Abstract
Background
Research suggests the neighborhood built environment is related to child physical activity and eating.
Purpose
Determine if characteristics of the neighborhood environment moderate the relationship between obesity treatment and weight loss, and if outcomes of particular treatments are moderated by built environment characteristics.
Method
The relationship between the built environment and zBMI changes for 191 8-12 year-old children who participated in one of four randomized, controlled trials of pediatric weight management was assessed using mixed models analysis of covariance.
Results
At 2 year follow-up, greater parkland, fewer convenience stores and fewer supermarkets were associated with greater zBMI reduction across all interventions. No treatments interacted with characteristics of the built environment.
Conclusions
Activity- and eating-related built neighborhood characteristics are associated with child success in behavioral obesity treatments. Efficacy may be improved by individualizing treatments based on built environment characteristics.
Keywords: built environment, weight loss, parkland, neighborhood block size, supermarkets, convenience stores
Research suggests that the built environment around a child’s home is cross-sectionally (1-4) and prospectively (5) related to childhood and adolescent obesity. Childhood obesity is associated with positive energy balance, with energy intake exceeding energy expenditure. Characteristics of the neighborhood built environment such as parkland or open space (2, 5-7), street connectivity (7, 8), housing density and mixed residential land use (6-8) and access to recreational facilities have also been related to physical activity and obesity (1, 9). Similarly, aspects of the food environment are associated with obesity. Greater density of fast-food or convenience stores around residences is associated with greater obesity in children (2-4) and adults (10), while supermarket proximity is associated with a reduced prevalence of obesity (10), presumably due to greater access to healthier foods in supermarkets versus convenience stores (11).
Given the consistent relationships between the built environment and energy balance behaviors, living in built environments with specific characteristics may impact the ability to lose weight or maintain better weight control. The social ecological model is a conceptual approach (12, 13) that describes how environmental factors (14) may interact with interventions to influence weight control. For example, living in environments with accessible parks may make it easier for a child to increase physical activity as part of an exercise program, and thus lose more weight. Similarly, living in environments with easy access to convenience stores that have high energy density snacks and low access to healthier low energy density foods may make it harder to adhere to a healthier low energy density diet. Children who live in environments with these characteristics may be less successful in losing weight.
To our knowledge there is no research on how the built environment impacts the effects of pediatric obesity treatment. We report for the first time the relationship between characteristics of the built environment and pediatric weight management in the context of an established family-based behavioral weight control program in children. The efficacy of family-based treatments has been replicated many times since the late 1970’s (15), and recently we demonstrated that the efficacy of family-based treatments have improved over time (16), despite changes in the environment that may promote obesity and are associated with the increase in the incidence and prevalence of pediatric obesity (17, 18).
Family-based treatment provides a platform to evaluate different treatment approaches to pediatric obesity (15). This paper examines the relationship between characteristics of the built environment and treatment outcome in four randomized controlled trials that include nine different treatments. The treatments included comparing the effectiveness of reducing sedentary behavior versus increasing physical activity (19), assessing the additive effects of including problem solving training in treatment (20), comparing stimulus control versus reinforcing reductions in sedentary behavior as ways to reduce sedentary behavior (21), and assessing the influence of reinforcing alternatives to eating (22). One advantage of including multiple forms of treatment is the opportunity to learn if the built environment moderates outcome of specific treatments, or conversely, if the built environment has strong non-specific effects that are observed across multiple types of treatment. In a short-term field study designed to assess the effect of manipulating sedentary behavior on physical activity we found that parkland moderated the effects of reducing sedentary behavior on physical activity, with greater increases in physical activity for those living close to parks in comparison to children who had no access to parks (23). Based on these data, one hypothesis to explore in the current analyses is that targeting reducing sedentary behavior (19, 21) would show an interaction with the built environment, such as as a greater reduction in sedentary behavior or weight loss for individuals with greater access to parkland. Likewise, it is possible that developing alternatives to food as a reinforcer (22) interacts with characteristics of the food built environment to predict outcome. However, interventions that did not differentially target physical activity or eating and might not interact with characteristics of the built environment. For example, a problem solving intervention (20), that does not differentially target eating or physical activity, may not show the built environment moderated treatment. An alternative hypothesis is that the built environment is a non-specific predictor of treatment outcome across a wide variety of treatments, such as greater weight loss for families who live close to parks or do not live close to convenience stores, independent of what type of treatment they are provided.
Methods
Participants
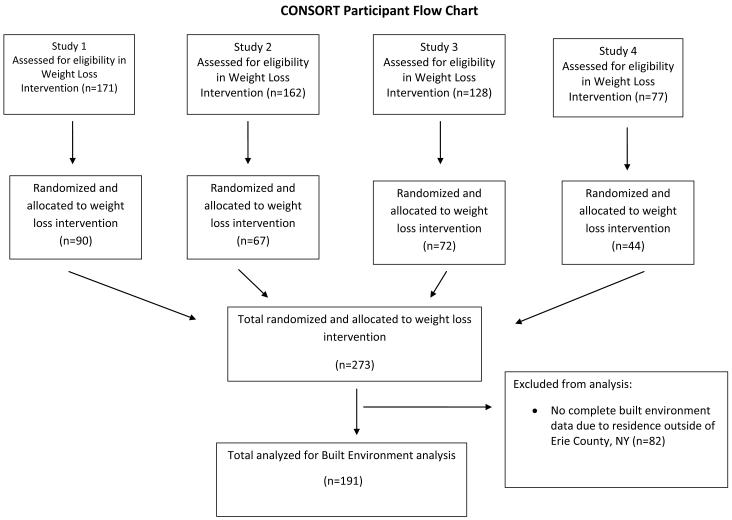
Participants included overweight or obese (> 85th Body Mass Index (BMI) percentile) 8-12 year-old children from 191 families who participated in four randomized, controlled outcome studies, details of which have been presented elsewhere (16). The number of treatment sessions ranged from 16 -20 in each study. The complete sample included 273 families, with 191 families who lived at addresses in Erie County from which we could calculate all the built environment variables (Figure 1).
Figure 1.
CONSORT Flow diagram for the four studies.
Commonalities and differences across studies
The family-based behavioral treatment program for overweight youth is a standardized systematic approach to the design of family-based treatments, with a common core used across all the studies, facilitating the comparison of treatment effects over time. All studies were implemented in a University-based specialized clinic for childhood obesity. In each study a parent was treated along with a child. All families had weekly weigh-in and individual meetings with a therapist, followed by separate parent and child groups. All families were provided treatment manuals that included information on recommended dietary changes based on the Traffic Light Diet, a physical activity program, and information on parenting. The Traffic Light Diet (15) is a comprehensive eating plan for families that is designed to increase nutrient density while it decreases energy intake. Foods are divided into the colors of the Traffic Light based on their energy, fat and/or added sugar content, and children and their parents are provided calorie goals and reducing RED food (high energy dense) goals. Active weight control treatment lasted for 6 months in all studies with follow-ups at 12 and 24 months after randomization. All studies were conceptualized as efficacy studies, and participants who had reported significant psychopathology, who could not read the materials and who could not complete behavioral tasks during screening were excluded from treatment. All children were at least 20% overweight, with an upper limit of 120% overweight (100% overweight is double the average weight for a child of that age and sex).
The first study randomized 90 families to treatment conditions that varied whether increasing physical activity or reducing sedentary behavior was targeted, with low and high doses of each target behavior in a 2 × 2 factorial design. Families were provided 20 sessions of treatment, and there was 16% attrition (19). Results showed that targeting either decreased sedentary behaviors or increased physical activity was associated with significant and similar decreases in percent overweight and body fat, and improved aerobic fitness, supporting the goal of targeting sedentary behaviors as an adjunct in the treatment of pediatric obesity. The second study randomized 67 families to standard family-based treatment plus parent and child problem solving, child problem solving or standard treatment with no problem solving. Families were provided 18 sessions of treatment, with 18% attrition (20). The standard group showed greater BMI decreases than the parent and child group through 2 years, suggesting that problem solving did not add to treatment effectiveness beyond the standard family-based treatment. The third study randomized 72 families to stimulus control or reinforcement to reduce sedentary behaviors. Families were provided 20 sessions of treatment, with a 5% attrition (21). Results suggested stimulus control and reinforcing reduced sedentary behaviors are equivalent ways to decrease sedentary behaviors, and behavioral economic relationships in eating and activity may mediate the effects of treatment. The fourth study randomized 44 families to compare the standard treatment with an experimental treatment that incorporated reinforcing children for engaging in alternative behaviors to eating. Families were provided 16 sessions of treatment, with 15% attrition (22). Results showed significant and maintained reduction in zBMI for both groups, with no significant differences between treatment conditions (Table 1).
Table 1.
Child characteristics, child zBMI and BMI changes and characteristics of the built environement across studies.
| Variable | Study 1 (19) | Study 2 (20) | Study 3(21) | Study 4 (22) | p |
|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||
| Age | 10.4 (1.2) | 10.2 (1.1) | 9.9 (1.2) | 10.1 (1.1) | NS |
| N | 67 | 45 | 52 | 27 | |
| Sex (Male/Female) | 21/46 | 22/23 | 21/31 | 11/16 | NS |
| zBMI | 2.2 (0.3) | 2.2 (0.3) | 2.2 (0.2) | 2.3 (0.3) | 0.051 |
| BMI | 28.1 (3.1) | 27.6 (3.1) | 27.6 (2.8) | 29.4 (3.3) | NS |
| % overweight | 66.0 (16.7) | 63.2 (16.2) | 65.3 (14.6) | 74.6 (19.2) | 0.032 |
| Socioeconomic status (SES) |
47.3 (10.2) | 49.1 (10.3) | 46.7 (9.9) | 48.2 (10.7) | NS |
| zBMI changes | |||||
| 0-6 months | −0.5 (0.3) | −0.6 (0.3) | −0.3 (0.2) | −0.3 (0.2) | <0.0013 |
| 0-12 months | −0.5 (0.5) | −0.5 (0.4) | −0.3 (0.3) | −0.3 (0.3) | <0.0013 |
| 0-24 months | −0.4 (0.4) | −0.3 (0.3) | +0.2 (0.2) | −0.2 (0.3) | 0.054 |
| BMI changes | |||||
| 0-6 months | −3.8 (1.9) | −3.9 (1.5) | −2.0 (1.7) | −2.1 (1.6) | <0.0013 |
| 0-12 months | −2.7 (2.7) | −2.5 (2.4) | −0.8 (2.2) | −1.1 (2.4) | <0.0013 |
| 0-24 months | −0.2 (3.3) | −0.1 (2.5) | 1.2 (2.0) | 0.4 (3.0) | 0.059 |
| Built environment variables | |||||
| Housing units/acre | 7.8 (7.2) | 5.9 (5.1) | 6.8 (4.8) | 6.7 (5.0) | NS |
| Number of intersections/mile (Block size) |
5.8 (1.8) | 5.6 (1.5) | 6.2 (1.7) | 6.2 (1.5) | NS |
| Parkland (Hectaries) | 6.2 (12.2) | 5.6 (9.0) | 3.5 (7.2) | 2.8 (5.6) | NS |
| Active recreation + parkland (Hectaries) |
9.9 (15.5) | 6.7 (9.1) | 6.0 (7.8) | 7.4 (10.5) | NS |
| # Grocery stores | 6.1 (7.5) | 4.2 (4.4) | 5.5 (6.1) | 5.5 (4.9) | NS |
| # Supermarkets | 1.6 (1.3) | 1.6 (1.3) | 1.6 (1.2) | 1.8 (1.5) | NS |
| # Convenience stores | 5.6 (5.5) | 4.8 (3.5) | 5.8 (4.9) | 4.9 (3.6) | NS |
Note – BMI = body mass index, kg/m2. The average socioeconomic level (SES) of our families suggested they were middle class families, such as owners of medium sized businesses, minor professionals, or technical workers. Housing units/acre, and average block size are based on being within 1/2 mile of the participant’s home, while parkland and active recreational space + parkland are based on being accessible from roads within 1/2 mile of the participants home. Number of grocery stores, supermarkets, and convenience stores are counted within a 5 min drive from the participants’ home.
Study 4 > Studies 1,2;
Study 4 > Studies 1,2,3;
Studies 1,2 < Studies 3,4;
Study 1 < Study 3.
Measurement
BMI and zBMI
BMI was calculated from height and weight (kg/m2). All treated children were greater than the 85th BMI percentile (24). The primary dependent measure was zBMI, calculated based on the mean and standard deviation from the U.S. sample (24) that was used to develop the BMI percentiles ((BMI – BMI 50th Percentile)/ BMI Standard Deviation). Percent overweight was also calculated for descriptive purposes, using the following formula ((BMI – BMI 50th Percentile/ BMI 50th Percentile)*100).
Socioeconomic status
The Hollingshead index (25) was used to calculate socioeconomic status for all families. The Hollinghead index assesses socioeconomic status on the basis of education level, occupation, and marital status.
Built and food environment variables
A geographic information system was used to map attributes of the neighborhood environment using ArcGIS 8 and ArcView 3.3 (network analyst) software (26). Each child’s address was geo-coded to a unique parcel in a land-parcel data layer of Erie County in New York State. The attribute table accompanying the data layer was used to identify the type of housing (e.g., single-family, two-family, garden apartment, or public housing project) in which the child lived. Variables related to housing density were derived from block-group data from the 2000 U.S. Census (retrieved from the Census Bureau’s American FactFinder Web site, http://factfinder.census.gov, on December 13, 2005). On the basis of previous theoretical and conceptual work from our laboratory (6, 7, 11, 23, 27), we chose to focus on 7 neighborhood-environment variables (housing units per residential acre, number of intersections/mile, amount of park area and the amount of park plus other types of recreational area, number of supermarkets, grocery stores and convenience stores) that reflect density, diversity, and design of the neighborhood built environment (28) within 0.5 miles along the street network of each child’s residence (Table 1). Density, a measure of the compactness of an environment or the degree to which residences are located close to each other, was calculated as the number of housing units per residential acre, using the number of parcels available in the parcel layer. A single family housing unit was measured as housing with one unit, a duplex as housing with two units, etc. This measure was chosen because neighborhoods with a greater density of destinations are associated with greater physical activity in adults (28, 29). Likewise, greater housing density indicates proximity between houses in the neighborhood and may influence children’s willingness to walk and play with their friends living in the neighborhood. Design of the neighborhood environment includes the degree to which the layout of the neighborhood facilitates connectivity through its transportation network. Design was assessed using the number of intersections per mile, which is related to block size, as fewer intersections directly relate to larger average block size. Given the relation between the number of intersections and block size, this variable is discussed throughout the paper as block size. Greater street connectivity has been related to increased physical activity in adults, due in part to active transportation and walking (8, 30). However, children may use street connectively less for active transport and walking for exercise, and may use streets more for play. Highly connected streets with greater traffic density may suppress this type of active play, with greater active play in less connected cul-de-sacs (31). Finally, diversity in land use was assessed by the amount of park area and the amount of park and recreational area within a child’s neighborhoods. Previous research has shown park area and or park plus recreational area is related to child physical activity (6, 7, 23). Park area included nature trails, bike paths, playgrounds, athletic fields, and state, county, and municipally-owned parks. Recreational area was defined as the area of land used for ice or roller skating rinks, swimming pools, health clubs, tennis courts, and camping facilities. Data for parks was obtained from the Erie County parcel data and supplemented with a parks geographic information system layer prepared by the Urban Design Project at the University at Buffalo. The University at Buffalo parks geographic information system data layer identified green spaces such as greenways as park area that would not be formally recognized as a park within the Erie County parcel layer.
To assess the neighborhood food environment, the number of grocery stores, supermarkets and convenience stores within each participant’s neighborhood were measured, with a neighborhood defined as within a five-minute drive from the family’s home, based on posted traffic speed limits for individual streets, consistent with previous recommendations (32). Each subject’s home address in the Erie County parcel layer was geocoded using ArcGIS. Then, using Network Analyst in ArcGIS, the distance each participant would traverse in five minutes from his or her home if s/he traveling at posted speed limit along the road network was measured. We then enumerated the number of different types of food destinations that lie along this five minute road network in all directions from each subject’s home. The distance covered by five-minute travel normalizes the size (in terms of travel time) of all subjects’ neighborhoods. The use of travel time (rather than distance) accounts for the opportunity cost of time associated with traveling to a particular food destination from a resident’s home based on posted traffic speed limits. In 2010, Americans spent about 10 minutes in travel related to eating and drinking – which works out to be 5 minutes travel time each way (33).
In computing the number of food destinations in a neighborhood, we included grocery stores, supermarkets, convenience stores, fruits and vegetable markets, specialty stores, and natural food stores. We have previously observed in the study area (Erie County) that convenience stores carry less healthful foods than supermarkets and grocery stores: 33 percent of convenience stores carried fresh produce in comparison to 100 percent of supermarkets; only 17 percent of convenience stores were found to carry whole grains in comparison to 80 percent of supermarkets (27). Food shopping destinations were identified and classified on the basis of standard industrial classification codes.
The data on food destinations, including standard industrial classification categorizations, which was obtained from Reference USA, a private vendor, was cleaned and verified before use in subsequent analyses. The database includes duplicate entries for a business and standard industrial classification categorizations are occasionally reported incorrectly. Prior to geocoding the food business data, we removed duplicate entries of food businesses, and verified the standard industrial classification categorizations by cross-referencing with description of the business provided in the databases. If the description and standard industrial classification categorization of a food business did not match, we made telephone calls to business owners to verify standard industrial classification categorization. The remaining food businesses were geocoded to the parcel layer, and the number of businesses available within each subject’s 5-minute neighborhood were counted using ArcGIS. The food environment data are described elsewhere in detail (27). Data on the food environment was available only for families who lived in Erie County, which was the limiting built environment factor for including families in the analysis. Data on treatment outcome and the food environment was available for 191 families. In the final models, only supermarkets, grocery stores, and convenience stores were used, since many families did not have any of the other types of stores in their neighborhoods. Based on prior work (27), because standard industrial classification codes do not make this distinction, supermarkets are distinguished from grocery stores on the basis of the number of employees, which serves as a proxy for size of store. We classified food retail stores with fewer than 50 employees as grocery stores and those with more than 50 employees as supermarkets.
Analytic Plan
Hierarchical mixed model analyses of covariance (ANCOVA) were used to determine which of the built environment variables were related to zBMI change from baseline to 6, 12 and 24 months after randomization, and if treatment condition moderated the effect of the built environment on zBMI change. Mixed model ANCOVA allows for the inclusion of all participants who have some treatment data. The first step included baseline zBMI, sex, age, family socioeconomic status as covariates and months as a predictor to determine if there were significant changes over time. Baseline zBMI was included as a covariate to control for differences in baseline zBMI across studies, sex, age and socioeconomic status were controlled because of their potential influence on child change in zBMI. The second step added treatment condition and the interaction of treatment condition × months to determine if there were significant differences in change over time by treatment condition. Since there were no differences as a function of exercise or reduced sedentary behavior dose in the first study (19), the treatment results were collapsed across dose. The third step involved four separate models for each built environment variable to assess whether an individual built environment variable predicted zBMI change, controlling for treatment condition. Finally, the fourth step tested whether there were differential effects observed for treatment condition for any built environment variable by examining built environment by treatment condition interactions. Significance levels were tested based on the new variables included in the model, so that the significance level of treatment condition was based on the results of step 2, and the effects of the built environment variables were significant based on results of step 3. This is necessary since studying effects of variables involved in higher order interactions can change the interpretation of these effects, and separate steps allowed for clearer interpretation of effects in each step (34). SAS mixed model influence diagnostics (35) for PROC MIXED were used to identify influential cases in significant models, and analyses were then tested with and without influential cases to establish generalizability of results. Significant interaction effects were probed by mixed model analyses of variance for low versus high levels of the variable based on median split of the variable. Low and high data points were based on the median split for the variables (breakpoints = 6.2, 2.0 and 4.0 for block size, supermarkets and convenience stores, respectively) with the exception of parkland. Parkland has a bivariate distribution, with 100 subjects not living near a park, and the other 91 living within 0.5 miles of a park. The breakpoint for parkland was no parkland versus at least some parkland. Analyses were conducted using SAS (35).
Results
The characteristics of participants in the sample are shown in Table 1. Pearson product moment correlation coefficients among the built environment variables showed that parkland was not correlated with block size, supermarkets or convenience stores (r’s = −0.07, 0.12 and 0.13, respectively, p’s > 0.05). Block size was negatively correlated with both supermarkets and convenience stores (r = −0.42, −0.42, p’s < 0.001), and the number of supermarkets and convenience stores were correlated (r = 0.50, p < 0.001).
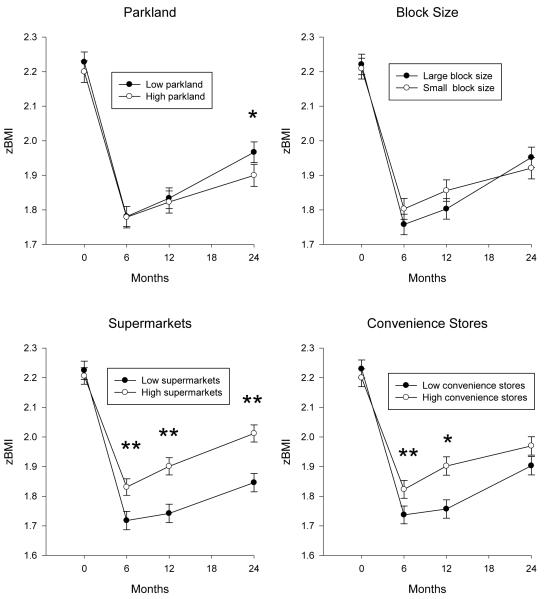
Results of the four step hierarchical mixed model ANCOVAs are shown in Table 2 for parkland, block size, supermarkets and convenience stores. There were no significant main effects of housing density, park plus recreational area, or grocery stores on zBMI change, nor did these variables interact with treatment condition to predict outcome, and data for these variables is not presented. In Step 2, adding the interaction of treatment condition × time was significant (F(24, 506) = 2.32, p = 0.0004). In Step 3 parkland (F(3, 503) = 3.32, p = 0.020), number of supermarkets (F(3, 503) = 7.92, p < 0.0001), and number of convenience stores (F(3, 503) = 3.58, p = 0.014) were significant predictors of zBMI over time beyond the effects of treatment condition. Figure 2 presents zBMI changes over time as a function of low versus high values of each built environment variable, controlling for the covariates in the model. Greater zBMI reduction was associated with living in environments with high access to parks at 24 months (p = 0.023), low number of supermarkets at 6 (p < 0.0001), 12 (p = 0.006), and 24 (p = 0.0014) months, and low number of convenience stores at 6 (p = 0.0065) and 12 (p = 0.018) months. Block size was not a significant predictor of outcome (F(3, 503) = 2.62, p = 0.051). To assist in interpretation of the magnitude of the zBMI changes in terms of access to different aspects of the built environment, zBMI changes from baseline to 2 years were calculated based on + 1 SD from the mean for supermarkets and convenience stores within a five minute drive from home, and none versus at least some access to parks within 0.5 miles along the street network from home. These analyses showed zBMI differences for none versus three or more supermarkets of −0.37 vs −0.20 zBMI units; −0.31 vs −0.24 zBMI units for access to no versus 10 or more convenience stores, and −0.31 vs −0.25 zBMI units for those with some versus no access to parks.
Table 2.
Hierarchical regression models to test effects of treatment condition, built environment variables and the interaction of treatment condition X built environment variables on zBMI change over 2 years.
| Effect | DF | F | P | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Step 1 | |||||||||
| Age | 1,181 | 1.03 | -.32 | ||||||
| Sex | 1,181 | 0.40 | 0.53 | ||||||
| Baseline zBMI | 1,181 | 310.03 | <0.0001 | ||||||
| Socioeconomic status (SES) | 1,181 | 2.76 | 0.10 | ||||||
| Months | 3, 530 | 163.15 | <0.0001 | ||||||
| Step 2 | |||||||||
| Treatment Condition | 8,173 | 3.01 | 0.0035 | ||||||
| Treatment Condition * Months | 24,506 | 2.32 | 0.0004 | ||||||
| Parkland | Block Size | Supermarkets | Convenience Stores | ||||||
| Step 3 | F | P | F | P | F | P | F | P | |
| Built environment | 1,172 | 2.28 | 0.13 | 2.06 | 0.15 | 9.96 | 0.0019 | 2.82 | 0.09 |
| Built environment * months | 3, 503 | 3.32 | 0.02 | 2.62 | 0.051 | 7.92 | <0.0001 | 3.58 | 0.014 |
| Step 4 | |||||||||
| Built environment * Treatment | 8, 164 | 1.79 | 0.08 | 1.00 | 0.44 | 1.85 | 0.07 | 1.22 | 0.29 |
| Condition | |||||||||
| Built environment * Treatment Condition * Months |
24, 479 | 1.30 | 0.16 | 0.70 | 0.86 | 1.09 | 0.35 | 1.01 | 0.45 |
Note – SES = socioeconomic status. For block size, df were 8,163 and 24,476 for the Built environment * Treatment Condition and Built environment * Treatment Condition * Months interactions respectively, due to removal of one influential participant.
Figure 2.
zBMI values (+ SEM) changes over time in relationship to parkland and block size (top graphs), and supermarkets and convenience stores (bottom graphs). The mixed model ANCOVA controlled for child age, sex, socioeconomic status, and baseline zBMI.
Significant differences from baseline = * p < 0.05 ** p < 0.01
Analysis of treatment by built environment showed no significant interactions of treatment by any characteristics of the built environment. Though there are limitations to interpretation of retrospective power (36, 37), retrospective power for the mixed model ANCOVA as determined by SAS was 0.925 for parkland, 0,608 for block size, 0.857 for supermarkets, and 0.820 for convenience stores. Preliminary analysis did show that block size interacted with the built environment, but the mixed model influence diagnostics showed one participant to be highly influential (Restricted likelihood distance = 13.27). Removal of that participant was associated with a reduction in the interaction from p = 0.0296 to p = 0.858, which justifies removal of that participant from final analyses.
Discussion
This report provides the first evidence that the built environment is associated with child zBMI changes to evidence-based, standardized family-based behavioral treatment. Controlling for child baseline zBMI, age, sex and socioeconomic status, three characteristics of the built environment, including proximity of parkland, convenience stores and supermarkets, were associated with weight control across different types of treatment programs. Access to neighborhood parks is associated with greater physical activity (5-7) and in the present study is associated with greater weight control in the long term. Convenience stores offer access to take away or snack foods, and were correlated with increased obesity (2-4) in prior studies and negatively impact weight control in the present study. This suggests that children with easy access to foods purchased at convenience stores may consume more snack foods and have difficulty with weight control. Supermarkets are often thought of as a positive influence on health (10, 11), since fruits and vegetables can be purchased which are often not readily available in convenience stores, and supermarkets can reduce negative impact of food deserts on access to healthier foods. However, the presence of supermarkets was a negative influence on weight control among treated overweight children in this study, with even stronger and longer lasting effects than convenience stores. This suggests that supermarkets may provide children in families with obesity even greater access to a wider variety and quantity of less healthy foods that may compromise weight control, rather than making it easier to lose weight. Research has shown that it is challenging to increase an individual’s purchase of fruits and vegetables in supermarkets and reduce energy intake or improve nutrient quality (38-40). Thus, the types of foods that families with obesity purchase at supermarkets may not be the healthiest options, and more access to food stores, regardless of type, may make it even more difficult for children to lose weight unless they are strongly motivated to eat healthier.
While we hypothesized that characteristics of the built environment might interact with interventions designed to differentially target reducing sedentary behavior, we were expecting parkland to differentially influence weight loss for those who were targeted to reduce sedentary behavior; we had previously shown greater increases in physical activity for children who were in an intervention to reduce sedentary behavior who lived close to parks (23). However, results showed that the built environment had uniform effects across all treatments studied. Additional research is needed to assess the stability of built environment effects across other treatments; this preliminary examination of how the built environment may influence weight loss suggests broad influences on outcome. The family-based treatments that were studied emphasize reducing energy intake in weight loss, but aspects of the built environment that prompt physical activity may be important to prevent obesity (5), as well as improve physical fitness in all children. Future research can assess if obese children respond the same way to physical activity programs as leaner children if they live in an environment that favors physical activity.
Some aspects of the built environment had quite large effects that were maintained over time. For example, children in families with reduced access to supermarkets had equivalent zBMI change at 24 months in comparison to children with greater access to supermarkets showed at 6 months. In other words, if you had reduced access to supermarkets that provide less access to choice or variety of healthier or less healthy foods, then a child would maintain greater zBMI change after two years compared to zBMI changes observed at the end of six month treatment for children who lived closer to supermarkets. The models predict that participants with no access to supermarkets within a 5 minute drive would have almost a 1.9 fold greater decrease in zBMI units over two years in comparison to having three or more supermarkets near your home. Participants living in an area with reduced access to convenience stores would be predicted to have 1.3 fold greater zBMI reduction over two years than those living in an area with easy access (10 or more) convenience stores. Participants living in an area with some access to parks would be predicted to have 1.24 fold greater zBMI changes than those who lived in an area with no access to parks.
One implication of these results is that family-based behavioral treatment programs should provide individualized treatment components that target challenges to weight loss that arise from the neighborhood food and activity built environment. Behavioral family-based programs may be ideal platforms for developing these treatment components since these treatments focus on familial behavior change and modifying the shared family environment. For example, families may need to identify venues for physical activity if the family lives in an environment that has no access to parks or has high street connectivity, and modify familial patterns to ensure that children have parental support to take advantage of these resources. Identifying a community resource for child sports teams and active play will have very little effect of weight loss programs if parents and children take advantage of proximal unhealthy food access (e.g., purchases at a convenience store) before or after sporting events. Easy access to convenience stores or supermarkets highlight the impact that food availability can have on obesity treatment, and for people who overeat due to easy food availability, intervention components may be needed to alter shopping behavior, travel patterns, and to reduce impulsive shopping (41). Families could be provided “walking maps” that purposely route families away from food purchasing or eating destinations (e.g. ice-cream shops) to more active or non-food destinations in their neighborhoods.
There are several limitations to the current study. Different definitions were used for measuring the boundaries of the physical activity and food purchasing built environments. Aspects of the built environment such as access to parkland was measured within 0.5 miles of their home, a walkable or bikeable distance for most children. The number of food purchasing and food purchasing establishments were measured within a five minute drive, which included all walkable and bikeable food purchasing establishments, but also included sites that may only be accessible by car for younger children and an older child without a bike or permission to ride a bike that far from home. Thus, because of this difference in the extent of the measured environments, it is possible that the impact of the food purchasing environment was stronger given that sites farther from the person’s home were included for food purchasing than for physical activity. Second, our dataset did not include food service establishments such as restaurants and cafes where people can eat on-site. Fast food restaurants or ice cream parlors in a participant’s neighborhood may make it hard to make healthier eating decisions, and research is needed that assesses the effects of such eating establishments on weight loss. Third, the built environment data were collected during 2006 for studies implemented from 1997 to 2005. The discrepancy between the years that treatment data were collected and neighborhood environment data were collected is likely to influence outcome because Erie County, the site of the study, does not have a fast pace of land development. Population in the county declined by 3.3% in the last decade, and less than 1000 building permits were issued county wide in 2009. As estimated from the Erie County Assessor’s databases for 2000 and 2004, only 1.6% of all land parcels in the county were developed between 2000 and 2004. Fourth, we based family’s built environments on their address when they entered the study, and we assumed the families did not move while they were in treatment or follow-up.
The prevalence of childhood obesity has been increasing over the past few decades(42) and one factor that has led to this increase are current environments that promote a lack of exercise and an increase in energy intake (43, 44). Many children do not live in environments that provide easy access to parks or active recreational areas, but have relatively easier access to stores from which they can purchase food. These cumulative effects highlight the importance of making changes to the built environment at a societal level that foster healthy eating and activity. Until that happens, it is incumbent upon those who treat pediatric obesity to understand the environmental press some families experience that can shape a sedentary lifestyle and unhealthy eating behaviors, and develop intervention components to help families combat the toxic environment within and outside of their homes that lead to and/or maintain their obesity (7).
Acknowledgements
CORRESPONDENCE AND REPRINT REQUESTS: This research was funded in part by grants HD 25997, HD 39778, HD 39792 and HD 42766 from the National Institute of Child Health and Human Development, grant DK 88380 from the National Institute of Diabetes and Digestive Diseases, awarded to Dr. Epstein, and Grant MH070446 from the National Institute of Mental Health awarded to Dr. Wilfley. The funding agencies were not involved in analysis or interpretation of the data.
Appreciation is expressed to Dominica Vito, CeCe Gordy, and Colleen Kilanowski, who coordinated studies at the University at Buffalo, and research assistants, therapists and families who made this research possible, to Robert Shibley, Dean of the School of Architecture and Planning, for providing a GIS parks layer, to Dale Morris, Erie County, New York, for providing Erie County GIS parcel layers, and Kruti Bhatia for assistance with land parcel data. The development of this article was funded in part by grants HD 25997, HD 39778, HD 39792 and HD 42766 from the National Institute of Child Health and Human Development, grant DK 88380 from the National Institute of Diabetes and Digestive Diseases, awarded to Dr. Epstein, and Grant MH070446 from the National Institute of Mental Health awarded to Dr. Wilfley.
Footnotes
Conflict of Interest The authors do not have any conflict of interests.
References
- 1.Gordon-Larsen P, Nelson MC, Page P, Popkin BM. Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics. 2006;117:417–424. doi: 10.1542/peds.2005-0058. [DOI] [PubMed] [Google Scholar]
- 2.Oreskovic NM, Winickoff JP, Kuhlthau KA, Romm D, Perrin JM. Obesity and the built environment among Massachusetts children. Clin Pediatr (Phila) 2009;48:904–912. doi: 10.1177/0009922809336073. [DOI] [PubMed] [Google Scholar]
- 3.Oreskovic NM, Kuhlthau KA, Romm D, Perrin JM. Built environment and weight disparities among children in high- and low-income towns. Acad Pediatr. 2009;9:315–321. doi: 10.1016/j.acap.2009.02.009. [DOI] [PubMed] [Google Scholar]
- 4.Grafova IB. Overweight children: assessing the contribution of the built environment. Prev Med. 2008;47:304–308. doi: 10.1016/j.ypmed.2008.04.012. [DOI] [PubMed] [Google Scholar]
- 5.Wolch J, Jerrett M, Reynolds K, et al. Childhood obesity and proximity to urban parks and recreational resources: A longitudinal cohort study. Health Place. 2011;17:207–214. doi: 10.1016/j.healthplace.2010.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roemmich JN, Epstein LH, Raja S, Yin L, Robinson J, Winiewicz D. Association of access to parks and recreational facilities with the physical activity of young children. 2006;43:437–41. doi: 10.1016/j.ypmed.2006.07.007. [DOI] [PubMed] [Google Scholar]
- 7.Roemmich JN, Epstein LH, Raja S, Yin L. The neighborhood and home environments: disparate relationships with physical activity and sedentary behaviors in youth. Ann Behav Med. 2007;33:29–38. doi: 10.1207/s15324796abm3301_4. [DOI] [PubMed] [Google Scholar]
- 8.Saelens BE, Sallis JF, Black JB, Chen D. Neighborhood-based differences in physical activity: an environment scale evaluation. Am J Public Health. 2003;93:1552–1558. doi: 10.2105/ajph.93.9.1552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Giles-Corti B, Macintyre S, Clarkson JP, Pikora T, Donovan RJ. Environmental and lifestyle factors associated with overweight and obesity in Perth, Australia. Am J Health Promot. 2003;18:93–102. doi: 10.4278/0890-1171-18.1.93. [DOI] [PubMed] [Google Scholar]
- 10.Morland KB, Evenson KR. Obesity prevalence and the local food environment. Health Place. 2009;15:491–495. doi: 10.1016/j.healthplace.2008.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Raja S, Yin L, Roemmich JN, et al. Food environment, built environment, and women’s BMI: Evidence from Erie County, New York. J Planning Educ Res. 2010;29:444–460. [Google Scholar]
- 12.Baranowski T, Cullen KW, Nicklas T, Thompson D, Baranowski J. Are current health behavioral change models helpful in guiding prevention of weight gain efforts? Obes Res. 2003;11(Suppl):23S–43S. doi: 10.1038/oby.2003.222. [DOI] [PubMed] [Google Scholar]
- 13.Egger G, Swinburn B. An “ecological” approach to the obesity pandemic. BMJ. 1997;315:477–480. doi: 10.1136/bmj.315.7106.477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.French SA, Story M, Jeffery RW. Environmental influences on eating and physical activity. Annu Rev Public Health. 2001;22:309–335. doi: 10.1146/annurev.publhealth.22.1.309. [DOI] [PubMed] [Google Scholar]
- 15.Epstein LH. Development of evidence-based treatments for pediatric obesity. In: Kazdin AE, Weisz JR, editors. Evidence-based psychotherapies for children and adolescents. Guilford Publications, Inc.; New York: 2003. pp. 374–388. [Google Scholar]
- 16.Epstein LH, Paluch RA, Roemmich JN, Beecher MD. Family-based obesity treatment, then and now: twenty-five years of pediatric obesity treatment. Health Psychol. 2007;26:381–91. doi: 10.1037/0278-6133.26.4.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ogden CL, Flegal KM, Carroll MD, Johnson CL. Prevalence and trends in overweight among US children and adolescents, 1999-2000. JAMA. 2002;288:1728–1732. doi: 10.1001/jama.288.14.1728. [DOI] [PubMed] [Google Scholar]
- 18.Troiano RP, Flegal KM, Kuczmarski RJ, Campbell SM, Johnson CL. Overweight prevalence and trends for children and adolescents. The National Health and Nutrition Examination Surveys, 1963 to 1991. Arch Pediatr Adolesc Med. 1995;149:1085–1091. doi: 10.1001/archpedi.1995.02170230039005. [DOI] [PubMed] [Google Scholar]
- 19.Epstein LH, Paluch RA, Gordy CC, Dorn J. Decreasing sedentary behaviors in treating pediatric obesity. Arch Pediatr Adolesc Med. 2000;154:220–226. doi: 10.1001/archpedi.154.3.220. [DOI] [PubMed] [Google Scholar]
- 20.Epstein LH, Paluch RA, Gordy CC, Saelens BE, Ernst MM. Problem solving in the treatment of childhood obesity. J Consult Clin Psychol. 2000;68:717–721. [PubMed] [Google Scholar]
- 21.Epstein LH, Paluch RA, Kilanowski CK, Raynor HA. The effect of reinforcement or stimulus control to reduce sedentary behavior in the treatment of pediatric obesity. Health Psychology. 2004;23:371–380. doi: 10.1037/0278-6133.23.4.371. [DOI] [PubMed] [Google Scholar]
- 22.Epstein LH, Roemmich JN, Stein RI, Paluch RA, Kilanowski CK. The challenge of identifying behavioral alternatives to food: clinic and field studies. Ann Behav Med. 2005;30:201–209. doi: 10.1207/s15324796abm3003_4. [DOI] [PubMed] [Google Scholar]
- 23.Epstein LH, Raja S, Gold SS, Paluch RA, Pak Y, Roemmich JN. Reducing sedentary behavior: the relationship between park area and the physical activity of youth. Psychol Sci. 2006;17:654–659. doi: 10.1111/j.1467-9280.2006.01761.x. [DOI] [PubMed] [Google Scholar]
- 24.Kuczmarski RJ, Ogden CL, Guo SS, et al. Vital Health Statistics. Vol. 246. National Center for Health Statistics; Hyattsville, MD: 2002. CDC growth charts for the United States: Methods and development; pp. 1–90. Series 11. [PubMed] [Google Scholar]
- 25.Hollingshead AB. Four factor index of social status. Yale University; New Haven, Conn: 1975. [Google Scholar]
- 26.ESRI . ArcGIS 9. ESRI GIS and Mapping software; Redlands, CA: 2004. [Google Scholar]
- 27.Raja S, Ma C, Yadav P. Beyond food deserts: Measuring and mapping disparities in the neighborhood food environment. J Plann Educ Res. 2008;27:469–482. [Google Scholar]
- 28.Ewing R. Can the physical environment determine physical activity levels? Exerc Sport Sci Rev. 2005;33:69–75. doi: 10.1097/00003677-200504000-00003. [DOI] [PubMed] [Google Scholar]
- 29.Frank LD, Schmid TL, Sallis JF, Chapman J, Saelens BE. Linking objectively measured physical activity with objectively measured urban form: findings from SMARTRAQ. Am J Prev Med. 2005;28:117–125. doi: 10.1016/j.amepre.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 30.Saelens BE, Sallis JF, Frank LD. Environmental correlates of walking and cycling: findings from the transportation, urban design, and planning literatures. 2003;25:80–91. doi: 10.1207/S15324796ABM2502_03. [DOI] [PubMed] [Google Scholar]
- 31.Mecredy G, Pickett W, Janssen I. Street connectivity is negatively associated with physical activity in Canadian youth. Int J Environ Res Public Health. 2011;8:3333–3350. doi: 10.3390/ijerph8083333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dunkley BA, Helling A, Sawicki DS. Accessibility versus scale: Examining the tradeoffs in grocery stores. J Plann Educ Res. 2004;23:387–401. [Google Scholar]
- 33.Department of Labor. American Time Use Survey (ATUS) Bureau of Labor Statistics. Inter-university Consortium for Political and Social Research; Ann Arbor, MI: 2010. [Google Scholar]
- 34.Jaccard J, Wan CK, Turrisi R. The detection and interpretation of interaction effects between continuous variables in multiple regression. Mult Behav Res. 1990;25:467–478. doi: 10.1207/s15327906mbr2504_4. [DOI] [PubMed] [Google Scholar]
- 35.SAS Institute Inc. SAS OnlineDoc® 9.1.3. SAS Institute Inc.; Cary, NC: 2004. [Google Scholar]
- 36.Nakagawa S, Foster TM. The case against retrospective statistical power analyses with an introduction to power analysis. Acta Ethol. 2004;7:103–108. [Google Scholar]
- 37.Hoenig JM, Heisey DM. The abuse of power: The pervasive fallacy of power calculations for data analysis. Am Stat. 2001;55:1–6. [Google Scholar]
- 38.Kristal AR, Goldenhar L, Muldoon J, Morton RF. Evaluation of a supermarket intervention to increase consumption of fruits and vegetables. Am J Health Promot. 1997;11:422–425. doi: 10.4278/0890-1171-11.6.422. [DOI] [PubMed] [Google Scholar]
- 39.Anderson JV, Bybee DI, Brown RM, et al. 5 a day fruit and vegetable intervention improves consumption in a low income population. J Am Diet Assoc. 2001;101:195–202. doi: 10.1016/S0002-8223(01)00052-9. [DOI] [PubMed] [Google Scholar]
- 40.Ni Mhurchu C, Blakely T, Jiang Y, Eyles HC, Rodgers A. Effects of price discounts and tailored nutrition education on supermarket purchases: a randomized controlled trial. Am J Clin Nutr. 2010;91:736–747. doi: 10.3945/ajcn.2009.28742. [DOI] [PubMed] [Google Scholar]
- 41.Nederkoorn C, Guerrieri R, Havermans RC, Roefs A, Jansen A. The interactive effect of hunger and impulsivity on food intake and purchase in a virtual supermarket. Int J Obes (Lond) 2009;33:905–912. doi: 10.1038/ijo.2009.98. [DOI] [PubMed] [Google Scholar]
- 42.Strauss RS, Pollack HA. Epidemic increase in childhood overweight, 1986-1998. JAMA. 2001;286:2845–2848. doi: 10.1001/jama.286.22.2845. [DOI] [PubMed] [Google Scholar]
- 43.Jeffery RW, French SA. Epidemic obesity in the United States: are fast foods and television viewing contributing? Am J Public Health. 1998;88:277–280. doi: 10.2105/ajph.88.2.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hill JO, Wyatt HR, Reed GW, Peters JC. Obesity and the environment: where do we go from here? Science. 2003;299:853–855. doi: 10.1126/science.1079857. [DOI] [PubMed] [Google Scholar]