Abstract
The role of negative cognition and effect in maintaining psychotic symptoms is increasingly recognized but has yet to be substantiated though longitudinal analysis. Based on an a priori theoretical model, we hypothesized that negative cognition and depressed mood play a direct causal role in maintaining paranoia in people with psychosis and that the effect of mood is mediated by negative cognition. We used data from the 301 patients in the Prevention of Relapse in Psychosis Trial of cognitive behavior therapy. They were recruited from consecutive Community Mental Health Team clients presenting with a recent relapse of psychosis. The teams were located in inner and outer London and the rural county of Norfolk, England. The study followed a longitudinal cohort design, with initial measures repeated at 3 and 12 months. Structural equation modeling was used to investigate the direction of effect between negative cognition, depressed mood, and paranoia. Overall fit was ambiguous in some analyses and confounding by unidentified variables cannot be ruled out. Nevertheless, the most plausible models were those incorporating pathways from negative cognition and depressed mood to paranoid symptoms: There was no evidence whatsoever for pathways in the reverse direction. The link between depressed mood and paranoia appeared to be mediated by negative cognition. Our hypotheses were thus corroborated. This study provides evidence for the role of negative cognition in the maintenance of paranoia, a role of central relevance, both to the design of psychological interventions and to the conceptualizations of psychosis.
Keywords: schizophrenia, paranoia, depression, cognitive schemas, structural equation modeling
Introduction
It is increasingly apparent that the etiology of psychosis is extremely complex and must include psychosocial interactions as well as neurobiological predispositions. A number of cognitive models have been proposed over the last decade to integrate the cognitive, social, and emotional processes believed to contribute both to the occurrence and to the persistence of positive psychotic symptoms.1–6 There are equivalent models of individual symptoms, such as persecutory delusions7,8 and auditory hallucinations.9 The models were derived from early empirical findings and from the experience of delivering cognitive behavior therapy (CBT) to people with psychosis: They had the specific intention of shaping research programmes. Although they differ somewhat in emphasis, they cohere in postulating psychological mechanisms that include both an increased vulnerability to anxiety and depression and biases in the cognitive processing of events and experiences.
The proposed role of dysfunctional thinking and emotional dysregulation in the development and maintenance of psychosis is increasingly supported by research.1,10–13 In particular, there is now evidence from epidemiological, questionnaire, experimental, and treatment studies that negative cognition (low self-esteem, self-critical thinking, and extreme negative beliefs about self and others) and depressed mood can contribute to the development of symptoms of psychosis.12–26
However, previous studies showing associations between positive psychotic symptoms, negative cognition, and mood have relied on cross-sectional designs that inevitably constrain causal inference. We ourselves have used such cross-sectional designs to demonstrate that extreme negative beliefs about self and others, and depressed mood were independently associated with persecutory delusions.27,28 These findings are consistent with others indicating a role for negative cognition in psychotic symptoms independent of mood.14 However, it remains unclear whether symptom development is influenced by negative cognition and emotional dysregulation or vice versa.
The current article is the first to test the plausibility of these hypothesized causal links in a large clinical sample involving longitudinal assessment of people with nonaffective psychosis. The analyses formed an ancillary part of the original protocol of the Psychological Prevention of Relapse in Psychosis (PRP) Trial. This was a British multicenter, randomized controlled trial of CBT and family intervention for psychosis (ISRCTN83557988). A comprehensive description of the trial and its methods is provided elsewhere.29 For present purposes, we treated the whole dataset as a cohort, utilizing data from baseline, 3-month, and 12-month assessments. Participants were selected on the basis that they had developed psychosis some time previously. We were thus investigating the factors that influenced the waxing and waning of psychotic symptoms already established.
Our focus here is specifically on symptoms of paranoia. We test associations between variables both within and across time points (cross-sectional and cross-lagged relationships), using structural equation modeling (SEM) in a nested model design. Our published cognitive model of psychosis4,5 suggests that negative cognition (low self-esteem, self-critical thinking, and extreme negative beliefs about self and others) and depressed mood can exacerbate and maintain paranoia. This contrasts with traditional views, which argue that emotional dysfunction is a natural consequence of the occurrence of paranoid states, with little etiological significance. Our aim was therefore to assess the plausibility of specific directional pathways leading from negative cognition and depressed mood to paranoia. The key test was the degree to which models incorporating specific directional pathways from negative cognition and depressed mood to paranoia would provide a better fit than those where the pathways were in the opposite direction. Our second prediction was that the effect of depressed mood on paranoia would be mediated by negative cognition. This was tested by examining the pattern of associations within a model that examined how the combination of negative cognition and depressed mood was associated with paranoia.
Methods
Participants
Participants were recruited from consecutive clients of Community Mental Health. Teams based in inner and outer London and in the rural county of Norfolk. They had experienced a relapse in positive symptoms within the last 3 months and had a current diagnosis of nonaffective psychosis (schizophrenia, schizoaffective disorder, and delusional disorder). They were aged 18–65 years and were required to have a rating of at least 4 (moderate severity) on the Positive and Negative Syndrome Scale (PANSS) on at least 1 positive psychotic symptom at initial interview. The current study used data from all participants in the PRP trial (N = 301). Seventy percent of the sample was male, and the mean age was 37.6 years (SD = 11.0 y). Sixty-eight percent had been admitted to hospital as a consequence of their recent relapse in psychosis. Seventy-two percent described themselves as White-British, 8% as Black-Caribbean, 9% as Black-African, and 11% as from other ethnic backgrounds. Eighty-five percent had a diagnosis of schizophrenia, 13% of schizoaffective disorder, and 2% of delusional disorder. The mean length of illness was 10.7 years (SD = 8.9 y), ranging from less than 1–44 years.
Measures
Scale for the Assessment of Positive Symptoms.
The Scale for the Assessment of Positive Symptoms (SAPS) is a 35-item 6-point (0–5) rating instrument administered by an interviewer. Symptoms are rated over the last month. Item 8, which specifically rates persecutory delusions, was used in the current analysis.30
Positive and Negative Syndrome Scale.
The PANSS is a 30-item 7-point (1–7) rating instrument, also interviewer-administered, of the phenomena associated with schizophrenia.31 Symptoms are rated over the last 72 hours. In the current analysis, we used item 6, which specifically rates suspiciousness and paranoia.
Brief Core Schema Scales.
The Brief Core Schema Scales (BCSS) is a 24-item 5-point self-report rating scale (0–4) assessing evaluative beliefs about the self and others.27 It was designed to create a quick and easy-to-use assessment of the type of extreme evaluations of self and others that are a defining feature of people with psychosis. Four scores are obtained: negative self (6 items), positive self (6 items), negative others (6 items), and positive others (6 items). The BCSS has good reliability and internal consistency, with Cronbach′s α coefficients >.78. Principal components analysis revealed a 4-component solution (consistent with the 4 subscale scores), accounting for 57% of the variance. The negative self-items in the BCSS measure strongly held negative self-evaluations (eg, I am bad, I am worthless) and provide an operational construct of negative schematic self-beliefs.
Beck Depression Inventory
The Beck Depression Inventory (BDI-II) is a 21-item self-report scale rated on a 4-point scale (0–3) of increasing severity, designed to assess symptoms of depression occurring over the past 2 weeks.32 The BDI-II consists of 2 factors: negative cognition (9 items; eg, self-dislike) and affective-somatic feelings (12 items; eg, loss of pleasure) and has been shown to have good psychometric properties. Moreover, it has been used in many studies with patients with psychosis33 and correlated at 0.91 with the interview-based Calgary Depression Scale for Schizophrenia.34
Analysis Plan
SEM is a confirmatory data analysis technique. The approach is theoretically driven, allowing a priori theoretical models to be applied to observed data, following which goodness of fit can be ascertained. We took a 2-step approach to the analysis, as follows.
Latent Variable Identification.
The SEM technique encourages the creation of factors that incorporate more than 1 source of measurement for any 1 single construct. The present analysis used 3 such factors: paranoia, negative cognition, and depressed mood.
Paranoia
The paranoia latent variable was predicted by the ‘persecutory delusions’ item from the SAPS (item 8) and the ‘suspiciousness/persecution’ item from the PANSS (item P6). The factor loadings of these items were 0.89 and 0.94, respectively.
Negative Cognition
The main hypotheses of the present study required a negative cognition latent variable. For this purpose, we combined the negative belief about self-subscale of the BCSS and the negative cognition subscale of the BDI-II (factor loadings of 0.82 and 0.86, respectively). We could have based our primary modeling on a negative cognition latent variable based only on BCSS subscales. However, we have already reported that there is considerable independence between the different aspects of beliefs about self and others identified by the BCSS.27 As a result, the prediction of individual BCSS subscales to the latent variable was uneven, with factor loadings of individual subscales of negative self, 0.77; negative other, 0.58; positive self, −0.43; and positive other, −0.32. The negative schema factor was thereby made less stable for modeling purposes. Nevertheless, for the sake of completeness, we also report on models obtained by constructing the negative cognition latent variable only from the BCSS variables.
Depressed Mood
The depressed mood latent variable was predicted by the combination of the individual items of affective-somatic factor of the BDI-II as suggested by the original psychometric analysis of the scale. It thus excluded the negative cognitions subscale of the BDI-II.
Model Hypotheses.
In the second stage of analysis, a series of 3-wave panel analyses (using data from baseline, 3-month, and 12-month assessments) were conducted using MPlus version 435 to test the longitudinal relationships of negative cognition and depressed mood with paranoia. A nested model comparison approach was used to assess relative changes in goodness of fit associated with the addition of paths between constructs.36 A number of theoretically plausible models were identified a priori, and our hypotheses were tested by comparing the fit of these models. The comparison of goodness of fit was examined by chi-square tests, the root mean square error of approximation (RMSEA),37 and the comparative fit index (CFI).38
Following recommendations for nested model designs,36 the starting point of the panel wave analysis was the estimation of the model consisting solely of autocorrelations, ie, the correlations between earlier and later time points within the variables (paranoia, negative cognition, and depressed mood). We then tested hypotheses through the sequential addition of specific pathways between variables. First, we assessed the significance of changes in model fit resulting from the addition to the autocorrelational model of directional pathways leading from paranoia either to negative cognition or to depressed mood. Next, we assessed the significance of adding to the autocorrelational model the directional pathways leading in the opposite direction, from negative cognition or from depressed mood to paranoia. If the additional pathways in either direction improved model fit significantly, the third step was to assess whether the incorporation of both directions of effect (ie, a reciprocal model) improved fit still further. The guiding principle in this hypothesis testing approach is that if adding a given path does not significantly improve the fit, the model with fewer paths (thereby the more parsimonious) must be regarded as superior.
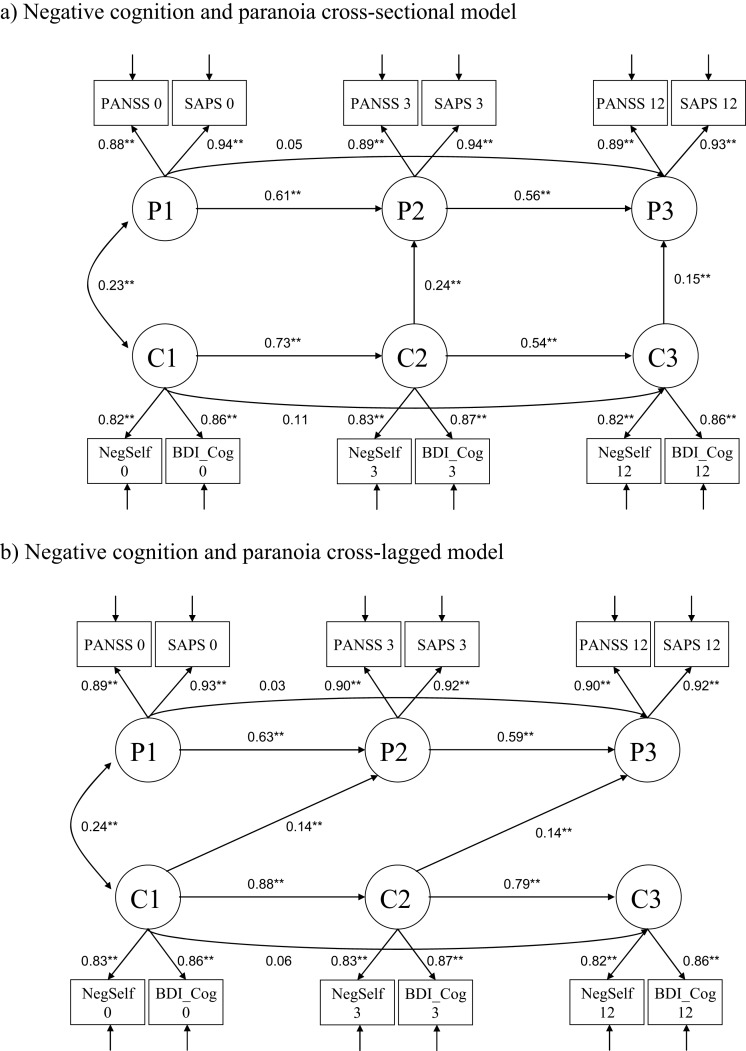
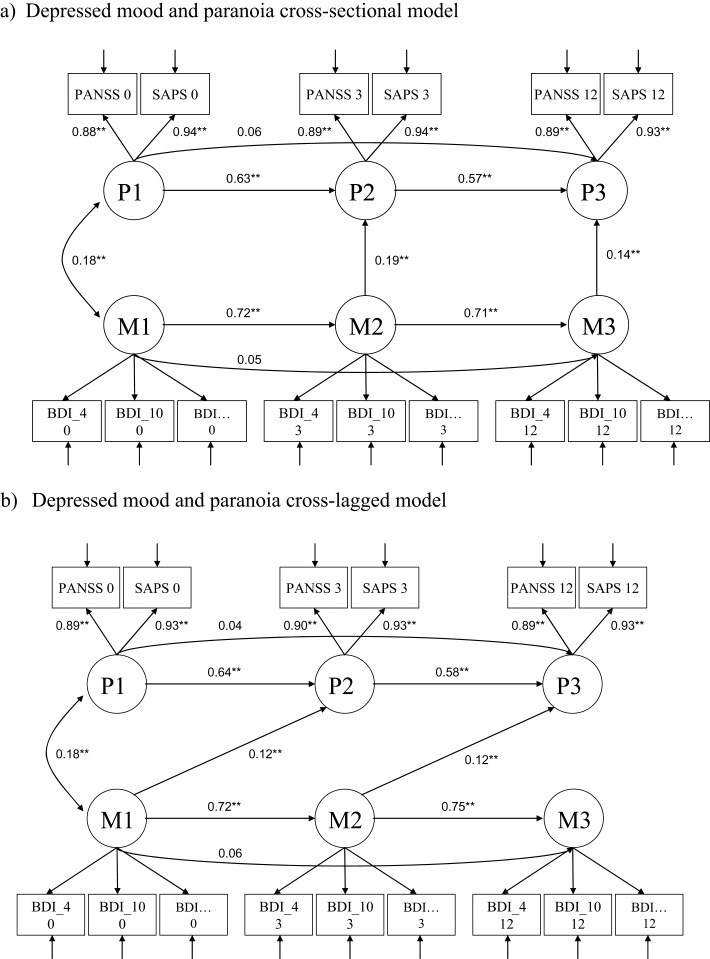
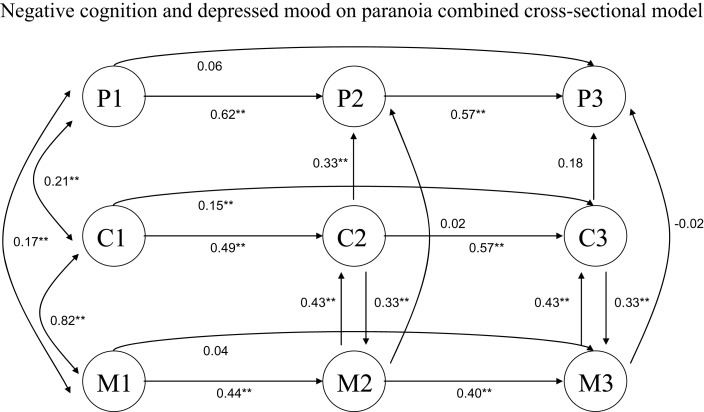
This sequence was followed in the analysis of 3 different kinds of theoretically plausible model, which were set up a priori for testing against the autocorrelational model. To understand these models, it may be helpful to inspect the path diagrams in figures 1–3 in conjunction with the text at this point. The first type was a cross-sectional (sometimes called recursive) model incorporating only the within-time point paths linking paranoia with negative cognition or depressed mood (as in figures 1a and 2a). The second type was a cross-lagged model (as in figures 1b and 2b). These models contained cross-lagged paths between variables at time t and variables at time t + 1. They are a more powerful test of the plausibility of causal directions because of the temporal displacement of the measurements. The third type of model (shown in the tables but not in the figures) included both cross-sectional and cross-lagged links.
Fig. 1.
Negative cognition and paranoia. *P < .05, **P < .01, ***P < 0.001. P1, paranoia at T1; P2, paranoia at T2; P3, paranoia at T3; C1, negative cognition at T1; C2, negative cogniton at T2; C3, negative cognition at T3; Positive and Negative Syndrome Scale (PANSS) 0, PANSS at baseline; PANSS 3, PANSS at 3 months; PANSS 12, PANSS at 12 months; Scale for the Assessment of Positive Symptoms (SAPS) 0, SAPS at baseline; SAPS 3, SAPS at 3 months; SAPS 12, SAPS at 12 months; NegSelf 0, Brief Core Schema Scales (BCSS) negative self at baseline; NegSelf 3, BCSS negative self at 3 months; NegSelf 12, BCSS negative self at 12 months, Beck Depression Inventory (BDI)_Cog 0, BDI-II negative cognition subscale at baseline; BDI_Cog 3, BDI-II negative cognition subscale at 3 months; BDI_Cog 12, BDI-II negative cognition subscale at 12 months; BDI … 0, BDI-II items at baseline; BDI … 3, BDI-II at 3 months; BDI … 12, BDI-II at 12 months.
Fig. 2.
Depressed mood and paranoia. *P < .05, **P < .01, ***P < .001. P1, paranoia at T1; P2, paranoia at T2; P3, paranoia at T3; M1, depressed mood at T1; M2, depressed mood at T2; M3, depressed mood at T3.
Fig. 3.
Negative cognition and depressed mood on paranoia combined cross sectional model. *P < .05, **P < .01, ***P < .001. P1, paranoia at T1; P2, paranoia at T2; P3, paranoia at T3; C1, negative cognition at T1; C2, negative cognition at T2; C3, negative cognition at T3; M1, depressed mood at T1; M2, depressed mood at T2; M3, depressed mood at T3.
Finally, in figure 3, we illustrate a model showing the impact on paranoia of depressed mood and negative cognition in combination. The purpose of this model was to test the hypotheses that negative cognition would have the strongest independent associations with paranoia and would mediate the effect of the affective-somatic dimension of depressed mood on paranoia.
Models with RMSEA values below 0.08 are considered to have a good fit, those with values above 0.10 indicating a poor fit. CFI values above 0.90 and nonsignificant chi-square values also indicate a good fit to the data. However, as the chi-square statistic is dependent on sample size, and likely to reject well-fitting models in moderately large samples such as ours,39 the use of multiple measures of fit was deemed appropriate. The key statistic used to evaluate tests of hypotheses relating to changes in model fit as a result of adding in directional pathways in this study was the significance of differences in chi-square values between autocorrelational and directional pathway models. Participants with incomplete data were included in the analysis on the assumption that the data were missing at random.
Results
Descriptive Statistics
The mean scores for the psychotic symptom, schema, and depression measures are presented in table 1. Fifty-four percent of the sample reported persecutory delusions rated moderate to severe on the SAPS.
Table 1.
Means and SD for All Variables
| Time 1 (Baseline) | Time 2 (3 mo) | Time 3 (12 mo) | |||||||
| N | Mean | SD | N | Mean | SD | N | Mean | SD | |
| PANSS paranoia | 301 | 3.49 | 1.65 | 257 | 2.95 | 1.68 | 248 | 2.88 | 1.65 |
| SAPS persecution | 301 | 2.35 | 1.80 | 258 | 1.74 | 1.76 | 248 | 1.69 | 1.70 |
| BCSS negative self | 255 | 7.19 | 5.89 | 221 | 6.11 | 5.89 | 211 | 5.50 | 5.59 |
| BCSS negative other | 253 | 8.97 | 6.81 | 217 | 8.10 | 7.42 | 207 | 6.97 | 6.60 |
| BDI-II | 272 | 22.17 | 13.15 | 238 | 20.30 | 13.45 | 226 | 16.84 | 13.39 |
Note: PANSS, Positive and Negative Syndrome Scale; SAPS, Scale for the Assessment of Positive Symptoms; BCSS, Brief Core Schema Scales; BDI-II, Beck Depression Inventory. All participants had to have data at at least one time point to be included in the modeling.
Structural Equation Modeling
Negative Cognition and Paranoia.
The overall fit was good for all models under all criteria, except for the RMSEA criterion for the cross-sectional model linking paranoia to negative cognition (table 2).
Table 2.
Cross-Sectional and Cross-Lagged Models Linking Negative Cognition and Paranoia
| χ 2 | df | RMSEA | CFI | Δχ 2 | |
| Cross-sectional | |||||
| Baseline (autocorrelational) model | 160.9 | 54 | 0.08 | 0.95 | |
| Model 1 (paranoia to negative self-schemas) | 175.3 | 53 | 0.09 | 0.94 | |
| Difference between baseline and Model 1 | 1 | 14.42*** | |||
| Model 2 (negative self-schemas to paranoia) | 154.2 | 53 | 0.08 | 0.95 | |
| Difference between baseline and Model 2 | 1 | −6.73*** | |||
| Cross-lagged | |||||
| Baseline (autocorrelational) model | 160.9 | 54 | 0.08 | 0.95 | |
| Model 1 (paranoia to negative self-schemas) | 157.2 | 53 | 0.08 | 0.95 | |
| Difference between baseline and Model 1 | 1 | −3.65 | |||
| Model 2 (negative self-schemas to paranoia) | 149.8 | 53 | 0.08 | 0.95 | |
| Difference between baseline and Model 2 | 1 | −11.11*** | |||
| Cross-sectional and cross-lagged combined | |||||
| Baseline model | 160.9 | 54 | 0.08 | 0.95 | |
| Model 1 (paranoia to negative cognition) | 157.8 | 52 | 0.08 | 0.95 | |
| Difference between baseline and Model 1 | 2 | −3.14 | |||
| Model 2 (negative cognition to paranoia) | 150.6 | 52 | 0.08 | 0.95 | |
| Difference between baseline and Model 2 | 2 | −10.31** | |||
Note: RMSEA, root mean square error of approximation; CFI, comparative fit index.
There was no evidence in support of directional pathways leading from paranoia to negative cognition. Compared with the autocorrelational model, the cross-lagged model was not significantly different, while the cross-sectional model incorporating these pathways was actually a significantly worse fit.
Conversely, and consistent with our hypothesis, in both cross-sectional and cross-lagged models, the inclusion of pathways leading from negative self-schemas to paranoia fitted significantly better than the autocorrelational model (table 2). This was true also of the model incorporating both cross-sectional and cross-lagged pathways. However, this model did not represent a significant improvement in fit over the cross-sectional model (Δχ2 = 3.6; df = 1; P = .06) or the cross-lagged model (Δχ2 = −0.2; df = 1; P = .65). Moreover, it is less parsimonious than models incorporating either cross-sectional or cross-lagged paths. The best-fitting models are therefore the cross-sectional model, in which negative cognition predicts paranoia within time points, as shown in figure 1a and the equivalent cross-lagged model in figure 1b.
We also tested models with reciprocal pathways linking negative cognition and paranoia, not included in the figures or tables. The cross-sectional version was not significantly different from the unidirectional cross-sectional model presented in figure 1a. However, the reciprocal cross-lagged model, ie, one including pathways going forward in time, and linking both negative self-schemas with paranoia, and paranoia with negative self-schemas, fitted the data well (χ2 [52] = 145.22, P > .05; CFI = 0.96; RMSEA = 0.08). This represented a relatively small but significant improvement in fit over the unidirectional model linking negative self-schemas to paranoia, as shown in figure 1b (Δχ2 = 4.6; df = 1; P = .03). This raises the possibility that while the predominant direction is clearly from negative cognition to paranoia, there may be some additional contribution from reciprocal relationships.
Depressed Mood and Paranoia.
Goodness of fit indices for cross-sectional and cross-lagged models linking depressed mood and paranoia are shown in table 3, while the models themselves are illustrated in figure 2. There was a consistent discrepancy in the indices, in that fit appeared good using RMSEA, but was poor when assessed by the CFI. Despite this, the overall pattern of results was similar to that for negative cognition. Thus, models incorporating pathways leading from paranoia to depressed mood did not fit the data significantly better than the autocorrelational model. (In fact, the model incorporating cross-sectional paths was significantly worse). By contrast, there were significant improvements in model fit with the addition of either cross-sectional or cross-lagged pathways leading from depressed mood to paranoia. The coefficients in the depressed mood to paranoia pathways were all significant (0.19 and 0.14, respectively, in the cross-sectional model and 0.12 and 0.12, respectively, in the cross-lagged model). Table 3 also displays the model incorporating both cross-sectional and cross-lagged pathways. Again, the model did not significantly improve fit over the cross-sectional model (Δχ2 = 0.2; df = 1; P = .65) or the cross-lagged model (Δχ 2 = −1.4; df = 1; P = .24).
Table 3.
Cross-Sectional and Cross-Lagged Models Linking Depressed Mood and Paranoia
| χ 2 | df | RMSEA | CFI | Δχ 2 | |
| Cross-sectional | |||||
| Baseline (autocorrelational) model | 1489.4 | 815 | 0.05 | 0.86 | |
| Model 1 (paranoia to depressed mood) | 1494.7 | 814 | 0.05 | 0.86 | |
| Difference between baseline and Model 1 | 1 | 5.30** | |||
| Model 2 (depressed mood to paranoia) | 1483.2 | 814 | 0.05 | 0.86 | |
| Difference between baseline and Model 2 | 1 | −6.21** | |||
| Cross-lagged | |||||
| Baseline (autocorrelational) model | 1489.4 | 815 | 0.05 | 0.86 | |
| Model 1 (paranoia to depressed mood) | 1489.2 | 814 | 0.05 | 0.86 | |
| Difference between baseline and Model 1 | 1 | −0.24 | |||
| Model 2 (depressed mood to paranoia) | 1481.6 | 814 | 0.05 | 0.86 | |
| Difference between baseline and Model 2 | 1 | −7.81** | |||
| Cross-sectional and cross-lagged combined | |||||
| Baseline model | 1489.4 | 815 | 0.05 | 0.86 | |
| Model 1 (paranoia to low mood) | 1486.7 | 813 | 0.05 | 0.86 | |
| Difference between baseline and Model 1 | 2 | −2.70 | |||
| Model 2 (low mood to paranoia) | 1483.0 | 813 | 0.05 | 0.86 | |
| Difference between baseline and Model 2 | 2 | −6.42** | |||
Note: Abbreviations are explained in the footnote to table 2.
The inclusion of reciprocal pathways did not significantly add to the unidirectional models linking depressed mood to paranoia, whether cross-sectional or cross-lagged.
Negative Cognition, Depressed Mood, and Paranoia.
In order to determine how mood and cognition combine in the maintenance of paranoia, we carried out a more complex panel analysis. This included all 3 latent variables (negative self-schemas and depressed mood as independent variables and paranoia as the dependent variable). The best-fitting model is illustrated in figure 3 and indicates that mood and cognition were reciprocally associated. However, only negative cognition had an additional and independent association with paranoia, with a significant coefficient of .33 in the pathway from negative cognition to paranoia. The fit of the overall model was ambiguous, being good only in respect of the RMSEA criterion (χ 2 [1068] = 2099.03, P < .05; CFI = 0.84; RMSEA = 0.06).
Models Incorporating Other Negative Schema Factors
We also ran models using factors derived from other combinations of BCSS subscales. Strikingly, they all followed the same pattern, in that, paranoia was predicted by every type of negative belief factor used, but the reverse was never true. However, the fit for the models using these combinations of BCSS subscales as the negative schema factor was weaker than for those using the factor restricted to negative beliefs about the self. The fit of the cross-lagged model using the schema latent variable combining negative self and lack of positive self (loadings 0.67 and 0.53, respectively) was denoted by chi-square = 164.43, df = 53, P < .0001, CFI = 0.93, RMSEA = 0.08. The fit of the cross-lagged model using the schema latent variable deriving from combining all BCSS subscales was denoted by chi-square = 600.07, P < .001, CFI = 0.79, RMSEA = 0.11.
Discussion
Affective dysregulation is very common even in so-called nonaffective psychosis. The concept of depression incorporates distinguishable emotional and cognitive components. In this study, we used our cognitive model of psychosis to derive key hypotheses linking paranoia to these components,2,4,11,27 which we then tested in people identified by having experienced a psychotic relapse. Seventy percent were male, typical of samples acquired in this way. While this was a treatment trial, there were no overall differences between the control and experimental groups in the variables tested here. It was therefore justifiable to treat the whole sample as a cohort. Specifically, we hypothesized that there would be clear evidence supporting directional pathways leading from negative cognition and depressed mood to paranoid symptoms and that negative cognition would comprise the component of affective dysregulation directly responsible for this relationship.
The results from the modeling were consistent with our hypotheses. Both cross-sectional and cross-lagged analyses indicated that models based on pathways where the direction was from negative cognition or depressed mood to paranoid symptoms had a better fit than those where the pathways ran in the opposite direction. Indeed, these analyses provided no evidence whatsoever that adding pathways leading from paranoia to depressed mood or to negative cognition significantly improved fit over an autocorrelational model. The direction of effect suggested by this modeling is therefore that hypothesized, viz, from negative cognition and depressed mood to paranoia. There was however some indication of weak reciprocal relationships, over and above the unidirectional pathway from negative cognition to paranoia. This would be credible as cognitive processes in psychosis are likely to be complex and to some degree transactive. Under some circumstances, a state of paranoia is likely to make self-critical and negative thinking about the self-worse, and this is not inconsistent with our cognitive model of paranoia. Nevertheless, evidence for reciprocal pathways was inconsistent: The overall pattern of findings from our study is clearly consonant with the interpretation that the dominant direction of effect is from self-critical and negative thinking, and from depressed mood, to paranoia.
These observations represent a significant advance over cross-sectional studies, where assumptions of the directionality of association must be especially tentative. All cross-sectional and cross-lagged models corroborated our hypotheses. However, the results from the cross-lagged analyses have particular value as they identify the sort of effects over time that can most plausibly be interpreted as causal.
This consistent direction of pathway was also observed in models combining both cross-sectional and cross-lagged pathways. In these models, the coefficients for the cross-lagged pathways were still apparent but no longer contributed significantly. It must however be remembered that models incorporating both cross-sectional and cross-lagged pathways are less parsimonious than those based solely on cross-lagged relationships.
Nevertheless, it is worth considering the implications. If, as appears, the strength of the cross-sectional relationships swamp the effects that operate between time points, the effects seen in models based solely on cross-lagged relationships could merely be an artifact of suppressing the cross-sectional pathways. The latter of course have less authority in the postulation of causal direction. However, if so, it would require an explanation (1) for the consistency of the cross-lagged pathways linking both depressed mood and negative self-schemas with paranoia and (2) for the conspicuous absence of links in the reverse direction in any of the cross-sectional models. Moreover, the models based solely on cross-sectional relationships mirror the findings for the cross-lagged relationships.
Thus, a more persuasive account may be that the relationship between, say, cognition at time t and paranoia at time t + 1 was mediated by cognition at time t + 1 (mediation therefore, not by another variable, but by the same variable at a different time). In particular, these results are what would be expected if the observed directions of effect were genuinely causal but operated over a much shorter period than the interval between measurements in the present study (cf.).40,41 The strong cross-sectional pathways would then arise because of a causal effect of depressed mood and negative self-schemas on paranoia and of autocorrelation between closely adjacent levels of paranoia. Supporting evidence for this interpretation comes from the use of the experience sampling method by the Maastricht group.42–44 In these studies, clear affective responses to minor stress were paralleled by moment-to-moment variation in subtle positive psychotic experiences, in a manner consistent with the present study.
The findings of our study also chime with cross-sectional studies reporting that negative schematic beliefs are associated with the persistence of paranoia14,15,28 and the observations of the influence of depression and anxiety on the evolution of psychosis from nonclinical longitudinal studies on epidemiological cohorts.24,40,41,45–49
The central role of negative cognition in mediating the effects of depressed mood on paranoia was also corroborated by our results. When we fitted models analyzing depressed mood, negative cognition, and paranoia together, the best fit involved reciprocal associations between mood and negative cognition, but the final common pathway to paranoia was specifically via negative cognition. Depressed mood had no independent association with paranoia in the presence of negative cognition. This was consistent with our secondary hypothesis that negative cognition would mediate the link between depressed mood and paranoia.
It should be noted that the negative cognition latent variable favored in our analyses derives both from the negative beliefs about self-subscale and from the cognitive factor derived from the BDI-II. The latter does contain elements reflecting mood rather than cognition, and some of the variance captured by the latent variable might therefore be dependent on this element rather than on cognition. However, this is relatively implausible: The BDI-II cognitive factor is dominated by cognitive items, and the original factor analysis suggested that it is these items that most strongly carry the variance (hence the term ‘cognitive factor’). The latent variable most closely based on mood items in the BDI-II had effects that were clearly mediated by the cognitive variable. Finally, we ran models using a negative cognition variable that excluded BDI-II items and was entirely cognitive. This produced similar, although weaker, results.
The present longitudinal study represents a considerable advance on cross-sectional studies. Traditional models of psychosis propose that depressed mood and negative self-evaluative thinking are simply epiphenomena and thus of no etiological importance. However, the most plausible explanation of our findings across all models is of a causal effect of self-critical and extreme negative thinking and of depressed mood on paranoia in people with established nonaffective psychosis. Nevertheless, although the longitudinal design is persuasive, the study is still correlational and thus subject to reservations about the interpretation of relationships. Moreover, although the dominant models clearly represented the best fit to the data, the fit of some models (in particular, the combined model in figure 3) was ambiguous, with discrepancies between the conventional indices of fit. Nor can we rule out confounding by unmeasured variables. The ultimate test must therefore be experimental.
Our results are consistent with other studies suggesting that the influence of social life events and family environment operate via effects on self and other appraisal and emotional dysfunction.50–52 Some experimental manipulations of controlled environments have been carried out and are also consistent with these hypotheses.53–56 In summary, there is increasingly strong evidence that depressed and anxious mood states and the associated self-critical and extreme negative thinking about self and others may contribute to the symptoms of paranoia occurring in people with established nonaffective psychosis. The findings have important clinical implications: They provide further support for the use of CBT for psychosis, which already incorporates targeted therapeutic strategies to address extreme negative thinking about self and others.57
Funding
Wellcome Trust Programme Grant (062452).
Acknowledgments
We thank all the patient participants, the staff of the Camden and Islington Mental Health and Social Care NHS Trust, North East London Mental Healthcare Trust, Norfolk and Waveney Mental Health Partnership NHS Trust, South London, and Maudsley NHS Foundation Trust. E.K. and P.G. acknowledge support for their clinical sessions from the NIHR Biomedical Research Centre for Mental Health at the South London and Maudsley NHS Foundation Trust and (Institute of Psychiatry) Kings College London. The Authors have declared that there are no conflicts of interest in relation to the subject of this study.
References
- 1.Birchwood M. Pathways to emotional dysfunction in first episode psychosis. Br J Psychiatry. 2003;182:373–375. [PubMed] [Google Scholar]
- 2.Fowler D. Psychological formulation of early psychosis: a cognitive model. In: Birchwood M, Fowler D, Jackson C, editors. Early Intervention in Psychosis. Chichester, UK: John Wiley and Sons; 2000. pp. 101–127. [Google Scholar]
- 3.Fowler D, Freeman D, Steel C, et al. The catastrophic interaction hypothesis: how do stress, trauma, emotion and information processing abnormalities lead to psychosis. In: Morrison A, Larkin W, editors. Trauma and Psychosis. Chichester, UK: John Wiley and Sons; 2006. pp. 101–124. [Google Scholar]
- 4.Garety PA, Kuipers EK, Fowler D, Freeman D, Bebbington PE. A cognitive model of the positive symptoms of psychosis. Psychol Med. 2001;31:189–195. doi: 10.1017/s0033291701003312. [DOI] [PubMed] [Google Scholar]
- 5.Garety PA, Bebbington P, Fowler D, Freeman D, Kuipers E. Implications for neurobiological research of cognitive models of psychosis: a theoretical paper. Psychol Med. 2007;37:1377–1391. doi: 10.1017/S003329170700013X. [DOI] [PubMed] [Google Scholar]
- 6.Morrison AP. The interpretation of intrusions in psychosis: an integrative cognitive approach to hallucinations and delusions. Behav Cogn Psychother. 2001;29:257–276. [Google Scholar]
- 7.Bentall RP, Corcoran R, Howard R, Blackwood N, Kinderman P. Persecutory delusions: a review and theoretical integration. Clin Psychol Rev. 2001;21:1143–1192. doi: 10.1016/s0272-7358(01)00106-4. [DOI] [PubMed] [Google Scholar]
- 8.Freeman D, Garety P, Kuipers E, Fowler D, Bebbington PE. A cognitive model of persecutory delusions. Br J Clin Psychol. 2002;41:331–347. doi: 10.1348/014466502760387461. [DOI] [PubMed] [Google Scholar]
- 9.Morrison AP, Wells A, Nothard S. Cognitive and emotional predictors of predisposition to hallucinations in nonpatients. Br J Clin Psychol. 2002;41:259–270. doi: 10.1348/014466502760379127. [DOI] [PubMed] [Google Scholar]
- 10.Birchwood M, Trower P. The future of cognitive-behavioural therapy for psychosis: not a quasi-neuroleptic. Br J Psychiatry. 2006;188:107–108. doi: 10.1192/bjp.bp.105.014985. [DOI] [PubMed] [Google Scholar]
- 11.Freeman D, Garety PA. Connecting neurosis and psychosis: the direct influence of emotion on delusions and hallucinations. Behav Res Ther. 2003;41:923–947. doi: 10.1016/s0005-7967(02)00104-3. [DOI] [PubMed] [Google Scholar]
- 12.Guillem F, Pampoulova T, Stip E, Lalonde P, Todorov C. The relationship between symptom dimensions and dysphoria in schizophrenia. Schizophr Res. 2005;75:83–96. doi: 10.1016/j.schres.2004.06.018. [DOI] [PubMed] [Google Scholar]
- 13.Häfner H, Maurer K, Trendler G, der Heiden Wan, Schmidt M, Konnecke R. Schizophrenia and depression: challenging the paradigm of two separate diseases—a controlled study of schizophrenia, depression and healthy controls. Schizophr Res. 2005;77:11–24. doi: 10.1016/j.schres.2005.01.004. [DOI] [PubMed] [Google Scholar]
- 14.Barrowclough C, Tarrier N, Humphreys L, et al. Self-esteem in schizophrenia: relationships between self-evaluation, family attitudes, and symptomatology. J Abnorm Psychol. 2003;112:92–99. [PubMed] [Google Scholar]
- 15.Bentall RP, Rowse G, Shryane N, et al. The cognitive and affective structure of paranoid delusions: a transdiagnostic investigation of patients with schizophrenia spectrum disorders and depression. Arch Gen Psychiatry. 2009;66:236–247. doi: 10.1001/archgenpsychiatry.2009.1. [DOI] [PubMed] [Google Scholar]
- 16.Bowins B, Shugar G. Delusions and self-esteem. Can J Psychiatry. 1998;43:154–158. doi: 10.1177/070674379804300204. [DOI] [PubMed] [Google Scholar]
- 17.Close H, Garety PA. Cognitive assessment of voices: further developments in understanding the emotional impact of voices. Br J Clin Psychol. 1998;37:173–188. doi: 10.1111/j.2044-8260.1998.tb01292.x. [DOI] [PubMed] [Google Scholar]
- 18.Drake RJ, Pickles A, Bentall RP, et al. The evolution of insight, paranoia and depression during early schizophrenia. Psychol Med. 2004;34:285–292. doi: 10.1017/s0033291703008821. [DOI] [PubMed] [Google Scholar]
- 19.Freeman D, Garety PA, Fowler D, et al. The London-East Anglia randomised controlled trial of cognitive-behaviour therapy for psychosis: IV. Self-esteem and persecutory delusions. Br J Clin Psychol. 1998;37:415–430. doi: 10.1111/j.2044-8260.1998.tb01399.x. [DOI] [PubMed] [Google Scholar]
- 20.Freeman D, Slater M, Bebbington PE, et al. Can virtual reality be used to investigate persecutory ideation? J Nerv Ment Dis. 2003;191:509–514. doi: 10.1097/01.nmd.0000082212.83842.fe. [DOI] [PubMed] [Google Scholar]
- 21.Hall Pl, Tarrier N. The cognitive behavioural treatment of low self-esteem in psychotic patients: a pilot study. Behav Res Ther. 2003;41:317–322. doi: 10.1016/s0005-7967(02)00013-x. [DOI] [PubMed] [Google Scholar]
- 22.Iqbal Z, Birchwood M, Chadwick P, Trower P. Cognitive approach to depression and suicidal thinking in psychosis: 2. Testing the validity of a social ranking model. Br J Psychiatry. 2000;177:522–528. [PubMed] [Google Scholar]
- 23.Krabbendam L, Janssen I, Bijl RV, Vollerburgh WAM, van Os J. Neuroticism and low self-esteem as risk factors for psychosis. Soc Psychiatry Psychiatr Epidemiol. 2002;37:1–6. doi: 10.1007/s127-002-8207-y. [DOI] [PubMed] [Google Scholar]
- 24.Krabbendam L, Myin-Germeys I, Hanssen M, et al. Development of depressed mood predicts onset of psychotic disorder in individuals who report hallucinatory experiences. Br J Clin Psychol. 2005;44:113–125. doi: 10.1348/014466504X19767. [DOI] [PubMed] [Google Scholar]
- 25.Martin JA, Penn DL. Brief report: social cognition and subclinical paranoid ideation. Br J Clin Psychol. 2001;40:261–265. doi: 10.1348/014466501163670. [DOI] [PubMed] [Google Scholar]
- 26.Trower P, Chadwick PDJ. Pathways to defence of the self: a theory of two types of paranoia. Clin Psychol: Sci Pract. 1995;2:263–278. [Google Scholar]
- 27.Fowler DG, Freeman D, Smith B, et al. The Brief Core Schema Scales (BCSS): psychometric properties and associations with paranoia and grandiosity in non-clinical and psychosis samples. Psychol Med. 2006;36:749–759. doi: 10.1017/S0033291706007355. [DOI] [PubMed] [Google Scholar]
- 28.Smith B, Fowler DG, Freeman D, et al. Emotion and psychosis: links between depression, self-esteem, negative schematic beliefs and delusions and hallucinations. Schizophr Res. 2006;86:181–188. doi: 10.1016/j.schres.2006.06.018. [DOI] [PubMed] [Google Scholar]
- 29.Garety PA, Fowler D, Freeman D, Bebbington P, Dunn G, Kuipers E. A randomised controlled trial of cognitive behavioural therapy and family intervention for the prevention of relapse and reduction of symptoms in psychosis. Br J Psychiatry. 2008;192:412–423. doi: 10.1192/bjp.bp.107.043570. [DOI] [PubMed] [Google Scholar]
- 30.Andreasen NC. The Scale for the Assessment of Positive Symptoms (SAPS) Iowa City, IA: The University of Iowa; 1984. [Google Scholar]
- 31.Kay SR. Positive and Negative Syndromes in Schizophrenia: Assessment and Research. New York, NY: Brunner/Mazel; 1991. [Google Scholar]
- 32.Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- 33.Fialko L, Freeman D, Bebbington PE, et al. Understanding suicidal ideation in psychosis: findings from the Psychological Prevention of Relapse in Psychosis (PRP) Trial. Acta Psychiatr Scand. 2006;114:177–186. doi: 10.1111/j.1600-0447.2006.00849.x. [DOI] [PubMed] [Google Scholar]
- 34.Addington D, Addington J, Maticka-Tyndale E. Assessing depression in schizophrenia: the Calgary Depression Scale. Br J Psychiatry Suppl. 1993;22:S39–S44. [PubMed] [Google Scholar]
- 35.Muthén LK, Muthén BO. Mplus User′s Guide. Los Angeles, CA: Muthén & Muthén; 2007. [Google Scholar]
- 36.Hoyle RH, Panter AT. Writing about structural equation models. In: Hoyle RH, editor. Structural Equation Modeling. Thousand Oaks, CA: Sage; 1995. pp. 158–176. [Google Scholar]
- 37.Steiger JE. Structural model evaluation and modification. Multivar Behav Res. 1990;25:173–180. doi: 10.1207/s15327906mbr2502_4. [DOI] [PubMed] [Google Scholar]
- 38.Bentler PM. Fit indexes, Lagrange multipliers, constraint changes and incomplete data in structural models. Multivar Behav Res. 1990;25:163–172. doi: 10.1207/s15327906mbr2502_3. [DOI] [PubMed] [Google Scholar]
- 39.Tanaka JS. How big is big enough?: sample size and goodness of fit in structural equation models with latent variables. Child Dev. 1987;58:134–146. [Google Scholar]
- 40.Krabbendam L, Myin-Germeys I, Hanssen M, et al. Hallucinatory experiences and onset of psychotic disorder: evidence that the risk is mediated by delusion formation. Acta Psychiatr Scand. 2004;110:264–272. doi: 10.1111/j.1600-0447.2004.00343.x. [DOI] [PubMed] [Google Scholar]
- 41.Wiles NJ, Zammit S, Bebbington P, Singleton N, Meltzer H, Lewis G. Self-reported psychotic symptoms in the general population. Br J Psychiatry. 2006;188:519–526. doi: 10.1192/bjp.bp.105.012179. [DOI] [PubMed] [Google Scholar]
- 42.Myin-Germeys I, van Os J, Schwartz JE, Stone AA, Delespaul PA. Emotional reactivity to daily life stress in psychosis. Arch Gen Psychiatry. 2001;58:1137–1144. doi: 10.1001/archpsyc.58.12.1137. [DOI] [PubMed] [Google Scholar]
- 43.Myin-Germeys I, Delespaul P, van Os J. Behavioural sensitization to daily life stress in psychosis. Psychol Med. 2005;35:733–741. doi: 10.1017/s0033291704004179. [DOI] [PubMed] [Google Scholar]
- 44.Myin-Germeys I, van Os J. Stress-reactivity in psychosis: evidence for an affective pathway to psychosis. Clin Psychol Rev. 2007;27:409–424. doi: 10.1016/j.cpr.2006.09.005. [DOI] [PubMed] [Google Scholar]
- 45.Cooper C, Morgan C, Byrne M, et al. Perceptions of social disadvantage, ethnicity and psychosis: results from the AESOP study. Br J Psychiatry. 2008;192:185–190. doi: 10.1192/bjp.bp.107.042291. [DOI] [PubMed] [Google Scholar]
- 46.Kuipers E, Bebbington P, Dunn G, et al. Influence of carer expressed emotion and affect on relapse in non-affective psychosis. Br J Psychiatry. 2006;188:173–179. doi: 10.1192/bjp.bp.104.007294. [DOI] [PubMed] [Google Scholar]
- 47.Birchwood M, Gilbert P, Gilbert J, et al. Interpersonal and role-related schema influence the relationship with the dominant ‘voice’ in schizophrenia: a comparison of three models. Psychol Med. 2004;34:1571–1580. doi: 10.1017/s0033291704002636. [DOI] [PubMed] [Google Scholar]
- 48.Krabbendam L, Myin-Germeys I, Bak M, van Os J. Explaining transitions over the hypothesized psychosis continuum. Aust N Z J Psychiatry. 2005;39:180–186. doi: 10.1080/j.1440-1614.2005.01541.x. [DOI] [PubMed] [Google Scholar]
- 49.Hanssen M, Krabbendam L, de Graaf R, Vollebergh W, van Os J. Role of distress in delusion formation. Br J Psychiatry Suppl. 2005;48:s55–s58. doi: 10.1192/bjp.187.48.s55. [DOI] [PubMed] [Google Scholar]
- 50.Brown GW, Birley JLT. Crises and life changes and the onset of schizophrenia. J Health Soc Behav. 1968;9:203–214. [PubMed] [Google Scholar]
- 51.Bebbington PE, Kuipers L. The predictive utility of expressed emotion in schizophrenia: an aggregate analysis. Psychol Med. 1994;24:707–718. doi: 10.1017/s0033291700027860. [DOI] [PubMed] [Google Scholar]
- 52.Tarrier N, Vaughn C, Lader M, Leff J. Bodily reactions to people and events in schizophrenics. Arch Gen Psychiatry. 1979;36:311–315. doi: 10.1001/archpsyc.1979.01780030077007. [DOI] [PubMed] [Google Scholar]
- 53.Freeman D. Studying and treating schizophrenia using virtual reality (vr): a new paradigm. Schizophr Bull. 2008;34:605–610. doi: 10.1093/schbul/sbn020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Freeman D, Pugh K, Antley A, et al. A virtual reality study of paranoid thinking in the general population. Br J Psychiatry. 2008;192:258–263. doi: 10.1192/bjp.bp.107.044677. [DOI] [PubMed] [Google Scholar]
- 55.Valmaggia LR, Freeman D, Green C, et al. Virtual reality and paranoid ideations in people with an ‘at-risk mental state’ for psychosis. Br J Psychiatry. 2007;191:63–68. doi: 10.1192/bjp.191.51.s63. [DOI] [PubMed] [Google Scholar]
- 56.Freeman D, Pugh K, Vorontsova N, Antley A, Slater M. Testing the continuum of delusional beliefs: an experimental study using virtual reality. J Abnorm Psychol. 2010;119:83–92. doi: 10.1037/a0017514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Fowler D, Garety PA, Kuipers L. Cognitive Behaviour Therapy for Psychosis. Chichester, UK: John Wiley and Sons; 1995. [Google Scholar]