Abstract
Background
Fibrates comprise a class of well-established antilipidemic agents that significantly reduce cardiovascular events. Given the concerns of cancer with fibrate therapy, we undertook a systematic review and meta-analysis to investigate the effects of fibrates on cancer outcomes.
Methods
We systematically searched Medline, Scopus, SCI Expanded, and the Cochrane Library for studies published up to 2012. We included randomized controlled trials (RCTs) that evaluated a fibrate therapy compared with placebo, had a minimum duration of two years, and reported data on the incidence of and/or deaths from cancer during the trial. Reviews of each study were performed and the relative data were abstracted. Pooled relative risk estimates (RR) and 95% confidence intervals (CIs) were calculated using the inverse variance weighted approach. Subgroup, sensitivity and meta-regression analyses were also conducted.
Results
Seventeen RCTs, involving 44,929 participants with an average follow-up of 5.2 years, contributed to the analysis. The degree of variability between trials was consistent with what would be expected to occur by chance alone. The quantitative synthesis of data retrieved from the RCTs was not indicative of a fibrate effect on cancer incidence (780 [fibrate] vs 814 [control]; RR = 1.02, 95% CI 0.92–1.12) or cancer death (385 [fibrate] vs 377 [control]; RR = 1.06, 95% CI: 0.92–1.22). When the analysis was restricted to major RCTs, the results did not substantially change. Similarly, we found no evidence of differential effects by length of follow-up or type of fibrate. Insignificant results were also obtained for the role of fibrates in cancers of the respiratory tract, breast, colon, gastrointestinal tract, prostate, genitourinary tract, or in melanoma.
Conclusion
Our findings demonstrate that fibrates have a neutral effect on cancer outcomes. However, it is important to continue monitoring their long-term safety profiles.
Introduction
Fibrates comprise an important class of therapeutic agents for the management of dyslipidemia. They are agonists of the peroxisome proliferator-activated receptors alpha (PPAR-α), which are mainly expressed in liver, heart and skeletal muscle [1]. Fibrates have been shown to stimulate the expression of genes involved in fatty acid and lipoprotein metabolism, resulting in a shift from hepatic fat synthesis to fat oxidation [2]. This leads to a substantial reduction in serum triglycerides and an increase in high-density lipoprotein cholesterol levels. Though cardiovascular protection using antilipidemic agents has largely been dominated by the 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors (statins) since the 1990s, fibrates have been particularly useful in patients with primary hypertriglyceridemia, mixed hyperlipidemia, and in patients with type 2 diabetes and dyslipidemia characterized by high triglyceride and low high-density lipoprotein cholesterol concentrations.
However, in the current era of intensive lipid-lowering therapies to reduce the risk of cardiovascular disease, there is still debate regarding the potential relationship between fibrates use and cancer. Concerns about a possible increase in cancer-related deaths arose initially due to fibrates’ contribution to the total mortality observed during the “in-trial” period of the World Health Organization (WHO) cooperative study [3], although subsequent extended follow-up showed a smaller difference in incidence of and death rates from cancer between treatment and control arms [4], [5]. On the other hand, a review of rodent carcinogenicity tests reported that lipid-lowering drugs, including fibrates, initiate or promote cancer in rats and mice [6]. However, in most of the reviewed studies the doses used were substantially higher than the recommended doses for humans and the employed bioassays were criticised for being inadequate to predict carcinogenicity in humans [7].
Given that the use of fibrates has steadily increased during the past decade [8], more knowledge is needed on the relationship between these medications and cancer. To address this issue, we conducted a systematic review and meta-analysis of randomized placebo-controlled trials published in the peer-reviewed literature.
Materials and Methods
Search Strategy
To identify the studies of interest, we systematically searched the following databases: (i) Medline, (ii) Scopus, and (iii) Science Citation Index Expanded, from the date of inception of each database to January 2012. Search terms included: “fibrate” or “fibric acid” or “fenofibrate” or “bezafibrate” or “ciprofibrate” or “clofibrate” or “gemfibrozil”. The search was limited to randomized controlled trials (RCTs), human subjects. The Cochrane Central Register of Controlled Trials was also reviewed. The title and abstract of studies identified in the computerized search were scanned to exclude any that were clearly irrelevant. The full text of the remaining articles was read to determine whether it contained information on the topic of interest. The reference lists of the articles were reviewed to identify citations to other studies of the same topic. No language restrictions were imposed.
Inclusion and Exclusion Criteria
The studies considered in this meta-analysis were RCTs that evaluated exposure to fibrates and cancer risk. They were considered eligible if they had evaluated a fibrate therapy compared with placebo, they had a minimum duration of two years, and reported data on the incidence of and/or deaths from cancer during the trial. We excluded trials that evaluated multi-interventional therapies where the effect of the fibrate could not be separated out.
We did not assess the methodological quality of the primary studies as quality assessment in meta-analysis is controversial and results can be highly misleading [9], [10]. Instead, we performed subgroup and sensitivity analyses according to study characteristics.
Data Extraction
Two reviewers (SB, GN) abstracted the data independently. The following information was collected from each study: (i) publication data: first author’s last name, year of publication and geographical location of the study; (ii) study design; (iii) number of participants; (iv) population characteristics; and (v) interventions’ parameters including type of drug, dose and duration. Study-level risk ratios and their 95% confidence intervals (CIs) were estimated by reconstructing contingency tables based on the number of patients randomly assigned and the number of patients who had experienced cancer events (intention-to-treat analysis). When no cancer events occurred in either or both arms, a continuity correction of 0.5 was added to each cell of the respective contingency table. Non-melanoma skin cancers were not included in the analysis because they were neither recorded nor routinely reported in the primary studies. Differences in data extraction were resolved by consensus, referring back to the original article.
Quantitative Data Synthesis
We used the inverse variance weighted approach to calculate summary effect-estimates. Outcome reporting bias was evaluated using the Begg-Mazumdar adjusted rank correlation test [11] and the Egger regression asymmetry test [12]. To evaluate whether the results of the studies were homogeneous, we used the Cochran’s Q test [13]. We also calculated the quantity I2 [14], [15] that describes the percentage variation across studies that is due to heterogeneity rather than chance. We regarded an I2 value less than 40% as indicative of “not important heterogeneity” and a value higher than 75% as indicative of “considerable heterogeneity” [16].
Subgroup analyses by fibrate type were also performed to investigate potentially different effects on risk. We, then, conducted a sensitivity analysis by restricting the meta-analysis: (i) to trials with a minimum duration of 5 years, (ii) to trials that enrolled at least 1,000 subjects, and (iii) to major trials that fulfilled both previous criteria. Last, we performed site-specific analyses to evaluate the association between fibrate use and type of cancer diagnosis (cancer subtypes: respiratory, breast, genitourinary, prostate, gastrointestinal, colorectal and melanoma). In those analyses, only RCTs reporting at least one site-specific new cancer diagnosis were included.
We also conducted a meta-regression analysis [17] to investigate the impact of certain study characteristics on the study estimates of relative risk. We first converted all risk ratios by logarithmic transformation to achieve more symmetrical distributions. The natural logarithm of the risk ratio was the dependent variable, and (i) the mean age of participants at enrollment, and (ii) the mean duration of follow-up, were entered as covariates. This analysis was an indirect way to deal with aspects such as the possibility of effect modification by age, and to examine for increasing or decreasing risks with increasing duration of drug use, a feature often associated with causal relationships. We applied a weighted regression model, so that the more precise studies have more influence in the analysis. The weight for each trial was equal to the inverse of the sum of the within-trial variance and the residual between-trial variance, which corresponds to a random effects meta-regression analysis [18]. Estimation of the residual between-trial variance was based on a restricted maximum likelihood method [19].
This work was performed in accordance with the PRISMA statement for the conduct of meta-analyses of intervention studies [20]. For all tests, a probability level lower than 0.05 was considered statistically significant. All statistical tests were two-sided. Stata 9 software was used for the statistical analyses (Stata Corp., College Station, Texas, USA).
Results
Search Results
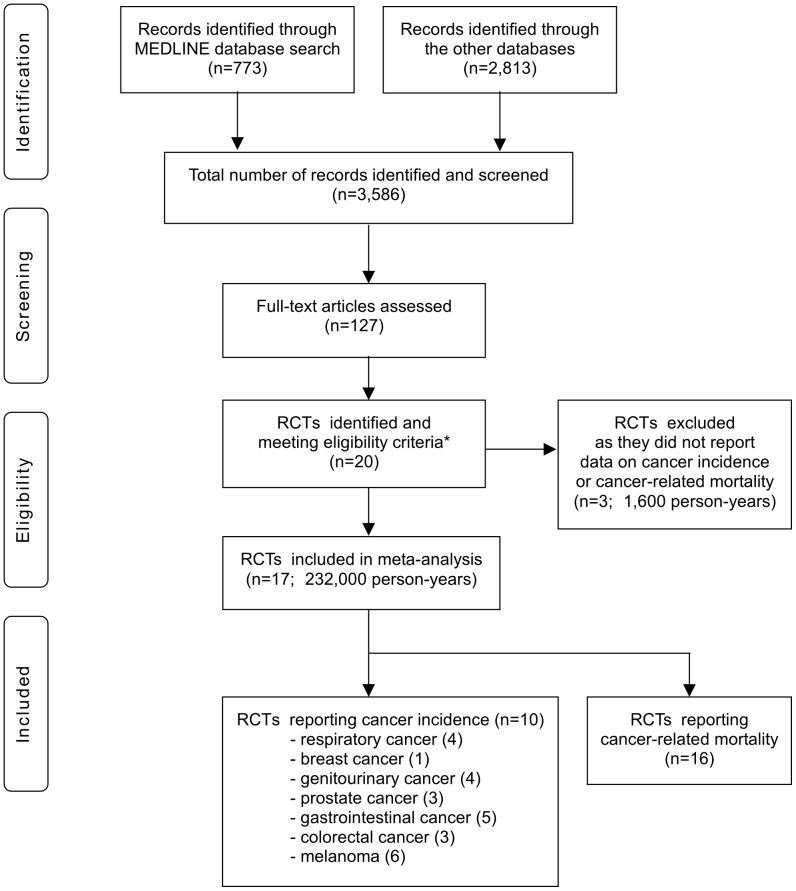
Our initial search yielded 3,586 literature citations (Figure 1). However, most abstracts were duplicates or did not specifically address the topic of our analysis and were excluded from full-text review. We retrieved 127 potentially relevant manuscripts. The full text was read and the reference lists were checked. We identified 20 studies of fibrates [3], [21]–[39], which conformed to our inclusion criteria. Seventeen of these [3], [21]–[36] evaluated adverse effects and reported data on the incidence of and/or deaths from cancer during the trial, and we were able to conduct post-hoc analyses to calculate risk ratios. For several studies, additional usable data were extracted from other publications [40]–[44]. All 17 studies were randomized placebo-controlled trials, and all but one [23] were double-blind.
Figure 1. Flow Diagram.
Footnote: * To be included in this meta-analysis, studies had to be (i) randomized trials of fibrates, (ii) placebo-controlled, and (iii) have a mean (or median) duration of patient follow-up of at least 2 years.
A total of 44,929 individuals participated in these trials; 21,627 in treatment groups and 23,302 in placebo groups. The participants had a mean age of 55 years at enrollment, and the average follow-up was 5.2 years. A total of 232,000 person-years were reached. Sixteen RCTs reported data on cancer deaths during the trial [3], [21]–[23], [25]–[36]. The overall cancer mortality was 1.82% (762 cancer deaths during the follow-up) corresponding to a rate of 0.36% per year. On the other hand, 10 RCTs reported data on new cancer diagnoses [3], [22], [24]–[26], [28]–[30], [32], [36]. The overall cancer incidence was 4.48% (1,594 cancer diagnoses) corresponding to a rate of 0.86% per year.
Bezafibrate had been evaluated in four trials [22], [24], [31], [35], clofibrate in six [3], [23], [25], [27], [33], [34], fenofibrate in three [21], [26], [28], and gemfibrozil in four trials [29], [30], [32], [36]. Tables 1 & 2 list the RCTs included in the meta-analysis together with the respective trial drug, the number and summary characteristics of patients, the duration of follow-up and the estimated risk ratios and their 95% CIs.
Table 1. Characteristics of studies included in the meta-analysis.
| Study | Location | Agent | Design | N | (active/placebo) | Mean age(yrs) | Follow-up (yrs) | Study population |
| ACCORD [21], 2010 | USA, Canada | Fenofibrate | r, db, pc | 5518 | (2765/2753) | 62.2 | 5.0 | Type 2 DM |
| BECAIT [22], 1996 | Sweden | Bezafibrate | r, db, pc | 92 | (47/45) | 42.0 | 5.0 | CAD |
| Begg Study [23], 1971 | Scotland | Clofibrate | r, pc | 155 | (76/79) | 56.0 | 3.5 | Peripheral arteriopathy |
| BIP [24], 2000 | Israel | Bezafibrate | r, db, pc | 3090 | (1548/1542) | 60.1 | 6.2 | CAD |
| CDP [25], 1975 | USA, Puerto Rico | Clofibrate | r, db, pc | 3892 | (1103/2789) | 52.0 | 6.2 | CAD |
| DAIS [26], 2001 | Canada, Finland,France, Sweden | Fenofibrate | r, db, pc | 418 | (207/211) | 56.8 | 3.3 | Type 2 DM |
| DIS [27], 1991 | Germany | Clofibricacid | r, db, pc | 761 | (379/382) | 46.0 | 5.0 | NIDDM |
| FIELD [28], 2005 | Australia,New Zealand, Finland | Fenofibrate | r, db, pc | 9795 | (4895/4900) | 62.2 | 5.0 | Type 2 DM |
| HHS [29], 1987 | Finland | Gemfibrozil | r, db, pc | 4081 | (2046/2035) | 47.3 | 5.0 | Dyslipidemia |
| HHS ancillary [30],1993 | Finland | Gemfibrozil | r, db, pc | 628 | (311/317) | 48.6 | 5.0 | Suspected CAD |
| LEADER [31], 2002 | United Kingdom | Bezafibrate | r, db, pc | 1568 | (783/785) | 68.2 | 4.6 | LEAD |
| LOCAT [32], 1997 | Finland | Gemfibrozil | r, db, pc | 395 | (197/198) | 59.2 | 2.5 | CAD |
| NEWCASTLE [33], 1971 | England | Clofibrate | r, db, pc | 497 | (244/253) | 52.5 | 3.6 | CAD |
| SCOTTISH [34], 1971 | Scotland | Clofibrate | r, db, pc | 717 | (350/367) | 52.1 | 3.4 | CAD |
| SENDCAP [35], 1998 | United Kingdom | Bezafibrate | r, db, pc | 164 | (81/83) | 50.9 | 3.0 | Type 2 DM |
| VA HIT [36], 1999 | USA | Gemfibrozil | r, db, pc | 2531 | (1264/1267) | 64.0 | 5.1 | CAD |
| WHO [3], 1978 | Scotland, Hungary,Czech Rep. | Clofibrate | r, db, pc | 10627 | (5331/5296) | 45.9 | 5.3 | High-cholesterol population |
Abbreviations: ACCORD, Action to Control Cardiovascular Risk in Diabetes; BECAIT, Bezafibrate Coronary Atherosclerosis Intervention Trial; BIP, Bezafibrate Infarction Prevention; CDP, Coronary Drug Project; DAIS, Diabetes Atherosclerosis Intervention Study; DIS, Diabetes Intervention Study; FIELD, Fenofibrate Intervention and Event Lowering in Diabetes; HHS, Helsinki Heart Study; LEADER, Lower Extremity Arterial Disease Event Reduction; LOCAT, Lopid Coronary Angiography Trial; SENDCAP, St. Mary’s, Ealing, Northwick Park Diabetes Cardiovascular Disease Prevention; VA HIT, Veterans Affairs High-Density Lipoprotein Cholesterol Intervention Trial; WHO, World Health Organization; r, randomized; db, double-blind; pc, placebo-controlled; DM, Diabetes Mellitus; CAD, Coronary Artery Disease; NIDDM, Non-Insulin-Dependent Diabetes Mellitus; LEAD, Lower Extremity Arterial Disease.
Table 2. Incidence of and/or deaths from cancer in the randomized placebo-controlled trials of fibrates.
| Study | Incident cancer, n (%*) | Cancer deaths, n (%*) | ||||||||||
| Fibrate | Placebo | RR | 95% CI | Fibrate | Placebo | RR | 95% CI | |||||
| ACCORD [21], 2010 | – | – | – | – | – | – | 57 | (2.06) | 58 | (2.11) | 0.98 | (0.68–1.40) |
| BECAIT [22], 1996 | 1 | (2.13) | 1 | (2.22) | 0.96 | (0.06–14.85) | 0 | (0.00) | 0 | (0.00) | 0.96 | (0.02–47.30) |
| Begg Study [23], 1971 | – | – | – | – | – | – | 0 | (0.00) | 0 | (0.00) | 1.04 | (0.02–51.71) |
| BIP [24], 2000 | 85 | (5.49) | 91 | (5.90) | 0.93 | (0.70–1.24) | – | – | – | – | – | – |
| CDP [25], 1975 | 32 | (2.90) | 79 | (2.83) | 1.02 | (0.68–1.54) | 10 | (0.91) | 24 | (0.86) | 1.05 | (0.51–2.20) |
| DAIS [26], 2001 | 5 | (2.42) | 7 | (3.32) | 0.73 | (0.23–2.26) | 0 | (0.00) | 3 | (1.42) | 0.15 | (0.01–2.80)** |
| DIS [27], 1991 | – | – | – | – | – | – | 2 | (0.53) | 3 | (0.79) | 0.67 | (0.11–4.00) |
| FIELD [28], 2005 | 393 | (8.03) | 373 | (7.61) | 1.05 | (0.92–1.21) | 168 | (3.43) | 148 | (3.02) | 1.14 | (0.91–1.41) |
| HHS [29], 1987 | 25 | (1.22) | 29 | (1.43) | 0.86 | (0.50–1.46) | 10 | (0.49) | 11 | (0.54) | 0.90 | (0.38–2.12) |
| HHS ancillary [30], 1993 | 5 | (1.61) | 4 | (1.26) | 1.27 | (0.35–4.70) | 0 | (0.00) | 2 | (0.63) | 0.20 | (0.01–4.23) |
| LEADER [31], 2002 | – | – | – | – | – | – | 47 | (6.00) | 47 | (5.99) | 1.00 | (0.68–1.48) |
| LOCAT [32], 1997 | 3 | (1.52) | 7 | (3.54) | 0.43 | (0.11–1.64) | 0 | (0.00) | 0 | (0.00) | 1.01 | (0.02–50.41) |
| NEWCASTLE [33], 1971 | – | – | – | – | – | – | 3 | (1.23) | 1 | (0.40) | 3.11 | (0.33–29.70) |
| SCOTTISH [34], 1971 | – | – | – | – | – | – | 3 | (0.86) | 5 | (1.36) | 0.63 | (0.15–2.61) |
| SENDCAP [35], 1998 | – | – | – | – | – | – | 0 | (0.00) | 0 | (0.00) | 1.02 | (0.02–51.02) |
| VA HIT [36], 1999 | 125 | (9.89) | 138 | (10.89) | 0.91 | (0.72–1.14) | 45 | (3.56) | 51 | (4.03) | 0.88 | (0.60–1.31) |
| WHO [3], 1978 | 106 | (1.99) | 85 | (1.60) | 1.24 | (0.93–1.64) | 40 | (0.75) | 24 | (0.45) | 1.66 | (1.00–2.74) |
Crude rates;
Reported in Saha et al. [43].
Abbreviations: ACCORD, Action to Control Cardiovascular Risk in Diabetes; BECAIT, Bezafibrate Coronary Atherosclerosis Intervention Trial; BIP, Bezafibrate Infarction Prevention; CDP, Coronary Drug Project; DAIS, Diabetes Atherosclerosis Intervention Study; DIS, Diabetes Intervention Study; FIELD, Fenofibrate Intervention and Event Lowering in Diabetes; HHS, Helsinki Heart Study; LEADER, Lower Extremity Arterial Disease Event Reduction; LOCAT, Lopid Coronary Angiography Trial; SENDCAP, St. Mary’s, Ealing, Northwick Park Diabetes Cardiovascular Disease Prevention; VA HIT, Veterans Affairs High-Density Lipoprotein Cholesterol Intervention Trial; WHO, World Health Organization; RR, relative risk (risk ratio); CI, confidence interval.
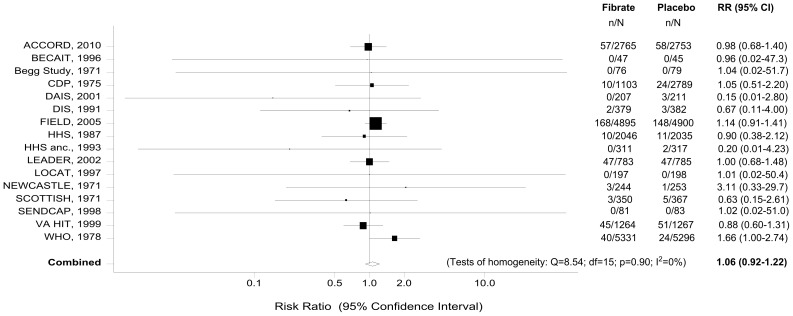
Meta-analysis of Fibrate Use and Cancer Mortality
Sixteen RCTs [3], [21]–[23], [25]–[36] reported data on cancer related-deaths. The meta-analysis of these trials showed no evidence of an association between fibrate therapy and cancer mortality (RR = 1.06, 95% CI: 0.92–1.22) (Table 3). Figure 2 graphs the risk ratios and the corresponding 95% CIs from the individual studies, and the pooled results. The Cochran’s Q test had a p-value of 0.90 and the corresponding I2 was 0%, which both indicate very small between-studies variability (Table 3). The p-values for the Begg’s and the Egger’s tests were p = 0.89 and p = 0.18, respectively, both suggesting that the assumption of no reporting bias is reasonable.
Table 3. Fibrate use and cancer risk: Meta-analysis and subgroup analysis.
| Pooled effect estimate | Tests of homogeneity | Tests for reporting bias | ||||||
| N | RR | (95% CI) | Q (d.f.) | p-value | I2 | Begg’s p | Egger’s p | |
| Cancer Deaths: | ||||||||
| All RCTs | 16 | 1.06 | (0.92–1.22) | 8.54 (15) | 0.90 | 0% | 0.89 | 0.18 |
| Bezafibrate | 3 | 1.00 | (0.68–1.48) | 0.00 (2) | 0.99 | 0% | 0.99 | 0.79 |
| Clofibrate | 6 | 1.31 | (0.90–1.92) | 2.88 (5) | 0.72 | 0% | 0.99 | 0.32 |
| Fenofibrate | 3 | 1.08 | (0.90–1.31) | 2.26 (2) | 0.32 | 12% | 0.30 | 0.077 |
| Gemfibrozil | 4 | 0.87 | (0.61–1.24) | 0.90 (3) | 0.83 | 0% | 0.31 | 0.43 |
| Duration ≥5 years | 9 | 1.08 | (0.93–1.26) | 5.85 (8) | 0.66 | 0% | 0.75 | 0.34 |
| Participants ≥1,000 | 7 | 1.08 | (0.94–1.24) | 4.55 (6) | 0.60 | 0% | 0.99 | 0.84 |
| Both previous criteria | 6 | 1.09 | (0.94–1.27) | 4.40 (5) | 0.49 | 0% | 0.99 | 0.89 |
| Cancer Incidence: | ||||||||
| All RCTs | 10 | 1.02 | (0.92–1.12) | 5.89 (9) | 0.75 | 0% | 0.72 | 0.28 |
| Bezafibrate | 2 | 0.93 | (0.70–1.24) | 0.00 (1) | 0.98 | 0% | 0.99 | – |
| Clofibrate | 2 | 1.16 | (0.92–1.47) | 0.57 (1) | 0.45 | 0% | 0.99 | – |
| Fenofibrate | 2 | 1.05 | (0.92–1.20) | 0.41 (1) | 0.52 | 0% | 0.99 | – |
| Gemfibrozil | 4 | 0.89 | (0.73–1.10) | 1.47 (3) | 0.69 | 0% | 0.73 | 0.64 |
| Duration ≥5 years | 8 | 1.02 | (0.93–1.13) | 3.95 (7) | 0.79 | 0% | 0.99 | 0.81 |
| Participants ≥1,000 | 6 | 1.02 | (0.93–1.13) | 3.84 (5) | 0.57 | 0% | 0.99 | 0.60 |
| Both previous criteria | 6 | 1.02 | (0.93–1.13) | 3.84 (5) | 0.57 | 0% | 0.99 | 0.60 |
| Respiratory Cancer | 4 | 0.99 | (0.71–1.37) | 1.36 (3) | 0.72 | 0% | 0.99 | 0.92 |
| Breast Cancer | 1 | 0.98 | (0.63–1.53) | – | – | – | – | – |
| Genitourinary Cancer | 4 | 1.11 | (0.89–1.38) | 2.05 (3) | 0.56 | 0% | 0.73 | 0.89 |
| Prostate Cancer | 3 | 1.25 | (0.96–1.63) | 1.24 (2) | 0.54 | 0% | 0.99 | 0.99 |
| Gastrointestinal Cancer | 5 | 0.91 | (0.73–1.14) | 5.29 (4) | 0.26 | 24% | 0.46 | 0.033 |
| Colorectal Cancer | 3 | 0.98 | (0.71–1.34) | 3.96 (2) | 0.14 | 49% | 0.99 | 0.43 |
| Melanoma | 6 | 0.54 | (0.22–1.31) | 5.50 (5) | 0.36 | 9% | 0.99 | 0.66 |
RR, risk ratio; CI, confidence interval; d.f., degrees of freedom.
Figure 2. Forest plot of the meta-analysis of fibrate use and cancer deaths.
Footnote: The risk ratios and their 95% confidence intervals are displayed on a logarithmic scale. The size of the data markers represents the relative weight of the trial according to size and occurrence of the outcome being measured.
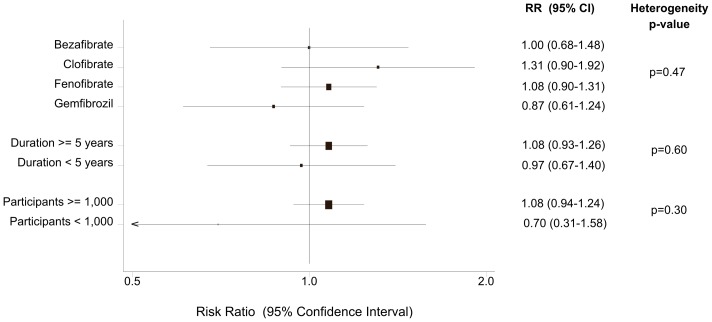
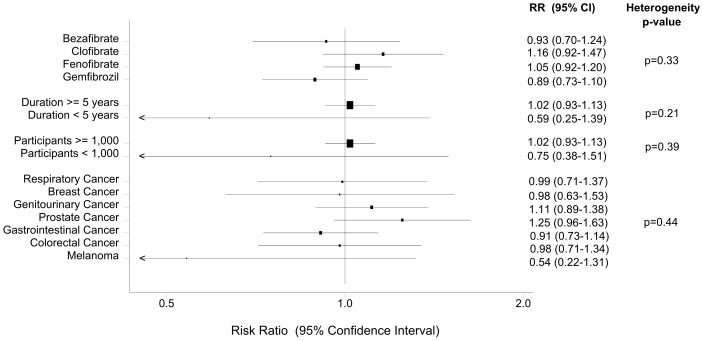
After stratifying the data into subgroups, according to the type of fibrate, we did not find any statistically significant association between bezafibrate, clofibrate, fenofibrate or gemfibrozil use and cancer mortality (Table 3, Figure 3).
Figure 3. Fibrate use and cancer deaths: Subgroup analyses.
When the analysis was restricted to studies with a minimum duration of 5 years (9 trials), we also found no evidence of an association (RR = 1.08, 95% CI: 0.93–1.26). Similarly, when only RCTs that enrolled at least 1,000 subjects contributed to the analysis (7 trials), the pooled effect estimate remained insignificant (RR = 1.08, 95% CI: 0.94–1.24) (Table 3, Figure 3). Finally, we performed a meta-analysis of six major trials [3], [21], [25], [28], [29], [36] that fulfilled both previous criteria. Once again, there was no statistically significant association between fibrate use and cancer mortality (RR = 1.09, 95% CI: 0.94–1.27). In this restricted analysis, there was no evidence of reporting bias (Begg’s p = 0.99, Egger’s p = 0.89) or heterogeneity (Cochran’s Q test: p = 0.49, I2 = 0%) (Table 3).
Meta-regression analysis, using the mean age of participants and the mean duration of follow-up as covariates, did not reveal any significant association (Table 4).
Table 4. Meta-regression’s results.
| Univariable analysis | |||
| Ratio of RR | (95% CI) | p-value | |
| Cancer Deaths: | |||
| - Mean age of participants (per 10-year increase) | 0.89 | (0.71–1.12) | 0.33 |
| - Mean duration of follow-up (per 1-year increase) | 1.19 | (0.81–1.74) | 0.37 |
| Cancer Incidence: | |||
| - Mean age of participants (per 10-year increase) | 0.92 | (0.79–1.08) | 0.33 |
| - Mean duration of follow-up (per 1-year increase) | 1.03 | (0.85–1.25) | 0.73 |
RR, risk ratio; CI, confidence interval.
Results are exponentiated regression coefficients and their 95% CIs, which show the proportional change in risk ratio for every one scale increase.
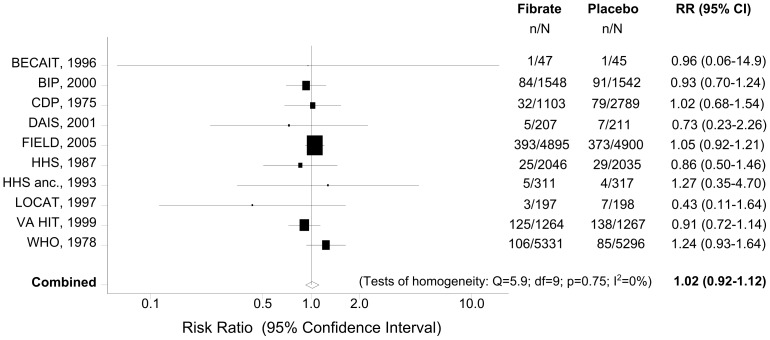
Meta-analysis of Fibrate Use and Cancer Incidence
Ten RCTs [3], [22], [24]–[26], [28]–[30], [32], [36] reported data on new cancer diagnoses. The quantitative synthesis of these studies provided no evidence of an association between fibrate use and cancer incidence. The calculated effect estimate indicated a neutral effect of fibrates (RR = 1.02, 95% CI: 0.92–1.12) (Table 3). Figure 4 presents a forest plot of the risk ratios and their 95% CIs from the 10 primary studies, and the pooled estimates. Reporting bias (Begg’s p = 0.72; Egger’s p = 0.28) or significant heterogeneity (Cochran’s p = 0.75; I2 = 0%) were not detected in this analysis (Table 3).
Figure 4. Forest plot of the meta-analysis of fibrate use and cancer incidence.
Footnote: The risk ratios and their 95% confidence intervals are displayed on a logarithmic scale. The size of the data markers represents the relative weight of the trial according to size and occurrence of the outcome being measured.
The subgroup analysis, according to the type of fibrate, did not demonstrate any significant association between bezafibrate, clofibrate, fenofibrate or gemfibrozil use and cancer incidence (Table 3, Figure 5).
Figure 5. Fibrate use and cancer incidence: Subgroup analyses.
When we restricted the analysis to studies with a minimum duration of 5 years (8 trials), we also found no evidence of association (RR = 1.02, 95% CI: 0.93–1.13). Similarly, when only RCTs with a minimum duration of 5 years and more than 1,000 participants (6 trials) [3], [24], [25], [28], [29], [36] contributed to the analysis, the summary effect estimate suggested a neutral effect of fibrates on cancer incidence (RR = 1.02, 95% CI: 0.93–1.13; Begg’s p = 0.99; Egger’s p = 0.60; Cochran’s p = 0.57; I2 = 0%) (Table 3, Figure 5).
No statistically significant differences were observed between patients receiving fibrate vs placebo for any of the prespecified cancer subtypes (Table 3, Figure 5). Heterogeneity or reporting bias were not observed in any of these site-specific analyses (p>0.14 for all) with the exception of gastrointestinal cancer (Egger’s p = 0.033; Table 3).
Last, in the meta-regression analysis, the results did not show any impact of either the mean age of participants or the duration of follow-up on the study estimates of relative risk (Table 4).
In a re-analysis, excluding all trials reporting zero cancer events in either or both arms, no statistically or clinically meaningful differences occurred vs the initial analyses (both for cancer mortality and cancer incidence).
Discussion
Fibrates comprise a class of lipid-lowering agents that significantly reduce cardiovascular events through a substantial reduction in serum levels of triglycerides and modest effects on levels of low-density and high-density lipoprotein cholesterol [45], [46]. The concerns that lipid-lowering drugs (including fibrates) might increase the risk of cancer have been present for three decades [6], [47]–[51]. However, while for the 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors (statins) several meta-analyses of existing data have convincingly demonstrated that they do not cause any substantial change in overall [52], [53] or site-specific cancer risk [54]–[59], this is the first meta-analysis that focuses specifically on the relationship between fibrates and cancer.
Our study encompassed 17 randomized placebo-controlled trials involving 45,000 individuals with a broad range of baseline characteristics, and accrued a total experience of 232,000 person-years. The analysis did not provide any evidence that the use of fibrates significantly affects the incidence of cancer or cancer-related death. When the analysis was restricted to major RCTs, the results remained practically unchanged. Similarly, when bezafibrate, clofibrate, fenofibrate and gemfibrozil were evaluated alone, we found no impact on cancer outcomes. No significant results were also noted for cancers of the respiratory tract, breast, colon, gastrointestinal tract, prostate, genitourinary tract, or skin (melanoma) when fibrates were used.
The neutral results of the present study are in line with several well-designed observational studies that have analysed overall cancer [60], [61] and site-specific cancers [62]–[64] in fibrate users, and exclude the strong protective effect of fibrates found in the PRIME study [65]. This large observational cohort, suggesting that cancer mortality was significantly lower in fibrate users as compared with untreated dyslipidemic subjects (hazard ratio: 0.52, 95% CI: 0.28–0.97), may have been affected by uncontrolled (unmeasured) or residual confounding or other biases, problems known to plague even well-designed observational studies because they lack the experimental random allocation of the intervention necessary to test exposure-outcome hypotheses [66].
Our study has several merits. We have conducted an extensive literature search to retrieve all relevant eligible trials. Moreover, the absence of significant between-study heterogeneity, the small likelihood of important reporting bias, as well as the stability of results in subgroup and sensitivity analyses, reinforce our confidence in the validity of the conclusion that fibrate use has a neutral effect on cancer outcomes. The strengths of this quantitative synthesis should be, however, weighed against some limitations. First, the trials included in this meta-analysis were not designed to specifically analyze the relationship between fibrates and cancer risk. They have assessed cancer outcomes as secondary (safety) endpoints. Thus, problems in cancer detection and reporting may exist. However, the definition used and the surveillance intensity were consistent within each study for the fibrate and placebo groups, so the relative impact should still be accurate. Second, our search was restricted to published studies and we did not seek for unpublished/original data. However, we did not impose any exclusion criteria with regard to language, place of publication or study quality. Last, a main issue remaining beyond our control is cancer latency. As the exposure and follow-up times only lasted for nearly five years, estimates of cancer risk resulting from longer exposure to fibrates are not possible. Thus, our results should be interpreted with caution.
In conclusion, the synthesis of existing data from randomized placebo-controlled trials supports a neutral effect of fibrates on cancer risk in the short term. We found no site-specific type of cancer whose risk was affected by fibrates, or subtype of fibrates that influenced the risk of cancer. However, given the steadily increasing use of fibrates during the past decade [8], and the indications for long-term and perhaps lifelong use, it is important to continue monitoring their long-term safety profiles.
Acknowledgments
Data Access and Responsibility
Stefanos Bonovas had full access to all the data in the study, takes responsibility for the integrity of the data and the accuracy of the data analysis and acts as guarantor of the paper.
Funding Statement
These authors have no support or funding to report.
References
- 1. Staels B, Fruchart JC (2005) Therapeutic roles of peroxisome proliferator-activated receptor agonists. Diabetes 54: 2460–2470. [DOI] [PubMed] [Google Scholar]
- 2. Després JP, Lemieux I, Robins SJ (2004) Role of fibric acid derivatives in the management of risk factors for coronary heart disease. Drugs 64: 2177–2198. [DOI] [PubMed] [Google Scholar]
- 3. WHO Cooperative Trial Committee of Principal Investigators (1978) A cooperative trial in the primary prevention of ischaemic heart disease using clofibrate. Br Heart J 40: 1069–1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. WHO Cooperative Trial Committee of Principal Investigators (1985) WHO cooperative trial on primary prevention of ischaemic heart disease using clofibrate to lower serum cholesterol: mortality follow-up. Lancet 2: 379–385. [PubMed] [Google Scholar]
- 5. Heady JA, Morris JN, Oliver MF (1992) WHO clofibrate/cholesterol trial: clarifications. Lancet 340: 1405–1406. [DOI] [PubMed] [Google Scholar]
- 6. Newman TB, Hulley SB (1996) Carcinogenicity of lipid-lowering drugs. JAMA 275: 55–60. [PubMed] [Google Scholar]
- 7. Dalen JE, Dalton WS (1996) Does lowering cholesterol cause cancer? JAMA 275: 67–69. [PubMed] [Google Scholar]
- 8. Jackevicius CA, Tu JV, Ross JS, Ko DT, Carreon D, et al. (2011) Use of fibrates in the United States and Canada. JAMA 305: 1217–1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Greenland S (1994) Invited commentary: a critical look at some popular meta-analytic methods. Am J Epidemiol 140: 290–296. [DOI] [PubMed] [Google Scholar]
- 10. Jüni P, Witschi A, Bloch R, Egger M (1999) The hazards of scoring the quality of clinical trials for meta-analysis. JAMA 282: 1054–1060. [DOI] [PubMed] [Google Scholar]
- 11. Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50: 1088–1101. [PubMed] [Google Scholar]
- 12. Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315: 629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cochran WG (1954) The combination of estimates from different experiments. Biometrics 8: 101–129. [Google Scholar]
- 14. Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21: 1539–1558. [DOI] [PubMed] [Google Scholar]
- 15. Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327: 557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Higgins JPT, Green S (2008) Cochrane handbook for systematic reviews of interventions. The Cochrane Collaboration.
- 17. Sharp S (1998) Meta-analysis regression. Stata Tech Bull 42: 16–24. [Google Scholar]
- 18. Berkey CS, Hoaglin DC, Mosteller F, Colditz GA (1995) A random-effects regression model for meta-analysis. Stat Med 14: 395–411. [DOI] [PubMed] [Google Scholar]
- 19. Thompson SG, Sharp SJ (1999) Explaining heterogeneity in meta-analysis: a comparison of methods. Stat Med 18: 2693–2708. [DOI] [PubMed] [Google Scholar]
- 20.Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151: 264–269, W64. [DOI] [PubMed]
- 21. Ginsberg HN, Elam MB, Lovato LC, Crouse JR 3rd, Leiter LA (2010) Effects of combination lipid therapy in type 2 diabetes mellitus. N Engl J Med 362: 1563–1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ericsson CG, Hamsten A, Nilsson J, Grip L, Svane B, et al. (1996) Angiographic assessment of effects of bezafibrate on progression of coronary artery disease in young male postinfarction patients. Lancet 347: 849–853. [DOI] [PubMed] [Google Scholar]
- 23. Begg TB, Rifkind BM (1971) Evaluation of clofibrate therapy in peripheral arteriopathy. Minerva Med 62: 3469–3475. [PubMed] [Google Scholar]
- 24. The BIP Study Group (2000) Secondary prevention by raising HDL cholesterol and reducing triglycerides in patients with coronary artery disease: the Bezafibrate Infarction Prevention (BIP) study. Circulation 102: 21–27. [DOI] [PubMed] [Google Scholar]
- 25. The Coronary Drug Project Research Group (1975) Clofibrate and niacin in coronary heart disease. JAMA 231: 360–381. [PubMed] [Google Scholar]
- 26. Diabetes Atherosclerosis Intervention Study Investigators (2001) Effect of fenofibrate on progression of coronary-artery disease in type 2 diabetes: the Diabetes Atherosclerosis Intervention Study, a randomised study. Lancet 357: 905–910. [PubMed] [Google Scholar]
- 27. Hanefeld M, Fischer S, Schmechel H, Rothe G, Schulze J, et al. (1991) Diabetes Intervention Study. Multi-intervention trial in newly diagnosed NIDDM. Diabetes Care 14: 308–317. [DOI] [PubMed] [Google Scholar]
- 28. Keech A, Simes RJ, Barter P, Best J, Scott R, et al. (2005) Effects of long-term fenofibrate therapy on cardiovascular events in 9795 people with type 2 diabetes mellitus (the FIELD study): randomised controlled trial. Lancet 366: 1849–1861. [DOI] [PubMed] [Google Scholar]
- 29. Huttunen JK, Heinonen OP, Manninen V, Koskinen P, Hakulinen T, et al. (1994) The Helsinki Heart Study: an 8.5-year safety and mortality follow-up. J Intern Med 235: 31–39. [DOI] [PubMed] [Google Scholar]
- 30. Frick MH, Heinonen OP, Huttunen JK, Koskinen P, Mänttäri M, et al. (1993) Efficacy of gemfibrozil in dyslipidaemic subjects with suspected heart disease. An ancillary study in the Helsinki Heart Study frame population. Ann Med 25: 41–45. [DOI] [PubMed] [Google Scholar]
- 31. Meade T, Zuhrie R, Cook C, Cooper J (2002) Bezafibrate in men with lower extremity arterial disease: randomised controlled trial. BMJ 325: 1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Frick MH, Syvänne M, Nieminen MS, Kauma H, Majahalme S, et al. (1997) Prevention of the angiographic progression of coronary and vein-graft atherosclerosis by gemfibrozil after coronary bypass surgery in men with low levels of HDL cholesterol. Lopid Coronary Angiography Trial (LOCAT) Study Group. Circulation 96: 2137–2143. [DOI] [PubMed] [Google Scholar]
- 33. Group of physicians of the Newcastle upon Tyne region (1971) Trial of clofibrate in the treatment of ischaemic heart disease. Five-year study. Br Med J 4: 767–775. [PMC free article] [PubMed] [Google Scholar]
- 34. Research Committee of the Scottish Society of Physicians (1971) Ischaemic heart disease: a secondary prevention trial using clofibrate. Br Med J 4: 775–784. [PMC free article] [PubMed] [Google Scholar]
- 35. Elkeles RS, Diamond JR, Poulter C, Dhanjil S, Nicolaides AN, et al. (1998) Cardiovascular outcomes in type 2 diabetes. A double-blind placebo-controlled study of bezafibrate: the St. Mary’s, Ealing, Northwick Park Diabetes Cardiovascular Disease Prevention (SENDCAP) Study. Diabetes Care 21: 641–648. [DOI] [PubMed] [Google Scholar]
- 36. Rubins HB, Robins SJ, Collins D, Fye CL, Anderson JW, et al. (1999) Gemfibrozil for the secondary prevention of coronary heart disease in men with low levels of high-density lipoprotein cholesterol. N Engl J Med 341: 410–418. [DOI] [PubMed] [Google Scholar]
- 37. Acheson J, Hutchinson EC (1972) Controlled trial of clofibrate in cerebral vascular disease. Atherosclerosis 15: 177–183. [DOI] [PubMed] [Google Scholar]
- 38. Cullen JF, Town SM, Campbell CJ (1972) Double-blind trial of Atromid-S in exudative diabetic retinopathy. Trans Ophthalmol Soc UK 94: 554–562. [PubMed] [Google Scholar]
- 39. The Veterans Administration Cooperative Study Group (1973) The treatment of cerebrovascular disease with clofibrate. Stroke 4: 684–693. [DOI] [PubMed] [Google Scholar]
- 40. The Coronary Drug Project Research Group (1978) Estrogens and cancer. JAMA 239: 2758–2759.349183 [Google Scholar]
- 41. Dewar HA (1972) Trial of clofibrate. Br Med J 2: 228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Freeman SR, Drake AL, Heilig LF, Graber M, McNealy K, et al. (2006) Statins, fibrates, and melanoma risk: a systematic review and meta-analysis. J Natl Cancer Inst 98: 1538–1546. [DOI] [PubMed] [Google Scholar]
- 43. Saha SA, Arora RR (2010) Fibrates in the prevention of cardiovascular disease in patients with type 2 diabetes mellitus: a pooled meta-analysis of randomized placebo-controlled clinical trials. Int J Cardiol 141: 157–166. [DOI] [PubMed] [Google Scholar]
- 44. Tenenbaum A, Boyko V, Fisman EZ, Goldenberg I, Adler Y, et al. (2008) Does the lipid-lowering peroxisome proliferator-activated receptors ligand bezafibrate prevent colon cancer in patients with coronary artery disease? Cardiovasc Diabetol 7: 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Abourbih S, Filion KB, Joseph L, Schiffrin EL, Rinfret S, et al. (2009) Effect of fibrates on lipid profiles and cardiovascular outcomes: a systematic review. Am J Med 122: 962.e1–8. [DOI] [PubMed] [Google Scholar]
- 46. Jun M, Foote C, Lv J, Neal B, Patel A, et al. (2010) Effects of fibrates on cardiovascular outcomes: a systematic review and meta-analysis. Lancet 375: 1875–1884. [DOI] [PubMed] [Google Scholar]
- 47. Muldoon MF, Manuck SB, Matthews KA (1990) Lowering cholesterol concentrations and mortality: a quantitative review of primary prevention trials. BMJ 301: 309–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Oliver MF (1991) Might treatment of hypercholesterolaemia increase non-cardiac mortality? Lancet 337: 1529–1531. [DOI] [PubMed] [Google Scholar]
- 49. Hulley SB, Walsh JM, Newman TB (1992) Health policy on blood cholesterol. Time to change directions. Circulation 86: 1026–1029. [DOI] [PubMed] [Google Scholar]
- 50. Davey Smith G, Pekkanen J (1992) Should there be a moratorium on the use of cholesterol lowering drugs? BMJ 304: 431–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Pedersen T (2009) Lipid-lowering drugs and risk for cancer. Curr Atheroscler Rep 11: 350–357. [DOI] [PubMed] [Google Scholar]
- 52. Bonovas S, Filioussi K, Tsavaris N, Sitaras NM (2006) Statins and cancer risk: a literature-based meta-analysis and meta-regression analysis of 35 randomized controlled trials. J Clin Oncol 24: 4808–4817. [DOI] [PubMed] [Google Scholar]
- 53. Emberson JR, Kearney PM, Blackwell L, Newman C, Reith C, et al. (2012) Lack of effect of lowering LDL cholesterol on cancer: meta-analysis of individual data from 175,000 people in 27 randomised trials of statin therapy. PLoS One 7: e29849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Bonovas S, Filioussi K, Tsavaris N, Sitaras NM (2005) Use of statins and breast cancer: a meta-analysis of seven randomized clinical trials and nine observational studies. J Clin Oncol 23: 8606–8612. [DOI] [PubMed] [Google Scholar]
- 55. Bonovas S, Filioussi K, Flordellis CS, Sitaras NM (2007) Statins and the risk of colorectal cancer: a meta-analysis of 18 studies involving more than 1.5 million subjects. J Clin Oncol 25: 3462–3468. [DOI] [PubMed] [Google Scholar]
- 56. Bonovas S, Nikolopoulos G, Filioussi K, Peponi E, Bagos P, et al. (2010) Can statin therapy reduce the risk of melanoma? A meta-analysis of randomized controlled trials. Eur J Epidemiol 25: 29–35. [DOI] [PubMed] [Google Scholar]
- 57. Bonovas S, Filioussi K, Sitaras NM (2008) Statins are not associated with a reduced risk of pancreatic cancer at the population level, when taken at low doses for managing hypercholesterolemia: evidence from a meta-analysis of 12 studies. Am J Gastroenterol 103: 2646–2651. [DOI] [PubMed] [Google Scholar]
- 58. Bonovas S, Filioussi K, Sitaras NM (2008) Statin use and the risk of prostate cancer: a meta-analysis of 6 randomized clinical trials and 13 observational studies. Int J Cancer 123: 899–904. [DOI] [PubMed] [Google Scholar]
- 59. Bonovas S, Filioussi K, Tsantes A, Sitaras NM (2007) Use of statins and risk of haematological malignancies: a meta-analysis of six randomized clinical trials and eight observational studies. Br J Clin Pharmacol 64: 255–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Olsen J, Johansen C, Sørensen H, McLaughlin J, Mellemkjaer L, et al. (1999) Lipid-lowering medication and risk of cancer. J Clin Epidemiol 52: 167–169. [DOI] [PubMed] [Google Scholar]
- 61. Blais L, Desgagné A, LeLorier J (2000) 3-Hydroxy-3-methylglutaryl coenzyme A reductase inhibitors and the risk of cancer: a nested case-control study. Arch Intern Med 160: 2363–2368. [DOI] [PubMed] [Google Scholar]
- 62. Murtola TJ, Tammela TL, Lahtela J, Auvinen A (2007) Cholesterol-lowering drugs and prostate cancer risk: a population-based case-control study. Cancer Epidemiol Biomarkers Prev 16: 2226–2232. [DOI] [PubMed] [Google Scholar]
- 63. Fortuny J, de Sanjosé S, Becker N, Maynadié M, Cocco PL, et al. (2006) Statin use and risk of lymphoid neoplasms: results from the European Case-Control Study EPILYMPH. Cancer Epidemiol Biomarkers Prev 15: 921–925. [DOI] [PubMed] [Google Scholar]
- 64. Poynter JN, Gruber SB, Higgins PD, Almog R, Bonner JD, et al. (2005) Statins and the risk of colorectal cancer. N Engl J Med 352: 2184–2192. [DOI] [PubMed] [Google Scholar]
- 65. Gardette V, Bongard V, Dallongeville J, Arveiler D, Bingham A, et al. (2009) Ten-year all-cause mortality in presumably healthy subjects on lipid-lowering drugs (from the Prospective Epidemiological Study of Myocardial Infarction [PRIME] prospective cohort). Am J Cardiol 103: 381–386. [DOI] [PubMed] [Google Scholar]
- 66. Davey Smith G, Ebrahim S (2002) Data dredging, bias, or confounding. BMJ 325: 1437–1438. [DOI] [PMC free article] [PubMed] [Google Scholar]