Abstract
Background
Children with overgrowth syndromes including isolated hemihyperplasia have an increased risk for developing embryonal tumors, particularly Wilms’ tumor and hepatoblastoma. Screening with sonography has been suggested as a method of identifying these tumors while they are still at an early stage.
Case Presentation
We describe an infant diagnosed with Wilms tumor in whom isolated hemihyperplasia had been overlooked by several physicians prior to the tumor diagnosis.
Conclusion
We recommend tumor surveillance for all patients with Beckwith-Wiedemann syndrome and isolated hemihyperplasia at least for the first six years of life since full molecular characterization of every patient is not readily available.
Keywords: Wilms Tumor, Neoplasms, Embryonal, Hemihyperplasia, Children, Infant
Introduction
The asymmetric overgrowth traditionally termed hemihypertrophy is more accurately referred to as hemihyperplasia, since the pathologic growth process involves an abnormal proliferation of cells (hemihyperplasia), rather than an increase in size of existing cells (hemihypertrophy)[1]. Hemihyperplasia is clinically defined as asymmetric growth due to the overgrowth of one or more body parts.
Hemihyperplasia may be an isolated finding, or it may be associated with a variety of multiple malformation syndromes, such as Beckwith-Wiedemann syndrome (BWS), Proteus syndrome, Russell-Silver syndrome, and Sotos syndrome[2, 3]. Rowe[4] proposed a classification system for hemihyperplasia, based on anatomic site of involvement. According to this classification, complex hemihyperplasia is defined as involvement of half of the body (at least one arm and one leg), simple hemihyperplasia is the involvement of a single limb and hemifacial hyperplasia is the involvement of one side of the face[4]. The degree of asymmetry is variable, and mild cases are easily overlooked[5]. The prevalence of isolated hemihyperplasia (IHH) is difficult to establish accurately because many cases may be so mild as not to come to medical attention. The prevalence for hemihyperplasia was reported as approximately 1 in 86,000[6].
It is well documented that children with BWS and IHH have an increased risk of developing embryonic neoplasms, including Wilms tumor[3, 5, 7–10]. Here we describe an infant with Wilms tumor in whom isolated hemihyperplasia had been overlooked by several physicians prior to tumor diagnosis.
Case Presentation
A 12-month old girl was referred to our pediatric oncology department for further investigation of an abdominal mass. On initial physical examination her weight was in 90th percentile, length in the 75th percentile. Her right cheek was slightly fuller than left cheek. The right arm and forearm were thicker than counterparts on the left. The right leg was thicker and measured approximately 2 cm longer than left leg. We noticed a right sided complex hemihyperplasia (Fig. 1a, 1b) as well as a right-sided abdominal mass of 10 cm dia-meter. Her blood pressure and other vital signs were normal. A detailed medical history showed that the mother first noticed the asymmetry of her legs when she was three months old and took her to a pediatrician. The physician's presumptive diagnosis was congenital hip dislocation. Therefore a hip ultrasonography (US) was performed which showed no evidence of hip dislocation. An orthopedic surgeon was consulted, who ruled out a hip problem. Then the family was told it was something constitutional and no other recommendation was made. The infant was otherwise healthy during the following months, however the family noticed that the cheeks were also growing asymmetric but they took no other action since they were told it was constitutional and would do no harm to the child. The family history was unremarkable and she was the first and only child of the parents who was born weighing 3.5 kg after an uneventful pregnancy.
Fig. 1.
Complex hemihyperplasia involving the right half of the face and the body
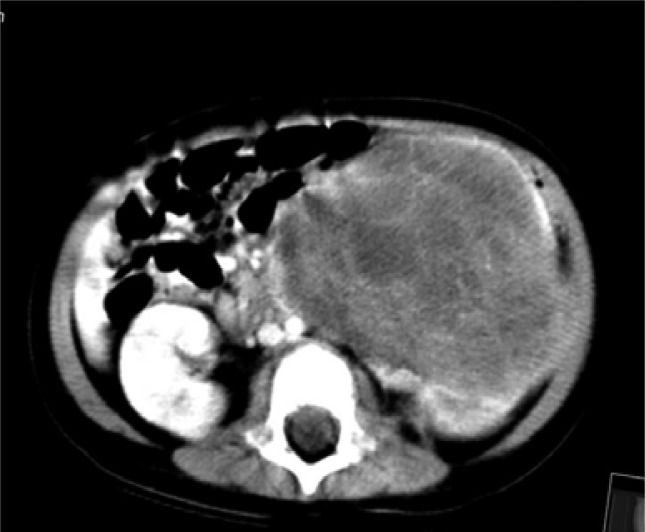
At the age of 12 months, when she developed macroscopic hematuria, an abdominal US showed a right sided renal mass. The patient was then referred to our hospital for further investigation and management. A renal mass and hematuria in an infant with isolated hemihyperplasia strongly suggested a Wilms’ tumor. An abdominal US and a computed tomography (CT) scan confirmed a cystic/solid mass of 10 cm in diameter at the right kidney consistent with Wilms tumor (Fig 2). Left renal vein and inferior vena cava were free of tumor infiltration. Right kidney was normal and there was no evidence of intraabdominal extention of tumor beyond the kidney. Metastatic work-up including chest X-ray and chest CT showed no distant metastatic disease.
Fig. 2.
Abdominal computerized tomography revealing a cystic/solid mass of 10 cm in diameter at the right kidney consistent with Wilms tumor.
A pre-operative diagnosis of Wilms tumor was made by clinical and radiological findings without biopsy. She was put on preoperative chemotherapy with two drugs (vincristine 1.4 mg/m2 weekly, 4 weeks; actinomycin-D 0.015 mg/kg/day, 1-5 days) since she had a large tumor to avoid capsule perforation during surgery. After significant regression with preoperative chemotherapy, a radical right nephrectomy was performed through a transabdominal approach. A final diagnosis of Wilms tumor, stage I favorable histology, was made. The patient received postoperative chemotherapy according to stage-I Wilms’ tumor (vincristine 1.4 mg/m2 weekly, 24 weeks; actinomycin-D 0.015 mg/kg/day, 1-5 days, 6 weeks interval). The treatment was well tolerated. We have been following her with regular (every three months) abdominal US and urine analysis to detect any recurrence of Wilms tumor or for the development of any other embryonal tumor. She has been in complete remission for four years. This screening process will be continued until she becomes 7 years old.
Discussion
Our patient had complex hemihyperplasia involving the right half of her body and face. The asymmetry may become more pronounced with age as it happened in this case[5]. Hemihyperplasia of the limb(s) involves a discrepancy in both length and circumference of the affected limb in comparison to the contralateral side as it can be seen in Fig 1b.
Although the mother of our patient noticed the asymmetry involving the legs when she was only 3 months of age, the physicians who previously evaluated her either overlooked hemihyperplasia or couldn't recognize the relation between overgrowth syndromes and embryonal tumors. Simple hemihyperplasia can be more easily overlooked, however complex hemihyperplasia is a more striking feature. A report from The National Wilms Tumor Study showed that in only 32% of children with Wilms tumor and IHH the asymmetry was appreciated more than one month prior to the diagnosis of the associated tumor[11]. Another study from UK demonstrated that the asymmetry was not detected until the diagnosis of cancer in 50% of IHH cases with cancer[12].
The association of embryonal tumors with overgrowth syndromes is well recognized. If a physician overlooks the findings of hemihyperplasia, he/she also overlooks the increased risk of embriyonal tumors in these children. In BWS, intra-abdominal tumors of embryonal origin, most commonly Wilms tumor (43%), hepatoblastoma (20%), adrenocortical carcinoma (7%) and neuroblastoma (5%) may occur[10]. The tumor incidence for IHH was reported as 5.9%, slightly lower than the 7.5-10% incidence in BWS[5, 8, 9]. Significantly less tumor-risk data is available for IHH than for BWS. This may partly be related to the fact that isolated hemihyperplasia is a poorly defined entity. Because of overlap in clinical findings and lack of generally agreed upon diagnostic criteria, these two disorders are often grouped together and it is uncertain if the difference in tumor risk is significant. Screening for early detection of abdominal malignancy has been advocated for children with hemihyperplasia as it has been recommended in BWS. A potential benefit of screening is to identify any potential embriyonal tumor early when surgery and less intensive chemotherapy is curative and thus decreases the long term sequelae associated with radiation and more intensive chemotherapy. Various surveillance protocols for children with BWS/IHH has been recommended[7, 10, 13–15]. According to the case series by Choyke et al[16] children with BWS/IHH may benefit from screening abdominal US at intervals of four months or less, but false positive screening exams may result in unnecessary surgery. Green et al[11] analyzed the impact of surveillance in children with aniridia, BWS and IHH who had developed Wilms tumor.
They showed a higher proportion of stage I tumors identified in children who underwent radiographic surveillance than in those who did not, but in the BWS/IHH groups there were insufficient data to draw any conclusions. The Wilms Tumour Surveillance Working Group recommended surveillance for children at >5% risk of Wilms tumor[13]. The overall risk of WT in IHH has been estimated at only 3.5% but a small number of children with IHH who had uniparental disomy 11p15 are at >5% risk of Wilms tumor[5]. However, Wilms tumor is not the only tumor with an increased prevalance in overgrowth syndromes. Clericuzio et al[14] noted the importance of a combined surveillance for Wilms and hepatoblastoma (HBL). They described three children with BWS and two with IHH who developed hepatoblastomas detected by surveillance with serum alpha fetoprotein (AFP) measurement in conjunction with hepatic US. All five tumors were stage I, although more than half of all HBL use to present with advanced stage disease at the time of diagnosis. There is currently no definitive evidence that screening results in a marked decrease in either overall mortality or tumor stage in Wilms tumor.
However, children with overgrowth syndromes may present with smaller tumors and early stage disease if they are screened[16].
Conclusion
In conclusion, our unscreened patient, in whom hemihyperplasia had been noticed at three months of age by her mother, might also have presented with late-stage or metastatic Wilms tumor. Depending on the current experience in the literature, we recommend tumor surveillance for all patients with BWS and IHH at least for the first six years of life since full molecular characterization of every patient is not readily available. The tumor surveillance may not make a significant impact on overall survival, but has the potential to reduce treatment-related morbidity due to early stage disease. Further studies including clinical and molecular markers are needed to define the patient subgroup who definitely benefit from a surveillance program.
References
- 1.Cohen MM., Jr A comprehensive and critical assessment of overgrowth and overgrowth syndromes. Adv Hum Genet. 1989;18:181,373–303,376. doi: 10.1007/978-1-4613-0785-3_4. [DOI] [PubMed] [Google Scholar]
- 2.Ballock RT, Wiesner GL, Myers MT, et al. Hemihypertrophy. Concepts and controversies. J Bone Joint Surg Am. 1997;79(11):1731–8. doi: 10.2106/00004623-199711000-00016. [DOI] [PubMed] [Google Scholar]
- 3.Clericuzio CL. Recognition and management of childhood cancer syndromes: A systems approach. Am J Med Genet. 1999;89(2):81–90. doi: 10.1002/(sici)1096-8628(19990625)89:2<81::aid-ajmg5>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 4.Rowe NH. Hemifacial hypertrophy: Review of the literature and addition of four cases. Oral Surg. 1962;15:572–6. doi: 10.1016/0030-4220(62)90177-9. [DOI] [PubMed] [Google Scholar]
- 5.Hoyme HE, Seaver LH, Jones KL, et al. Isolated hemihyperplasia (hemihypertrophy): report of a prospective multicenter study of the incidence of neoplasia and review. Am J Med Genet. 1998;79(4):274–8. [PubMed] [Google Scholar]
- 6.Ringrose RE, Jabbour JT, Keele DK. Hemihypertrophy. Pediatrics. 1965;36(3):434–48. [PubMed] [Google Scholar]
- 7.Beckwith JB. Certain conditions have an increased incidence of Wilms’ tumor. AJR Am J Roentgenol. 1995;164(5):1294–5. doi: 10.2214/ajr.164.5.7717255. [DOI] [PubMed] [Google Scholar]
- 8.Wiedemann H. Tumors and hemihypertrophy associated with the Wiedemann-Beckwith syndrome. Eur J Pediatr. 1983;141(2):129. (Letter to editor) [Google Scholar]
- 9.DeBaun MR, Tucker MA. Risk of cancer during the first four years of life in children from The Beckwith-Wiedemann Syndrome Registry. J Pediatr. 1998;132(3 pt 1):398–400. doi: 10.1016/s0022-3476(98)70008-3. [DOI] [PubMed] [Google Scholar]
- 10.Lapunzina P. Risk of tumorigenesis in overgrowth syndromes: a comprehensive review. Am J Med Genet. 2005;137(1):53–71. doi: 10.1002/ajmg.c.30064. [DOI] [PubMed] [Google Scholar]
- 11.Green DM, Breslow NE, Beckwith JB, et al. Screening of children with hemihypertrophy, aniridia, and Beckwith-Wiedemann syndrome in patients with Wilms tumor: a report from The National Wilms Tumor Study. Med Pediatr Oncol. 1993;21(3):188–92. doi: 10.1002/mpo.2950210307. [DOI] [PubMed] [Google Scholar]
- 12.Craft AW, Parker L, Stiller C, et al. Screening for Wilms’ tumour in patients with aniridia, Beckwith syndrome, or hemihypertrophy. Med Pediatr Oncol. 1995;24(4):231–4. doi: 10.1002/mpo.2950240404. [DOI] [PubMed] [Google Scholar]
- 13.Surveillance for Wilms tumour in at-risk individuals– pragmatic recommendations for best practice. The Wilms Tumour Surveillance Working Group. 2005. Available from: http://www.bshg.org.uk/documents/other_docs/Wilms%20Tumour%20surveillance%20recommendations.pdf.
- 14.Clericuzio CL, Chen E, McNeil DE, et al. Serum alpha- fetoprotein screening for hepatoblastoma in children with Beckwith–Wiedemann syndrome or isolated hemihyperplasia. J Pediatr. 2003;143(2):270–2. doi: 10.1067/S0022-3476(03)00306-8. [DOI] [PubMed] [Google Scholar]
- 15.Tan TY, Amor DJ. Tumour surveillance in Beckwith–Wiedemann syndrome and hemihyperplasia: A critical review of the evidence and suggested guidelines for local practice. J Paediatr Child Health. 2006;42(9):486–90. doi: 10.1111/j.1440-1754.2006.00908.x. [DOI] [PubMed] [Google Scholar]
- 16.Choyke PL, Siegel MJ, Craft AW, et al. Screening for Wilms tumor in children with Beckwith–Wiedemann syndrome or idiopathic hemihypertrophy. Med Pediatr Oncol. 1999;32(3):196–200. doi: 10.1002/(sici)1096-911x(199903)32:3<196::aid-mpo6>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]