Abstract
Objective
Malnutrition, overweight and obesity are major health concerns in modern societies and especially among children. Overweight and obesity affect children's current and future health. It is known that the prevalence of overweight differs by race, sex, and geographic location.
Methods
In a cross-sectional study 30092 Iranian children aged 7-18 years in six ethnic groups were selected by a cluster sampling. Prevalence of obesity and overweight and distribution of body mass index (BMI) by gender, age, and ethnicity were measured. Cutoff points of BMI for defining obesity and overweight were based on the Iranian, and IOTF standard values.
Findings
This study showed a significant ethnic difference in BMI. Prevalence of overweight and obesity among Iranian children was 9.27% and 3.22% respectively comparing international standards. The frequency of overweight and obesity was higher in boys.
Conclusion
This study showed a significant difference in BMI among different ethnic groups.
Keywords: BMI, Overweight, Obesity, School Children, Ethnicity
Introduction
Malnutrition, overweight and obesity are major health concerns in modern societies and especially among children[1]. There is substantial body of evidence that the prevalence of overweight has been significantly increased among children in recent years[2–5]. In the US, among persons aged 6-19 years, 31% were overweight or at risk for overweight[3]. In another survey in 2003, it was indicated that 27% of high-school students were overweight or at risk for overweight[6]. In National Health and Nutrition Examination Survey (NHANES), the prevalence of overweight among children aged 6-11 years was increased by about 11% from 1970-1974 till 1999-2000 in the US[7]. In a study in Iran, prevalence of overweight and obesity in children aged 6-18 years was 10.1% and 4.79% according to national cut-offs [8].
Some studies in different populations have assessed the prevalence of overweight among children [2–4, 8–10]. It is known that the prevalence of overweight differs by race, sex, and geographic location [7]. Few data on obesity prevalence, based on the optimum definition using body mass index (BMI), exist for children in developing countries[11].
Overweight or obese children are at risk for high blood pressure, dyslipidemia and diabetes type II [5, 12–15]. These children may eventually become overweight or obese adults [16–19]. Many studies have shown that schools can play an important role in improving lifestyle and children's behavior and subsequently prevent overweight and obesity [20–22].
Assessment of body composition can be performed by direct (e.g. estimation of lean body mass) or indirect (e.g. weight for height measurement) methods. The indirect methods are less precise but less expensive and simpler than the direct methods, especially for children [23].
Measuring students’ height, weight, and BMI in schools is an important approach to identify the prevalence of overweight and obesity and then try to reduce it [20, 21, 24, 25].
BMI has been recommended by many authors for evaluation of childhood obesity [26] and The American Academy of Pediatrics (AAP) recommend annual assessments of BMI as a strategy for preventing and combating childhood obesity [27].
Reference values for BMI have been measured in many developed countries such as America, Germany, and Britain [23, 28, 29]. International obesity task force (IOTF) and center of disease control and prevention (CDC) have defined reference values for different parts of the world [30, 31]. In Iran, these reference values have been measured in different studies [8, 32].
There are few studies in Iran about the prevalence of obesity among pre-school children[8, 33]. We conducted this study to assess body mass index of school children in all grades aged 7-18 years from different ethnicities in Iran and compare it with Iranian and IOTF standard values.
Subjects and Methods
In a cross-sectional study 30092 Iranian children aged 7-18 years in six ethnicities (i.e. Fars, Kurd, Lor, Baluch, Turk, and Arab) were assessed. 204 subjects without data on date of birth were excluded from the study, so the final data set used in the analysis consisted of 29988 children (14924 boys and 14964 girls) in six ethnicities. Sample size was measured using ISO 15535 Method[34].
Subjects were selected by multistage random cluster sampling from different parts of Iran. We selected a province as the representative of each ethnicity: Yazd (Fars), Sistan (Balouch), Kurdestan (Kurd), Lorestan (Lor), Zanjan (Turk), and Khoozestan (Arab). In each province persons who were native (those whose grandparents were from that ethnicity according to their parents’ testimony) were selected, non-native children and those with doubtful ethnicity were excluded from the study. We selected about 200 cases in each grade (from 1-12) from 12 primary, 8 intermediate and 10 high schools in different urban and rural parts of each province.
Then body weight, height and BMI were measured for all subjects. Measurements were made in winter and spring 2009 in a 6 month period.
Body weight was measured using a digital weight scale (Laica, Italy, accuracy: 100 grams) and height was measured by an anthropometer designed by researchers and validated by a pilot study (accuracy: 5 milimeters). Children wore light indoor clothing and no shoes during measurements.
Mean, standard deviation and key percentiles (5, 50, 85, and 95) were measured for weight, height and BMI. Prevalence of obesity (BMI>95th percentile) and overweight (BMI>85th percentile) was measured and compared among different Iranian ethnicities.
Cut-off points for defining obesity and overweight were based on the Iranian data from Hosseini et al[29] and international obesity task force (IOTF) standard values data[28]. Although according to Kelishadi et al[8] the standard values of CDC were closer to the measurements of our population, we used IOTF standard values to compare BMI of our children with an international standard.
Data was analyzed by SPSS (ver. 16). Independent samples t-test was used for comparison of means between two genders and one way ANOVA was used for the comparison of means among different ethnicities.
We obtained an informed consent from parents after explanation of the procedure.
Findings
A total of 29988 Iranian children (14924 boys and 14964 girls), 7-18 years old in six ethnicities including 4895 Fars, 4872 Kurd, 4908 Lor, 5389 Baluch, 5119 Turk, and 4705 Arab children entered the study.
Table 1 shows the mean and standard deviation for weight, height and BMI in all age groups and key percentiles (5, 50, 85 and 95) for BMI in two genders separately. BMI in 8 and 18 year-old boys was significantly higher than in girls (P=0.002, and P<0.001, respectively); and 12, 13, 14, 15, and 16 year-old girls had a higher BMI than boys (P=0.02 for 12, and P<0.001 for others).
Table 1.
Descriptive statistics for weight, height and body mass index in Iranian children
| Age | Sex | Weight( kg) | Height( m) | Body Mass Index | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SD*) | Mean (SD*) | Mean (SD*) | 5 th | 50 th | 85 th | 95th | |||||
| 7 | Boys | 22.25 (4.38) | 1.20 (0.06) | 15.22 (2.06) | 12.85 | 14.95 | 16.58 | 18.43 | |||
| Girls | 21.70 (4.97) | 1.19(0.06) | 15.06 (2.17) | 12.43 | 14.70 | 16.72 | 18.83 | ||||
| 8 | Boys | 25.49 (5.62) | 1.26(0.06) | 15.79 (2.43) | 13 | 15.34 | 17.57 | 20.84 | |||
| Girls | 24.53 (5.00) | 1.25(0.06) | 15.50 (2.40) | 12.61 | 15.08 | 17.55 | 19.89 | ||||
| 9 | Boys | 28.86 (6.52) | 1.32(0.06) | 16.24 (2.61) | 13.36 | 15.67 | 18.25 | 21.10 | |||
| Girls | 28.28 (6.50) | 1.31 (0.06) | 16.22 (2.77) | 13.14 | 15.43 | 18.89 | 21.67 | ||||
| 10 | Boys | 32.08 (7.54) | 1.37 (0.06) | 16.87 (3.05) | 13.60 | 16.15 | 19.73 | 23.08 | |||
| Girls | 31.59 (7.36) | 1.36 (0.06) | 16.72 (3.00) | 13.28 | 15.98 | 19.68 | 22.63 | ||||
| 11 | Boys | 36.36 (9.08) | 1.43 (0.07) | 17.38 (3.37) | 13.45 | 16.41 | 20.76 | 24.21 | |||
| Girls | 36.00 (9.32) | 1.43 (0.07) | 17.52 (3.29) | 13.55 | 16.76 | 20.93 | 24.02 | ||||
| 12 | Boys | 39.87 (10.16) | 1.47 (0.08) | 18.13 (3.62) | 14.07 | 17.21 | 21.63 | 25.25 | |||
| Girls | 41.66 (9.82) | 1.49 (0.07) | 18.49 (3.51) | 13.98 | 17.85 | 22 | 25.50 | ||||
| 13 | Boys | 45.39 (11.61) | 1.54 (0.09) | 18.74 (3.63) | 14.26 | 17.97 | 22.53 | 25.92 | |||
| Girls | 46.52 (10.93) | 1.53 (0.06) | 19.63 (3.890 | 14.82 | 18.90 | 23.46 | 27.13 | ||||
| 14 | Boys | 51.07 (13.50) | 1.61 (0.09) | 19.50 (4.00) | 14.72 | 18.58 | 23.12 | 27.70 | |||
| Girls | 50.25 (10.15) | 1.56 (0.05) | 20.45 (3.61) | 15.61 | 19.73 | 24.33 | 27.02 | ||||
| 15 | Boys | 55.23 (13.08) | 1.66 (0.08) | 19.86 (3.96) | 15.14 | 18.98 | 23.35 | 28.74 | |||
| Girls | 52.31 (10.03) | 1.57 (0.05) | 21.00 (3.69) | 16.05 | 20.28 | 24.97 | 27.98 | ||||
| 16 | Boys | 58.88 (12.70) | 1.69 (0.07) | 20.31 (3.74) | 15.88 | 19.51 | 23.56 | 28.20 | |||
| Girls | 53.41 (10.11) | 1.58 (0.05) | 21.32 (3.73) | 16.44 | 20.66 | 25.04 | 28.33 | ||||
| 17 | Boys | 62.91 (12.44) | 1.72 (0.06) | 21.11 (3.73) | 16.54 | 20.32 | 24.76 | 28.22 | |||
| Girls | 53.76 (9.85) | 1.58 (3.05) | 21.34 (3.57) | 16.65 | 20.74 | 25.06 | 28.03 | ||||
| 18 | Boys | 64.53 (13.10) | 1.72 (0.06) | 21.60 (3.98) | 16.85 | 20.74 | 25.10 | 29.35 | |||
| Girls | 52.69 (9.69) | 1.58 (0.05) | 21.00 (3.54) | 16.42 | 20.35 | 24.24 | 28.11 | ||||
SD: standard deviation
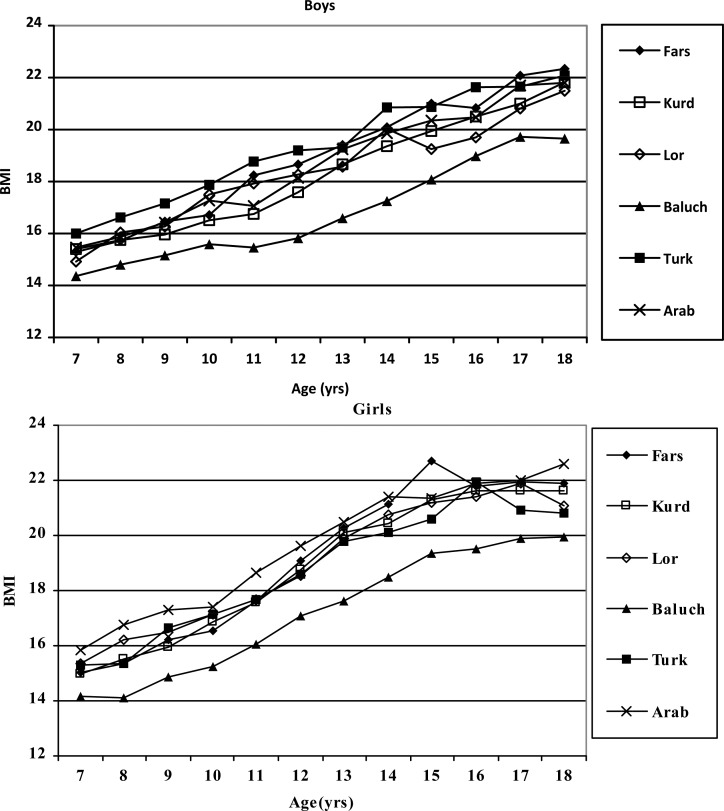
Figure 1 shows the gender- and age-specific mean BMI among school children of six ethnicities. There was a significant BMI difference in boys and girls in different ethnicities (P<0.001). Baluch boys and girls had the lowest BMI in all age groups, but the highest BMI was seen in different ethnicities for different ages (e.g. Arab girls had the highest BMI in 8, 9, 12, 13, and 16 year olds, and the highest BMI in 7 and 11 year olds was observed in Turk boys).
Fig. 1.
Gender- and age-specific mean BMI among school children of six ethnic groups
Considering IOTF, 2774 (9.27%) of Iranian children were overweight (10.49% of boys and 8.07% of girls), and 965 (3.22%) of them were obese (3.75% of boys and 2.71% of girls). But if we consider national standard (1999), these prevalence rates will be much higher. According to this standard 3787 (12.67%) of Iranian children were overweight (11.82% of boys and 13.50% of girls), and 3128 (10.47%) of them (12.06% of boys and 8.9% of girls) were obese. Tables 2 and 3 show the prevalence of overweight and obese boys and girls in different ethnicities, respectively.
Table 2.
Prevalence of overweight and obesity among boys of six ethnic groups
| Age(year) | Ethnicities | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fars | Kurd | Lor | Baluch | Turk | Arab | |||||||
| IRN* | IOTF* | IRN | IOTF | IRN | IOTF | IRN | IOTF | IRN | IOTF | IRN | IOTF | |
| 7 (OW** ) | 12.1 | 3.0 | 9.9 | 4.4 | 7.9 | 4.8 | 3.4 | 1.0 | 19.6 | 6.7 | 9.4 | 3.9 |
| 7 (Ob**) | 4.3 | 2.1 | 5.4 | 1.5 | 7.9 | 3.5 | 1.7 | 0.7 | 9.1 | 3.5 | 5.9 | 2.5 |
| 8 (OW ) | 9.7 | 9.7 | 17.7 | 4.3 | 12.9 | 12.9 | 9.0 | 5.4 | 15.9 | 9.9 | 13.7 | 6.8 |
| 8 (Ob) | 12.8 | 3.1 | 6.2 | 1.9 | 18.8 | 5.9 | 5.4 | 0 | 16.4 | 6.9 | 10.2 | 3.9 |
| 9 (OW ) | 10.9 | 7.8 | 16.3 | 5.8 | 11.8 | 7.4 | 12.3 | 4.7 | 17.1 | 16.2 | 12.6 | 10.5 |
| 9 (Ob) | 13.0 | 4.7 | 6.8 | 1.1 | 11.8 | 3.9 | 5.2 | .5 | 22.2 | 3.7 | 13.7 | 2.1 |
| 10 (OW ) | 7.1 | 13.6 | 9.9 | 7.3 | 14.6 | 17 | 6.7 | 2.9 | 17.7 | 17.7 | 8.8 | 11.0 |
| 10(Ob) | 16.2 | 1.9 | 10.9 | 2.6 | 22.2 | 4.1 | 4.6 | 1.3 | 23.6 | 4.5 | 18.2 | 6.1 |
| 11 (ow ) | 13.4 | 16.0 | 12.1 | 7.1 | 14.4 | 17.8 | 4.8 | 3.9 | 17.6 | 20.9 | 12.9 | 9.1 |
| 11(Ob) | 23.5 | 6.7 | 9.1 | 2.0 | 22.5 | 3.8 | 4.8 | 0.5 | 26.4 | 5.5 | 11.5 | 2.4 |
| 12 (OW ) | 11.6 | 16.9 | 8.6 | 7.2 | 10.1 | 13.2 | 4.8 | 0.8 | 17.8 | 18.8 | 12.1 | 11.7 |
| 12(Ob) | 20.0 | 4.4 | 9.9 | 2.6 | 17.6 | 4.8 | 2.4 | 1.6 | 21.6 | 5.3 | 15.0 | 4.4 |
| 13 (OW ) | 12.1 | 21.1 | 11.0 | 11.9 | 10.6 | 13.7 | 6.0 | 5.3 | 13.8 | 12.8 | 14.3 | 16.5 |
| 13(Ob) | 21.5 | 4.9 | 13.7 | 2.6 | 12.8 | 4.0 | 4.7 | 1.3 | 14.3 | 4.9 | 17.7 | 3.8 |
| 14 (OW ) | 11.3 | 15.7 | 14.1 | 9.0 | 15.3 | 20.8 | 5.8 | 5.4 | 16.8 | 15.8 | 14.0 | 15.5 |
| 14(Ob) | 17.4 | 6.5 | 8.5 | 4.5 | 15.3 | 4.4 | 4.5 | 1.3 | 17.9 | 8.2 | 14.7 | 5.4 |
| 15 (OW ) | 15.8 | 14.7 | 10.2 | 10.7 | 4.7 | 6.1 | 3.8 | 5.0 | 16.2 | 13.8 | 9.4 | 11.2 |
| 15(Ob) | 15.8 | 9.8 | 7.0 | 2.8 | 6.6 | 3.8 | 5.0 | 2.9 | 12.9 | 6.2 | 11.6 | 6.7 |
| 16 (OW ) | 11.5 | 11 | 10.6 | 8.7 | 4.8 | 6.9 | 7.5 | 7.9 | 16.3 | 13.8 | 10.8 | 5.9 |
| 16(Ob) | 11.5 | 5.0 | 6.8 | 2.4 | 6.9 | 1.6 | 5.0 | 1.7 | 13.3 | 7.7 | 5.9 | 3.9 |
| 17 (OW ) | 9.5 | 13.1 | 11.5 | 12.5 | 12.2 | 7.9 | 5.9 | 7.4 | 17 | 18.3 | 13.9 | 10.2 |
| 17(Ob) | 17.6 | 9.0 | 7.3 | 1.6 | 6.1 | 1.7 | 7.8 | 3.4 | 2.6 | 3.0 | 10.2 | 4.6 |
| 18 (OW ) | 18.5 | 13.9 | 11.9 | 11.1 | 14.8 | 7.5 | 5.1 | 5.2 | 14 | 11.4 | 14.0 | 13.2 |
| 18(Ob) | 15.1 | 7.4 | 11.1 | 2.5 | 8.0 | 3.1 | 5.1 | 0 | 12.8 | 5.1 | 12.1 | 5.2 |
Table 3.
Prevalence of overweight and obesity among girls of six ethnic groups
| Age(year) | Ethnicitis | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fars | Kurd | Lor | Baluch | Turk | Arab | |||||||
| IRN* | IOTF* | IRN | IOTF | IRN | IOTF | IRN | IOTF | IRN | IOTF | IRN | IOTF | |
| 7 (OW** ) | 13.2 | 2.9 | 9.5 | 5 | 18.9 | 8 | 6.4 | 2.8 | 12.4 | 7.1 | 15.7 | 7.8 |
| 7 (Ob**) | 4.4 | 2.5 | 5.5 | 2.5 | 7.1 | 2.8 | 2.8 | .4 | 7.1 | 2.1 | 9.3 | 4.4 |
| 8 (OW ) | 10.8 | 7.4 | 13.4 | 10.1 | 18.7 | 13.9 | 5 | 1.9 | 12.9 | 4.9 | 16.3 | 10.4 |
| 8 (Ob) | 7.8 | 2 | 8.4 | .6 | 13.4 | 1.9 | 2.3 | .8 | 4.9 | 1.2 | 17.3 | 9.9 |
| 9 (OW ) | 15.1 | 10.7 | 14.2 | 9.6 | 13.3 | 11.8 | 9.7 | 3.1 | 20.3 | 12.1 | 19.9 | 17.5 |
| 9 (Ob) | 9.8 | 2.4 | 8.8 | 1.3 | 12.8 | 3.6 | 2.6 | .4 | 12.9 | 4.7 | 20.4 | 7.3 |
| 10 (OW ) | 15.7 | 12.2 | 17.2 | 11.6 | 15.1 | 12.5 | 5.7 | 3.9 | 15.2 | 14.3 | 16.6 | 12.2 |
| 10(Ob) | 10.7 | 2.5 | 12.6 | 2.5 | 14.1 | 4.7 | 3.9 | .4 | 15.7 | 3 | 15.6 | 4.4 |
| 11 (ow ) | 14.9 | 15.3 | 15.3 | 12.6 | 14.9 | 12.3 | 9 | 5.4 | 15.6 | 15.1 | 20.3 | 19.3 |
| 11(Ob) | 15.3 | 3.3 | 12.1 | 4.2 | 11.3 | 3.1 | 4.5 | .9 | 13.2 | 2.4 | 18.9 | 4.7 |
| 12 (OW ) | 16.9 | 17.5 | 17 | 14.2 | 17.2 | 11.6 | 7.7 | 6 | 16.1 | 12.9 | 19.7 | 19.7 |
| 12(Ob) | 16.9 | 5.4 | 15.3 | 4 | 11.9 | 2.6 | 6.9 | 1.7 | 11.3 | 1.6 | 23.5 | 6.1 |
| 13 (OW ) | 19.9 | 21.4 | 16.7 | 16.2 | 15.7 | 18.2 | 8.7 | 6 | 16.6 | 13.3 | 18.4 | 17 |
| 13(Ob) | 17.4 | 6.5 | 16.2 | 4.9 | 15.3 | 3.8 | 3.2 | 4 | 10.4 | 3.8 | 17 | 7.5 |
| 14 (OW ) | 19.1 | 19.5 | 15.5 | 15.9 | 19.5 | 20.5 | 9.6 | 8.2 | 16.8 | 14.4 | 20 | 20.7 |
| 14(Ob) | 14.2 | 4.1 | 7.1 | 3.5 | 10 | 3.5 | 1.4 | .5 | 5.8 | 1.4 | 12.4 | 4 |
| 15 (OW ) | 16.2 | 23.2 | 14.3 | 18.8 | 15.8 | 22.1 | 9.3 | 9.7 | 12.6 | 14.1 | 16.9 | 21.5 |
| 15(Ob) | 18.7 | 9.6 | 8.5 | 2.7 | 8.4 | .5 | 2.4 | 1.2 | 4.5 | 2 | 6.2 | 0 |
| 16 (OW ) | 13.2 | 17.6 | 9.8 | 13 | 12.1 | 16.5 | 4.3 | 5.5 | 11.5 | 16.4 | 14.3 | 20.1 |
| 16(Ob) | 7 | 4.8 | 6.5 | 5.4 | 3.4 | 1.9 | 1.6 | 1.6 | 6.6 | 4.9 | 6.1 | 4.1 |
| 17 (OW ) | 11.8 | 14.9 | 8.2 | 13.1 | 11.4 | 16.9 | 6.1 | 8.2 | 7.4 | 10.4 | 14.9 | 19.6 |
| 17(Ob) | 3.6 | 3.1 | 4.1 | 3.3 | 3.9 | 3.9 | 1.6 | 1.6 | 2.6 | 2.2 | 3.1 | 3.1 |
| 18 (OW ) | 10.2 | 13.2 | 5.8 | 10.3 | 6.5 | 7.8 | 5.1 | 5.6 | 3.8 | 7 | 17.4 | 16.7 |
| 18(Ob) | 3.4 | 2.6 | 4.7 | 3.8 | .9 | 0 | 1 | 1.2 | 1 | 1.3 | 8.7 | 11.1 |
Discussion
Child obesity is an epidemic with serious social, economic, and health consequences having the potential to continue into adulthood[25], so identification of children who are overweight or obese based on different age, gender, and ethnicity and intervention to prevent the development of obesity-related conditions is important.
Parents' occupation, education and urbanization are major risk factors for childhood obesity in developing countries [1, 11]. It is known that the prevalence of overweight differs by race, sex, and geographic location [7].
This is the first study for comparing BMI among different ethnicities from a large national sample in Iran. Although Kelishani et al have assessed the prevalence of overweight and obesity in a large national sample, they haven't compared their results among different ethnicities [8].
In our study, centiles of BMI were higher than the study of Hosseini et al in all age groups [32], and they were much closer to the international standards which shows a tendency to increase BMI among Iranian children during the last decade.
Centiles of BMI were also higher than those of Vietnamese and Chinese children [1, 35]. Prevalence of overweight and obesity was higher than that of Chinese children [35].
We found a prevalence of 12.67% and 10.47% for overweight and obesity according to national cut-off points, which was higher than the results of Kelishadi et al [8].
We found a significant difference between various ethnicities within Iran which was consistent with last studies [35, 36]. In our study, mean BMI in Baluch children was lower than in other ethnicities, which may be due to ethnicity or geographical area.
It seems that Iran has experienced a rapid “nutrition transition” during the last decade, with urbanization and decreases in physical activity, and increases in calorie and fat intake.
Our study had some limitations. We used BMI which is an indirect measure of overweight and obesity. We couldn't measure the percentiles of BMI by Lamda-Mu-Sigma (LMS) method, because the software was not available to us. There were some children from a hybrid ethnic group and we could not exclude all of them. Some observed differences are probably due to geographical difference which was not considered in this study. These data can be used for planning nutritional strategies for children and as basic information for later studies.
Conclusion
It is concluded from this study that BMI has increased in children of our population and prevalence of overweight and obesity has increased during last years.
Acknowledgment
This work was supported by Iranian Ministry of Health and Shahid Sadoughi University of Medical Sciences. The study was approved by ethics committee of Shahid Sadoughi University of Medical Sciences.
We thank all of the students who participated in this study and all managers and employees of the schools. In addition, we thank Mohammad Javad Zare who helped us in designing the study and we are grateful to Hesam Akbari, Abbas Hosseini, Somayeh Montazeri, Maliheh Dehghan, and Mrs. Sadeghian who helped us in this study.
Conflict of Interest
None
References
- 1.Aurelius G, Khanh NC, Truc DB, et al. Height, weight, and body mass index (BMI) of Vietnamese (Hanoi) schoolchildren aged 7–11 years related to parents' occupation and education. J Trop Pediatr. 1996;42(1):21–6. doi: 10.1093/tropej/42.1.21. [DOI] [PubMed] [Google Scholar]
- 2.Molaison EF, Kolbo JR, Meyer MK, et al. Prevalence of overweight among elementary and middle school students in Mississippi compared with prevalence data from the youth risk behavior surveillance system. Prev Chronic Dis. 2006;3(3):A84. [PMC free article] [PubMed] [Google Scholar]
- 3.Hedley A, Ogden C, Johnson C, et al. Prevalence of overweight and obesity among US children, adolescents, and adults,1999–2002. JAMA. 2004;291(23):2847–50. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- 4.Ogden CL, Carroll MD, Curtin LR, et al. Prevalence of overweight and obesity in the United States,1999–2004. JAMA. 2006;295(13):1549–55. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention (CDC) Assessment of Body Mass Index Screening of Elementary School Children. MMWR Morb Mortal Wkly Rep. 2009;58(17):460–3. [PubMed] [Google Scholar]
- 6.Grunbaum JA, Kann L, Kinchen S, et al. Youth risk behavior surveillance-United States, 2003. MMWR Surveill Summ. 2004;53(2):1–96. [PubMed] [Google Scholar]
- 7.Ogden CL, Flegal KM, Carroll MD, Johnson CL. Prevalence and trends in overweight among US children and adolescents,1999–2000. JAMA. 2002;288(14):1728–32. doi: 10.1001/jama.288.14.1728. [DOI] [PubMed] [Google Scholar]
- 8.Kelishadi R, Ardalan G, Gheiratmand R, et al. Caspian Study Group. Thinness, overweight and obesity in a national sample of Iranian children and adolescents: CASPIAN Study. Child Care Health Dev. 2008;34(1):44–54. doi: 10.1111/j.1365-2214.2007.00744.x. [DOI] [PubMed] [Google Scholar]
- 9.Nelson JA, Chiasson MA, Ford V. Childhood overweight in a New York City WIC population. Am J Public Health. 2004;94(3):458–62. doi: 10.2105/ajph.94.3.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hoelscher DM, Day RS, Lee ES, et al. Measuring the prevalence of overweight in Texas schoolchildren. Am J Public Health. 2004;94(6):1002–8. doi: 10.2105/ajph.94.6.1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Martorell R, Khan L, Hughes ML, Grummer-Strawn LM. Overweight and obesity in pre-school children from developing countries. Int J Obes. 2000;24(8):959–67. doi: 10.1038/sj.ijo.0801264. [DOI] [PubMed] [Google Scholar]
- 12.Freedman DS, Dietz WH, Srinivasan SR, Berenson GS. The relation of overweight to cardiovascular risk factors among children and adolescents: the Bogalusa Heart Study. Pediatrics. 1999;103(6):1175–82. doi: 10.1542/peds.103.6.1175. [DOI] [PubMed] [Google Scholar]
- 13.Freedman DS. Clustering of coronary heart disease risk factors among obese children. J Pediatr Endocrinol Metab. 2002;15(8):1099–108. doi: 10.1515/JPEM.2002.15.8.1099. [DOI] [PubMed] [Google Scholar]
- 14.Freedman DS, Dietz WH, Tang R, et al. The relation of obesity throughout life to carotid intima-media thickness in adulthood: the Bogalusa Heart Study. Int J Obes Relat Metab Disord. 2004;28(1):159–66. doi: 10.1038/sj.ijo.0802515. [DOI] [PubMed] [Google Scholar]
- 15.Odegaard AO, Koh WP, Vazquez G, et al. BMI and diabetes risk in Singaporean Chinese. Diabetes Care. 2009;32(6):1104–6. doi: 10.2337/dc08-1674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Krebs NF, Jacobson MS. Prevention of pediatric overweight and obesity. Pediatrics. 2003;112(2):424–30. doi: 10.1542/peds.112.2.424. [DOI] [PubMed] [Google Scholar]
- 17.Whitaker RC, Wright JA, Pepe MS, et al. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337(13):869–73. doi: 10.1056/NEJM199709253371301. [DOI] [PubMed] [Google Scholar]
- 18.Guo SS, Huang C, Maynard LM, et al. Body mass index during childhood, adolescence, and young adulthood in relation to adult overweight and adiposity: the Fels Longitudinal Study. Int J Obes Relat Metab Disord. 2000;24(12):1628–35. doi: 10.1038/sj.ijo.0801461. [DOI] [PubMed] [Google Scholar]
- 19.Freedman DS, Khan LK, Serdula MK, et al. Inter-relationships among childhood BMI, childhood height, and adult obesity: the Bogalusa Heart Study. Int J Obes Relat Metab Disord. 2004;28(1):10–6. doi: 10.1038/sj.ijo.0802544. [DOI] [PubMed] [Google Scholar]
- 20.Nihiser AJ, Lee SM, Wechsler H, et al. BMI Measurement in Schools. Pediatrics. 2009;124(Supple 1):S89–S97. doi: 10.1542/peds.2008-3586L. [DOI] [PubMed] [Google Scholar]
- 21.Gortmaker S, Peterson K, Wiecha J, et al. Reducing obesity via a school-based interdisciplinary intervention among youth: Planet Health. Arch Pediatr Adolesc Med. 1999;153(4):409–18. doi: 10.1001/archpedi.153.4.409. [DOI] [PubMed] [Google Scholar]
- 22.Kelishadi R, Ardalan G, Gheiratmand R, et al. CASPIAN Study Group. Association of physical activity and dietary behaviours in relation to the body mass index in a national sample of Iranian children and adolescents: CASPIAN Study. Bull World Health Organ. 2007;85(1):19–26. doi: 10.2471/BLT.06.030783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hammer LD, Kraemer HC, Wilson DM, et al. Standardized percentile curves of body-mass index for children and adolescents. Am J Dis Child. 1991;145(3):259–63. doi: 10.1001/archpedi.1991.02160030027015. [DOI] [PubMed] [Google Scholar]
- 24.Ikeda JP, Crawford PB, Woodward-Lopez G. BMI screening in schools: helpful or harmful. Health Educ Res. 2006;21(6):761–9. doi: 10.1093/her/cyl144. [DOI] [PubMed] [Google Scholar]
- 25.Johnson A, Ziolkowski GA. School-based body mass index screening program. Nutr Today. 2006;41(6):274–9. [Google Scholar]
- 26.Himes JH, Dietz WH. Guidelines for overweight in adolescent preventive services: recommenddations from an expert committee. Am J Clin Nutr. 1994;59(2):307–16. doi: 10.1093/ajcn/59.2.307. [DOI] [PubMed] [Google Scholar]
- 27.Krebs NF, Jacobson MS. American Academy of Pediatrics Committee on Nutrition Prevention of pediatric overweight and obesity. Pediatrics. 2003;112(2):424–30. doi: 10.1542/peds.112.2.424. [DOI] [PubMed] [Google Scholar]
- 28.Schaefer F, Georgi M, Wuehl E, et al. Body mass index and percentage fat mass in healthy German schoolchildren and adolescents. Int J Obes. 1998;22(5):461–9. doi: 10.1038/sj.ijo.0800608. [DOI] [PubMed] [Google Scholar]
- 29.Cole TJ, Freeman JV, Preece MA. Body mass index reference curves for the UK. Arch Dis Child. 1995;73(1):25–29. doi: 10.1136/adc.73.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cole TJ, Bellizzi MC, Flegal KM, et al. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320(7244):1240–5. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM. CDC growth charts: United States. Advanced Data. 2000;314:1–27. [PubMed] [Google Scholar]
- 32.Hosseini M, Carpenter RG, Mohammad K, Jones ME. Standardized percentile curves of body mass index of Iranian children compared to the US population. Int J Obes. 1999;23(8):783–6. doi: 10.1038/sj.ijo.0800924. [DOI] [PubMed] [Google Scholar]
- 33.Ziaoddini H, Kelishadi R, Kamsari F, et al. First nationwide survey of prevalence of weight disorders in Iranian children at school entry. World J Pediatr. 2010;16(3):223–7. doi: 10.1007/s12519-010-0206-z. [DOI] [PubMed] [Google Scholar]
- 34.International Standard Organization, ISO 15535: 2006. Switzerland, Geneva: 2006. General requirements for establishing anthropometric databases. [Google Scholar]
- 35.Yan WL, Zheng YJ, Wu J, et al. Ethnic differences in body mass index and prevalence of obesity in school children of Urumqi City, Xinjiang, China. Biomed Environ Sci. 2006;19(6):469–73. [PubMed] [Google Scholar]
- 36.Dorosty AR, Siassi F, Reilly JJ. Obesity in Iranian children. Arch Dis Child. 2002;87(5):388–91. doi: 10.1136/adc.87.5.388. [DOI] [PMC free article] [PubMed] [Google Scholar]