A. Verma V. Distribution of hepatitis C virus genotypes in beta-thalassaemic patients from Northern India. Transfus Med. 2006;16(6):433–8. doi: 10.1111/j.1365-3148.2006.00704.x. [DOI] [PubMed] [Google Scholar]
- 29.Farci P, Purcell RH. Clinical significance of hepatitis C virus genotypes and quasispecies. Semin Liver Dis. 2000;20(1):103–26. [PubMed] [Google Scholar]
- 30.Sharara AI, Hunt CM, Hamilton JD, Hepatitis C. Ann Intern Med. 1996;125(8):658–68. doi: 10.7326/0003-4819-125-8-199610150-00006. [DOI] [PubMed] [Google Scholar]
- 31.Svirtlih N, Delic D, Simonovic J, et al. Hepatitis C virus genotypes in Serbia and Montenegro: the prevalence and clinical significance. World J Gastroenterol. 2007;13(3):355–60. doi: 10.3748/wjg.v13.i3.355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zein NN, Rakela J, Krawitt EL, et al. Hepatitis C virus genotypes in the United States: epidemiology, pathogenicity, and response to interferon therapy. Ann Intern Med. 1996;125(8):634–9. doi: 10.7326/0003-4819-125-8-199610150-00002. [DOI] [PubMed] [Google Scholar]
- 33.Martinot-Peignoux M, Marcellin P, Pouteau M, et al. Pretreatment serum hepatitis C virus RNA levels and hepatitis C virus genotype are the main and independent prognostic factors of sustained response to interferon alfa therapy in chronic hepatitis C. Hepatology. 1995;22(4 pt 1):1050–6. [PubMed] [Google Scholar]
- 34.Wonke B, Hoffbrand AV, Brown D, Dusheiko G. Antibody to hepatitis C virus in multiply transfused patients with thalassaemia major. J Clin Pathol. 1990;43(8):638–40. doi: 10.1136/jcp.43.8.638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ameli M, Besharati S, Nemati K, Zamani F. Relationship between elevated liver enzyme with iron overload and viral hepatitis in thalassemia major patients in Northern Iran. Saudi Med J. 2008;29(11):1611–5. [PubMed] [Google Scholar]
- 36.Prati D, Zanella A, Farma E, et al. A multicenter prospective study on the risk of acquiring liver disease in anti-hepatitis C virus negative patients affected from homozygous beta-thalassemia. Blood. 1998;92(9):3460–4. [PubMed] [Google Scholar]