Abstract
Background
Little is known about the frequency of traumatic event exposure and the development of post-traumatic stress disorder (PTSD) among German soldiers serving in Afghanistan.
Methods
We studied a random sample consisting of 1599 soldiers who had served in the 2009/2010 ISAF mission in Afghanistan, stratified by deployment location and unit. Twelve months after their return to Germany, the soldiers were assessed with a Composite International Diagnostic Interview (CIDI) to establish the diagnoses of mental disorders and PTSD according to the DSM-IV. 889 similar soldiers who had not been deployed abroad were assessed in the same way.
Results
49.2% (95% confidence interval [CI]: 46.4 to 52.1) of the deployed soldiers experienced at least one traumatic event during their deployment, and 13% experienced more than three. The 12-month prevalence of PTSD among returning soldiers was 2.9% (95% CI: 2.1 to 4.1), while the service-related incidence after deployment was 0.9% (95% CI: 0.5 to 1.6). These figures imply a two- to fourfold elevation of the risk of PTSD. The risk of PTSD was highest among soldiers who had served in Kunduz (Afghanistan) and in combat units. Only half of all soldiers with PTSD sought professional help.
Conclusion
Deployment abroad is associated with a high frequency of traumatic experiences and a two- to fourfold elevation of the risk of PTSD. Each year, about 300 cases of PTSD develop for every 10 000 soldiers who return to Germany; thus, the cumulative number of returnees with PTSD from the beginning of German deployment abroad may currently run into the thousands. 45% of all PTSD cases, or about one in two, are neither diagnosed nor treated. Deployment abroad also substantially increases the risk of developing a number of other mental disorders.
There is a well established connection between stressful military events and events defined as traumatic and the occurrence of posttraumatic stress disorder (PTSD) as defined in DSM-IV (Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition) (1, 2– 5). The probability of onset and the risk factors of PTSD, however, are extremely variable (e.g. [5–8). These studies have made clear that results on prevalence, incidence, and risk factors are dependent on the research methods used. For example, in military samples, differences in findings on prevalence and incidence were shown to be due to
The evidently huge dependency of findings on sample and context makes it difficult to generalize results. Thus US studies report PTSD rates of between 9% and more than 20%, depending on type of troop and differentiation of severity on diagnosis (10). In contrast, a significantly lower rate of approximately 4% is given for British soldiers in Iraq and Afghanistan (11). It is problematic that knowledge on this subject is based almost exclusively on cross-sectional studies that do not state which soldiers had already been exposed to traumatic events before deployment or even were already suffering from PTSD, and which soldiers were previously healthy and suffered from PTSD for the first time during or following deployment.
Other than administrative statistics, there are no reliable data as yet for Germany (12). There are no comprehensive, representative clinical and epidemiological findings available either on trauma and PTSD or on psychological morbidity in general after deployment (13). What is undisputed is that according to administrative hospital data the frequency of PTSD has significantly increased since the beginning of overseas deployment. The German armed forces’ statistics on outpatient and inpatient psychiatric illnesses show a significant increase in stress reactions (ICD-10 Disorder Code F43) in 2006 when compared to 2000 (12). For a total of 61 925 soldiers deployed between 2006 and 2008, the German Federal Ministry of Defense reports a total of 245 cases of PTSD for 2008 treated in German armed forces hospitals alone. This is nearly twice the figure for 2007 and three times the figure for 2006. On the basis of approximately 25 000 soldiers deployed overseas in 2008, however, this rough estimate of prevalence of 245÷25 000 = 0.98% seems extremely low; these figures may therefore be only the tip of the iceberg, as they refer only to cases seen in German armed forces hospitals. These figures also seem implausible when compared with morbidity figures for the European population as a whole and with international data from military samples (14, 15). For US Army troops stationed in Afghanistan, a PTSD prevalence rate of 6.2% was reported 3 to 4 months after return from deployment. The equivalent figure reported for those returning from the Iraq War (Marines) was 12.2%.
One year after returning from Iraq, 16.6% of all soldiers met the criteria for PTSD (16). For US veterans (17), the actual rate (the hidden problem) in the USA is estimated at 16% (18). However, British findings on military personnel in Iraq (11, 19), which reported a PTSD prevalence of only 3% to 6%, show that these high estimates should not be generalized.
Against this backdrop of incomplete, contradictory information, it seems that studies assessing the true extent of PTSD are urgently required.
Questions
This article investigates the following main questions:
How common are traumatic events among German soldiers who have and have not been deployed overseas?
How many soldiers meet the criteria for PTSD according to DSM-IV following deployment overseas (12-month prevalence) (Box 1)?
What proportion of PTSD cases can be directly attributed to traumatic events during deployment overseas (deployment-related incidence)?
Box 1. Definition of trauma.
The DSM-IV (Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition) (1) defines two essential criteria for trauma that must both be met in order for posttraumatic stress disorder to be diagnosed:
Criterion A1:
The person experienced or witnessed or was confronted with an event or events that involved actual or threatened death or serious injury, or a threat to the physical integrity of self or others.
Criterion A2:
The person’s response involved intense fear, helplessness, or horror.
This study is based on this definition of trauma.
In addition, the findings are used to estimate the possible extent of the hidden problem.
Methods
Data were collected in the cross-sectional part of the Prevalence, Incidence and Determinants of PTSD and Other Mental Disorders (PID-PTSD+3) study. The design and methods of this stratified clinical epidemiological research program are described only briefly (details in [20], see article at www.psychologie.tu-dresden.de/i2/klinische/PTSD-STUDY/methods.pdf).
Samples
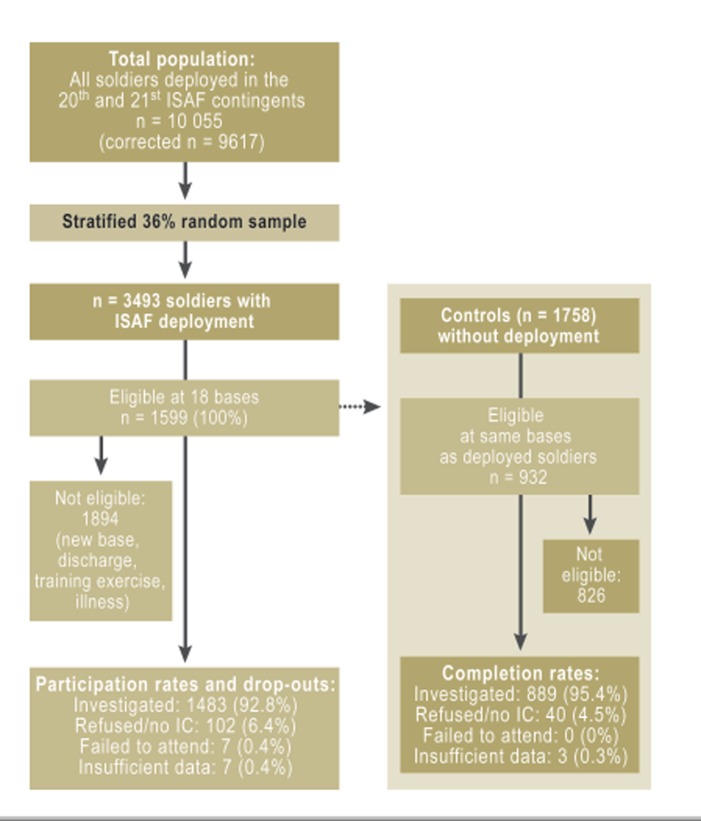
The PID-PTSD+3 cross-sectional study is based on a stratified random sample (Figure, Box 2) of n = 1599 German soldiers deployed in Afghanistan in the year before the study as part of the German ISAF (International Security Assistance Force) mission and a control group of n = 889 soldiers who had never been deployed overseas (Figure). The soldiers who had been on overseas deployment were taken from the population of all eligible soldiers of the 20th and 21st German ISAF contingents. Of the 1599 eligible soldiers (100%), n = 102 (6.4%) refused to take part, n = 7 (0.4%) did not consent to the timeframe for the study, and n = 7 (0.4%) provided incomplete information. A total of n = 1483 study participants (response rate: 92.8%) were investigated.
Figure.
Total population, sampling, eligibility, and response rate of soldiers who have been deployed overseas and those who have not (control group); ISAF: International Security Assistance Force; IC: informed consent
Box 2. Representativeness of the study for deployed soldiers.
The total population from which the study sample was taken consisted of 9617 soldiers from the 20th and 21st contingents of the 2009/2010 ISAF mission of the German armed forces in Afghanistan. Because project resources were limited, a random sample stratified by soldiers’ features (e.g. combat units were more likely to be included in the sample) and additional inclusion and eligibility criteria were required. Because clinical examination had to be performed by the study team in person on site, these criteria included the following:
The soldiers were at the location in question during the weeks of the study, defined previously.
There were enough (more than 50) eligible soldiers at each study location.
The soldiers gave informed consent.
Because updated information on these features was not available to the German armed forces, the eligibility of each individual could not be determined until after the sample had been taken.
On the basis of power calculations, feasibility considerations, and the assumption of a high proportion of ineligible soldiers, a 36% random sample (n = 3493) was taken. Of these soldiers, 1599 at 18 sufficiently large locations met all the inclusion criteria. 1894 soldiers were ineligible because they were stationed in other locations or locations that were too small (49.3%), had left the German armed forces (23.9%), were on leave (5.2%) or training (15.7%), or were recorded as sick (5.9%).
The ineligible soldiers did not differ significantly from the eligible soldiers in terms of military and deployment-related features; the exception was an overrepresentation of low-ranking fixed-term soldiers not stationed in Kunduz. Also, additional internal verifications of medical records by the German armed forces ruled out an increasing frequency of potential PTSD cases (20).
Against this backdrop, and in view of the exceptionally high completion rates of eligible patients, we cannot identify any significant limitations on the data’s representativeness regarding soldiers deployed on the 2009/2010 ISAF mission.
In order to investigate the risk of morbidity, n = 932 soldiers who had not been deployed overseas were drawn, from the same locations and according to the same criteria. Of these, n = 889 were successfully investigated (response rate: 95.4%, refusal to participate: n = 40, incomplete information: n = 3). Both study groups were weighted for probability of being selected and response rate effects, or adjusted for differences in features in comparisons between the groups (Figure, Box 2).
Procedures and methods
The study was explained to all soldiers at the same point in time (2010) at their home base locations an average of 12 months following deployment overseas, by experienced, trained clinical interviewers (65 clinical psychologists). They were investigated using the computer-assisted (CAPI) standardized, clinical and diagnostic Munich Composite International Diagnostic Interview (DIA-X/M-CIDI [21]), military version. The DIA-X/M-CIDI allows the standardized assessment and objective analysis and evaluation of symptoms, syndromes, and diagnoses according to the criteria of DSM-IV text revision (TR) (22, 23). The 12-month and lifetime versions were used, supplemented with modules that were relevant to the aims of the study in a military context. For example, the trauma section was supplemented by separating military and non-military events, separating mission-related and non-mission-related events, and using scales (e.g. the Combat Experiences Scale [MHAT-VI] and the Posttraumatic Diagnostic Scale [PDS (24)]). In addition, the section “Seeking Help/Treatment” included all services available in the German armed forces before and after intervention.
Analysis
Outcome measures are as follows:
12-month prevalence (DSM-IV criteria for PTSD met within the last 12 months)
12-month incidence (first-time onset of PTSD)
Lifetime prevalence (a case of PTSD, whether in the last 12 months or earlier)
In addition, distinctions were drawn between the following:
Traumatic events according to DSM-IV/A2
Distressing events of any kind according to DSM-IV/A1
Deployment-related and other events in the individual’s life.
Results are shown as non-weighted n and weighted percentages and 95% confidence intervals (95% CIs) or weighted means and standard deviations. Only weighted figures and statistical tests should be interpreted (see [20]). Differences in outcome variables with multiple categories are tested using a design-based modification of the chi-square test of independence (25). Linear regressions are calculated for dimensional outcome variables, and logistical regressions with odds ratios (ORs) are calculated for binary dependent variables (26). Statistical tests are performed bilaterally at the 5% level, and p-values are compared with the 5% test. All analyses are performed using Stata 12.1 (27).
Results
Sample characteristics
The examined sample of deployed soldiers (Table 1) consisted of 1439 men (97%) and 44 women, with a mean age of 30.8 years. 15.9% had graduated from general secondary school (Hauptschule), and 17.9% from university preparatory high school (Gymnasium). The proportion of soldiers who were as yet unmarried was 59.9%. 34.8% were married, and 5.3% divorced, separated, or widowed. 38.9% had children. There were no significant differences between this group and the n = 889 controls.
Table 1. Biosocial and military features of soldiers.
| Deployed soldiers (n = 1483) | Control group (n = 889) | Test* | |||||||||||
| ntotal | n | % | W % | ntotal | n | % | W % | p-value | |||||
| Sex | |||||||||||||
| Male | 1483 | 1439 | 97.0 | 94.8 | 889 | 779 | 87.6 | 95.5 | 0.499 | ||||
| Female | 44 | 3.0 | 5.2 | 110 | 12.4 | 4.5 | |||||||
| Age, M (SD) | 1483 | 29.6 (7.3) | 30.8 (7.7) | 889 | 26.1 (6.7) | 30.8 (7.7) | 0.103 | ||||||
| 18 to 24 | 398 | 26.8 | 20.2 | 476 | 53.4 | 28.0 | 0.018 | ||||||
| 25 to 29 | 555 | 37.4 | 37.3 | 284 | 32.0 | 37.3 | |||||||
| 30 to 39 | 349 | 23.5 | 26.7 | 69 | 7.8 | 19.1 | |||||||
| ≤ 40 | 181 | 12.2 | 15.9 | 60 | 6.8 | 15.6 | |||||||
| BMI, M (SD) | 1476 | 25.5 (2.9) | 25.4 (2.9) | 885 | 25.0 (3.2) | 26.0 (3.2) | 0.617 | ||||||
| Level of schooling | |||||||||||||
| General secondary school (Hauptschule) | 1483 | 275 | 18.5 | 15.9 | 889 | 182 | 20.5 | 18.2 | 0.391 | ||||
| Intermediate secondary school (Realschule) | 961 | 64.8 | 66.2 | 541 | 60.9 | 62.1 | |||||||
| University preparatory high school, specialized college | 247 | 16.7 | 17.9 | 166 | 18.7 | 19.8 | |||||||
| Marital status | |||||||||||||
| Single | 1483 | 960 | 64.7 | 59.9 | 887 | 719 | 81.1 | 66.3 | 0.138 | ||||
| Married | 449 | 30.3 | 34.8 | 149 | 16.8 | 28.6 | |||||||
| Separated/widowed/divorced | 5.0 | 5.3 | 19 | 2.1 | 5.1 | ||||||||
| Children | |||||||||||||
| Yes | 516 | 34.8 | 38.9 | 889 | 177 | 19.9 | 36.3 | 0.399 | |||||
| Rank | |||||||||||||
| Lower ranks | 1483 | 533 | 35.9 | 24.5 | 889 | 246 | 28.0 | 33.5 | 0.008 | ||||
| Intermediate ranks | 799 | 53.9 | 62.7 | 565 | 64.0 | 55.5 | |||||||
| Higher ranks (Officer) | 151 | 10.2 | 12.8 | 78 | 8.8 | 11.0 | |||||||
| Type of unit | |||||||||||||
| Combat unit | 1478 | 616 | 41.7 | 25.0 | 881 | 158 | 18.0 | 21.1 | 0.006 | ||||
| Medical services | 67 | 4.5 | 6.6 | 77 | 8.7 | 8.2 | |||||||
| Other | 795 | 53.8 | 68.3 | 646 | 73.0 | 70.6 | |||||||
| Branch | |||||||||||||
| Army | 1481 | 995 | 67.2 | 57.8 | 881 | 434 | 49.0 | 61.3 | 0.623 | ||||
| Air force | 384 | 25.9 | 32.7 | 346 | 39.0 | 30.4 | |||||||
| Marines | 1 | 0.1 | 0.1 | 2 | 0.2 | 0.3 | |||||||
| Joint Support Service | 33 | 2.2 | 2.8 | 32 | 3.6 | 2.2 | |||||||
| Medical services | 68 | 4.6 | 6.7 | 67 | 7.6 | 5.8 | |||||||
BMI, body mass index; W %, weighted percentage; M, mean; SD, standard deviation
Soldiers deployed overseas adjusted to feature distribution in the total population; for the control group. the weighted data shown are adjusted to soldiers deployed overseas.
*For categorical variables: design-based test of independence (adjusted data), for dimensional variables: t-test. reliable estimate of standard error (adjusted data) using Huber–White sandwich matrix
N.B.:
Please note that due to weighting factors and varying conventions for data evaluation there are some minor differences between the figures shown here and an earlier presentation (press conference of 23 March 2011, Berlin).
The soldiers had served in the German armed forces for an average of 10 years. 25.6% had served for less than five years. 25.0% (non-weighted value 41.7%) of the deployed soldiers belonged to combat units, 68.3% to combat support or health support forces (6.6%); they were serving in the following branches: army (57.8%), air force (32.7%), medical support (6.7%), Joint Support Service (2.8%), Marine (0.1%). 43.0% of the soldiers served overseas for the first time in 2009, 37.0% had previously been deployed overseas between two and four times, and 19.9% five or more times. During their 2009 deployment, the deployed soldiers were mostly stationed in Mazar-e Sharif (67.7%) or Kunduz (19.6%). The mean length of deployment was 3.8 months (standard deviation [SD] 1.6).
Traumatic events
The classification of events as distressing (criterion DSM-IV/A1) or traumatic (criterion DSM-IV/A2) is based on the MHAT scale for deployed soldiers, and on the 28 categories of events in the CIDI for both groups (Table 2).
Table 2. Traumatic events in a military context, on overseas deployment, and over lifetime.
| Soldiers deployed overseas (n = 1483) | Control group (n = 889) | ||||||
| n | W % (95% CI) | n | W % (95% CI) | p-value | |||
| Traumatic events during deployment | |||||||
| % suffering at least one event | 1323 | 85.5 (83.3 to 87.5) | –*2 | ||||
| Mean (95% CI), SD*1 | 6.2 | (5.9 to 6.5), 5.3 | –*2 | ||||
| Traumatic personal events during deployment | |||||||
| % suffering at least one event | 394 | 24.2 (21.9 to 26.7) | 97 | 11.1 (8.2 to 14.9) | 0.000 | ||
| Mean (95% CI), SD*1 | 1.2 | (1.2 to 1.3), 0.5 | 1.0 | (1.0 to 1.1), 0.1 | 0.000 | ||
| Other traumatic events (lifetime) | |||||||
| % suffering at least one event | 604 | 40.1 (37.3 to 42.9) | 385 | 43.6 (38.2 to 49.6) | 0.258 | ||
| Mean (95% CI), SD*1 | 1.6 | (1.5 to 1.7), 0.9 | 1.5 | (1.4 to 1.7), 1.0 | 0.434 | ||
| Total traumatic events (lifetime) | |||||||
| % suffering at least one event | 754 | 49.2 (46.4 to 52.1) | 429 | 49.9 (44.3 to 55.6) | 0.833 | ||
| Mean (95% CI), SD*1 | 2.0 | (1.9 to 2.1), 1.3 | 1.8 | (1.6 to 1.9), 1.1 | 0.009 | ||
*1Mean of those suffering at least one event, regardless of frequency;
*2Applicable only to soldiers deployed overseas 95% CI, 95% confidence interval; W %, weighted percentage
85.5% (95% CI: 83.3 to 87.5) of all deployed soldiers (2) reported at least one, but usually several, distressing events (mean: 6.2; SD: 5.3). 24.2% (95% CI: 21.9 to 26.7) of the deployed soldiers reported that they personally had experienced at least one traumatic event during deployment. In the control group, traumatic military events were significantly (p<0.000) rarer, at 11.1% (95% CI: 8.2 to 14.9). Deployed soldiers also reported a significantly higher number (p <0.001) of traumatic events. For other lifetime, non-military events, there were no differences between the groups.
Soldiers stationed in Kunduz showed a significantly higher number of distressing events (mean difference): 3.7; 95% CI: 3.0 to 4.4) and a higher probability of traumatic events during deployment (OR: 1.8; 95% CI: 1.4 to 2.3) than soldiers stationed in other locations. This probability was equally increased among combat units (OR: 1.7; 95% CI: 1.2 to 2.3) and combat support/health support forces (OR: 1.9; 95% CI: 1.3 to 2.7). Other than the main effect “location of deployment,” there was no evidence of a significant interaction (Table 3).
Table 3. 12-month and lifetime prevalence and 12-month incidence of posttraumatic stress disorder in soldiers who have been deployed and those who have not (control group).
| 12-month diagnosis | 12-month incidence | Lifetime prevalence | |||||||||||||
| n | % | W % (95% CI) | n | % | W % (95% CI) | n | % | W % (95% CI) | |||||||
| Total population | |||||||||||||||
| Deployed soldiers | 43 | 2.9 | 2.9 (2.1 to 4.1) | 18 | 2.1 | 0.9 (0.5 to 1.6) | 65 | 4.4 | 4.6 (3.6 to 6.0) | ||||||
| Control group | 22 | 2.5 | 1.2 (0.6 to 2.5) | 2 | 0.2 | 0.2 (0.04 to 1.1) | 42 | 4.7 | 2.7 (1.6 to 4.5) | ||||||
| OR, 95% CI, SL* | 2.5 (1.1 to 5.6) p = 0.033 | 4.2 (0.7 to 24.5) p = 0.071 | 1.7 (0.96 to 3.1) p = 0.066 | ||||||||||||
| Deployed soldiers, subgroups* | |||||||||||||||
| Kunduz (n = 537) | 15 | 2.8 | 2.5 (1.3 to 4.8) | 10 | 1.9 | 1.4 (0.6 to 3.1) | 22 | 4.1 | 4.5 (2.7 to 7.4) | ||||||
| OR, 95% CI, SL* | 2.1 (0.8 to 5.8) p = 0.148 | 6.6 (1.03 to 41.9) p = 0.046 | 1.7 (0.8 to 3.6) p = 0.166 | ||||||||||||
| Combat units (n = 681) | 19 | 2.8 | 2.6 (1.6 to 4.3) | 12 | 1.8 | 1.5 (0.8 to 2.8) | 25 | 3.7 | 3.7 (2.3 to 5.6) | ||||||
| OR, 95% CI, SL* | 3.3 (0.5 to 23.7) p = 0.240 | No cases in control group | 2.6 (0.7 to 9.4) p = 0.147 | ||||||||||||
*The control group for soldiers deployed overseas consists of control soldiers (soldiers who have not been deployed overseas); the sample section “Deployed soldiers in combat units” was compared with combat units not deployed overseas; soldiers deployed overseas in Kunduz were compared with all members of the control group.
OR, odds ratio; 95% CI, 95% confidence interval; SL, significance level
N.B.:
Please note that due to weighting factors and varying conventions for data evaluation there are some minor differences between the figures shown here and an earlier presentation (press conference of 23 March 2011, Berlin).
Posttraumatic stress disorder
12-month prevalence: At 2.9% (n = 43; 95% CI: 2.1 to 4.1), significantly more deployed soldiers (OR: 2.5; 95% CI: 1.1 to 5.6; p<0.033) met the DSM-IV-TR criteria for PTSD (Table 3) than soldiers in the control group (1.2%; n = 22; 95% CI: 0.6 to 2.5) in the 12 months preceding the interview.
12-month incidence: Deployed soldiers (0.9%, 95% CI: 0.5 to 1.6) also showed first-time (incident) onset of PTSD in the last 12 months significantly more frequently than soldiers in the control group (0.2%; 95% CI: 0.4 to 1.1). This difference may not meet the significance level because of a lack of statistical power (OR: 4.2; 95% CI: 0.7 to 24.5, p = 0.071).
Lifetime prevalence: in addition to the n = 43 deployed soldiers with 12-month PTSD, a further n = 22 had met the criteria for PTSD earlier in their lives (before the 12-month period). This gives a lifetime prevalence of 4.6% (95% CI: 3.6 to 6.6) for deployed soldiers. This is higher (OR: 1.7; 95% CI: 0.96 to 3.1) than in the control group (n = 42, 2.7%; 95% CI: 1.6 to 4.5), albeit not to a significant extent (Table 3).
Deployed soldiers stationed in Kunduz and combat units show a higher probability of PTSD than other deployed soldiers, although the difference is only significant for 12-month incidence (Kunduz: OR: 6.6; 95% CI: 1.0 to 41.9; p = 0.046, deployed soldiers in combat units ([design-based F-test (1.855) = 4.9; p = 0.027]).
Events during soldiers’ overseas deployment
Table 4 shows the most common types of events in deployed soldiers, ordered by frequency in the total study population. The differing percentages for incident PTSD and sometimes significantly lower frequency figures for 12-month or lifetime PTSD, as well as individuals reporting traumatic events but not PTSD, indirectly reveal that the type of any single event is not essential for PTSD to occur; rather it appears to be the number of events that matters (Table 4).
Table 4. Frequency of deployment events for soldiers deployed overseas.
| Total overseas | Of which: | ||||||||||||||
| At least 1 traumatic event (no PTSD) | Lifetime PTSD diagnosis | 12-month PTSD diagnosis | Incident PTSD diagnosis | ||||||||||||
| Sorted by frequency | (n = 1483) | (n = 689) | (n = 65) | (n = 43) | (n = 18) | ||||||||||
| Experienced at least once: | n | W % | n | W % | n | W % | n | W % | n | W % | |||||
| Seeing destroyed homes or villages | 1131 | 70.4 | 563 | 76.4 | 54 | 78.7 | 38 | 87.6 | 16 | 86.7 | |||||
| Receiving incoming artillery, rocket, or mortar fire | 697 | 36.0 | 386 | 43.6 | 35 | 44.8 | 26 | 53.0 | 14 | 78.7 | |||||
| Having hostile reactions from civilians | 608 | 32.6 | 330 | 39.4 | 40 | 54.7 | 28 | 61.2 | 13 | 69.5 | |||||
| Seeing ill/injured women or children, but unable to help | 533 | 32.0 | 302 | 39.4 | 36 | 54.3 | 28 | 67.4 | 13 | 70.7 | |||||
| Seeing dead or seriously injured comrades | 474 | 31.3 | 290 | 41.7 | 30 | 45.9 | 21 | 49.6 | 11 | 67.9 | |||||
| Being attacked or ambushed | 625 | 30.5 | 355 | 38.6 | 35 | 48.0 | 25 | 54.5 | 11 | 61.7 | |||||
| Seeing dead bodies or human remains | 482 | 29.6 | 282 | 38.5 | 33 | 46.4 | 24 | 51.8 | 11 | 57.5 | |||||
| Knowing someone seriously injured or killed | 504 | 28.6 | 305 | 38.3 | 38 | 54.3 | 27 | 61.7 | 13 | 61.7 | |||||
| Receiving small arms fire | 555 | 24.6 | 319 | 31.1 | 35 | 45.4 | 25 | 50.4 | 13 | 66.2 | |||||
| Witnessing violence within the local population | 391 | 21.0 | 214 | 24.9 | 26 | 38.7 | 23 | 54.5 | 8 | 45.7 | |||||
| Improvised explosive device (IED)/booby trap exploded nearby | 396 | 20.4 | 235 | 27.2 | 20 | 31.3 | 14 | 35.8 | 7 | 36.6 | |||||
| Clearing/searching caves or bunkers | 396 | 20.4 | 235 | 27.2 | 20 | 31.3 | 14 | 35.8 | 7 | 36.6 | |||||
| Working in mined areas | 372 | 19.2 | 214 | 24.2 | 21 | 30.5 | 16 | 35.5 | 6 | 24.1 | |||||
| Shooting or directing fire at the enemy | 432 | 18.1 | 255 | 23.6 | 27 | 30.1 | 18 | 30.0 | 10 | 43.8 | |||||
| Had a close call, unexploded dud landed nearby | 361 | 17.1 | 213 | 22.1 | 27 | 32.5 | 20 | 37.8 | 10 | 34.5 | |||||
| Witnessing an accident which resulted in serious injury or death | 291 | 17.0 | 170 | 21.8 | 25 | 33.5 | 16 | 30.9 | 8 | 29.1 | |||||
| Having a member of his/her own unit become a casualty | 292 | 12.0 | 174 | 16.1 | 22 | 27.5 | 16 | 30.1 | 8 | 34.3 | |||||
| Participating in demining operations | 254 | 10.7 | 138 | 12.0 | 15 | 18.9 | 12 | 24.4 | 5 | 28.3 | |||||
| Clearing/searching homes or buildings | 233 | 10.2 | 131 | 12.6 | 16 | 21.8 | 14 | 29.9 | 6 | 24.4 | |||||
| Disarming civilians | 176 | 9.0 | 98 | 11.1 | 16 | 21.6 | 14 | 29.4 | 7 | 31.5 | |||||
| Being in threatening situations, unable to respond because of rules of engagement | 178 | 8.3 | 111 | 11.6 | 16 | 19.0 | 13 | 22.9 | 8 | 33.7 | |||||
| Witnessing brutality/mistreatment toward non-combatants | 149 | 7.9 | 85 | 9.7 | 13 | 19.4 | 9 | 20.7 | 4 | 15.3 | |||||
| Had a close call, equipment shot off body | 149 | 7.9 | 85 | 9.7 | 13 | 19.4 | 9 | 20.7 | 4 | 15.3 | |||||
| Handling or uncovering human remains | 105 | 6.9 | 65 | 9.5 | 10 | 15.9 | 6 | 13.8 | 3 | 12.3 | |||||
| Calling in fire on the enemy | 197 | 6.8 | 106 | 8.0 | 13 | 13.4 | 12 | 20.9 | 7 | 27.3 | |||||
| Had a close call, was shot or hit but rescued | 114 | 5.2 | 72 | 7.0 | 8 | 9.5 | 4 | 4.9 | 3 | 10.6 | |||||
| Informed others of a comrade’s death | 85 | 5.1 | 54 | 7.4 | 10 | 13.5 | 8 | 16.8 | 4 | 21.4 | |||||
| Being directly responsible for the death of an enemy combatant | 131 | 4.2 | 77 | 5.6 | 11 | 7.6 | 10 | 11.7 | 6 | 18.2 | |||||
| Observing abuse of Laws of War/Geneva Convention | 68 | 3.4 | 45 | 5.2 | 7 | 7.6 | 7 | 12.2 | 5 | 23.9 | |||||
| Being wounded or injured | 42 | 2.3 | 25 | 3.3 | 6 | 8.2 | 4 | 8.3 | 3 | 17.6 | |||||
| Engaging in hand-to-hand combat | 50 | 2.2 | 28 | 2.8 | 7 | 6.5 | 5 | 6.3 | 3 | 7.6 | |||||
| Had a comrade nearby shot or killed | 49 | 1.9 | 28 | 2.7 | 5 | 6.4 | 5 | 10.3 | 3 | 11.2 | |||||
| Being responsible for a comrade’s serious injury or death | 9 | 0.4 | 7 | 0.8 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | |||||
“Experienced at least once” means that traumatic events experienced more than once are not shown here.PTSD, posttraumatic stress disorder; W %, weighted percentage
Discussion
On the basis of a representative sample of 1483 soldiers who have been deployed overseas and 889 who have not, we obtained the following results:
2.9% of the soldiers deployed in Afghanistan in 2009 as part of the ISAF mission returned from deployment (12-month prevalence) with clinically significant posttraumatic stress disorder (PTSD) according to the DSM-IV-TR criteria. Of these, one-third were suffering from PTSD for the first time (12-month incidence: 0.9%). The onset of PTSD occurred shortly (between 2 and 11 months) afterwards.
In absolute terms, this means that for every 10 000 German soldiers who serve overseas in the ISAF for an average of four months, in the 12 months following the beginning of deployment 291 soldiers (95% CI: 209 to 405) suffer from PTSD; of these, 89 (95% CI: 51 to 156) are soldiers suffering from PTSD for the first time (incident cases), i.e. new cases of PTSD.
This corresponds to an odds ratio of 2.5 for PTSD prevalence, and OR 4.2 for incidence. The risk of PTSD is highest for Kunduz (OR: 6.6) and for combat units.
These findings refer to a randomly-selected group of 2009 ISAF soldiers and should not be generalized, because of possible differences in deployment features and locations over time. The effect of relevant factors such as length of deployment, trauma, and comorbidity on the risk of PTSD, and the perhaps significantly higher risk of other deployment-related psychological disorders such as depression, anxiety, or addiction, are examined in depth in subsequent publications.
With a PTSD prevalence of 2.9% and an incidence of 0.9%, the number of new deployment-related PTSD cases is certainly not as high as has been suspected by many and discussed in the lay press.
However, we also point out that our PTSD data alone do not yet adequately take into account the full extent of psychological consequences of deployment. Firstly, proper account must be taken of other clinically relevant psychological syndromes caused by deployment, in addition to PTSD. Secondly, we consider only soldiers who served in 2009/2010. This means that there is a considerable accumulation of cases of PTSD and other psychological disorders from the beginning of overseas deployment mission, depending on the total number of all soldiers deployed overseas each year. The total number of cases of deployment-related PTSD alone up to 2012 may be conservatively estimated at several thousand soldiers. Thirdly, we have only included PTSD cases that exhibit the full clinical picture of PTSD according to DSM-IV. The proportion of soldiers who already met the criteria for PTSD before overseas deployment in 2009 but have not exhibited the full clinical picture in the last 12 months, which at 1.7% is not inconsiderable, indicates that in addition to the 2.9% of current PTSD cases there may be a further high-risk group that cannot yet be sufficiently described. This finding also gives rise to the question of whether current diagnostic screening for PTSD before deployment is sufficiently sensitive.
Preliminary further analyses show that only around half of PTSD sufferers have sought professional help for their disorder. The current status of analysis does not provide information on whether any treatment was actually received or why help was not sought. The fact that only some soldiers with PTSD have sought professional help hints that there may be a substantial number of hidden cases. On the basis of an approximate total of 15 000 soldiers deployed to Afghanistan in 2009 and assuming comparable military deployment conditions and identical help seeking patterns, the number of these hidden cases can be estimated at approximately 150 of a total of 291 PTSD sufferers (12-month prevalence). Although epidemiological findings should not be directly and uncritically interpreted as a need for treatment, in this article we show quantitatively for the first time the currently unmet need for additional intervention in diagnosis, counseling, or treatment.
Clearly, the PTSD rates of German soldiers are significantly lower than those of British or American soldiers who have served in Iraq or Afghanistan, for example (11, 16). It might be suspected that the lower PTSD rates in Germany than in the USA are connected with more effective medical selection procedures or other types of deployment of the German armed forces overseas. This might include more intensive preparation for deployment, shorter average duration of deployment (4 to 5 months rather than 1 to 2 years), or less total direct exposure to combat situations compared to US or British soldiers. It should also be noted that the 12-month and lifetime prevalence of PTSD in deployed soldiers is not only significantly higher than for soldiers in the control group who have not been deployed, but also significantly higher than the rates for the age- and sex-adjusted German and European general population (15).
The relatively low rate of PTSD in German soldiers should under no circumstances lead one to overlook the fact that overseas deployment of the German armed forces is regularly associated with a high degree of trauma and stress. Traumatic deployment-related events such as combat confrontations, injury, and death occur to almost all soldiers during deployment, often several times. Focusing only on PTSD also overlooks the fact that other deployment-related mental disorders, e.g. depression, sleep disorders, and fatigue, may play a considerably greater role than PTSD itself. This is indicated by preliminary analyses, which show that the actual extent of deployment-related mental disorders is several times higher than the frequency of PTSD. This suggests that the focus of future preventive and curative measures for the problem of mission-related adverse mental outcomes should be broadened to include the whole spectrum of mental disorders.
Key Messages.
For soldiers in the German armed forces, overseas deployments as part of the ISAF (International Security Assistance Force) are associated with frequent, traumatic events and a two- to four-fold increase in the risk of posttraumatic stress disorder (PTSD).
2.9% of the soldiers deployed in Afghanistan as part of the 2009 ISAF mission returned with clinically significant posttraumatic stress disorder (PTSD) according to the criteria of DSM-IV-TR.
The cumulative total number of PTSD cases since the beginning of German overseas deployment may therefore be in the thousands. It seems that half of PTSD cases remain undiagnosed and untreated (hidden cases: 45%).
Although these epidemiological findings should not be directly and uncritically interpreted as a need for treatment, this article shows quantitatively for the first time the considerable degree of unmet need for diagnosis, counseling, and treatment.
Also, in addition to the risk of PTSD, there is a several times higher risk of other forms of deployment-related mental disorders. The actual extent of deployment-related mental disorders is therefore several times higher than the frequency of PTSD. This suggests that the focus of future preventive and curative measures for the problem of deployment-related mental health should be broadened to include the whole spectrum of mental disorders.
Acknowledgments
Translated from the original German by Caroline Devitt, MA.
The project received content-related and logistical advice and support from the Center for Psychiatry and Psychological Trauma at the Hospital of the German Federal Armed Forces, Berlin. It was also guided by a Steering and Advisory Board of the German armed forces and an Advisory Panel of scientific experts (Prof. Dr. Ronald C. Kessler; Prof. Matthew J. Friedman, MD, Ph.D.; Prof. Ariel Shalev, Prof. Yosep Zohar).
The study was approved and endorsed by the Ethics Committee of the Faculty of Medicine of TU Dresden (the Technical University of Dresden) (EK 72022010). Study conduct complies with the current ICH GCP (Good Clinical Practice) Guidelines.
Footnotes
Conflict of interest statement\
Dr. Schönfeld has received reimbursement of conference fees and travel expenses from Pfizer.
Prof. Wittchen, Prof. Kirschbaum, Dipl.-Psych. Thurau, Dipl.-Psych. Trautmann, Dipl.-Psych. Steudte, Dr. Klotsche, Dr. Höfler, Dr. med. Hauffa, and PD Dr. Zimmermann declare that no conflict of interest exists.
References
- 1.American Psychiatric Association. (4th ed., text rev.) Washington, DC: American Psychiatric Association; 2000. Diagnostic and statistical manual of mental disorders. [Google Scholar]
- 2.Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Eng J Med. 2004;351:13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- 3.Kessler RC, Wittchen HU. Post-disaster mental health need assessment surveys—the challenge of improved future research. Int J Methods Psychiatr Res. 2008;17:1–5. doi: 10.1002/mpr.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stein DJ, Cloitre M, Nemeroff CB, Nutt DJ, Seedat S, Shalev AY, et al. Cape Town consensus on post-traumatic stress disorder. CNS Spectrum. 2009;14:52–58. [PubMed] [Google Scholar]
- 5.Committee on Gulf War and Health. Gulf War and Health: Volume 7: Long-term consequences of traumatic brain injury. Washington, D.C.: The National Academies Press; 2008. Brain injury in veterans and long-term health outcomes; pp. 1–372. [PubMed] [Google Scholar]
- 6.Sareen J, Cox BJ, Afifi TO, Stein MB, Balik SL, Meadows G, et al. Combat and peacekeeping operations in relation to prevalence of mental disorders and perceived need for mental health care—Findings from a large representative sample of military personnel. Arch Gen Psychiatry. 2007;64:843–852. doi: 10.1001/archpsyc.64.7.843. [DOI] [PubMed] [Google Scholar]
- 7.Wittchen HU, Gloster A, Beesdo K, Schönfeld S, Perkonigg A. Posttraumatic stress disorder: Diagnostic and epidemiological perspectives. CNS Spectrum. 2009;14:5–12. [PubMed] [Google Scholar]
- 8.Perkonigg A, Pfister H, Stein MB, Höfler M, Lieb R, Maercker A. Longitudinal course of posttraumatic stress disorder and posttraumatic stress disorder symptoms in a community sample of adolescents and young adults. Eur Neuropsychopharmacol. 2006;16:453–454. doi: 10.1176/appi.ajp.162.7.1320. [DOI] [PubMed] [Google Scholar]
- 9.Zohar J, Sonnino R, Juven-Wetzler A, Cohen H. Can posttraumatic stress disorder be prevented? CNS Spectrum. 2009;14:44–51. [PubMed] [Google Scholar]
- 10.Thomas JL, Wilk JE, Riviere LA, McGurk D, Castro CA, Hoge CW. Prevalence of mental health problems and functional impairment among active component and national guard soldiers 3 and 12 months following combat in Iraq. Arch Gen Psychiatry. 2010;67:614–623. doi: 10.1001/archgenpsychiatry.2010.54. [DOI] [PubMed] [Google Scholar]
- 11.Fear NT, Jones M, Murphy D, Hull L, Iversen AC, Coker B, et al. What are the consequences of deployment to Iraq and Afghanistan on the mental health of the UK armed forces? A cohort study. Lancet. 2010;375:1783–1797. doi: 10.1016/S0140-6736(10)60672-1. [DOI] [PubMed] [Google Scholar]
- 12.Zimmermann P, Hahne HH, Ströhle A. Psychiatrische Erkrankungen bei Bundeswehrsoldaten - Veränderungen in der Inanspruchnahme psychiatrischer Versorgungssysteme im Vergleich der Jahre 2000 und 2006. Trauma und Gewalt. 2009;3:316–327. [Google Scholar]
- 13.Hauffa R, Brahler E, Biesold K, Tagay S. Psychological strain following foreign assignment—Results of an investigation among German soldiers serving in ISAF VII. Psychotherapie Psychosomatik Medizinische Psychologie. 2007;57:373–378. doi: 10.1055/s-2007-970833. [DOI] [PubMed] [Google Scholar]
- 14.Wittchen HU, Jacobi F. Size and burden of mental disorders in Europe—a critical review and appraisal of 27 studies. Eur Neuropsychopharmacol. 2005;15:357–376. doi: 10.1016/j.euroneuro.2005.04.012. [DOI] [PubMed] [Google Scholar]
- 15.Wittchen HU, Jacobi F, Rehm J, Gustavsson A, Svensson M, Jonsson B, et al. The size and burden of mental disorders and other disorders of the brain in Europe 2011. Eur Neuropsychopharmacol. 2011;21:655–679. doi: 10.1016/j.euroneuro.2011.07.018. [DOI] [PubMed] [Google Scholar]
- 16.Hoge CW, Auchterlonie JL, Milliken CS. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA. 2006;295:1023–1032. doi: 10.1001/jama.295.9.1023. [DOI] [PubMed] [Google Scholar]
- 17.Schlenger WE, Kulka RA, Fairbank JA, Hough RL, Jordan BK, Marmar CR, et al. The prevalence of posttraumatic-stress-disorder in the vietnam generation—a multimethod, multisource assessment of psychiatric disorder. J Trauma Stress. 1992;5:333–363. [Google Scholar]
- 18.Solomon Z. A 3-Year Prospective Study of Post-traumatic Stress Disorder in Israeli Combat Veterans. J Trauma Stress. 1989;2:59–73. [Google Scholar]
- 19.Hotopf M, Hull L, Fear NT, Browne T, Horn O, Iversen A, et al. The health of UK military personnel who deployed to the 2003 Iraq war: A cohort study. Lancet. 2006;367:1731–1741. doi: 10.1016/S0140-6736(06)68662-5. [DOI] [PubMed] [Google Scholar]
- 20.Wittchen HU, Schönfeld S, Thurau C, Trautmann S, Galle M, Mark K, et al. German soldiers deployed in Afghanistan: Design and methods of the PID-PTSD-Cube study (PID-PTSD+3) examining the prevalence, incidence and determinants of post traumatic stress and other mental disorders. Int J Methods in Psychiatr Res. 2012 doi: 10.1002/mpr.1356. online version. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wittchen HU, Pfister H, editors. Frankfurt: Swets and Zeitlinger; 1997. DIA-X-Interviews: Manual für Screening-Verfahren und Interview; Interviewheft Längsschnittuntersuchung (DIA-X-Lifetime); Ergänzungsheft (DIA-X-Lifetime); Interviewheft Querschnittuntersuchung (DIA-X-Monate); Ergänzungsheft (DIA-X-Monate); PC-Programm zur Durchführung des Interviews (Längs- und Querschnittuntersuchung); Auswertungsprogramm. [Google Scholar]
- 22.Lachner G, Wittchen HU, Perkonigg A, Holly A, Schuster P, Wunderlich U, et al. Structure, content and reliability of the Munich Composite International Diagnostic Interview (M-CIDI) substance use sections. Eur Addict Res. 1998;4:28–41. doi: 10.1159/000018922. [DOI] [PubMed] [Google Scholar]
- 23.Wittchen HU, Lachner G, Wunderlich U, Pfister H. Test-retest reliability of the computerized DSM-IV version of the Munich-Composite International Diagnostic Interview (M-CIDI) Soc Psychiatry Psychiatr Epidemiol. 1998;33:568–578. doi: 10.1007/s001270050095. [DOI] [PubMed] [Google Scholar]
- 24.Ehlers A, Steil R, Winter H, Foa EB. Deutsche Übersetzung der Posttraumatic Stress Diagnostic Scale (PDS) Oxford: University Warneford Hospital. 1996 [Google Scholar]
- 25.Choi WJ, Mc Hugh RB. A reduction factor in goodness-of-fit and independence tests for clustered and weighted observations. Biometrics. 1989;45:979–996. [PubMed] [Google Scholar]
- 26.Royall R. Model robust inference using maximum likelihood estimators. International Statistical Review. 1998;54:221–226. [Google Scholar]
- 27.StataCorp. College Station, TX: Stata Corporation. 2011. Stata Statistical Software, Release 11.2. [Google Scholar]