Abstract
Transforming growth factor β (TGF-β1) is a pleiotropic cytokine with many and complex effects in cell and tissue physiology. This is made possible by a very complex and interwoven signaling system, whose regulation continues to be the focus of a growing line of research. This complex regulation translates to a key role in cardiovascular physiology, hemostasis, and the blood–vessel interface. In accordance with this, the TGF-β1 pathway appears to be deregulated in related disorders, such as atherosclerotic vascular disease and myeloproliferative syndromes. It is expected that the growing amount of experimental and clinical research will yield medical advances in the applications of knowledge of the TGF-β1 pathway to diagnosis and therapeutics.
Keywords: transforming growth factor beta, pathway, Smads, non-Smads, atherosclerosis, myeloproliferative syndromes
Introduction
Transforming growth factor β (TGF-β1) is a pleiotropic cytokine, which has been demonstrated to regulate a wide array of biological processes. It plays a major role in the regulation of vascular function and hemostasis. Therefore, it can be considered as a putative therapeutic target in disorders of the blood–vessel interface, such as atherosclerosis and myeloproliferative syndromes. The present narrative review highlights the most important advances in the knowledge of TGF-β regulation in cardiovascular disease. This review has been prepared after a comprehensive search through MEDLINE. Search terms were “TGF beta”, “cardiovascular”, “atherosclerosis”, “myeloproliferative syndromes”, “pathway”, and “regulation”. A broader coverage of research strategy can be found in Gasparyan et al.1
Regulation of TGF-β1 physiology
The canonical TGF-β1 pathway
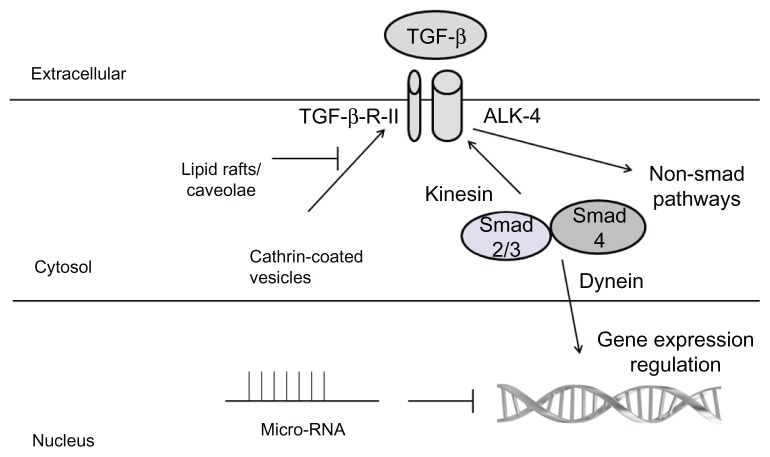
The regulation of TGF-β1 is shown in Figure 1. Briefly, active TGF-β1 is released from its latency-associated peptide by activating proteases. Then, it binds to the TGF-β-RII, which acts as a Ser/Thre kinase.2 This Ser/Thre kinase activity phosphorylates TGF-β-RI which may be present in several isoforms termed activinlike kinases (ALKs).3 In general, TGF-β1 stimulates ALK-5 and phosphorylates second messenger proteins termed Smads.4 Smad2 or Smad3 form a heterodimer with Smad4, and internalize into the nucleus to decrease the proliferation/apoptosis ratio,5 increase differentiation,6 and inhibit the expression of inflammatory molecules.7 In endothelial cells, TGF-β1 can stimulate ALK-4/5/7 and Smad2/3, or stimulate ALK-1 and Smad1/5/8 and increase cell proliferation.8 Smad6 and 7 are inhibitory Smads, since they bind Smad4 and inhibit its internalization into the nucleus.9 Endoglin is an accessory to the TGF-β receptor that seems to modulate receptor binding and ALK stimulation.10 It is mutated in hereditary hemorrhagic telangiectasia type 1,11 whereas ALK-1 is mutated in hereditary hemorrhagic telangiectasia type 2.12
Figure 1.
Summary of the main regulators of the TGF-β pathway.
Notes: Briefly, TGF-β binds to receptor type 2 and phosphorylates the type 1 receptor, whose main isoform is termed ALK-4 (activin-like kinase). This kinase phosphorylates and activates Smad2 or Smad3, which forms a heterodimer with Smad4, and internalizes into the nucleus to regulate gene expression. TGF-β can also act by means of non-Smad mediators, such as p38 MAP kinase and Small GTPases, like RhoA. Cytoskeleton and receptor endocytosis are additional mechanisms to regulate the TGF-β signaling. Gene expression can also be eventually modified by micro-RNAs.
Abbreviatons: TGF-β, transforming growth factor beta; Smad, second messenger protein; ALKs, activin-like kinases.
In addition to this classical Smad-dependent pathway, other crosstalks have been described among TGF-β1 and several signaling pathways,13 including mitogen-activated protein (MAP) kinases14 and small GTPases, such as RhoA.15 Non-Smad pathways seem to be especially important to regulate the TGF-β-mediated fibrotic effect. In particular, focal adhesion kinase has been shown to regulate TGF-β-mediated fibrosis. This is mediated by a TGF-β-mediated recruitment of the p85 subunit of PI3K to focal adhesion kinase to regulate signal transduction, which is independent of tyrosine kinase activation.16 Among MAP kinases, JNK plays a necessary role in mediating TGF-β-mediated epithelial-to-mesenchymal transition in rat peritoneal fibroblasts, in cooperation with Smad3.17 In addition, the ERK MAP kinase regulates epithelial-to-mesenchymal transition in mesothelial cells by involving nuclear factor-κB (NFκB);18 Conversely, p38 MAP kinase seems to inhibit this effect in the same cell model.19 This antifibrotic effect of TGF-β is also mediated by peroxisome proliferator-activated receptor-γ by preventing p300 recruitment, subsequent histone H4 hyperacetilation, and eventual collagen synthesis.20
New insights in TGF-β1 regulation
In recent years, a growing body of experimental medicine suggests an important role of several factors which may act (in a real-time manner) as rheostats for the fine tuning of the TGF-β1 pathway, and thus adapt cell response of TGF-β1 to a given cellular circumstance.
The first important factor is receptor endocytosis. Recent reports indicate that receptor endocytosis is a key event in proper signaling and receptor recycling.21 Moreover, it has been clarified that clathrin-coated pits-mediated endocytosis enhances TGF-β function,22 and that early endosomes behave as signaling organelles to promote TGF-β signaling. Conversely, however, the lipid rafts-caveolae endocytic system inhibits TGF-β signaling.23 Interestingly, it has been described that, given that caveolae localize in cholesterol-rich membrane domains, cholesterol itself inhibits TGB-β signaling in vitro,24 and this might mediate, at least in part, atherogenic effects of cholesterol in vivo. In fact, caveolin, a protein that is a key component of caveolae, physically interacts with TGF-β-R-I to block Smad signaling.25
The second key event is micro-RNA (miRNA) regulation.26 This is achieved by noncoding RNA fragments which are able to silence gene expression. In particular, the miRNA 200 family (miR-200a, miR-200b, miR-200c, miR-141, and miR-429) cooperate with TGF-β signaling to regulate epithelial-to-mesenchymal transition.27 Interestingly, other miRNAs are able to inhibit the antitumor effects of TGF-β and thus are accumulated in human tumors, as seen with the miRNA 25 cluster (miRNA 106b, miRNA 93, and miRNA 25) in gastric cancer,28 neuroblastoma, and multiple myeloma; and the miRNA 17–92 cluster (miRNA 17, miRNA 18a, miRNA 19a, miRNA 20a, miRNA 19b-1, miRNA 92a) in diffuse large B cell lymphoma and small-cell lung cancer.26 MiRNAs miRNA 106b-25 and miR-92 regulate TGF-β-mediated antiproliferative and apoptotic effects.29 In particular, miR-106b and miR-93 inhibit TGF-β-mediated cell cycle arrest, whereas miR-25 inhibits TGF-β-mediated apoptosis.26,29 Of note, this crosstalk between the TGF-β pathway and miRNA seems to be a bidirectional process. Thus, miRNA not only affects the TGF-β pathway, but also, miR-21 is directly upregulated by TGF-β1, and plays a key role in vascular smooth muscle cell differentiation.30 It is expected that this TGF-β-mediated effect also takes place in many other miRNAs. These effects seem to take place postranscriptionally by affecting the Drosha miRNA-stabilizing machinery.26 Therefore, miRNAs are plausible key regulators of the cell response of TGF-β, in a real-time and context-dependent manner.
A third emerging mechanism to control the complex regulation of TGF-β1 signaling is the cytoskeleton. Smads are tightly anchored to the cytoskeleton and constantly shuttle the cytoplasm and the nucleus in basal cell conditions.31 In fact, all Smads are associated to cell microtubules and their trafficking is controlled, at least in part, by microtubules-related proteins, such as kinesin for going to cell membrane receptors,32 and dynein when they direct to the nucleus.33 In cell culture models, nuclear accumulation of Smads has been considered to be a direct marker of TGF-β1 signaling,34,35 and this could be mediated by nuclear phosphatases, which dephosphorylate the C-terminal di-serine motifs Smads.36
Yet again, this link between TGF-β and cytoskeleton acts in a bidirectional manner, given that TGF-β regulates actin polymerization by the non-Smad-signaling pathways RhoA and p38,37 and by affecting epithelial-to-mesenchymal transition.
In recent years, several mathematical models have been developed that will predict the cell response of TGF-β1 in a given circumstance in silico, and thus help to design target-designed novel molecules, in order to modulate the important roles exerted by TGF-β1 signaling in health and disease.38 These models are based on a network of molecular components. In order to describe how a given parameter changes with time, systems of ordinary differential equations were incorporated to build a kinetic model, since these could express molecular changes (concentrations and biochemical modifications) over time, and relate these data to empirical ones.38
TGF-β1 in cardiovascular disease
TGF-β1 in vascular and hemostasis physiology
In general, TGF-β1 is considered as an anti-inflammatory cytokine in the vessel wall.39 In normal vessels, TGF-β1 inhibits endothelial40 and vascular smooth muscle41 cell proliferation. It also increases apoptosis to avoid excessive cellular accumulation,42 and stimulates vascular cell differentiation,43 with a parallel decrease of the expression of inflammatory molecules.44 In the blood–vessel interface, TGF-β1 decreases expression of cell adhesion molecules in vascular cells.45 In addition, in leukocytes, it decreases the activation of integrins46 and stimulates the function of endothelial progenitor cells, which may help to restore the denuded vessel wall.47 In hemostasis, TGF-β1 seems to behave as an antifibrinolytic factor48 and stimulates platelet-induced vascular repair.49 TGF-β1 is a normal component of platelet alpha granules.50 In fact, the vast majority of serum TGF-β1 comes from platelet degranulation.51
TGF-β1 in atherosclerosis
In atherosclerosis, TGF-β1 is considered to be an antiatherogenic factor, especially in the early stages of the disease, according to what has been termed the protective cytokine hypothesis.52 Thus, TGF-β1 inhibits excessive vascular smooth muscle cell accumulation in the neointima,53 and avoids plaque rupture by means of its stimulation of extracellular matrix synthesis and tissue repair.54 In addition, it controls local inflammation by stimulating Th3 function and regulatory T cells (CD3+/CD25+ cells).55 Therefore, it avoids the excessive immune attack (from both innate and acquired immunity mechanisms) that characterizes atherosclerotic vascular disease. 56 In the clinical arena, decreased serum levels of TGF-β1 have been correlated to clinical atherosclerosis.51 However, this parameter has remained an elusive atherosclerosis marker, given that these levels may vary according to the time course of the disease and age.57 The majority of serum TGF-β levels originate from platelets and thus are markers of platelet activation in atherosclerosis2 and rheumatoid arthritis.58 TGF-β levels can be calculated as an active or total (active and acid-activatable) form. In systemic lupus erythematous patients, a lower serum activation index has been associated with increased lymphocyte apoptosis, irreversible organ damage, disease duration, low-density lipoprotein, and increased carotid intima-media thickness.59 Endoglin is an accessory TGF-β receptor and soluble endoglin may interfere with TGF-β interaction with membrane-bound receptors and thus decrease TGF-β signaling.60 Increased levels of soluble endoglin have been related to atherosclerosis,61 as well as preeclampsia. 62
However, in late stages of the disease, TGF-β1 seems to behave as a proatherogenic factor by increasing excessive extracellular matrix,63 promotion of in-stent restenosis,64 and induction of pathologic vascular remodeling.65 In fact, it has been demonstrated that end-organ damage in hypertension has been related to increased levels of TGF-β1 in serum and urine.66 Moreover, in atherosclerotic vascular disease, it has been demonstrated that cells become insensitive to TGF-β1 signaling by means of decreased TGF-β1 activation,67 decreased receptor2,68 and Smad downregulation,2,69 altered endocytosis and intracellular trafficking pattern,21 or alteration of any of the other multiple cellular pathways that crosstalk with the TGF-β1 signaling pathway.2 Interestingly, many of these factors may be altered at the genetic level by means of congenital atherosclerotic-related plymorphisms70–72 and genetic determinants of aortic aneurysms.73 Moreover, even acquired mutations have been postulated to modulate these facts.74
TGF-β1 in myeloproliferative syndromes
Philadelphia-negative myeloproliferative syndromes (polycythemia vera, essential thrombocytosis, essential myelofibrosis) are clonal hematological neoplasms in which an increased risk of arterial thrombosis occurs. A growing body of clinical and experimental evidence suggests that these variable phenotypes can follow a graded natural history, from initial essential thrombocytosis to subsequent polycythemia vera, and eventual spent-phase secondary myelofibrosis.75 These three disorders are associated with increased risk of arterial thrombosis, and in polycythemia vera, this risk is 20% at 10 years.75
In essential thrombocytosis, the abnormal clone seems to lose sensitivity to the proliferation-control effects of TGF-β1.76 In polycythemia vera, the abnormal clone equally loses response to the cytokine.77
However, essential or secondary myelofibrosis is the chronic myeloproliferative syndrome which is associated with the shortest survival rate.78 The risk of thrombosis is similar to that found in essential thrombocythemia (1%–3% per patient per year).79 This is the variant of myeloproliferative syndrome which has the strongest link to dysregulation of the TGF-β1 pathway.78 In fact, TGF-β increases myelofibrosis in murine models.80 In cell culture models, TGF-β secretion seems to be regulated by NFκB.81 In myeloproliferative syndromes, there seems to be a progressive grading in TGF-β1 in the prefibrotic state, although established myelofibrosis has lower TGF-β1 levels.82 Higher TGF-β levels seem to be correlated with increased allelic charge of JAK2, and decreased EPC levels.82,83
Therapy of myelofibrosis is a clinical challenge and supportive care has been the only treatment to date.77 Current JAK-2 inhibitors have shown only a limited benefit in regard to spleen size.84 Advances in the knowledge of TGF-β signaling in myeloproliferative syndromes may guide the choice of synergistic novel therapies such as small-molecule TGF-β pathway blockers including, SB-431542/ALK-4 inhibitor of the ALK-4 kinase activity2, heat-shock protein inhibitors, NFκB inhibitors,85 or epigenetic drugs.86
Thus, progressive TGF-β dysfunction can be considered as a shared pathogenic event in atherosclerosis and Philadelphia-negative myeloproliferative syndromes, and a putative diagnostic and therapeutic tool.
Conclusion
TGF-β1 is a key factor in diseases affected by cardiovascular disorders, such as atherosclerosis and myeloproliferative syndromes. The current knowledge of the complex TGF-β1 regulation of physiological and pathological processes may help to design novel diagnostic techniques and target-designed innovative therapies.
Acknowledgment/disclosure
Our lab received support by FISS (Health Research Fund, PI080920) and Red Temática de Investigación Cardiovascular RECAVA (RD06/0014/1007), both from the Instituto de Salud Carlos III, Spanish Ministry of Health (ISCIII). The authors report no conflicts of interest in this work.
Footnotes
Authors’ contributions
SR conceived the idea of the manuscript and wrote the first schematic draft. SR and TT designed the search strategy. SR, JN-D, MR, UM, and TT performed the review of the literature. All authors collaborated in the definitive version, and approved the final draft of the manuscript.
References
- 1.Gasparyan AY, Ayvazyan L, Blackmore H, Kitas GD. Writing a narrative biomedical review: considerations for authors, peer reviewers, and editors. Rheumatol Int. 2011;31(11):1409–1417. doi: 10.1007/s00296-011-1999-3. [DOI] [PubMed] [Google Scholar]
- 2.Redondo S, Santos-Gallego CG, Tejerina T. TGF-beta1: a novel target for cardiovascular pharmacology. Cytokine Growth Factor Rev. 2007;18(3–4):279–286. doi: 10.1016/j.cytogfr.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 3.Lebrin F, Goumans MJ, Jonker L, et al. Endoglin promotes endothelial cell proliferation and TGF-beta/ALK1 signal transduction. EMBO J. 2004;23(20):4018–4028. doi: 10.1038/sj.emboj.7600386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Loureiro J, Schilte M, Aguilera A, et al. BMP-7 blocks mesenchymal conversion of mesothelial cells and prevents peritoneal damage induced by dialysis fluid exposure. Nephrol Dial Transplant. 2010;25(4):1098–1108. doi: 10.1093/ndt/gfp618. [DOI] [PubMed] [Google Scholar]
- 5.Redondo S, Ruiz E, Santos-Gallego CG, Padilla E, Tejerina T. Pioglitazone induces vascular smooth muscle cell apoptosis through a peroxisome proliferator-activated receptor-gamma, transforming growth factor-beta1, and a Smad2-dependent mechanism. Diabetes. 2005;54(3):811–817. doi: 10.2337/diabetes.54.3.811. [DOI] [PubMed] [Google Scholar]
- 6.Tang Y, Yang X, Friesel RE, Vary CP, Liaw L. Mechanisms of TGF-β-induced differentiation in human vascular smooth muscle cells. J Vasc Res. 2011;48(6):485–494. doi: 10.1159/000327776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Azuma M, Motegi K, Aota K, Yamashita T, Yoshida H, Sato M. TGF-beta1 inhibits NF-kappaB activity through induction of IkappaB-alpha expression in human salivary gland cells: a possible mechanism of growth suppression by TGF-beta1. Exp Cell Res. 1999;250(1):213–222. doi: 10.1006/excr.1999.4503. [DOI] [PubMed] [Google Scholar]
- 8.Goumans MJ, Valdimarsdottir G, Itoh S, et al. Activin receptor-like kinase (ALK)1 is an antagonistic mediator of lateral TGFbeta/ALK5 signaling. Mol Cell. 2003;12(4):817–828. doi: 10.1016/s1097-2765(03)00386-1. [DOI] [PubMed] [Google Scholar]
- 9.Tojo M, Takebe A, Takahashi S, et al. Smad7-deficient mice show growth retardation with reduced viability. J Biochem. 2012;151(6):621–631. doi: 10.1093/jb/mvs022. [DOI] [PubMed] [Google Scholar]
- 10.Lebrin F, Deckers M, Bertolino P, Ten Dijke P. TGF-beta receptor function in the endothelium. Cardiovasc Res. 2005;65(3):599–608. doi: 10.1016/j.cardiores.2004.10.036. [DOI] [PubMed] [Google Scholar]
- 11.McAllister KA, Grogg KM, Johnson DW, et al. Endoglin, a TGF-beta binding protein of endothelial cells, is the gene for hereditary haemorrhagic telangiectasia type 1. Nat Genet. 1994;8(4):345–351. doi: 10.1038/ng1294-345. [DOI] [PubMed] [Google Scholar]
- 12.Berg JN, Gallione CJ, Stenzel TT, et al. The activin receptor-like kinase 1 gene: genomic structure and mutations in hereditary hemorrhagic telangiectasia type 2. Am J Hum Genet. 1997;61(1):60–67. doi: 10.1086/513903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moustakas A, Heldin CH. Non-Smad TGF-beta signals. J Cell Sci. 2005;118(Pt 16):3573–3584. doi: 10.1242/jcs.02554. [DOI] [PubMed] [Google Scholar]
- 14.Yang F, Chung AC, Huang XR, Lan HY. Angiotensin II induces connective tissue growth factor and collagen I expression via transforming growth factor-beta-dependent and -independent Smad pathways: the role of Smad3. Hypertension. 2009;54(4):877–884. doi: 10.1161/HYPERTENSIONAHA.109.136531. [DOI] [PubMed] [Google Scholar]
- 15.Tsapara A, Luthert P, Greenwood J, Hill CS, Matter K, Balda MS. The RhoA activator GEF-H1/Lfc is a transforming growth factor-beta target gene and effector that regulates alpha-smooth muscle actin expression and cell migration. Mol Biol Cell. 2010;21(6):860–870. doi: 10.1091/mbc.E09-07-0567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hong M, Wilkes MC, Penheiter SG, Gupta SK, Edens M, Leof EB. Non-Smad transforming growth factor-β signaling regulated by focal adhesion kinase binding the p85 subunit of phosphatidylinositol 3-kinase. J Biol Chem. 2011;286(20):17841–17850. doi: 10.1074/jbc.M111.233676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu Q, Zhang Y, Mao H, et al. A crosstalk between the Smad and JNK signaling in the TGF-β-induced epithelial-mesenchymal transition in rat peritoneal mesothelial cells. PLoS One. 2012;7(2):e32009. doi: 10.1371/journal.pone.0032009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Strippoli R, Benedicto I, Pérez Lozano ML, Cerezo A, López-Cabrera M, del Pozo MA. Epithelial-to-mesenchymal transition of peritoneal mesothelial cells is regulated by an ERK/NF-kappaB/Snail1 pathway. Dis Model Mech. 2008;1(4–5):264–274. doi: 10.1242/dmm.001321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Strippoli R, Benedicto I, Foronda M, et al. p38 maintains E-cadherin expression by modulating TAK1-NF-kappa B during epithelial-to-mesenchymal transition. J Cell Sci. 2010;123(Pt 24):4321–4331. doi: 10.1242/jcs.071647. [DOI] [PubMed] [Google Scholar]
- 20.Ghosh AK, Bhattacharyya S, Wei J, et al. Peroxisome proliferator-activated receptor-gamma abrogates Smad-dependent collagen stimulation by targeting the p300 transcriptional coactivator. FASEB J. 2009;23(9):2968–2977. doi: 10.1096/fj.08-128736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen YG. Endocytic regulation of TGF-beta signaling. Cell Res. 2009;19(1):58–70. doi: 10.1038/cr.2008.315. [DOI] [PubMed] [Google Scholar]
- 22.Hayes S, Chawla A, Corvera S. TGF beta receptor internalization into EEA1-enriched early endosomes: role in signaling to Smad2. J Cell Biol. 2002;158(7):1239–1249. doi: 10.1083/jcb.200204088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Razani B, Zhang XL, Bitzer M, von Gersdorff G, Böttinger EP, Lisanti MP. Caveolin-1 regulates transforming growth factor (TGF)-beta/SMAD signaling through an interaction with the TGF-beta type I receptor. J Biol Chem. 2001;276(9):6727–6738. doi: 10.1074/jbc.M008340200. [DOI] [PubMed] [Google Scholar]
- 24.Chen CL, Liu IH, Fliesler SJ, Han X, Huang SS, Huang JS. Cholesterol suppresses cellular TGF-beta responsiveness: implications in atherogenesis. J Cell Sci. 2007;120(Pt 20):3509–3521. doi: 10.1242/jcs.006916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhao B, Wang Q, Du J, Luo S, Xia J, Chen YG. PICK1 promotes caveolin-dependent degradation of TGF-β type I receptor. Cell Res. 2012 doi: 10.1038/cr.2012.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ikushima H, Miyazono K. Cellular context-dependent “colors” of transforming growth factor-beta signaling. Cancer Sci. 2010;101(2):306–312. doi: 10.1111/j.1349-7006.2009.01441.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gregory PA, Bert AG, Paterson EL, et al. The miR-200 family and miR-205 regulate epithelial to mesenchymal transition by targeting ZEB1 and SIP1. Nat Cell Biol. 2008;10(5):593–601. doi: 10.1038/ncb1722. [DOI] [PubMed] [Google Scholar]
- 28.Petrocca F, Visone R, Onelli MR, et al. E2F1-regulated microRNAs impair TGFbeta-dependent cell-cycle arrest and apoptosis in gastric cancer. Cancer Cell. 2008;13(3):272–286. doi: 10.1016/j.ccr.2008.02.013. [DOI] [PubMed] [Google Scholar]
- 29.Ventura A, Young AG, Winslow MM, et al. Targeted deletion reveals essential and overlapping functions of the miR-17 through 92 family of miRNA clusters. Cell. 2008;132(5):875–886. doi: 10.1016/j.cell.2008.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kumarswamy R, Volkmann I, Jazbutyte V, Dangwal S, Park DH, Thum T. Transforming growth factor-β-induced endothelial-to-mesenchymal transition is partly mediated by microRNA-21. Arterioscler Thromb Vasc Biol. 2012;32(2):361–369. doi: 10.1161/ATVBAHA.111.234286. [DOI] [PubMed] [Google Scholar]
- 31.Hata A, Davis BN. Control of microRNA biogenesis by TGFbeta signaling pathway-A novel role of Smads in the nucleus. Cytokine Growth Factor Rev. 2009;20(5–6):517–521. doi: 10.1016/j.cytogfr.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Batut J, Howell M, Hill CS. Kinesin-mediated transport of Smad2 is required for signaling in response to TGFbeta ligands. Dev Cell. 2007;12(2):261–274. doi: 10.1016/j.devcel.2007.01.010. [DOI] [PubMed] [Google Scholar]
- 33.Jin Q, Ding W, Mulder KM. Requirement for the dynein light chain km23-21 in a Smad2-dependent transforming growth factor-beta signaling pathway. J Bio Chem. 2007;282(26):19122–19132. doi: 10.1074/jbc.M609915200. [DOI] [PubMed] [Google Scholar]
- 34.Kurisaki A, Kose S, Yoneda Y, Heldin CH, Moustakas A. Transforming growth factor-beta induces nuclear import of Smad3 in an importin-beta1 and Ran-dependent manner. Mol Biol Cell. 2001;12(4):1079–1091. doi: 10.1091/mbc.12.4.1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chen HB, Rud JG, Lin k, Xu H. Nuclear targeting of transforming growth factor-beta-activated Smad complexes. J Biol Chem. 2005;280(22):21329–21336. doi: 10.1074/jbc.M500362200. [DOI] [PubMed] [Google Scholar]
- 36.Knockaert M, Sapkota G, Alarcón C, Massaqué J, Brivanlou AH. Unique players in the BMP pathway: small C-terminal domain phosphatases dephosphorylate Smad1 to attenuate BMP signaling. Proc Natl Acad Sci U S A. 2006;103(32):11940–11945. doi: 10.1073/pnas.0605133103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vardouli L, Moustakas A, Stournaras C. LIM kinase and cofilin phosphorylation mediate actin cytoskeleton reorganization induced by transforming growth factor-beta. J Biol Chem. 2005;280(12):11448–11457. doi: 10.1074/jbc.M402651200. [DOI] [PubMed] [Google Scholar]
- 38.Clarke DC, Liu X. Decoding the quantitative nature of TGF-beta/Smad signaling. Trends Cell Biol. 2008;18(9):430–442. doi: 10.1016/j.tcb.2008.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lebastchi AH, Khan SF, Qin L, et al. Transforming growth factor beta expression by human vascular cells inhibits interferon gamma production and arterial media injury by alloreactive memory T cells. Am J Transplant. 2011;11(11):2332–2341. doi: 10.1111/j.1600-6143.2011.03676.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Castanares C, Redondo-Horcajo M, Magán-Marchal N, ten Dijke P, Lamas S, Rodríguez-Pascual F. Signaling by ALK5 mediates TGF-beta-induced ET-1 expression in endothelial cells: a role for migration and proliferation. J Cell Sci. 2007;120(Pt 7):1256–1266. doi: 10.1242/jcs.03419. [DOI] [PubMed] [Google Scholar]
- 41.Redondo S, Santos-Gallego CG, Ganado P, et al. Acetylsalicylic acid inhibits cell proliferation by involving transforming growth factor-beta. Circulation. 2003;107(4):626–629. doi: 10.1161/01.cir.0000045664.75269.a5. [DOI] [PubMed] [Google Scholar]
- 42.Ruiz E, Redondo S, Gordillo-Moscoso A, Tejerina T. Pioglitazone induces apoptosis in human vascular smooth muscle cells from diabetic patients involving the transforming growth factor-beta/activin receptor-like kinase-4/5/7/Smad2 signaling pathway. J Pharmacol Exp Ther. 2007;321(2):431–438. doi: 10.1124/jpet.106.114934. [DOI] [PubMed] [Google Scholar]
- 43.Jaffe M, Sesti C, Washington IM, et al. Transforming growth factor-β signaling in myogenic cells regulates vascular morphogenesis, differentiation, and matrix synthesis. Arterioscler Thromb Vasc Biol. 2012;32(1):e1–e11. doi: 10.1161/ATVBAHA.111.238410. [DOI] [PubMed] [Google Scholar]
- 44.Feinberg MW, Watanabe M, Lebedeva MA, et al. Transforming growth factor-beta1 inhibition of vascular smooth muscle cell activation is mediated via Smad3. J Biol Chem. 2004;279(16):16388–16393. doi: 10.1074/jbc.M309664200. [DOI] [PubMed] [Google Scholar]
- 45.Walshe TE, Dole VS, Maharaj AS, Pattern IS, Wagner DD, D’Amore PA. Inhibition of VEGF or TGF-{beta} signaling activates endothelium and increases leukocyte rolling. Arterioscler Thromb Vasc Biol. 2009;29(8):1185–1192. doi: 10.1161/ATVBAHA.109.186742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Basoni C, Nobles M, Grimshaw A, et al. Inhibitory control of TGF-beta1 on the activation of Rap1, CD11b, and transendothelial migration of leukocytes. FASEB J. 2005;19(7):822–824. doi: 10.1096/fj.04-3085fje. [DOI] [PubMed] [Google Scholar]
- 47.Redondo S, Hristov M, Gümbel D, Tejerina T, Weber C. Biphasic effect of pioglitazone on isolated human endothelial progenitor cells: involvement of peroxisome proliferator-activated receptor-gamma and transforming growth factor-beta1. Thromb Haemost. 2007;97(6):979–987. [PubMed] [Google Scholar]
- 48.Vayalil PK, Olman M, Murphy-Ullrich JE, Postlethwait EM, Liu RM. Glutathione restores collagen degradation in TGF-beta-treated fibroblasts by blocking plasminogen activator inhibitor-1 expression and activating plasminogen. Am J Physiol Lung Cell Mol Physiol. 2005;289(6):L937–L945. doi: 10.1152/ajplung.00150.2005. [DOI] [PubMed] [Google Scholar]
- 49.Anitua E, Aguirre JJ, Algorta J, et al. Effectiveness of autologous preparation rich in growth factors for the treatment of chronic cutaneous ulcers. J Biomed Mater Res B Appl Biomater. 2008;84(2):415–421. doi: 10.1002/jbm.b.30886. [DOI] [PubMed] [Google Scholar]
- 50.Meyer A, Wang W, Qu J, et al. Platelet TGF-β1 contributions to plasma TGF-β1, cardiac fibrosis, and systolic dysfunction in a mouse model of pressure overload. Blood. 2012;119(4):1064–1074. doi: 10.1182/blood-2011-09-377648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Grainger DJ, Mosedale DE, Metcalfe JC, Weissberg PL, Kemp PR. Active and acid-activatable TGF-beta in human sera, platelets and plasma. Clin Chim Acta. 1995;235(1):11–31. doi: 10.1016/0009-8981(94)05995-4. [DOI] [PubMed] [Google Scholar]
- 52.Grainger DJ. Transforming growth factor beta and atherosclerosis: so far, so good for the protective cytokine hypothesis. Arterioscler Thromb Vasc Biol. 2004;24(3):399–404. doi: 10.1161/01.ATV.0000114567.76772.33. [DOI] [PubMed] [Google Scholar]
- 53.Lutgens E, Gijbels M, Smook M, et al. Transforming growth factor-beta mediates balance between inflammation and fibrosis during plaque progression. Arterioscler Thromb Vasc Biol. 2002;22(6):975–982. doi: 10.1161/01.atv.0000019729.39500.2f. [DOI] [PubMed] [Google Scholar]
- 54.Dai J, Michineau S, Franck G, et al. Long term stabilization of expanding aortic aneurysms by a short course of cyclosporine A through transforming growth factor-beta induction. PLoS One. 2011;6(12):e28903. doi: 10.1371/journal.pone.0028903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ji QW, Guo M, Zheng JS, et al. Downregulation of T helper cell type 3 in patients with acute coronary syndrome. Arch Med Res. 2009;40(4):285–293. doi: 10.1016/j.arcmed.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 56.Koenen RR, Weber C. Chemokines: established and novel targets in atherosclerosis. EMBO Mol Med. 2011;3(12):713–725. doi: 10.1002/emmm.201100183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Okamoto Y, Gotoh Y, Uemura O, Tanaka S, Ando T, Nishida M. Age-dependent decrease in serum transforming growth factor (TGF)-beta 1 in healthy Japanese individuals; population study of serum TGF-beta 1 level in Japanese. Dis Markers. 2005;21(2):71–74. doi: 10.1155/2005/381215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gasparyan AY, Stavropoulos-Kalinoglou A, Mikhailidis DP, Douglas KM, Kitas GD. Platelet function in rheumatoid arthritis: arthritic and cardiovascular implications. Rheumatol Int. 2011;31(2):153–164. doi: 10.1007/s00296-010-1446-x. [DOI] [PubMed] [Google Scholar]
- 59.Jackson M, Ahmad Y, Bruce IN, Coupes B, Brenchley PE. Activation of transforming growth factor-beta1 and early atherosclerosis in systemic lupus erythematosus. Arthritis Res Ther. 2006;8(3):R81. doi: 10.1186/ar1951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.López-Novoa JM, Bernabeu C. The physiological role of endoglin in the cardiovascular system. Am J Physiol Heart Circ Physiol. 2010;299(4):H959–H974. doi: 10.1152/ajpheart.01251.2009. [DOI] [PubMed] [Google Scholar]
- 61.Blázquez-Medela AM, García-Ortiz L, Gómez-Marcos MA, et al. Increased plasma soluble endoglin levels as an indicator of cardiovascular alterations in hypertensive and diabetic patients. BMC Med. 2010;8:86. doi: 10.1186/1741-7015-8-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.López-Novoa JM. Soluble endoglin is an accurate predictor and a pathogenic molecule in pre-eclampsia. Nephrol Dial Transplant. 2007;22(3):712–714. doi: 10.1093/ndt/gfl768. [DOI] [PubMed] [Google Scholar]
- 63.Dees C, Akhmetshina A, Zerr P, et al. Platelet-derived serotonin links vascular disease and tissue fibrosis. J Exp Med. 2011;208(5):961–972. doi: 10.1084/jem.20101629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Pallero MA, Talbert Roden M, Chen YF, et al. Stainless steel ions stimulate increased thrombospondin-1-dependent TGF-beta activation by vascular smooth muscle cells: implications for in-stent restenosis. J Vasc Res. 2010;47(4):309–322. doi: 10.1159/000265565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kieć-Wilk B, Stolarz-Skrzypek K, Sliwa A, Zdienicka A, Kawecka-Jaszcz K. Peripheral blood concentrations of TGFβ1, IGF-1 and bFGF and remodelling of the left ventricle and blood vessels in hypertensive patients. Kardiol Pol. 2010;68(9):996–1002. [PubMed] [Google Scholar]
- 66.Laviades C, Varo N, Díez J. Transforming growth factor beta in hypertensives with cardiorenal damage. Hypertension. 2000;36(4):517–522. doi: 10.1161/01.hyp.36.4.517. [DOI] [PubMed] [Google Scholar]
- 67.Sakamoto Y, Miyazaki A, Tamagawa H, Wang GP, Horiuchi S. Specific interaction of oxidized low-density lipoprotein with thrombospondin-1 inhibits transforming growth factor-beta from its activation. Atherosclerosis. 2005;183(1):85–93. doi: 10.1016/j.atherosclerosis.2005.02.032. [DOI] [PubMed] [Google Scholar]
- 68.McCaffrey TA, Du B, Fu C, et al. The expression of TGF-beta receptors in human atherosclerosis: evidence for acquired resistance to apoptosis due to receptor imbalance. J Mol Cell Cardiol. 1999;31(9):1627–1642. doi: 10.1006/jmcc.1999.0999. [DOI] [PubMed] [Google Scholar]
- 69.Kalinina N, Agrotis A, Antropova Y, et al. Smad expression in human atherosclerotic lesions: evidence for impaired TGF-beta/Smad signaling in smooth muscle cells of fibrofatty lesions. Arterioscler Thromb Vasc Biol. 2004;24(8):1391–1396. doi: 10.1161/01.ATV.0000133605.89421.79. [DOI] [PubMed] [Google Scholar]
- 70.Rao M, Guo D, Jaber BL, Tighiouart H, Pereira BJ, Balakrishnan VS for HEMO Study Group. Transforming growth factor-beta 1 gene polymorphisms and cardiovascular disease in hemodialysis patients. Kidney Int. 2004;66(1):419–427. doi: 10.1111/j.1523-1755.2004.00748.x. [DOI] [PubMed] [Google Scholar]
- 71.Sie MP, Uitterlinden AG, Bos MJ, et al. TGF-beta 1 polymorphisms and risk of myocardial infarction and stroke: the Rotterdam Study. Stroke. 2006;37(11):2667–2671. doi: 10.1161/01.STR.0000244779.30070.1a. [DOI] [PubMed] [Google Scholar]
- 72.Peng Z, Zhan L, Chen S, Xu E. Association of transforming growth factor-β1 gene C-509T and T869C polymorphisms with atherosclerotic cerebral infarction in the Chinese: a case-control study. Lipids Health Dis. 2011;10:100. doi: 10.1186/1476-511X-10-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Biros E, Norman PE, Jones GT, et al. Meta-analysis of the association between single nucleotide polymorphisms in TGF-β receptor genes and abdominal aortic aneurysm. Atherosclerosis. 2011;219(1):218–223. doi: 10.1016/j.atherosclerosis.2011.07.105. [DOI] [PubMed] [Google Scholar]
- 74.Clark KJ, Cary NR, Grace AA, Metcalfe JC. Microsatellite mutation of type II transforming growth factor-beta receptor is rare in atherosclerotic plaques. Arterioscler Thromb Vasc Biol. 2001;21(4):555–559. doi: 10.1161/01.atv.21.4.555. [DOI] [PubMed] [Google Scholar]
- 75.Alvarez-Larrán A, Pereira A, Cervantes F, et al. Assessment and prognostic value of the European LeukemiaNet criteria for clinicohematologic response, resistance, and intolerance to hydroxyurea in polycythemia vera. Blood. 2012;119(6):1363–1369. doi: 10.1182/blood-2011-10-387787. [DOI] [PubMed] [Google Scholar]
- 76.Kuroda H, Matsunaga T, Terui T, et al. Decrease of Smad4 gene expression in patients with essential thrombocythaemia may cause an escape from suppression of megakaryopoiesis by transforming growth factor-beta1. Br J Haematol. 2004;124(2):211–220. doi: 10.1046/j.1365-2141.2003.04755.x. [DOI] [PubMed] [Google Scholar]
- 77.Li J, Bench AJ, Huntly BJ, Green AR. Mutation and methylation analysis of the transforming growth factor beta receptor II gene in polycythaemia vera. Br J Haematol. 2001;115(4):872–880. doi: 10.1046/j.1365-2141.2001.03215.x. [DOI] [PubMed] [Google Scholar]
- 78.Vannucchi AM. Management of myelofibrosis. Hematology Am Soc Hematol Educ Program. 2011;2011:222–230. doi: 10.1182/asheducation-2011.1.222. [DOI] [PubMed] [Google Scholar]
- 79.Ponce CC, de Lourdes F, Chauffaille M, Ihara SS, Silva MR. The relationship of the active and latent forms of TGF-β1 with marrow fibrosis in essential thrombocythemia and primary myelofibrosis. Med Oncol. 2011 Dec 27; doi: 10.1007/s12032-011-0144-1. [Epub ahead of print.] [DOI] [PubMed] [Google Scholar]
- 80.Gastinne T, Vigant F, Lavenu-Bombled C, et al. Adenoviral-mediated TGF-beta1 inhibition in a mouse model of myelofibrosis inhibit bone marrow fibrosis development. Exp Hematol. 2007;35(1):64–74. doi: 10.1016/j.exphem.2006.08.016. [DOI] [PubMed] [Google Scholar]
- 81.Rameshwar P, Narayanan R, Qian J, Denny TN, Colon C, Gascon P. NF-kappa B as a central mediator in the induction of TGF-beta in monocytes from patients with idiopathic myelofibrosis: an inflammatory response beyond the realm of homeostasis. J Immunol. 2000;165(4):2271–2277. doi: 10.4049/jimmunol.165.4.2271. [DOI] [PubMed] [Google Scholar]
- 82.Campanelli R, Rosti V, Villani L, et al. Evaluation of the bioactive and total transforming growth factor β1 levels in primary myelofibrosis. Cytokine. 2011;53(1):100–106. doi: 10.1016/j.cyto.2010.07.427. [DOI] [PubMed] [Google Scholar]
- 83.Sozer S, Wang X, Zhang W, et al. Circulating angiogenic monocyte progenitor cells are reduced in JAK2V617F high allele burden myeloproliferative disorders. Blood Cells Mol Dis. 2008;41(3):284–291. doi: 10.1016/j.bcmd.2008.06.008. [DOI] [PubMed] [Google Scholar]
- 84.Verstovsek S, Kantarjian HM, Estrov Z, et al. Long-term outcomes of 107 patients with myelofibrosis receiving JAK1/JAK2 inhibitor ruxolitinib: survival advantage in comparison to matched historical controls. Blood. 2012;120(6):1201–1209. doi: 10.1182/blood-2012-02-414631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Wagner-Ballon O, Pisani DF, Gastinne T, et al. Proteasome inhibitor bortezomib impairs both myelofibrosis and osteosclerosis induced by high thrombopoietin levels in mice. Blood. 2007;110(1):345–353. doi: 10.1182/blood-2006-10-054502. [DOI] [PubMed] [Google Scholar]
- 86.Thepot S, Itzykson R, Seegers V, et al. for Groupe Francophone des Myelodysplasies (GFM) Treatment of progression of Philadelphia-negative myeloproliferative neoplasms to myelodysplastic syndrome or acute myeloid leukemia by azacitidine: a report on 54 cases on the behalf of the Groupe Francophone des Myelodysplasies (GFM) Blood. 2010;116(19):3735–3742. doi: 10.1182/blood-2010-03-274811. [DOI] [PubMed] [Google Scholar]