Abstract
Background
Ferrous sulfate drops are routinely used in Iran in infants older than 6 months of age. Effect of ferrous sulfate drops in preventive or therapeutic doses on gastrointestinal mucosa of infants is not studied as yet. Upper gastrointestinal complications due to acute iron poisoning are well known in this age group. In this article, we reviewed published articles on iron deposition in upper gastro-intestinal tract and also introduce clinical, endoscopic and histological findings in three cases with iron deposition in duodenal mucosa.
Cases Presentation
We encountered three cases of iron deposition in duodenal mucosa among about 8000 biopsies during a 10 year period which is a very low incidence despite routine use of iron supplement in children above 6 months of age in this country. One of our cases suffered from steatorrhea and another from failure to thrive, which raises concern about effects of iron deposition in small intestine.
Conclusion
The clinical significance and effects of iron deposition in pediatric age group is yet to be elucidated. Iron deposition as a solitary finding is not reported in duodenal biopsies of infants as yet. Since iron supplement is widely used in this age group, it is justified to consider its deposition and possible effects on absorption.
Keywords: Iron, Gastrointestinal Tract, Ferrous Sulfate, Malabsorption, Duodenal Diseases, Children
Introduction
Iron, the most abundant trace mineral, is used mainly in synthesis of hemoglobin and myoglobin. In a normal term infant there is little change in total body iron and little need for exogenous iron before 4 months of age, but after that, iron reserves become marginal, and unless exogenous sources of iron are provided, the infant becomes progressively at risk for anemia[1]. Iron needs can be met by supplementation (as ferrous sulfate drops) or by iron containing complementary foods[1]. Ferrous sulfate drops are routinely used in this country in infants above 6 months of age. Effect of ferrous sulfate drops in preventive or therapeutic doses on gastrointestinal mucosa of infants is not studied as yet. Upper gastrointestinal complications due to acute iron poisoning are well known in this age group[2,3].
Upper gastrointestinal injury from iron tablets at therapeutic doses is studied in adults in a few articles[4,5,6]. Iron deposition without evident erosive mucosal injury is also seen in a small proportion (14%) of biopsies in Abraham's article[5]. There is strong evidence that the toxic effects of iron are influenced by the type of iron preparation ingested. In rabbits and dogs fed aqueous solutions of iron, lethal serum levels of iron were obtained without demonstrable erosion or ulceration of the gastrointestinal tract in autopsy[7]. Eckstein and Symons stated that liquid preparations should be used in patients with preexisting ulcers or gastrointestinal dysmotility [8]. So we suggest that mucosal injury from ferrous sulfate drops used in infants is negligible. We encountered 3 cases with iron deposition in duodenal biopsies in tip of villi in a 10 year period in almost 8000 duodenal biopsies in our hospital which is a referral children's hospital.
The aim of this article is to describe clinical, endoscopic and histological findings in these cases and in addition we give a rough estimate of the prevalence of iron deposition in duodenal biopsies of children who are on routine supplementation of iron drops. To the best of our knowledge, isolated iron deposition in duodenal biopsy has not been reported as yet in this age group.
Cases Presentation
Duodenal biopsies taken by endoscopy in a ten year period (1999-2008) in Children's Medical Center affiliated to Tehran University of Medical Sciences were reviewed. Near 8000 biopsies were taken in this period. Only three cases showed iron deposition in duodenal lamina propria in tip of villi which was proved by Perl's staining (Fig. 1 and 2). Clinical data and endoscopic findings were retrieved from patients’ files.
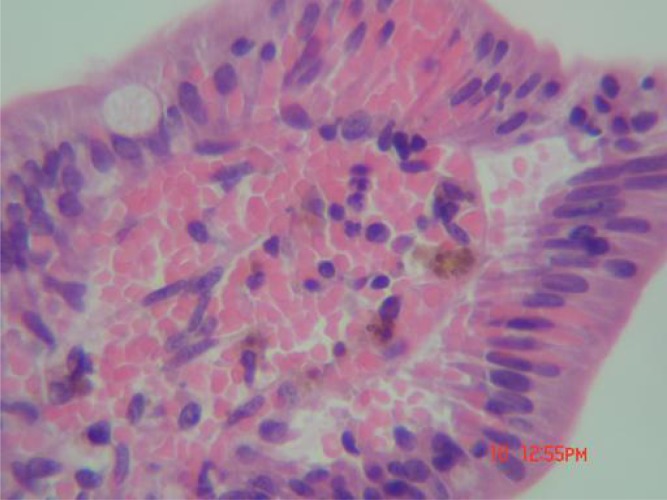
Fig. 1.
Duodenal mucosa with deposition of brown pigment in tip of villi, mainly in the macrophages (Hematoxylin Eosin stain, ×400)
Fig. 2.
Same field as Fig. 1. Brown pigments proved to be iron granules by iron specific staining (Perl's staining, ×400)
Out of almost 8000 duodenal biopsies only three cases show iron deposition in duodenal mucosa.
Case 1: This 22 month-old boy suffered from steatorrhea and received routine prophylactic doses of ferrous sulfate drops.
Case 2: This one year old boy was referred with failure to thrive (FTT). He was also a known case of minor thalassemia. Failure to thrive was later attributed to constitutional delay. He was taking therapeutic doses of iron since one month before endoscopic examination.
Case 3: This 21 month-old girl suffered from gastro-esophageal reflux disease (GERD). Final diagnosis of this case was renal tubular acidosis. She received routine prophylactic doses of ferrous sulfate drops.
Histological features: All three patients had normal mucosal patterns on endoscopic examination of duodenum. The one with steatorrhea revealed mild gastritis in gastric biopsy and mild duodenitis with an increase of eosinophils (2-17/HPF) in duodenal biopsy which may be attributable to food allergy in this case. The other two showed mild esophagitis with presence of few eosinophils in one and follicular esophagitis in the other (no gastric biopsies were taken). Both revealed mild to moderate villous atrophy and mild chronic duodenitis in duodenal biopsies. Iron deposition was not seen in either esophageal or gastric biopsies. No significant erosion and no ulceration were seen, but some degree of mucosal congestion was evident in duodenal biopsies of all cases. Iron deposition was seen mainly in mucosal macrophages as brown pigment (Fig. 1); few granules were seen freely in lamina propria. By special staining for iron (Perl's staining) brown granules were proved to be iron (Fig. 2).
Discussion
Upper gastrointestinal complications due to acuteiron poisoning are well known in pediatric age group[2,3], but doses of iron prescribed as medication is different from doses leading to poisoning, and also liquid form is used in this age, which is believed to be less toxic and even in adults changing tablets to liquid form of iron will decrease upper GI complications[5,7,8].
Our hospital is a referral center with many duodenal biopsies per year, but in the last 10 years we found iron deposition in only three duodenal biopsies which showed iron deposits mainly in macrophages in lamina propria with no associated mucosal injuries.
According to the fact that all children older than 6 months in our country take ferrous sulfate drops, rough incidence of iron deposition in duodenal biopsies is very low (3 in 8000: 0.00037). If we relate this phenomenon to oral iron intake, why only three in 8000 duodenal biopsies had iron deposition?
In our cases, only one took therapeutic doses of iron and the other two used it as in routine infant care programs. We think there should be another reason which resulted in iron deposition in these cases. Absorption of iron is related to other ingested materials taken simultaneously, such as iron chelators, ascorbic acid, etc. Spelman showed that in lemurs vitamin C and not tannin (a plant product which is an iron chelator) could increase iron absorption in gastrointestinal mucosa and even could lead to siderosis. She suggested that immediate correction of captive diets in lemurs may limit siderosis[9]. Whether deposition of iron in our cases is related to other ingested materials in these cases is yet to be elucidated.
Iron deposition in gastrointestinal tract can also be a manifestation of systemic hemochromatosis[10]. Iron deposition is mainly seen in gastric mucosa of these patients, while in gastric biopsy of one of our cases no gastric iron deposition was detected. Also hemochromatosis is very rare in this country (personal experience) and our cases lacked other clinical features of hemochromatosis. So we do not suppose that our cases belong to this category, however, no genetic study was performed in our cases.
Although we could not explain the exact etiology of iron deposition in these three infants, clinical manifestation (malabsorption) in two of them is worth attention. Whether iron deposition is the cause of steatorrhea and failure to thrive in these infants or has some contributory effect should yet be elucidated. We suppose pediatric gastroenterologists should take this fact into account and institute some measures to reduce iron content in gastrointestinal tract.
Conclusion
In summary, although iron deposition in duodenal biopsies is rare in infants and is not, as far as we know, reported as an isolated finding in this age group, it is worth attention in study of gastrointestinal complaints of infants.
References
- 1.Krebs NF, Primak LE. Pediatric nutrition and nutritional disorders. In: Kliegman, Marcdante, Jenson, Behrman, editors. Nelson Essentials of Pediatrics. Philadelphia: Saunders-Elsevier; 2006. pp. 154–5. [Google Scholar]
- 2.Banner W, Tong TG. Iron poisoning. Pediatric Clin North Am. 1986;33(2):393–409. doi: 10.1016/s0031-3955(16)35010-6. [DOI] [PubMed] [Google Scholar]
- 3.Mc Guigan MA. Acute iron poisoning. Pediatr Ann. 1996;25(1):33–8. doi: 10.3928/0090-4481-19960101-08. [DOI] [PubMed] [Google Scholar]
- 4.Kaye P, Abdulla K, Wood J, et al. Iron induced mucosal pathology of the upper gastrointestinal tract: a common finding in patients on oral iron therapy. Histopathology. 2008;53(3):311–7. doi: 10.1111/j.1365-2559.2008.03081.x. [DOI] [PubMed] [Google Scholar]
- 5.Abraham SC, Yardley JH, Wu T. The erosive injury to the upper gastrointestinal tract in patients receiving iron medication, an under recognized entity. Am J Surg Path. 1999;23(10):1241–5. doi: 10.1097/00000478-199910000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Hongxiu J, Yardley JH. Iron medication associated gastric mucosal injury. Arch Pathol Lab Med. 2004;128(7):821–2. doi: 10.5858/2004-128-821-IMGMI. [DOI] [PubMed] [Google Scholar]
- 7.Reissmann KR, Coleman TJ, Budai BS, Moriarty LR. Acute intestinal iron intoxication. I. Iron absorption, serum iron, and autopsy findings. Blood. 1955;10:35–45. [PubMed] [Google Scholar]
- 8.Eckstein RP, Symons P. Iron tablets cause histopathologically distinctive lesions in mucosal biopsies of the stomach and esophagus. Pathology. 1996;28:142–5. doi: 10.1080/00313029600169763. [DOI] [PubMed] [Google Scholar]
- 9.Spelman LH, Osborn KG, Anderson MP. Pathogenesis of hemosiderosis in Lemurs: Role of dietary iron, tannin, and ascorbic acid. Zoo Biology. 2005;8(3):239–51. [Google Scholar]
- 10.Marginean EC, Bennick M, Cyczk JR, et al. Gastric siderosis: patterns and significance. Am J Surg Path. 2006;30(4):514–20. doi: 10.1097/00000478-200604000-00013. [DOI] [PubMed] [Google Scholar]