Abstract
Objective
Beta thalassemia major is a prevalent hereditary disease in Mediterranean region especially Iran. Early blood transfusion is necessary for most of the patients and frequent transfusion can cause various medical problems for the patients. The aim of this study was to find major causes of hospital admission in beta thalassemia major patients to reach the accurate preventive and therapeutic plans for these patients.
Methods
Four hundred twenty six patients were admitted to the Nemazee Hospital (the main University referral Hospital Center affiliated to Shiraz University of Medical Sciences in Fars Province, southern Iran) during 3 years period (January 2007 to January 2010). A questionnaire was filled containing age, gender, hemoglobin level, frequency of blood transfusions, deferoxamine injection, cause of hospital admission and hospital course.
Findings
The mean age of patients was 11.28 years. The mean serum ferritin level was 1820±749 µg/lit. Two hundred fifty five (59.75%) patients were male and 171 (40.25%) patients were female. The top five most prevalent causes of hospital admission were splenectomy (21.8%), infections (19.9%), congestive heart failure (19.0%), diabetes mellitus (13.4%), and Liver biopsy (11.5%). (P=0.0002)
Conclusion
Results of this study revealed that infections and complications due to iron overload are major causes of hospital admission in beta thalassemia major patients.
Keywords: Beta Thalassemia major, Hospitalization, Complication, Iran
Introduction
Beta thalassemia major (BTM) is one of the most prevalent hereditary diseases in Mediterranean region especially Iran. Thalassemia is found in some 60 countries with the highest prevalence in the Mediterranean region, parts of North and West Africa, the Middle East, the Indian subcontinent, southern Far East and southeastern Asia, together composing the so-called thalassemia belt. The gene frequency of β-thalassemia, however, is high and varies considerably from area to area, having its highest rate of more than 10% around the Caspian sea, and Persian Gulf. The prevalence of the disease in other areas is between 4% and 8%. In Isfahan, in the central part of Iran, the frequency rises again to about 8%. In the Fars Province, in southern Iran, the gene frequency is also high and reaches 8-10%[1] This disease affects several organs and systems of the body and causes various damages to these systems such as cardiac, reticuloendothelial, immunity and endocrine systems.
Regular transfusion therapy to maintain hemoglobin levels of at least 9 to 10 g per deciliter is required to improve growth and development and also to reduce bone deformities and hepatosplenomegaly due to extramedullary hematopoiesis[2, 3].
Without transfusion the death is inevitable during first two decades of life in BTM patients.
Various researches on BTM performed between 1979 and 1988, revealed a mortality of 11% in patients, with a median age of 13 years and 2 months[4]. The main cause of death was congestive heart failure. In 1994, effective use of deferoxamine against cardiac complications of iron overload was confirmed by two studies[5, 6]. In addition, these studies showed the severity of body iron overload as the main determinant of the clinical outcome. Recent studies from Italy further confirmed a beneficial outcome of chelation therapy on survival and the incidence of cardiac diseases[7, 8].
The combination of regular blood transfusions and chelation therapy has dramatically increased the life expectancy of thalassemics into 4th and 5th decades of life. On the other hand, frequent blood transfusion has also led to iron overload with many complications including endocrinopathies, behavioral and neurotic problems, growth failure, cardiovascular problems, liver disease, gonadal dysfunction and delayed puberty. Frequent blood transfusions can also lead to increased chances of transfusion related infections. Our aim of the study was to investigate the prevalence of causes of hospital admission in BTM patients during 2007 to 2010 in Shiraz, south west Iran.
Subjects and Methods
In this cross sectional study, 426 BTM patients were admitted to the Nemazee Hospital (the main University referral Hospital Center affiliated to Shiraz University of Medical Sciences in Fars Province, southern Iran) during 3 years period (January 2007 to January 2010).
After obtaining the approval by ethical committee of Shiraz University of Medical Sciences, a questionnaire was filled containing age, gender, hemoglobin level, frequency of blood transfusion, deferoxamine injection, cause of hospital admission and hospital course. The study was approved by the Medical Ethics Committee of Shiraz University of Medical Sciences for iron-chelation therapy.
The diagnosis of BTM was based on complete blood count and hemoglobin electrophoresis. All patients were on regular blood transfusion.
The data were evaluated and analyzed by chi-square test. P-value less than 0.05 was considered significant.
Findings
Two hundred fifty five (59.75%) patients were male and 171 (40.25%) were female. The mean age of patients was 11.28 years. The mean serum ferritin level was 1820±749 µg/lit. Splenectomy and sepsis were the most common causes of hospitalization (Table 1).
Table 1.
Causes of hospital admission in Beta thalassemia major patients from 2007-2010 in Iran
| No | Causes of admission | Number of patients |
|---|---|---|
| 1 | Splenectomy | 93(21.8%) |
| 2 | Infections | 85(19.9%) |
| 3 | Congestive heart failure | 81(19.0%) |
| 4 | Diabetes and DKA | 57(13.4%) |
| 5 | Liver biopsy | 49(11.5%) |
| 6 | Convulsion due to hypoparathyroidism | 17(4.0%) |
| 7 | Other types of surgery | 13(3.0%) |
| 8 | Severe anemia | 8(1.9%) |
| 9 | Upper GI bleeding | 5(1.2%) |
| 10 | Interferon therapy | 5(1.2%) |
| 11 | Aloimmunization | 5(1.2%) |
| 12 | Malignancy | 4(0.9%) |
| 13 | Acute renal failure | 2(0.4%) |
| 14 | Deep vein thrombosis | 2(0.4%) |
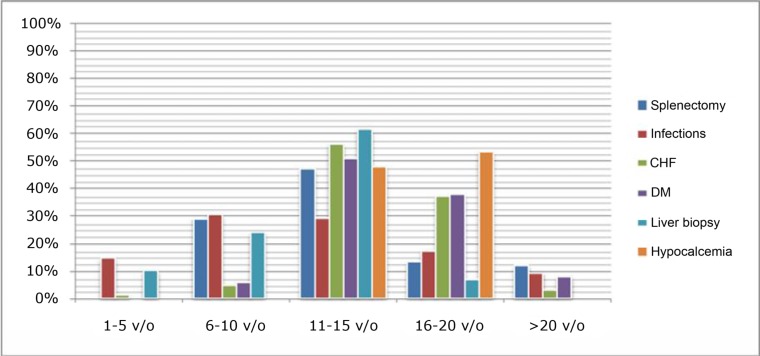
Splenectomy was performed in 93 BTM patients during these 3 years. Among 93 patients, 43 (46.2%) patients and 27 (29.0%) patients were in the age range of 11-15 years and 6-10 years, respectively. Eighty five BTM patients were admitted in hospital due to infection. The most prevalent infections among BTM patients were urinary tract infections, pneumonia, meningitis, liver abscesses and sepsis. Forty four (51.7%) patients who had been admitted to hospital due to infections had history of previous splenectomy.
The mean age of patients admitted with congestive heart failure (CHF) was 14.1 years. Among 81 patients admitted with CHF, 71 (87.6%) patients were in the second decade of life (Table 2). Diabetes mellitus (DM) or complications of DM like diabetic ketoacidosis were the causes of hospital admission in 57 patients. 50 (87.7%) patients were in the second decade of life (Table 2).
Table 2.
Age distribution of patients in 6 major causes of hospital admission in southern Iran
| Age (years) | 1-5 | 6-10 | 11-15 | 16-20 | >20 |
|---|---|---|---|---|---|
| Number of patients | 46(10.3%) | 89(20.8%) | 193(45.30%) | 77(18.0%) | 23(5.3%) |
| Splenectomy | 0(0.0%) | 27(29.0%) | 43(46.2%) | 12(12.9%) | 11(11.8%) |
| Infection | 12(14.1%) | 26(30.6%) | 25(29.4%) | 14(16.5%) | 8(9.4%) |
| Congestive heart failure | 1(1.2%) | 3(4.2%) | 43(55.3%) | 28(36.2%) | 2(2.7%) |
| Diabetes mellitus | 0(0.0%) | 3(5.3%) | 29(50.8%) | 21(36.8%) | 4(7.0%) |
| Liver biopsy | 5(10.2%) | 11(23.5%) | 30(61.2%) | 3(6.1%) | 0(0.0%) |
| Hypoparathyroidism | 0(0.0%) | 0.(0.0%0 | 8(47.0%) | 9(53.0%) | 0(0.0%) |
Forty nine patients were admitted for liver biopsy. Liver biopsy was done for BTM patients to evaluate the grade of liver hemochromatosis or pre bone marrow transplantation evaluations. Sixty one point two percent of patients were in the age range 11 to 15 years. Liver biopsy revealed 9 hepatitis C virus (HCV) positive and 6 (30.6%) hepatitis B virus (HBS) positive patients.
Seventy patients had been admitted due to convulsion. The cause of convulsion was hypocalcemia due to hyperparathyroidism. All patients were 11 to 20 years old. Calcium level was below 8.5 mg/dl in all patients.
Fig. 1 shows the differences in presentation of BTM complications in various age periods.
Fig. 1.
Prevalence of BTM complications in different age groups in southern Iran
Discussion
BTM patients have been admitted to hospital due to various reasons, but the age range of presentation of complications is different depending on the pathophisiology of the diseases (Fig 1).
Splenectomy was the major surgical and non-surgical cause of admission. 46.2% of patients admitted for splenectomy were 11 to 15 years old which is in agreement with previous study[9]. The main reasons for splenectomy were:
Increasing demand for blood transfusion
Thrombocytopenia
Frequent left upper quadrant pain due to splenomegaly
Sixty percent of patients admitted with infections were 6 to 15 years old. Splenectomy increases the risk of infections in BTM patients. Fifty four percent of patients who had been admitted due to infections had previous history of splenectomy.
Congestive heart failure is the main cause of death in BTM patients. Two major causes of congestive heart failure in BTM patients are severe anemia and iron deposition in myocardium. Multiple blood transfusions, red blood cells hemolysis and increased intestinal iron absorption are three major causes of iron deposition in tissues such as myocardium.
Cardiomyopathy arisen from severe anemia was the major cause of congestive heart failure in past decades but by improvement in management of anemia, now the major cause of CHF in BTM patients is iron overload and hemochromatosis[10].
Treatment of iron overload by iron chelators such as deferoxamine can delay the process of cardiomyopathy in BTM patients. There are some reports indicating that combined iron chelation therapy can reverse the process of heart failure and improve the cardiovascular function in BTM patients [11]. Ninety one point five percent of admissions due to congestive heart failure were at the age range of 11 to 20 years. The main (55.3%) age range of admission due to CHF was 11 to 15 years who showed poor compliance to Iron chelation therapy.
Eighty Seven point six of patients admitted for management of diabetes complications were 11 to 20 years old. Iron overload and iron deposition in endocrine glands cause endocrine abnormalities such as diabetes mellitus. Another factor that can increase the risk of diabetes in BTM patients is chronic hepatitis and hepatic fibrosis in BTM patients. Liver damage increases the resistance of cells to insulin. The amplified resistance of cells to insulin increases insulin blood level at first, but iron deposition in beta cells of pancreas and subsequent injury to the cells decreases the production of insulin by pancreas.
In the study performed by Li et al [12] on 81 thalassemic patients with mean age of 11.7 years, 74% of patients had grade III and IV liver hemochromatosis. Liver diseases are second cause of death in BTM patients. About 84% of patients admitted to our center for liver biopsy were at the age range of 6 to 15 years. From 49 liver biopsies, 18.3% were HCV positive and 12.2% HBV positive. It means that near one third of admitted patients were positive for blood borne infections.
Hypoparathyroidism is relatively common in BTM patients [13]. The prevalence is reported 4.5% to 7.5% in various studies. 4% of hospitalizations was due to hypocalcemia and Hypoparathyroidism. All Admitted patients were 5 to 15 years old. There are two major explanations for hypocalcemia in BTM patients:
Iron deposition in parathyroid glands impairs the secretion of parathyroid hormone (PTH) in the blood.
During the period of anemia, compensatory increased bone marrow volume replaces the bone and releases calcium in the blood but after blood transfusion and correction of the anemia, the process will be reversed and calcium will be restored in bone and cause hypocalcemia.
Malignancy can occur in patients with BTM and the incidence maybe more prevalent in patients with beta thalassemia intermedia compared to BTM; however, in case of leukocytosis detected by abnormal cells in peripheral blood or mass detection should be evaluated completely [14].
Conclusion
This study revealed that beside splenomegaly which is the result of red cell destruction, infections and complications of iron overload are the major causes of hospital admission in BTM patients. Regular iron chelating therapy and preventive immunization as well as antibiotic prophylaxis in splenectomized patients can decrease the incidence of complications leading to hospital admission.
Acknowledgment
This manuscript is relevant to the thesis of J. Hosseini and L. Shoja. We thank Shirin Parand at the Hematology Research Center, Shiraz University of Medical Sciences for editorial assistance of the manuscript.
Conflict of Interest
None
References
- 1.Haghshenas M, Zamani J. 1st ed. Shiraz: Shiraz University of Medical Sciences Publishing Center; 1997. Thalassemia. (In Persian) [Google Scholar]
- 2.Cunningham MJ, Macklin EA, Neufeld EJ, Cohen AR. Complications of β-thalassemia major in North America. Blood. 2004;104(1):34–9. doi: 10.1182/blood-2003-09-3167. [DOI] [PubMed] [Google Scholar]
- 3.Malik S, Syed S, Ahmed N. Complications in transfusion–dependent patients of ß-thalassemia major: A review. Pak J Med Sci. 2009;25(4):678–82. [Google Scholar]
- 4.Lin KH, Lin KS. Results of therapy for beta-thalassemia major. J Formos Med Assoc. 1992;91(2):126–30. [PubMed] [Google Scholar]
- 5.Brittenham GM, Griffith PM, Nienhuis AW, et al. Efficacy of deferoxamine in preventing complications of iron overload in patients with thalassemia major. N Engl J Med. 1994;331(9):567–73. doi: 10.1056/NEJM199409013310902. [DOI] [PubMed] [Google Scholar]
- 6.Olivieri NF, Nathan DG, MacMillan JH, et al. Survival in medically treated patients with homozygous ß-thalassemia. N Engl J Med. 1994;331(9):574–8. doi: 10.1056/NEJM199409013310903. [DOI] [PubMed] [Google Scholar]
- 7.Borgna-Pignatti C, Rugolotto S, De Stefano P, et al. Survival and complications in patients with thalassemia major treated with transfusion and deferoxamine. Haematologica. 2004;89(10):1187–93. [PubMed] [Google Scholar]
- 8.Borgna-Pignatti C, Cappellini MD, De Stefano P, et al. Survival and complications in thalassemia. Ann NY Acad Sci. 2005;1054:40–7. doi: 10.1196/annals.1345.006. [DOI] [PubMed] [Google Scholar]
- 9.Barzgar M, Peiravian F, Abedpour F, Karimi M. Causes for hospitalization and death in Iranian patients with β-thalassemia major. Pediatr Hematol Oncol. 2011;28(2):134–9. doi: 10.3109/08880018.2010.503336. [DOI] [PubMed] [Google Scholar]
- 10.Kyriacou K, Michaelides Y, Senkus R, et al. Ultrastructural Pathology. Ultrastruct Pathol. 2000;24(2):75–81. doi: 10.1080/01913120050118549. [DOI] [PubMed] [Google Scholar]
- 11.Tsironi M, Deftereos S, Andriopoulos P, et al. Reversal of heart failure in thalassemia major by combined chelation therapy: a case report. Eur J Haematol. 2005;74(1):84–5. doi: 10.1111/j.1600-0609.2004.00335.x. [DOI] [PubMed] [Google Scholar]
- 12.Li CK, Chik KW, Lam CW, et al. Liver disease in transfusion dependent thalassemia major. Arch Dis Childh. 2002;86(5):344–7. doi: 10.1136/adc.86.5.344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Angelopoulos NG, Goula A, Rombopoulos G, et al. Hypoparathyroidism in transfusion-dependent patients with β-thalassemia. J Bone Miner Metab. 2006;24(2):138–45. doi: 10.1007/s00774-005-0660-1. [DOI] [PubMed] [Google Scholar]
- 14.Karimi M, Giti R, Haghpanah S, et al. Malignancies in patients with beta-thalassemia major and beta-thalassemia intermedia: A multicenter study in Iran. Pediatr Blood Cancer. 2009;53(6):1064–7. doi: 10.1002/pbc.22144. [DOI] [PubMed] [Google Scholar]