Background
Cognitive behavioral therapy (CBT) is now a recommended treatment for people with schizophrenia. In CBT, links are made between the person’s feelings and patterns of thinking that underpin their distress. At present, a variety of interventions have been labeled as CBT and it is difficult to provide a single, unambiguous definition. In recognition, the review authors have constructed criteria that are felt to be both workable and to capture the elements of good practice in CBT.
Cognitive behavioral therapy is becoming increasingly available for people with schizophrenia, with recent recommendations of treatment guidelines in, for example, the United Kingdom suggesting that CBT should be more widely available for people with schizophrenia.
It should be noted that many of the trials of CBT for psychosis have incorporated additional active therapeutic elements (eg, psychoeducation and relapse prevention) that would be considered adjunctive to techniques that are specifically targeted at eliciting belief change (eg, guided discovery or behavioral experiments).
The comparison arm of the trials reported other psychosocial therapies, such as supportive therapy, psychoeducation, family therapy, and other “talking therapies.” The full review distinguishes between trials that described “active” psychosocial interventions (eg, family therapy) aimed at a meaningful symptom reduction and those trials that have used “nonactive” psychosocial interventions (eg, supportive therapy), which act as merely a control for the nonspecific effects of therapy (eg, time spent with therapist). Outcomes are presented separately for active and nonactive psychosocial interventions and the pooled effect of these trials is also presented.
Search Methods
We searched the Cochrane Schizophrenia Group Trials Register (March 2010) that is based on regular searches of CINAHL, EMBASE, MEDLINE, and PsycINFO. We inspected all references of the selected articles for further relevant trials, and, where appropriate, contacted authors.
Selection Criteria
All relevant randomized controlled trials of CBT for people with schizophrenia-like illnesses.
Data Collection and Analysis
Studies were reliably selected and assessed for methodological quality. Two review authors, working independently, extracted data. We analyzed dichotomous data on an intention-to-treat basis and continuous data with 65% completion rate are presented. Where possible, for dichotomous outcomes, we estimated a risk ratio (RR) with the 95% confidence interval (CI) along with the number needed to treat/harm.
Main Results
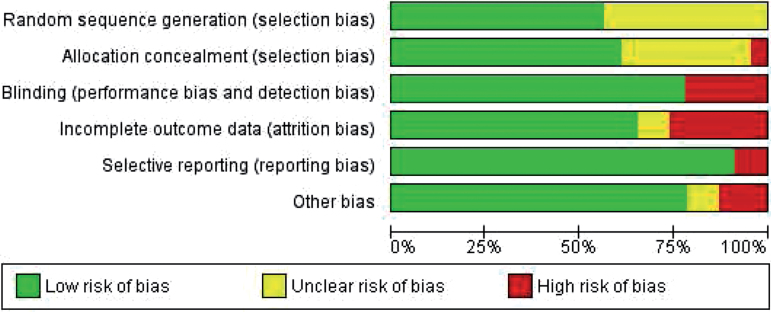
Thirty articles described 20 trials. Trials were often small and of limited quality. In figure 1 the various risks of bias are presented as percentages across all included studies.
Fig. 1.
Risk of bias chart.
The main findings of this review are summarized in table 1. When CBT was compared with other psychosocial therapies, no difference was found for outcomes relevant to adverse effect/events (2 RCTs, n = 202, RR death 0.57 CI 0.12–2.60). Relapse was not either reduced over any time period (5 RCTs, n = 183, RR long term 0.91 CI 0.63–1.32) nor was rehospitalization (5 RCTs, n = 294, RR in longer term 0.86 CI 0.62–1.21). Various global mental state measures failed to show difference (4 RCTs, n = 244, RR no important change in mental state 0.84 CI 0.64–1.09). More specific measures of mental state failed to show differential effects on positive or negative symptoms of schizophrenia, but there may be some long-term effect for affective symptoms (2 RCTs, n = 105, mean difference (MD) Beck Depression Inventory (BDI) −6.21 CI −10.81 to −1.61). Few trials report on social functioning or quality of life. Findings do not convincingly favor either of the interventions (2 RCTs, n = 103, MD Social Functioning Scale (SFS) 1.32 CI −4.90 to 7.54; n = 37, MD EuroQOL −1.86 CI −19.20 to 15.48). For the outcome of leaving the study early, we found no significant advantage when CBT was compared with either nonactive control therapies (4 RCTs, n = 433, RR 0.88 CI 0.63–1.23) or active therapies (6 RCTs, n = 339, RR 0.75 CI 0.40–1.43).
Table 1.
Summary of Findings
| Cognitive behavioral therapy compared with other psychosocial therapies for schizophrenia | ||||||
| Patient or population: patients with schizophreniaSettings: in either community or in hospital settingsIntervention: cognitive behavioral therapyComparison: other psychosocial therapies | ||||||
| Outcomes | Illustrative Comparative Risks a (95% CI) | Relative Effect (95% CI) | No. of Participants (Studies) | Quality of the Evidence (GRADE) | Comments | |
| Assumed Risk | Corresponding Risk | |||||
| Other Psychosocial Therapies | Cognitive Behavioral Therapy | |||||
| Adverse effect/event: 2. Adverse effects—any—medium term only Follow-up: 26–52 weeks | Low 1 | RR 2 (0.71—5.64) | 198 (1 study) | ⊕⊝⊝⊝ very low 2 , 3 , 4 , 5 | ||
| 10 per 1000 | 20 per 1000 (7–56) | |||||
| Moderate 1 | ||||||
| 50 per 1000 | 100 per 1000 (35–282) | |||||
| High 1 | ||||||
| 100 per 1000 | 200 per 1000 (71–564) | |||||
| Global state: 1. Relapse—long term Follow-up: 12 months6 | Low | RR 0.91 (0.63—1.32) | 350 (5 studies) | ⊕⊕⊝⊝low 2 , 5 | ||
| 100 per 1000 | 91 per 1000 (63–132) | |||||
| Moderate | ||||||
| 500 per 1000 | 455 per 1000 (315–660) | |||||
| High | ||||||
| 700 per 1000 | 637 per 1000 (441–924) | |||||
| Global state: 2. Rehospitalization—long term Follow-up: 12 months6 | Low 1 | RR 0.86 (0.62 to 1.21) | 294 (5 studies) | ⊕⊕⊝⊝low 2 , 5 | ||
| 100 per 1000 | 86 per 1000 (62–121) | |||||
| Moderate 1 | ||||||
| 300 per 1000 | 258 per 1000 (186–363) | |||||
| High 1 | ||||||
| 500 per 1000 | 430 per 1000 (310–605) | |||||
| Mental state: 1. General—No important or reliable change—long term Follow-up: 12 months6 | Low 1 | RR 0.84 (0.64 to 1.09) | 244 (4 studies) | ⊕⊝⊝⊝ very low 2 , 5 , 7 | ||
| 400 per 1000 | 336 per 1000 (256–436) | |||||
| Moderate 1 | ||||||
| 600 per 1000 | 504 per 1000 (384–654) | |||||
| High 1 | ||||||
| 800 per 1000 | 672 per 1000 (512–872) | |||||
| Social functioning: 1a. Average scores (Social Functioning Scale, high = good) Follow-up: median 26 weeks | The mean social functioning: 1a. average scores (social functioning scale, high = good) in the intervention groups was 8.8 higher (4.07 lower to 21.67 higher) | 65 (1 study) | ⊕⊝⊝⊝ very low 2 , 5 , 8 | No studies reported “employment” as was prestated to be of interest for the table in review protocol. | ||
| Quality of life: Average score (EuroQOL, high = good)—long term only Follow-up: 26 weeks | The mean quality of life: average score (euroqol, high = good)—long term only in the intervention groups was 1.86 lower (19.2 lower to 15.48 higher) | 37 (1 study) | ⊕⊝⊝⊝ very low 2 , 3 , 5 | |||
a The basis for the assumed risk (eg, the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio.
GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate.
1 Medium risk: roughly equates with that of the trial control groups. 2Limitation in design—rated “serious”: studies short, randomization poorly described, blinding at outcome—single at best and untested. 3Imprecision—rated “serious”: one small study. 4Imprecision—rated “serious”: no other studies made any report of adverse effects. 5Publication bias: rated “likely”: all trials were small—searches may fail to identify other small less positive trials. 6Long term: defined as over 1 year. 7Indirectness—rated “serious”: various measures used with differing criteria. 8Indirectness—rated “serious”: scale derived data—not “employment” as stated in protocol.
Authors’ Conclusions
The use of CBT has been associated with some reduction in symptoms, particularly affective problems associated with having such a serious illness. However, there is considerable variability in the findings of the various studies and, at present, it is not possible to assert any substantial benefit for cognitive behavioral therapy over other psychological therapies. Full details are published in the Cochrane Review (Jones, 2012).
Reference
- Jones C, Hacker D, Cormac I, Meaden A, Irving CB. Cognitive behaviour therapy versus other psychosocial treatments for schizophrenia.Cochrane Database of Systematic Reviews. 2012; doi: 10.1002/14651858.CD008712.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]