Abstract
The objective of this study was to characterize the subgingival microbiota of African-American children with Localized Aggressive Periodontitis (LAP). Fifty-one children were included. Subgingival plaque samples were taken from diseased (DD) and healthy sites (DH) in LAP and from healthy sites in HS and HC and analyzed by 16S rRNA-based microarrays. Aggregatibacter actinomycetemcomitans (Aa) was the only species found to be both more prevalent (OR = 8.3, p = 0.0025) and abundant (p < 0.01) in DD. Filifactor alocis (Fa) was also found to be more prevalent in DD (OR 2.31, CI 1.06-5.01, p = 0.03). Most prevalent species in healthy sites were Selenomonas spp, Veillonella spp, Streptococcus spp, Bergeyella sp, and Kingella oralis. Overall, Streptococcus spp, Campylobacter gracilis, Capnocytophaga granulosa, Haemophilus parainfluenzae, and Lautropia mirabilis were most abundant in healthy children, while Aa, Fa, Tannerella sp, Solobacterium moorei, Parvimonas micra, and Capnocytophaga sp were most abundant in LAP. Based on a comprehensive analysis with 16S rRNA-based microarrays, Aa was strongly associated and site-specific in LAP. In contrast, other species were found to be associated with healthy sites and individuals (ClinicalTrials.gov number CT01330719).
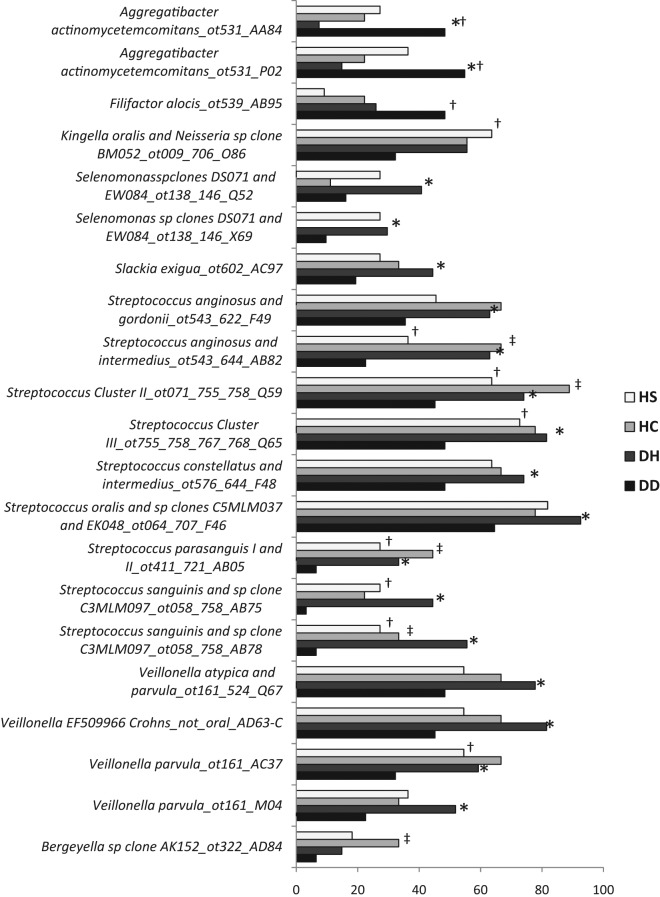
Abbreviations: healthy site in healthy sibling (HS); healthy site in healthy control child (HC).
Keywords: localized aggressive periodontitis, diagnosis, microbiology, Aggregatibacter actinomycetemcomitans, HOMIM, subgingival microbiota
Introduction
Aggressive periodontitis (AgP) is comprised of a group of less frequent, often severe, rapidly progressive forms of periodontitis. This disease is characterized by an early age of onset, with molar and incisor teeth to be the first ones affected in localized forms (LAP), and a propensity for familial involvement. Albandar and Tinoco (Ickenstein et al., 1999) reported a prevalence of AgP in children/adolescents from 0.1% (Europe) to 7.6% (Africa). Given its rare occurrence and difficulties in gathering large populations for study, our knowledge on AgP is still limited.
Numerous reports have aimed to characterize the microbiota associated with AgP. Some studies have associated the species Aggregatibacter (previously Actinobacillus) actinomycetemcomitans (Aa) with AgP in different populations (Zambon et al., 1983; Kaldahl et al., 1988; Haffajee et al., 2003; Leung et al., 2005; Yang et al., 2005; Kaner et al., 2007). Recent studies have shown a specific clone of Aa (JP2) to be associated with AgP in adolescents living in or originating from north and west Africa (Haubek et al., 1996, 1997). This species has also been reported to be associated with the initiation of attachment loss in adolescents (Spinozzi and Langer, 1999; Haubek et al., 2008).
Other studies have found other species, such as P. gingivalis (Pg), to be more prevalent in AgP (Gajardo et al., 2005; Mayorga-Fayad et al., 2007). Thiha et al. (2007) reported that a population of Japanese individuals with either chronic or AgP was found to harbor no different amounts of the main periodontopathogenic species, Aa, Pg, and T. forsythia, although Aa was found to be more prevalent in LAP (Thiha et al., 2007).
With the latest advances in molecular biology techniques, recent studies have shown that recognized periodontal pathogens can also be recovered from healthy adults and children (Alaluusua and Asikainen, 1988; Yang et al., 2002), and new uncultivated species have been associated with periodontitis (Kumar et al., 2003; Riep et al., 2009). Thus, with different reports in the literature, different techniques being used for the detection of periodontopathogens, and different populations studied, the role of specific periodontopathogens in the destructive process of AgP is still not clear. We have identified a cohort of African-American children diagnosed with LAP within one clinical setting in Florida. Since this is a homogeneous group in terms of race, age, and patterns of disease, and this is a rare type of disease, the objective of this study was to use 16S rRNA-based microarrays to run a comprehensive characterization of the subgingival microbial flora present in this disease when compared with healthy siblings and unrelated control children.
Materials & Methods
Demographics of the Study Population
This study aimed to characterize, clinically and microbiologically, a population of children with LAP in Florida. Children included in the study were recruited from the Leon County Health Department, Tallahassee, Florida, from February 2007 to August 2010. All children and their families were informed about the study protocol and signed an informed consent previously approved by the Institutional Review Board at University of Florida. Complete medical and dental histories were taken from all participants. Children with LAP were included as they were diagnosed with the disease and met inclusion criteria. Siblings of children with disease (healthy or diseased) were examined and included as well. Healthy unrelated control children were randomly selected from the same clinic and included as they met inclusion criteria. Attempts were made to match control children for age and gender. Inclusion criteria for all individuals were that they were between 5 and 21 years old, and were African-Americans. Localized aggressive disease was defined by the presence of less than 30% of sites but at least 2 teeth [incisor and/or first molar, but no more than 2 teeth other than first molar and incisors (Armitage, 1999)] with PD ≥ 5 mm in the presence of interproximal attachment loss and ≥ 2 mm bone loss detected on radiographic examination. Healthy participants were defined by the absence of pocket depth > 4 mm in the presence of attachment/bone loss (pseudo/gingival pockets with no attachment/bone loss were allowed). Patients in any category were excluded if they: had been diagnosed with any systemic diseases or conditions that could influence the progression and/or clinical characteristics of periodontal disease (e.g., diabetes or blood disorders); had taken antibiotics within the preceding 3 mos or any medications that could influence the characteristics of the disease (e.g., phenytoin, cyclosporine); were smokers; and/or were pregnant/lactating women.
Clinical Measurements
The following periodontal clinical parameters were taken by one calibrated examiner at the initial visit for all patients: pocket depth (PD), bleeding on probing (BoP); gingival margin position (GM); clinical attachment level (CAL: distance from the CEJ to the bottom of the pocket); Plaque Index (PI): and presence or absence of visible plaque. Measurements were performed with a UNC-15 periodontal probe at 6 sites per tooth (mesio-buccal, buccal, disto-buccal, mesio-lingual, lingual, and disto-lingual) and were recorded with computer software (Florida Probe, Gainesville, FL, USA ). Periapical and bite-wing x-rays were taken of the compromised teeth to confirm LAP diagnosis. Intra-examiner calibration was obtained when 80% of duplicate measures of probing depth and CAL were within 1 mm.
Collection of Bacterial Subgingival Biofilm
Bacterial subgingival biofilm was collected from 1 diseased site (first molar or incisor) with PD ≥ 5 mm and BoP and from 1 healthy site (PD ≤ 3 mm, no BoP) from children with LAP (non-affected molar or incisor). Samples were also collected from healthy sites from healthy siblings and healthy unrelated control children (molar or incisor). The area of collection was isolated with cotton rolls, and supragingival plaque was carefully removed. Collection was done with a sterile endodontic paperpoint. Following sampling, the paperpoint was stored at −70ºC until processed.
DNA Isolation and Microarray Analysis
DNA was isolated from plaque samples with the use of a DNA Purification kit according to the manufacturer’s instructions (MasterPure, EPICENTRE Biotechnologies, Madison, WI, USA). After purification, DNA concentration was tested with the Nanodrop (ND-1000 Spectrophotometer, Nanodrop Technologies Inc., Wilmington, DE, USA). A 200-ng quantity of each sample at a minimum concentration of 20 ng/µL was submitted to The Forsyth Institute for HOMIM (Human Oral Microbe Identification Microarray) analysis. [The method has been described in detail elsewhere (Colombo et al., 2009).] Briefly, 16S rRNA genes were PCR-amplified from DNA extracts with 16S rRNA universal forward and reverse primers and labeled via incorporation of Cy3-dCTP in a second nested PCR. HOMIM uses 16S rRNA-based, reverse-capture oligonucleotide probes (typically 18 to 20 bases), which are printed on aldehyde-coated glass slides and probed with labeled PCR products (described above) which are hybridized in duplicate. The microarray slides are scanned in an Axon 4000B scanner, and crude data are extracted with GenePix Pro software (Molecular Devices, Sunnyvale, CA, USA). Microbial profiles were generated from image files of scanned arrays with a HOMIM online analysis tool (http://bioinformatics.forsyth.org/homim/). Detection of a particular taxon was determined by the presence of a fluorescent spot for that unique probe. A mean intensity for each taxon was calculated from hybridization spots of the same probe, and signals were normalized by comparison of individual signal intensities with the average of signals from universal probes and calculated as described previously (Colombo et al., 2009). Any original signal that was less than two times the background value was re-set to 1 and was assigned to the signal level 0. Signals greater than 1 were categorized into scores from 1 to 5, corresponding to ranked signal levels.
Statistical Analysis
Analysis of variance (ANOVA) with Tukey’s multiple comparisons was applied among groups for clinical and demographic parameters. A paired t test was applied for differences in PD between DD and DH sites in LAP. ANOVA models were applied for the microbiological results among groups (diseased and healthy sites from LAP, healthy sites from siblings and unrelated control children). Least-squared means of each group were estimated, and a post hoc t test was performed to determine differences in the amount of each species. Logistic regression was performed, generating an odds ratio estimation, to compare the frequency of each probe among groups. Rank products analysis was performed to compare abundance of species between healthy individuals (sites pooled from healthy individuals) and those with disease (sites pooled in LAP individuals). SAS software (SAS Institute, Cary, NC, USA) was used for all statistical analyses.
Results
Thus far, over 60 African-American children with LAP have been diagnosed in the Leon County Health Department. The present study addresses the periodontal conditions and microbial profiles of 31 LAP children, 11 healthy siblings, and 9 healthy unrelated control children. All children included were African-Americans. Mean age of children and gender distribution along with clinical parameters for all children are shown in Table 1.
Table 1.
Clinical and Demographic Parameters for Different Groups Evaluated
| Age (yrs) | M/F | %PD > 4 mm | %BoP | %Plaque | Mean PD Sites/All | Mean CAL | PD Site | |
|---|---|---|---|---|---|---|---|---|
| LAP | 14.29 ± 3.52 | 14m/17f | 14.42 ± 9.51† | 24.52 ± 32.84 | 45.16 ± 25.68 | 4.97 ± 0.69† | 3.74 ± 1.51 | 6.00 ± 1.37 DD†‡ |
| 2.35 ± 0.42† | 2.18 ± 0.67 DH | |||||||
| Siblings | 12.38 ± 3.89 | 9m/2f | 3.25 ± 3.15 | 9.13 ± 6.58 | 31.75 ± 31.92 | 2.06 ± 2.21 | 0 | 2.67 ± 0.7 |
| 1.91 ± 0.31 | ||||||||
| Controls | 13.44 ± 5.05 | 4m/5f | 1.11 ± 1.45 | 7.00 ± 3.32 | 28.22 ± 25.81 | 1.37 ± 2.06 | 0 | 2.50 ± 0.76 |
| 1.97 ± 0.07 | ||||||||
| p Value | 0.3939 | 0.0984 | < 0.0001 | 0.0911 | 0.2518 | < 0.0001 | < 0.0001 | < 0.0001 |
| 0.0017 |
Values are given by means ± Standard Deviation. M = male; F = female; Mean PD sites = Mean pocket depth of sites with PD > 4 mm; Mean PD all = mean PD of all sites; CAL = clinical attachment level of affected sites; BoP = bleeding on probing; PD site = Pocket depth from sampled site: DD = diseased site in LAP; DH = healthy site in LAP. †Statistically different from siblings and control children by ANOVA. ‡ Statistically different from DH site by paired t test.
In total, 422 bacterial species were analyzed in the subgingival plaque samples of all individuals. All samples collected were successfully analyzed. Of these, 52 bacterial species showed significant differences among groups for abundance (Tables 2 and 3) and 21 for prevalence (Fig.).
Table 2.
Significant Levels of Species Abundance in the Different Sites/Groups
| Most Abundant Species in LAP Disease Sites (DD) | DD | DH | HC | HS | p Value |
|---|---|---|---|---|---|
| Aggregatibacter actinomycetemcomitans_ot531_AA84 | 1.8235a | 0.2143b | 0.4444b | 1.2308ab | <.0001 |
| Aggregatibacter actinomycetemcomitans_ot531_P02 | 2.1765a | 0.4286b | 0.4444b | 1.5385ab | 0.0002 |
| Most Abundant Species in LAP Healthy Sites (DH) | DD | DH | HC | HS | p Value |
| Capnocytophaga sp clones BM058 and BU084_ot329_O08 | 0.0588a | 0.4286b | 0.2222ab | 0.3077ab | 0.0364 |
| Capnocytophaga sputigena_ot775_AC15 | 0.0000a | 0.1786b | 0.0000ab | 0.0000ab | 0.0308 |
| Catonella morbi and sp clone BR063_ot164_165_O56 | 0.7941a | 1.3214b | 0.6667ab | 1.0000ab | 0.0441 |
| Eubacterium sp clone 7 69_ot846_AB31 | 0.0000a | 0.1786b | 0.0000ab | 0.0000ab | 0.0028 |
| Eubacterium[11][G-7] yurii_ot377_W84 | 1.3235a | 2.1071b | 1.2222ab | 1.4615ab | 0.0344 |
| Fusobacterium periodontium_ot201_R20 | 0.2941a | 1.0714b | 0.5556ab | 0.6154ab | 0.0086 |
| Kingella denitrificans_ot582_X41 | 0.0294a | 0.2500b | 0.0000ab | 0.0000ab | 0.0436 |
| Prevotella melaninogenica and sp clone BE073_ot298_469_T81 | 0.0588a | 0.4286b | 0.0000ab | 0.0000ab | 0.0142 |
| Selenomonas sp clones DS071 and EW084_ot138_146_Q52 | 0.2647a | 0.7857b | 0.1111ab | 0.7692ab | 0.0214 |
| Selenomonas sp clones DS071 and EW084_ot138_146_X69 | 0.1176a | 0.5357b | 0.0000ab | 0.4615ab | 0.0088 |
| Streptococcus anginosus and intermedius_ot543_644_AB82 | 0.5294a | 1.3214b | 1.2222ab | 0.5385ab | 0.0048 |
| Streptococcus anginosus and intermedius_ot543_644_Q62 | 1.7647a | 2.8929b | 2.6667ab | 2.2308ab | 0.0021 |
| Streptococcus constellatus and intermedius_ot576_644_F48 | 0.9412a | 1.8214b | 1.7778ab | 1.1539ab | 0.0056 |
| Streptococcus mitis bv2 and sp clone FP064_ot069_398_Q64 | 0.1471a | 0.5357b | 0.4444ab | 0.2308ab | 0.0146 |
| Streptococcus sanguinis and sp clone C3MLM097_ot058_758_AB75 | 0.0882a | 0.7143b | 0.5556ab | 0.5385ab | 0.0026 |
| Streptococcus sanguinis and sp clone C3MLM097_ot058_758_AB78 | 0.1176a | 1.0714b | 0.6667ab | 0.6154ab | 0.0002 |
| Veillonella atypica and parvula_ot161_524_Q67 | 1.0000a | 2.0714b | 2.0000ab | 1.5385ab | 0.0066 |
| Veillonella EF509966 Crohns_not_oral_AD63-C | 0.8529a | 1.6786b | 1.5556ab | 1.2308ab | 0.0074 |
| Veillonella parvula_ot161_D96 | 0.0294a | 0.2143b | 0.1111ab | 0.0769ab | 0.0386 |
| Veillonella parvula_ot161_M04 | 0.3529a | 0.8571b | 0.6667ab | 0.5384ab | 0.0169 |
| Most Abundant Species in Healthy Control Sites (HC) | DD | DH | HC | HS | p Value |
| Bergeyella sp clone AK152_ot322_AD84 | 0.1176a | 0.1200ab | 0.6600b | 0.1500ab | 0.0210 |
| Campylobacter concisus_ot575_X33 | 0.0000a | 0.0000a | 0.1111b | 0.0000b | 0.0062 |
| Haemophilus parainfluenzae_ot718_W79 | 0.7941a | 1.1429a | 1.8889b | 1.7692b | 0.0412 |
| Neisseria flavescens_ot610_AA76 | 0.1176a | 0.2500ab | 0.5556b | 0.0769ab | 0.0357 |
| Rothia dentocariosa and mucilaginosa_ot587_681_E52 | 0.0000a | 0.1786ab | 0.3333b | 0.0769ab | 0.0304 |
| Streptococcus Cluster II_ot071_755_758_Q59 | 0.7353a | 1.7500a | 2.3333b | 1.4616b | 0.0007 |
| Streptococcus Cluster III_ot755_758_767_768_Q65 | 0.9706a | 1.7857b | 2.0000b | 1.2308ab | 0.0085 |
| Streptococcus constellatus and intermedius_ot576_644_AB77 | 0.7353a | 1.7857b | 2.0000b | 0.8462ab | 0.0019 |
| Streptococcus parasanguis I and II_ot411_721_AB05 | 0.1176a | 0.4286b | 0.6667b | 0.2308ab | 0.0101 |
| Treponema lecithinolyticum_ot653_D52 | 0.0000a | 0.0000a | 0.1111b | 0.0769b | 0.0524 |
| Most Abundant Species in Healthy Sibling Sites (HS) | DD | DH | HC | HS | p Value |
| Actinomyces Cluster II_ot180_181_671_701_AC99 | 0.0000a | 0.0000ab | 0.0000ab | 0.0769b | 0.0310 |
| Actinomyces meyeri and odontolyticus_ot671_701_AA88 | 0.0000a | 0.0000ab | 0.0000ab | 0.0769b | 0.0310 |
| Actinomyces sp strain B27SC_ot178_W02 | 0.0000a | 0.0000ab | 0.0000ab | 0.0769b | 0.0310 |
| Cardiobacterium valvulum_ot540_AD79 | 0.0000a | 0.0714a | 0.0000b | 0.4615b | 0.0003 |
| Cardiobacterium valvulum_ot540_AD80 | 0.0000a | 0.0357a | 0.0000b | 0.2308b | 0.0008 |
| Leptotrichia hofstadii_ot224_AA58 | 0.0000a | 0.0000ab | 0.0000ab | 0.1539b | 0.0310 |
| Porphyromonas endodontalis_ot273_N99 | 0.000a | 0.0000ab | 0.0000ab | 0.0769b | 0.0310 |
| Sphaerocytophaga S3_ot337_X23 | 0.0882a | 0.2857ab | 0.4444ab | 0.5385b | 0.0370 |
| SR1[G-1] sp _X112_ot345_AC72 | 0.0000a | 0.0000ab | 0.0000ab | 0.0769b | 0.0310 |
| SR1[G-1] sp _X112_ot345_AC73 | 0.0000a | 0.0000ab | 0.0000ab | 0.0769b | 0.0310 |
| Treponema denticola_ot584_O40 | 0.0000a | 0.0000ab | 0.0000ab | 0.0769b | 0.0310 |
| Treponema sp clone _T021_ot231_AC45 | 0.0000a | 0.0000ab | 0.0000ab | 0.0769b | 0.0310 |
Abundance values are represented here as the least-square mean intensity value (from HOMIM ranked signal scale 0-5) for each group. Means followed by different superscript letters represent statistical differences among groups by ANOVA. DD = diseased sites in children with disease; DH = healthy sites in children with disease; HS = healthy site in healthy sibling; HC = healthy site in healthy control child. Different letters show statistically significant differences among groups.
Table 3.
Most Abundant Species in Healthy and Diseased Individuals
| Most Abundant Species in Healthy Individuals | ||||
|---|---|---|---|---|
| Taxa | p Values | Fold-change | Mean | SD |
| Lautropia mirabilis_ot0.00122_X44 | 0.004672897 | 0.8911174 | 0.058425285 | 0.27918294 |
| Haemophilus parainfluenzae_ot718_W79 | 0 | 0.5493658 | 1.1729078 | 1.4559939 |
| Streptococcus Cluster II_ot0.00171_755_758_Q59 | 1.40E-04 | 0.6446244 | 1.3452182 | 1.3010002 |
| Campylobacter gracilis_ot623_Q0.0014 | 0 | 0.6073211 | 1.6900116 | 1.4961808 |
| Campylobacter gracilis_ot623_X34 | 0 | 0.58508325 | 2.1496668 | 1.5956601 |
| Capnocytophaga granulosa and sp clone BB167_ot325_326_AA89 | 0 | 0.49718076 | 1.7015518 | 1.6428522 |
| Most Abundant Species in LAP Individuals | ||||
| Taxa | p Values | Fold-change | Mean | SD |
| Solobacterium moorei_ot678_AC0.0012 | 0.00182243 | 1.3059351 | 0.33411482 | 0.74152595 |
| Filifactor alocis_ot539_AB94 | 0.001214953 | 1.3419528 | 0.9087584 | 1.6108342 |
| Aggregatibacter actinomycetemcomitans_ot531_AA84 | 0.001682243 | 1.2631507 | 1.1615744 | 1.7507974 |
| Parvimonas micra_ot111_L97 | 4.67E-05 | 1.5799938 | 1.4027699 | 1.5877612 |
| Aggregatibacter actinomycetemcomitans_ot531_P0.0012 | 4.67E-05 | 1.3636757 | 1.4258847 | 1.9681077 |
| Parvimonas micra_ot111_V0.0015 | 0 | 1.7198296 | 1.4487239 | 1.6045148 |
| Capnocytophaga sp clone _X0.00166_ot335_AD22 | 7.48E-04 | 1.285298 | 1.8162187 | 1.0944762 |
| Tannerella sp clone BU0.00163_ot286_T83 | 0.004299066 | 1.1626025 | 0.2996665 | 0.6835908 |
The Table shows the most abundant bacterial taxa in diseased and healthy groups by Rank products. SD = standard deviation. ‘Mean’ indicates mean abundance of species in the group (top, healthy or bottom, LAP). Fold-change indicates change in mean abundance between healthy and LAP groups.
Figure.
Bacterial species which showed significantly different prevalence among sites/groups. DD = diseased sites in children with disease; DH = healthy sites in children with disease; HS = healthy sites in healthy sibling; HC = healthy sites in healthy control children. Significant differences denoted by * DD vs. DH, † DD vs. HS, and ‡DD vs. HC.
Two species of Aa were more frequently detected in diseased sites in LAP individuals: Aa_ot531_AA84 (OR = 8.33, CI = 2.11 - 32.90, p = 0.0025) and Aa_ot531_P02 (OR = 5.82, CI = 1.79 - 18.97, p = 0.0034), along with Filifactor alocis_ot539_AB95 (OR = 2.31, CI = 1.06 - 5.01), when compared with healthy sites in LAP (Aa species) and HS (Aa and F. alocis) (Fig.). Interestingly, Aa was also found in 2/9 HC and 4/11 HS and a few healthy sites children with LAP, albeit in less abundance (Table 2).
The two probes of Aa mentioned above were also more abundant in diseased sites in LAP when compared with healthy sites in both LAP and HC (Table 2, p < 0.001). Some of the most abundant species in HC were Bergeyella sp, Campylobacter concisus, Haemophilus parainfluenzae, Rothia dentocariosa and mucilaginosa, Neisseria flavescens, Streptococcus sp, and Treponema lecithinolyticum, whereas the most abundant in HS were Actinomyces, Campylobacter, Capnocytophaga, Cardiobacterium valvulum, Porphyromonas endodontalis, Leptotrichia hofstadii, Sphaerocytophaga, and Treponema sp. (Table 2).
In comparisons of healthy and diseased individuals as a group, species such as Lautropia mirabilis, Haemophilus parainfluenzae, Streptococcus Cluster II, Campylobacter gracilis, and Capnocytophaga granulosa were most abundant in healthy individuals (p < 0.01), whereas Tannerella sp, Filifactor alocis, the two probes for Aa, Parvimonas micra, Capnocytophaga sp, and Solobacterium moorei were more abundant in children with LAP (p < 0.01, Table 3).
Discussion
The prevalence of aggressive periodontal disease in children and young adults in the US is around 1 to 2% and is estimated to be up to 3 times more prevalent in Blacks (Ickenstein et al., 1999). Although the prevalence of this disease is relatively low and is apparently confined to specific susceptible groups, early stages of this disease could easily go underdiagnosed until clearer signs of alveolar bone loss are detected in radiographic examination. Therefore, the detection of specific bacteria associated with this disease in children at a young age, before disease breakdown occurs, would be desirable for the successful prevention and/or treatment of this disease.
In the present investigation, we evaluated diseased and healthy sites of 31 children with LAP, 11 healthy siblings, and 9 healthy unrelated control children. We have identified several bacterial species that could be playing a destructive or even a possible protective role in this disease.
Aa was very strongly associated with LAP in this population, in both prevalence and abundance. This species has also been associated with AgP/LAP in previous studies (Kaldahl et al., 1988; Haffajee et al., 2003; Kaner et al., 2007). We also observed Aa to be very site-specific, since it was more prevalent and abundant in diseased vs. healthy sites in LAP. Similarly, Lopez et al. found 6% of healthy sites vs. 44% diseased sites harboring Aa in localized juvenile periodontitis in Chile (Lopez et al., 1995). This is an interesting finding, since this disease is localized to specific sites in the mouth.
Additionally, Aa was present in some healthy control children and siblings, as observed in other studies (Alaluusua and Asikainen, 1988; Yang et al., 2002; Riep et al., 2009). However, it was less prevalent and less abundant in these individuals when compared with LAP disease sites and slightly more prevalent and abundant in siblings when compared with control children, although that difference was not significant. Recent longitudinal evaluations of Aa in children and adolescents indicated that the presence of this species in healthy children could represent a risk marker for LAP initiation (Spinozzi and Langer, 1999; Haubek et al., 2008). A longitudinal analysis of these children will enable us to detect the possible initiation of disease in the healthy groups, especially the siblings, who are at greater risk for this disease.
Other species associated with diseased individuals included Parvimonas micra and Filifactor alocis, which is in agreement with previous studies (Kumar et al., 2003, 2006). P. gingivalis has been associated with AgP in other populations (Gajardo et al., 2005; Mayorga-Fayad et al., 2007); however, this species was not frequently present in this population.
An interesting finding in the present study was regarding health-associated species. Most of those were present in larger quantities and proportions in healthy sites, including in an individual with disease, such as Selenomonas sp, Veillonella, and Streptococcus. In contrast, some species not typically detected, such as Bergeyella sp, Kingella oralis, and Neisseria sp, were more frequently found in HC and HS. This could indicate that some health-associated species could be playing a possible protective role in maintaining periodontal health. Stingu et al. have reported a higher prevalence of S. sanguinis in healthy individuals compared with those with AgP (Stingu et al., 2008). These authors observed that the absence of S. sanguinis was associated with clinical periodontal breakdown. In addition, Colombo et al. reported that Capnocytophaga, Cardiobacterium, Haemophilus, Kingella, Lautropia, Neisseria, Rothia, Streptococcus, and Veillonella spp. were more associated with periodontal therapeutic success (Colombo et al., 2012). Thus, there is a possible protective role of healthy subgingival species in periodontal disease that needs to be further elucidated. Longitudinal analysis of treatment responses in this cohort and analysis of a greater number of individuals will enable us to associate some of these species with treatment response.
Finally, the pathogenesis of periodontitis does not seem to rely solely on bacterial composition. It also depends upon the immune and inflammatory responses to bacterial colonization of the gingival sulcus (Offenbacher, 1996; Page and Kornman, 1997). We have already reported a hyper-inflammatory response by an elevated release of inflammatory mediators both systemically (Shaddox et al., 2010) and locally (Alfant et al., 2008; Shaddox et al., 2011) in this LAP population. Therefore, there is a multitude of factors that could be associated with the rapid periodontal breakdown in LAP (for review, see Schenkein et al., 2007). Thus, questions remain to be answered to better define this disease and to enable us to establish proper treatment and prevention.
In summary, we have encountered a very similar pattern of LAP in African-Americans in north Florida. Specific bacteria, such as Aa, seem to play a destructive role in this disease, whereas other species may be playing a more protective role against LAP. Longitudinal evaluation of this group could lead us to important understanding of the role of these bacteria in the initiation and progression of LAP and its treatment.
Acknowledgments
The authors thank the doctors and staff in Leon County Dental Clinic for their assistance in coordinating our visits to the clinic, patient care, and their dental needs.
Footnotes
We acknowledge financial support of NIH/NIDCR (R01DE019456).
The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
References
- Alaluusua S, Asikainen S. (1988). Detection and distribution of Actinobacillus actinomycetemcomitans in the primary dentition. J Periodontol 59:504-507 [DOI] [PubMed] [Google Scholar]
- Alfant B, Shaddox LM, Tobler J, Magnusson I, Aukhil I, Walker C. (2008). Matrix metalloproteinase levels in children with aggressive periodontitis. J Periodontol 79:819-826 [DOI] [PubMed] [Google Scholar]
- Armitage GC. (1999). Development of a classification system for periodontal diseases and conditions. Ann Periodontol 4:1-6 [DOI] [PubMed] [Google Scholar]
- Colombo AP, Boches SK, Cotton SL, Goodson JM, Kent R, Haffajee AD, et al. (2009). Comparisons of subgingival microbial profiles of refractory periodontitis, severe periodontitis, and periodontal health using the human oral microbe identification microarray. J Periodontol 80:1421-1432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colombo AP, Bennet S, Cotton SL, Goodson JM, Kent R, Haffajee AD, et al. (2012). Impact of periodontal therapy on the subgingival microbiota of severe periodontitis: comparison between good responders and “refractory” subjects by the Human Oral Microbe Identification Microarray (HOMIM). J Periodontol [epub ahead of print 2/10/2012] (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gajardo M, Silva N, Gomez L, Leon R, Parra B, Contreras A, et al. (2005). Prevalence of periodontopathic bacteria in aggressive periodontitis patients in a Chilean population. J Periodontol 76:289-294 [DOI] [PubMed] [Google Scholar]
- Haffajee AD, Socransky SS, Gunsolley JC. (2003). Systemic anti-infective periodontal therapy. a systematic review. Ann Periodontol 8:115-181 [DOI] [PubMed] [Google Scholar]
- Haubek D, Poulsen K, Westergaard J, Dahlén G, Kilian M. (1996). Highly toxic clone of Actinobacillus actinomycetemcomitans in geographically widespread cases of juvenile periodontitis in adolescents of African origin. J Clin Microbiol 34:1576-1578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haubek D, Dirienzo JM, Tinoco EM, Westergaard J, Lopez NJ, Chung CP, et al. (1997). Racial tropism of a highly toxic clone of Actinobacillus actinomycetemcomitans associated with juvenile periodontitis. J Clin Microbiol 35:3037-3042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haubek D, Ennibi OK, Poulsen K, Vaeth M, Poulsen S, Kilian M. (2008). Risk of aggressive periodontitis in adolescent carriers of the JP2 clone of Aggregatibacter (Actinobacillus) actinomycetemcomitans in Morocco: a prospective longitudinal cohort study. Lancet 371:237-242 [DOI] [PubMed] [Google Scholar]
- Ickenstein GW, Klotz JM, Langohr HD. (1999). [Headache caused by Polycythemia vera. Classification of a headache under the heading of metabolic disturbances]. Schmerz 13:279-282 [in German]. [DOI] [PubMed] [Google Scholar]
- Kaldahl WB, Kalkwarf KL, Patil KD, Dyer JK, Bates RE. (1988). Evaluation of four modalities of periodontal therapy. Mean probing depth, probing attachment level and recession changes. J Periodontol 59:783-793 [DOI] [PubMed] [Google Scholar]
- Kaner D, Christan C, Dietrich T, Bernimoulin JP, Kleber BM, Friedmann A. (2007). Timing affects the clinical outcome of adjunctive systemic antibiotic therapy for generalized aggressive periodontitis. J Periodontol 78:1201-1208 [DOI] [PubMed] [Google Scholar]
- Kumar PS, Griffen AL, Barton JA, Paster BJ, Moeschberger ML, Leys EJ. (2003). New bacterial species associated with chronic periodontitis. J Dent Res 82:338-344 [DOI] [PubMed] [Google Scholar]
- Kumar PS, Leys EJ, Bryk JM, Martinez FJ, Moeschberger ML, Griffen AL. (2006). Changes in periodontal health status are associated with bacterial community shifts as assessed by quantitative 16S cloning and sequencing. J Clin Microbiol 44:3665-3673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung WK, Ngai VK, Yau JY, Cheung BP, Tsang PW, Corbet EF. (2005). Characterization of Actinobacillus actinomycetemcomitans isolated from young Chinese aggressive periodontitis patients. J Periodontal Res 40:258-268 [DOI] [PubMed] [Google Scholar]
- Lopez NJ, Mellado JC, Giglio MS, Leighton GX. (1995). Occurrence of certain bacterial species and morphotypes in juvenile periodontitis in Chile. J Periodontol 66:559-567 [DOI] [PubMed] [Google Scholar]
- Mayorga-Fayad I, Lafaurie GI, Contreras A, Castillo DM, Barón A, Aya Mdel R. (2007). [Subgingival microbiota in chronic and aggressive periodontitis in Bogota, Colombia: an epidemiological approach]. Biomedica 27:21-33 [in Spanish]. [PubMed] [Google Scholar]
- Offenbacher S. (1996). Periodontal diseases: pathogenesis. Ann Periodontol 1:821-878 [DOI] [PubMed] [Google Scholar]
- Page RC, Kornman KS. (1997). The pathogenesis of human periodontitis: an introduction. Periodontology 2000 14: 9-11 [DOI] [PubMed] [Google Scholar]
- Riep B, Edesi-Neuss L, Claessen F, Skarabis H, Ehmke B, Flemmig TF, et al. (2009). Are putative periodontal pathogens reliable diagnostic markers? J Clin Microbiol 47:1705-1711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schenkein HA, Barbour SE, Tew JG. (2007). Cytokines and inflammatory factors regulating immunoglobulin production in aggressive periodontitis. Periodontology 2000 45: 113-127 [DOI] [PubMed] [Google Scholar]
- Shaddox L, Wiedey J, Bimstein E, Magnuson I, Clare-Salzler M, Aukhil I, et al. (2010). Hyper-responsive phenotype in localized aggressive periodontitis. J Dent Res 89:143-148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaddox LM, Wiedey J, Calderon NL, Magnusson I, Bimstein E, Bidwell JA, et al. (2011). Local inflammatory markers and systemic endotoxin in aggressive periodontitis. J Dent Res 90:1140-1144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spinozzi G, Langer J. (1999). Spontaneous classification in action by a human-enculturated and language-reared bonobo (Pan paniscus) and common chimpanzees (Pan troglodytes). J Comp Psychol 113:286-296 [DOI] [PubMed] [Google Scholar]
- Stingu CS, Eschrich K, Rodloff AC, Schaumann R, Jentsch H. (2008). Periodontitis is associated with a loss of colonization by Streptococcus sanguinis. J Med Microbiol 57(Pt 4):495-499 [DOI] [PubMed] [Google Scholar]
- Thiha K, Takeuchi Y, Umeda M, Huang Y, Ohnishi M, Ishikawa I. (2007). Identification of periodontopathic bacteria in gingival tissue of Japanese periodontitis patients. Oral Microbiol Immunol 22:201-207 [DOI] [PubMed] [Google Scholar]
- Yang EY, Tanner AC, Milgrom P, Mokeem SA, Riedy CA, Spadafora AT, et al. (2002). Periodontal pathogen detection in gingiva/tooth and tongue flora samples from 18- to 48-month-old children and periodontal status of their mothers. Oral Microbiol Immunol 17:55-59 [DOI] [PubMed] [Google Scholar]
- Yang HW, Huang YF, Chan Y, Chou MY. (2005). Relationship of Actinobacillus actinomycetemcomitans serotypes to periodontal condition: prevalence and proportions in subgingival plaque. Eur J Oral Sci 113:28-33 [DOI] [PubMed] [Google Scholar]
- Zambon JJ, Christersson LA, Slots J. (1983). Actinobacillus actinomycetemcomitans in human periodontal disease. Prevalence in patient groups and distribution of biotypes and serotypes within families. J Periodontol 54:707-711 [DOI] [PubMed] [Google Scholar]