Abstract
Low BMD increases fracture risk; how changes in BMD influence fracture risk in older men is uncertain.
BMD was assessed at 2–3 time points over 4.5 years using DXA for 4,470 men aged ≥65 years in the MrOS study. Change in femoral neck BMD was estimated using mixed effects linear regression models. BMD change was categorized as “accelerated” (≤−0.034 g/cm2), “expected” (between 0 and −0.034 g/cm2), or “maintained” (≥0 g/cm2). Fractures were adjudicated by central medical record review. Multivariate proportional hazards models estimated the risk of hip; non-spine non-hip; and non-spine fracture over 4.5 years after the final BMD measure, during which time 371 (8.3%) men experienced at least one non-spine fracture, including 78 (1.7%) hip fractures. Men with accelerated femoral neck BMD loss had an increased risk of non-spine (HR: 2.0, 95% CI: 1.4, 2.8); non-spine non-hip (HR: 1.6, 95% CI: 1.1, 2.3); and hip fracture (HR: 6.3, 95% CI: 2.7, 14.8) compared to men who maintained BMD over time. No difference in risk was seen for men with expected loss. Adjustment for the initial BMD measure did not alter the results. Adjustment for the final BMD measure attenuated the change in BMD/non-spine fracture and the change in BMD/non-spine non-hip relationships such that they were no longer significant, while the change in BMD-hip fracture relationship was attenuated (HR: 2.6, 95% CI: 1.1, 6.4). Total hip BMD change produced similar results.
Accelerated decrease in BMD is a strong, independent risk factor for hip and other non-spine fractures in men.
Introduction
In both men and women, bone mineral density (BMD) declines with age,(1–9) and low BMD is an established risk factor for fractures.(10,11) In women, a faster rate of BMD loss has been associated with an increased fracture risk, independent of baseline BMD, in some,(12–17) but not all studies(18). Reports of the association between change in BMD and fracture risk in men have been limited.(19) The single previous report examined change in BMD and risk of fracture concurrently, and the study relied on self-reported fracture outcomes. Since fractures may lead to subsequent inactivity that might, in turn, lead to bone loss, it is important to assess fracture risk after the assessment of change in BMD in order to identify the effects of bone loss on fracture and to exclude the effect of fracture on the subsequent loss of bone. Previous reports have demonstrated that loss of bone density accelerates with increasing age in older men(9,20–23) but it is not known whether such accelerated loss is associated with increased fracture risk subsequent to the BMD change period.
The goal of these analyses was to test the hypothesis that men with the greatest amount of BMD loss had the highest risk of subsequent hip; non-spine; and non-spine non-hip fractures compared to men who maintained BMD over time. We tested this hypothesis using data from the Osteoporotic Fractures in Men (MrOS) Study.
Methods
The MrOS Study
The MrOS study enrolled 5,994 men at the baseline visit between March 2000 and April 2002. Men were recruited from six clinical centers (Birmingham, AL; Minneapolis, MN; Palo Alto, CA; Monongahela Valley near Pittsburgh, PA; Portland, OR; and San Diego, CA) as described previously.(24,25) To be eligible for the study, men must have been aged 65 years or older, not have had bilateral hip replacements and able to walk without assistance. For these analyses, we used data from two follow-up visits: the “sleep visit” (December 2003–March 2005), an ancillary study designed to understand the consequences of sleep disorders in older men in a sub-cohort of participants; and “Visit 2” (March 2005–May 2006), a follow-up visit for all surviving baseline participants.
Assessment of BMD
At all study visits, participants who attended the clinic visit had hip dual x-ray absorptiometry (DXA) scans completed on Hologic 4500 scanners (Hologic, Waltham, 2MA, USA) as previously described.(20) Briefly, centralized quality control procedures, certification of DXA operators, and standardized procedures for scanning were used to ensure reproducibility of DXA measurements. Each clinic scanned a spine and hip phantom throughout the study to monitor longitudinal changes in measures of BMD, and correction factors were applied to participant data as appropriate. To adjust for inter-clinic differences, statistical models include indicator variables for clinical center. The precision of DXA scans of the spine and hip is 1–2% in clinical settings(26); the coefficient of variation of the MrOS DXA scanners estimated using a central phantom ranged from 0.3% to 0.7% for the total hip (data not shown.) The participant’s right hip was scanned unless there was a fracture, implant, hardware, or other problem preventing the right hip from being scanned; in those instances, the left hip was scanned. A participant had the same hip scanned at all visits unless he had to switch sides for one of these reasons. If, during the study, a different hip side or scan mode was used, scans at later visits were matched to the first scan of the new hip side or scan mode; scans using the previous side were then set to missing. This occurred for 49 participants during follow-up (sleep visit and visit 2). In addition, 5 participants had both hips become ineligible for scanning during follow-up (that is, both hips over time eventually had fracture, implant, hardware, or other problems that precluded scanning.) T-scores were calculated using young white male normative values from Looker.(27)
Fracture ascertainment
Study participants were contacted via mailed questionnaire every 4 months after Visit 1 and were asked to report recent fractures. When a participant did not return a mailed questionnaire in a timely fashion, clinic staff contacted the participant’s next of kin. Clinic staff was usually notified of a participant’s death through these contacts for missing questionnaires. Response amongst survivors to the mailed questionnaires exceeded 99%. Fractures were adjudicated by centralized physician review of radiology reports. Three fracture outcomes were analyzed: 1) hip 2) non-spine and 3) non-spine, non-hip. We included all three groups of fractures because each provides separate information: hip fractures are most important in terms of disability; all non-spine fractures are important as they would be considered as a single group in clinical settings; and non-spine non-hip fractures to understand if the associations remain with non-spine fractures once hip fractures are excluded. All fractures, regardless of the trauma that resulted in the fracture, were included in our analyses, since previous work suggests that event traumatic fractures are associated with lower BMD.(28)
Other measures
At all visits, weight was measured on a balance beam or digital scale, height was measured using wall-mounted stadiometers. BMI was calculated as weight (kg)/height2 (m2). Participants self-reported a physician diagnosis of diabetes, stroke, hyper- or hypothyroidism, Parkinson’s disease, heart attack, congestive heart failure, chronic obstructive pulmonary disease, cancer, hypertension, arthritis (osteoarthritis or rheumatoid), and angina pectoris. Participants were considered to have 1 or more medical conditions if they reported at least one condition from the list above. Activity level was determined by the Physical Activity Scale for the Elderly (PASE).(29) Race, alcohol use, smoking status, self-rated health (excellent/good vs. fair/poor/very poor), and history of fracture before the baseline visit were by self-report. Men also self-rated health at Visit 2. Change in self-rated health between visits was analyzed as three categories: increased (one level or greater improvement since baseline), stable (same level as reported at baseline), or decreased (one level or worse decline since baseline). Men also reported limitations in three instrumental activities of daily living (meal preparation, shopping, and housework) and in two physical tasks (walking 2–3 blocks and climbing 10 stairs); those who reported any difficulty with any task were considered to have a limitation.(30) Participants completed a battery of physical performance tests including walking speed over a 6 m course; the average of two trials was used (m/s). Average grip strength (kg) from two tests of each hand was assessed using Jamar handheld dynamometers. Frailty was defined using modified CHS criteria as previously described.(31,32)
Analysis sample
For these analyses, men must have had provided BMD data from at least the baseline visit and visit 2, as we were interested in risk of fracture after visit 2. BMD data from the sleep visit (attended between baseline and visit 2) was also included in the mixed effects regression models when available (see statistical methods, below), as this data improved the estimates of rate of change.
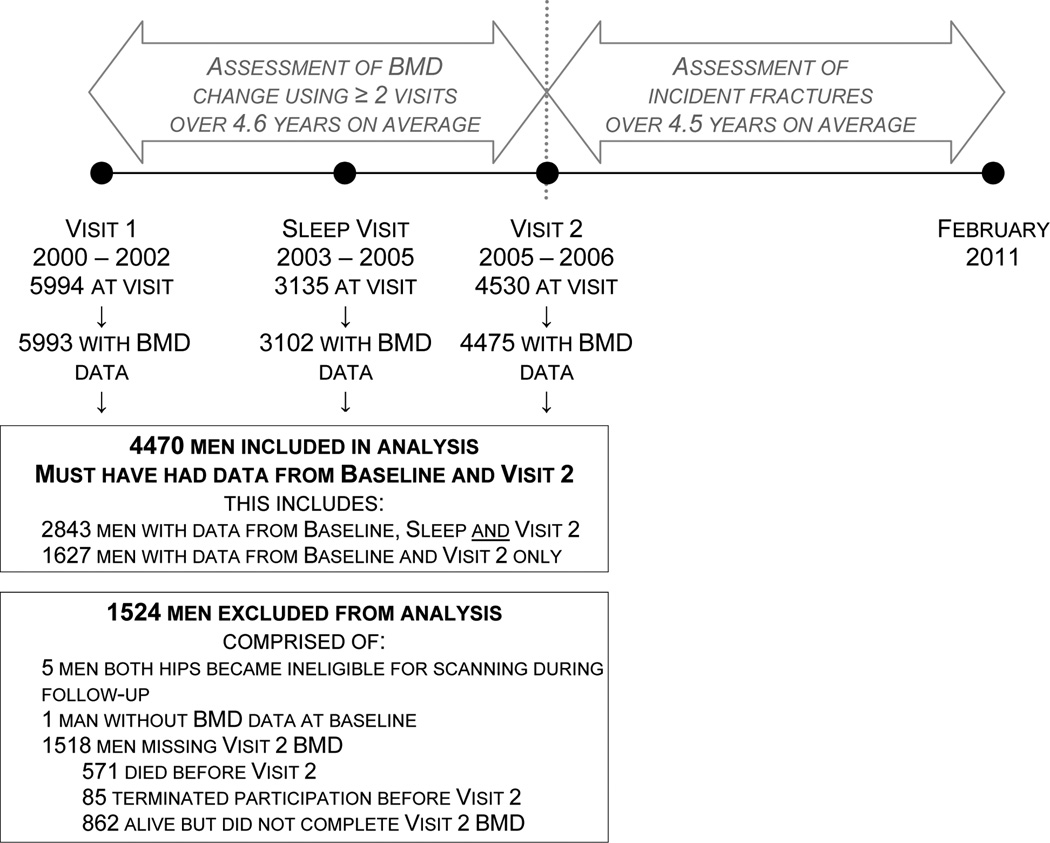
Of the 5994 men at baseline, we included 4470 men (74.6%) with DXA data for at least Baseline and Visit 2 (Figure 1). Of these, 2843 (63.6%) had BMD data for all three visits (Baseline, Sleep Visit and Visit 2) and 1627 (36.4%) had data at Baseline and Visit 2 only. Of the 1524 men not included in our analysis, 5 (0.3%) did not have the same hip scanned at Baseline and the follow-up visit(s), 1 (0.1%) did not have any BMD measurements at any visit; and 1518 men did not have Visit 2 BMD data. Of these, 571 (37.6%) had died before Visit 2; 85 (5.6%%) had terminated participation before Visit 2; 109 (7.2%) were living but did not attend Visit 2; and 753 (49.6%) provided some data at Visit 2 but did not have a DXA scan. At baseline, men who were excluded from the analyses were older, weighed less and had lower BMD at the total hip and femoral neck than men who were included in the analyses (p<.001). Average time between the baseline and visit 2 was 4.57 ± 0.35 yr, and average time between the baseline and sleep visit scans was 3.39 ± 0.48 (SD) yr.
Figure 1.
Participants included in analysis
Statistical analysis
The first stage of the analysis was to determine rate of change of BMD; to categorize this rate of change, and to describe characteristics of participants by category of change. The second stage of the analyses was to relate this BMD change to risk of fracture. These steps are described below.
Stage 1: Mixed effects models for determination of BMD change and categories of change
The first step in the analyses was to determine rate of change in BMD. As previously described,(20) change in total hip and femoral neck BMD were determined for all participants with at least baseline and Visit 2 repeat DXA assessments using random effects regression models (PROC MIXED procedure in SAS Version 9.2, SAS Institute, Cary, N.C., USA). These models allow a different number of BMD measures to be included per participant. We included either two measures (baseline and visit 2) or three measures (baseline, sleep and visit 2) of BMD per participant which this allows for more precise estimates of change. Random effects models account for between- and within-subject correlation between repeat measurements, and allow for each participant to have a unique estimated intercept (baseline BMD level) and estimated trajectory (change in BMD). Time was modeled as age at the time of the BMD measurement, centered to the median age of 75.5 years. We tested whether BMD loss increased nonlinearly with increasing age by testing the significance of a quadratic term for age; since the quadratic term was significant, age was modeled quadratically in the mixed models. Clinical center was modeled as a fixed effect. We then used the output from the random effects models; the participants’ BMD for each visit was output. Next, each participant’s change in BMD between baseline and Visit 2 was calculated as the difference of these estimated values at baseline and Visit 2. We then grouped participants into three categories based on BMD change, for the femoral neck and total hip separately: maintained BMD (estimated change ≥ 0 g/cm2); expected loss (estimated change between 0 and 1 SD below mean change, −0.034 g/cm2 for femoral neck and −0.042 g/cm2 for total hip); and accelerated loss (estimated change ≥ 1 SD below mean change). We also analyzed change in BMD as a continuous variable. Change in weight and change in PASE score were also estimated using mixed effects models, with age as the time variable expressed linearly.
Characteristics of participants by category of total hip BMD change were tabulated. Differences between these groups were assessed using chi-square tests of categorical variables, ANOVA for normally distributed continuous variables, and Kruskall-Wallis test for skewed continuous variables. Baseline BMD was categorized into tertiles.
Stage 2: Risk of fracture by BMD change
Relative risk of three fracture outcomes [1) hip; 2) non-spine, and 3) non-spine non-hip] after Visit 2 was estimated as hazard ratios using Cox proportional hazards models with those who maintained BMD as the referent group. Models were run separately for change in femoral neck BMD and change in total hip BMD, both as categorical variables (above) and continuous values. For each of the BMD sites, three sets of adjusted models were run: a “base model”, adjusted for age, race, presence of at least one co-morbid condition at baseline, physical activity at baseline, change in physical activity from Visit 1 to Visit 2, weight at baseline, change in weight from Visit 1 to Visit 2, self-rated health at baseline, and change in self-rated health from Visit 1 to Visit 2. The covariates in the base model were selected a priori as potential confounders of the association between change in BMD and subsequent risk of fracture. The second set of adjusted models included those covariates in the base model, plus adjustment for baseline BMD. The third set of adjusted models included those covariates in the base model, plus adjustment for Visit 2 BMD.
Poisson regression was used to estimate the absolute risk of first fracture (expressed per 100 person-years) by category of BMD change. Absolute risk models were adjusted for the same set of covariates as the relative risk models and the estimated rates expressed at the mean values of the covariates in the model. Absolute risk of fracture was also graphically displayed for the nine combination categories of baseline BMD and category of BMD change; these rates were adjusted for the “base model” set of covariates. Finally, for all models described above, sensitivity analyses were completed where men who experienced a fracture during the BMD change period were excluded, and the analyses were re-run.
We tested for the presence of effect modification in the relative risk models, for both hip and non-spine fracture. We evaluated whether baseline BMD, baseline age or baseline weight modified the association between change in BMD and risk of fracture. To do this, we separately tested the significance of an interaction term that was defined as the potential effect modifier (baseline BMD, baseline age or baseline weight) as a continuous variable times the change in BMD as a continuous variable; presence of an interaction was considered significant at a p<0.10. Models were run separately for femoral neck and total hip BMD.
Results
Characteristics of participants by change in BMD
Mean change in total hip BMD was 1.3% (0.012 g/cm2) for the maintained group, −1.9% (−0.018 g/cm2) for the expected loss group, and −6.8% (−0.062 g/cm2) for the accelerated loss group during 4.5 years between baseline and Visit 2. Participants classified as having accelerated loss of total hip BMD at the baseline exam tended to be less healthy at baseline than those in the expected or maintained BMD groups. For example, men with accelerated loss tended to be older, have lower baseline total hip and femoral neck BMD, lower weight, worse self-rated health, lower physical activity, worse physical performance and reported more prevalent medical conditions than those who had expected BMD loss or maintained BMD at the total hip over time (Table 1). There was no difference in the history of fracture before baseline by category of BMD loss.
Table 1.
Characteristics of participants (mean ± SD or N, %) by category of total hip BMD change
| Maintained (N= 1171) |
Expected loss (N= 2689) |
Accelerated loss (N= 610) |
p-value | |
|---|---|---|---|---|
| Age at baseline (years) | 71.5 ± 4.9 | 72.8 ± 5.3 | 75.9 ± 5.7 | <.001 |
| Baseline total hip BMD (g/cm2) | 0.97 ± 0.15 | 0.96 ± 0.13 | 0.95 ± 0.14 | <.001 |
| Visit 2 total hip BMD (g/cm2) | 1.00 ± 0.15 | 0.94 ± 0.13 | 0.86 ± 0.14 | <.001 |
| Change in total hip BMD, baseline to Visit 2 (%) | 1.25 ± 1.17 | −1.89 ± 1.24 | −6.82 ± 2.51 | <.001 |
| Baseline femoral neck BMD (g/cm2) | 0.80 ± 0.14 | 0.79 ± 0.12 | 0.77 ± 0.13 | <.001 |
| Visit 2 femoral neck BMD (g/cm2) | 0.81 ± 0.14 | 0.77 ± 0.12 | 0.71 ± 0.13 | <.001 |
| Change in femoral neck BMD, baseline to Visit 2 (%) | 0.23 ± 2.17 | −1.72 ± 2.07 | −5.18 ± 3.24 | <.001 |
| Weight at baseline (kg) | 84.6 ± 13.8 | 83.1 ± 12.5 | 83.4 ± 14.0 | 0.001 |
| Weight change category, baseline to Visit 2 | ||||
| No change or gain | 368 (31.4) | 527 (19.6) | 63 (10.3) | <.001 |
| Loss < 5% | 770 (65.8) | 1929 (71.7) | 367 (60.2) | |
| At least 5% loss | 33 (2.8) | 233 (8.7) | 180 (29.5) | |
| Height at baseline (cm) | 174.9 ± 6.9 | 174.5 ± 6.8 | 173.7 ± 6.8 | 0.002 |
| BMI at baseline (kg/m2) | 27.6 ± 3.9 | 27.3 ± 3.6 | 27.6 ± 4.3 | 0.017 |
| Excellent, good self-reported health at baseline | 1060 (90.5) | 2398 (89.2) | 516 (84.6) | 0.001 |
| Change in health status, baseline to Visit 2 | ||||
| Improved | 178 (15.2) | 383 (14.3) | 65 (10.7) | <.001 |
| Stable | 759 (64.8) | 1750 (65.1) | 373 (61.2) | |
| Declined | 234 (20.0) | 554 (20.6) | 172 (28.2) | |
| At least 1 medical condition at baseline* | 904 (77.2) | 2031 (75.53) | 503 (82.5) | 0.001 |
| PASE score at baseline | 153.5 ± 70.2 | 152.4 ± 65.6 | 145.1 ± 69.4 | 0.029 |
| Change in PASE, baseline to Visit 2 (%/yr) | −2.5 ± 4.0 | −2.6 ± 5.3 | −3.1 ± 6.7 | 0.024 |
| White race | 1030 (88.0) | 2448 (91.0) | 562 (92.1) | 0.003 |
| History of any fracture before baseline | 639 (54.6) | 1490 (55.4) | 358 (58.7) | 0.236 |
| Smoking status at baseline | ||||
| Never | 435 (37.2) | 1074 (40.0) | 240 (39.3) | 0.014 |
| Past | 710 (60.6) | 1535 (57.1) | 341 (55.9) | |
| Current | 26 (2.2) | 79 (2.9) | 29 (4.8) | |
| Alcoholic drinks per week at baseline | ||||
| None | 349 (29.8) | 903 (33.6) | 229 (37.7) | 0.010 |
| 1–13 | 667 (57.0) | 1481 (55.1) | 315 (51.8) | |
| 14+ | 155 (13.2) | 302 (11.2) | 64 (10.5) | |
| Walking speed at baseline (m/s) | 1.25 ± 0.2 | 1.24 ± 0.2 | 1.15 ± 0.2 | <.001 |
| Grip strength at baseline (kg) | 40.5 ± 8.0 | 39.7 ± 7.8 | 36.6 ± 7.7 | <.001 |
| IADL limitation at baseline† | 112 (9.6) | 269 (10.0) | 121 (20.1) | <.001 |
| Physical limitation at baseline‡ | 86 (7.4) | 241 (9.0) | 128 (21.0) | <.001 |
| Frailty status at baseline§ | ||||
| Robust | 558 (47.7) | 1280 (47.6) | 198 (32.5) | <.001 |
| Intermediate | 545 (46.6) | 1237 (46.0) | 331 (54.3) | |
| Frail | 67 (5.7) | 171 (6.4) | 81 (13.3) | |
| Non-spine fracture after Visit 2 | 80 (6.8) | 209 (7.8) | 82 (13.4) | <.001 |
| Hip fracture after Visit 2 | 9 (0.8) | 39 (1.5) | 30 (4.9) | <.001 |
BMD: bone mineral density; BMI: body mass index; PASE: Physical Activity Scale for the Elderly
At least one of the following conditions: diabetes, stroke, hyper- or hypothyroidism, Parkinson’s disease, heart attack, congestive heart failure, chronic obstructive pulmonary disease, cancer, hypertension, arthritis (osteoarthritis or rheumatoid), and angina pectoris.
Any self-reported difficulty with meal preparation, shopping or housework
Any self-reported difficulty with walking 2–3 blocks or climbing 10 stairs
Main analyses: relative risk of fracture
Over an average of 4.5 years of follow-up after Visit 2, 371 (8.3%) men experienced at least one non-spine fracture, including 78 men (1.7%) who experienced at least one hip fracture. Most common types of fractures after Visit 2 were rib fractures (N=83, 22.9% of first fractures after Visit 2); hip fractures (N=72, 19.4% of first fractures after Visit 2); and fractures of the ankle/foot/toes and heel (N=65, 17.5 of first fractures after Visit 2%). Men classified as having accelerated loss at the femoral neck were about 2 times as likely to have at least one non-spine fracture than men who maintained BMD over time, after adjustment for age and other potential confounders (Table 2). This association was essentially unchanged after further adjustment for baseline BMD. The association was attenuated and of borderline significance (p=0.1) after adjustment for Visit 2 BMD. Men with accelerated loss of BMD at the femoral neck also had a very high risk of hip fractures (HR=6.28, 95% CI; 2.66, 14.81) compared to men who maintained BMD over time. This association was essentially unchanged by adjustment for baseline BMD, and was somewhat attenuated but remained significant after adjustment for Visit 2 BMD. Results for change in total hip BMD were similar to results for change in femoral neck BMD. Men with expected loss in either total hip or femoral neck BMD were not at an increased risk of non-spine fracture compared to the maintained group. Similarly, men with expected loss in total hip BMD did not have an increased risk of hip fracture compared to those who maintained BMD during the 4.6 years between exams. Results for non-spine, non-hip fractures were slightly attenuated when compared to results for all non-spine fractures.
Table 2.
Hazard ratio (95% confidence interval) for non-spine, hip, and non-spine non-hip fracture by category of femoral neck and total hip BMD change
| Change in Femoral neck BMD | |||
|---|---|---|---|
| Multivariate model (Base Model)* |
Base Model + baseline BMD |
Base Model + visit 2 BMD |
|
| Non-spine fracture | |||
| Maintained | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Expected loss | 1.11 (0.85, 1.45) | 1.08 (0.83, 1.41) | 0.89 (0.68, 1.16) |
| Accelerated loss | 1.98 (1.42, 2.75) | 2.06 (1.48, 2.87) | 1.34 (0.95, 1.89) |
| Hip fracture | |||
| Maintained | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Expected loss | 2.41 (1.08, 5.37) | 2.41 (1.08, 5.36) | 1.52 (0.68, 3.41) |
| Accelerated loss | 6.28 (2.66, 14.81) | 7.19 (3.04, 17.03) | 2.63 (1.08, 6.38) |
| Non-hip, non-spine fracture | |||
| Maintained | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Expected loss | 1.00 (0.76, 1.32) | 0.98 (0.74, 1.29) | 0.84 (0.63, 1.11) |
| Accelerated loss | 1.56 (1.08, 2.25) | 1.61 (1.11, 2.32) | 1.15 (0.78, 1.68) |
| Change in Total hip BMD | |||
| Non-spine fracture | |||
| Maintained | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Expected loss | 1.13 (0.87, 1.47) | 1.15 (0.89, 1.50) | 0.99 (0.76, 1.29) |
| Accelerated loss | 1.92 (1.37, 2.69) | 1.89 (1.35, 2.64) | 1.32 (0.93, 1.88) |
| Hip fracture | |||
| Maintained | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Expected loss | 1.87 (0.90, 3.89) | 2.06 (0.99, 4.30) | 1.53 (0.74, 3.20) |
| Accelerated loss | 6.10 (2.74, 13.59) | 6.20 (2.79, 13.76) | 3.08 (1.36, 6.98) |
| Non-hip, non-spine fracture | |||
| Maintained | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Expected loss | 1.10 (0.83, 1.46) | 1.12 (0.85, 1.48) | 0.99 (0.75, 1.31) |
| Accelerated loss | 1.51 (1.03, 2.21) | 1.48 (1.01, 2.17) | 1.10 (0.74, 1.64) |
Adjusted for age, race, presence of at least one medical condition at baseline, Physical Activity Scale for the Elderly score (PASE) at baseline, change in PASE score from baseline to Visit 2, weight at baseline, change in weight from baseline to Visit 2, self-rated health at baseline, and category of change in self-rated health from baseline to Visit 2.
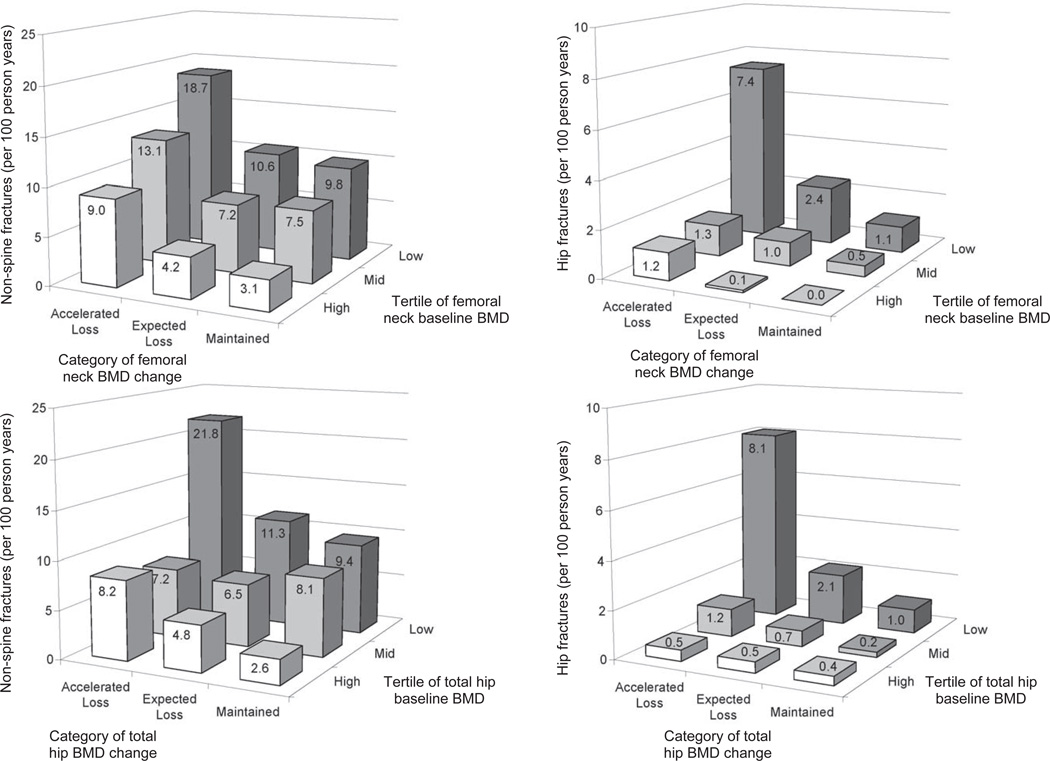
Men with the most BMD loss over time and who had the lowest BMD at baseline had the highest incidence of hip and non-spine fractures compared to other groups (Figure 2). For example, the multivariate adjusted rate of fracture for the men who had accelerated loss of femoral neck BMD and who were in the lowest tertile of femoral neck BMD at baseline was 7.4 per 100 person years (95% CI, 3.0 to 11.9) for hip fractures and 18.7 per 100 person years (95% CI, 12.1 to 25.3) for non-spine fractures. In comparison, none of the 411 men who maintained femoral neck BMD and were in the highest tertile of femoral neck BMD experienced a hip fracture during follow-up, and the multivariate adjusted rate of non-spine fractures in this group was only 3.1 per 100 person years (95% CI, 1.5 to 4.8). In fact, the majority of hip fractures occurred in men who were in the lowest tertile of baseline femoral neck BMD who also had expected or accelerated loss of BMD: 52 of the 78 hip fractures observed in this cohort (67%) occurred in this group of men. In contrast, only 7 of the 78 hip fractures (9.0%) occurred in men who maintained femoral BMD over time, regardless of their BMD at baseline.
Figure 2.
Adjusted rate of non-spine and hip fracture per 100 person years, by category of BMD change and tertile of baseline BMD.
Cut-points for baseline total hip BMD tertiles are: low < 0.90 g/cm2 (t-score < −0.98); mid 0.90–1.02 g/cm2 (t-score of −0.98 to −0.15); high ≥1.02 g/cm2 (t-score ≥ −0.15). Cut-points for baseline femoral neck BMD are: low < 0.73 g/cm2 (t-score < −1.49); mid 0.73–0.83 g/cm2 (t-score −1.49 to −0.76); high ≥0.83 g/cm2 (t-score≥−0.76). For femoral neck BMD, there were 350 men in the low baseline BMD/maintained group; 969 men in the low baseline BMD/expected loss group; 170 men in the low baseline BMD/accelerated loss group; 352 men in the mid baseline BMD/maintained group; 966 men in the mid baseline BMD/expected loss group; 172 men in the mid baseline BMD/accelerated loss group; 411 men in the high baseline BMD/maintained group; 871men in the high baseline BMD/expected loss group; and 209 men in the high baseline BMD/accelerated loss group. For total hip BMD, there were 387 men in the low baseline BMD/maintained group; 869 men in the low baseline BMD/expected loss group; 233 men in the low baseline BMD/accelerated loss group; 347 men in the mid baseline BMD/maintained group; 944 men in the mid baseline BMD/expected loss group; 199 men in the mid baseline BMD/accelerated loss group; 437 men in the high baseline BMD/maintained group; 876 men in the high baseline BMD/expected loss group; and 178 men in the high baseline BMD/accelerated loss group
Main analyses: absolute risk of fracture
Men with accelerated loss of BMD had a high absolute risk of hip fracture. For example, in the multivariate models not further adjusted for Visit 1 or Visit 2 BMD, the rate of hip fracture for men with accelerated loss of femoral neck BMD was 2.9 per 100 person years (95% CI: 1.5, 4.3). Absolute risk models (i.e., models that report the rate) of first non-spine and hip fracture results (Table 3) were similar to the relative risk models (i.e., models that report the hazard ratio): those with accelerated loss had an increased rate of fracture that was slightly attenuated by adjustment for Visit 1 BMD and more strongly attenuated by adjustment for Visit 2 BMD.
Table 3.
Adjusted rate of first non-spine and hip fracture per 100 person years (95% confidence interval) by category of femoral neck and total hip BMD change
| Change in Femoral neck BMD | |||
|---|---|---|---|
| Multivariate model (Base Model)* |
Base Model + baseline BMD |
Base Model + visit 2 BMD |
|
| Non-spine fracture | |||
| Maintained | 6.6 (5.1, 8.1) | 6.2 (4.8, 7.6) | 7.3 (5.6, 9.0) |
| Expected loss | 7.3 (6.3, 8.3) | 6.7 (5.7, 7.7) | 6.5 (5.6, 7.5) |
| Accelerated loss | 13.0 (9.9, 16.0) | 12.7 (9.7, 15.8) | 9.7 (7.2, 12.2) |
| Hip fracture | |||
| Maintained | 0.5 (0.1, 0.8) | 0.3 (0.05, 0.5) | 0.4 (0.1, 0.8) |
| Expected loss | 1.1 (0.7, 1.5) | 0.7 (0.4, 1.0) | 0.7 (0.4, 1.0) |
| Accelerated loss | 2.9 (1.5, 4.3) | 2.0 (1.0, 3.1) | 1.1 (0.5, 1.8) |
| Change in Total hip BMD | |||
| Non-spine fracture | |||
| Maintained | 6.5 (5.0, 8.0) | 6.0 (4.6, 7.3) | 6.8 (5.3, 8.4) |
| Expected loss | 7.4 (6.3, 8.4) | 6.9 (5.9, 7.9) | 6.8 (5.8, 7.8) |
| Accelerated loss | 12.5 (9.5, 15.6) | 11.2 (8.5, 14.0) | 9.0 (6.7, 11.4) |
| Hip fracture | |||
| Maintained | 0.5 (0.2, 0.9) | 0.4 (0.1, 0.6) | 0.5 (0.1, 0.8) |
| Expected loss | 1.0 (0.6, 1.4) | 0.8 (0.4, 1.1) | 0.7 (0.4, 1.0) |
| Accelerated loss | 3.2 (1.7, 4.8) | 2.2 (1.2, 3.3) | 1.4 (0.7, 2.2) |
Adjusted for age, race, presence of at least one medical condition at baseline, Physical Activity Scale for the Elderly score (PASE) at baseline, change in PASE score from baseline to Visit 2, weight at baseline, change in weight from baseline to Visit 2, self-rated health at baseline, and category of change in self-rated health from baseline to Visit 2. Estimated rates are expressed at the mean values of the covariates in the model.
Sensitivity analyses
Exclusion of participants with fractures during BMD change period
During the BMD change period (between baseline and Visit 2), 258 men had at least one non-spine fracture and 21 men experienced at least one hip fracture. Exclusion of these men who experienced a non-spine or hip fracture during the BMD change period (from baseline to Visit 2) did not substantially change results for either non-spine or hip fractures nor for change in total hip BMD or femoral neck BMD (data not shown).
Analysis of change in BMD as a continuous variable
Analysis of femoral neck or total hip BMD as a continuous variable demonstrated similar results to the analysis of categories of change, therefore, only the categorical analyses are presented.
Stratified analyses
When the analyses were stratified by tertile of baseline weight, the association between change in BMD and risk of non-spine fracture was highest in the lowest tertile of baseline weight. For those in the lowest baseline weight tertile (weight < 77.0 kgs), the HR for non-spine fracture for accelerated loss of femoral neck BMD was 3.6 (95% CI; 2.0, 6.4) compared to maintained. In comparison, for those in the highest tertile of baseline weight (weight ≥ 87.7 kgs), the HR for non-spine fracture for accelerated loss of femoral neck BMD was only 1.4 (95% CI: 0.81, 2.4). The interaction term for weight and change in BMD was significant: p for interaction, change in femoral neck BMD*weight = 0.045; p for interaction, change in total hip BMD*weight = 0.038. There was no evidence of an interaction between baseline BMD or age and change in BMD (either femoral neck or total hip) and the risk of hip; non-spine non-hip; or non-spine fracture (p≥0.10 for all).
Subtypes of hip fracture
Finally, we examined the association between change in BMD and relative risk of subtypes of hip fracture. Of the 72 first hip fractures that occurred after Visit 2, 40 were at the femoral neck, 28 were intertrochanteric, and 2 were other types of hip fracture. Estimates of the association between change in total hip BMD and risk of subtypes of hip fracture were unstable as only one participant who maintained total hip BMD experienced an intertrochanteric fracture. The results for the association between change in femoral neck BMD and risk of subtypes of hip fracture suggested that the association between change in femoral neck BMD was similarly related to each fracture subtype. For example, in the multivariate model not adjusted for baselne or Visit 2 BMD, men with accelerated loss of femoral neck BMD were 5.60 (95% CI: 1.80, 17.39) times more likely to have a femoral neck hip fracture and 5.95 (95% CI: 1.56, 22.74) times more likely to have a intertrochanteric hip fracture than men who maintained BMD over time. Adjustment for baseline BMD did not substantially alter these results, while adjustment for Visit 2 BMD attenuated the results such that they were not longer significant.
Discussion
We found that change in BMD was a very strong risk factor for subsequent fracture, especially hip fracture in older men. This association was not explained by covariates or initial BMD. The relation between change in BMD and risk of fracture was similar for both total hip and femoral neck BMD. This association was somewhat, but not completely, attenuated by the final BMD measurement. Those with accelerated loss of BMD had a high absolute risk of hip fracture, and those who had both accelerated loss of BMD and a low BMD at baseline had a very high risk of hip; any non-spine; and non-hip non-spine fracture. The association between change in BMD and risk of fracture was somewhat stronger among men who were in the lowest tertile of initial weight. The relation between change in BMD and risk of fracture was stronger for hip fractures than for any non-spine fractures. There was a modest association between change in BMD and non-hip non-spine fractures, suggesting that the association between change in BMD and non-spine fracture risk is not solely due to the relation between the change in BMD and hip fracture risk.
These results suggest that the most proximal measure of BMD explains some, but not all, of the association between change in BMD and risk of hip fracture or any non-spine fracture. Even those men who start with high BMD and who have accelerated loss over time are at an increased risk of hip and any non-spine fracture compared to those who maintain BMD over time. Thus, we conclude that change in BMD itself is an important factor to consider when assessing fracture risk, particularly since hip fractures are important causes of disability. However, the most proximal measure of BMD did attenuate the association between change in BMD and risk of non-spine non-hip fracture, suggesting that change in BMD may not be an important risk factor for peripheral fractures at sites other than the hip.
While the association between change in BMD and risk of fracture has been previously studied in women,(12–17) we know of only one report of the relation between change in BMD and risk of fracture in older men.(19) The previous reports in both men and women have tended to demonstrate an association between greater loss of BMD with increased fracture risk. Our work and previous studies are not directly comparable, because other studies did not use mixed effects models to assess change and because the quadratic nature of the change in our models precludes reporting annualized change values. The Berger study found that each 0.01 g/cm2/yr loss at the femoral neck was associated with an 1.6 fold increased risk of fracture in men, while our results showed that men classified as accelerated loss (−5.18% loss at the femoral neck over 4.8 years) was associated with a 1.98 fold increased risk of non-spine fracture. Qualitatively it appears that our measure of accelerated loss is more strongly associated with fracture risk, especially hip fracture risk, than other methods to assess or define change in BMD. This may be because our definition of bone loss is more precise, or because it defines a somewhat different population than other definitions of bone loss; our definition may be identifying more extreme categories of bone loss than previous analyses. Additionally, our analyses include older men (who have greater loss than younger men) and adjudicated fracture outcomes which might reduce measurement error and result in stronger effect estimates.
The reason for the relation between change in BMD and risk of fracture is not completely clear. Our results suggest that change, in and of itself, is important for fracture risk, independent of the first or final measure of BMD. However, at least some of the effect of change on fracture risk is due to the fact that the BMD measurement closer to the time of the fracture is most predictive of that fracture. We speculate that change in BMD as measured by DXA, especially rapid changes in BMD, may be reflective not only of changes in apparent BMD, but also of changes in bone mechanical properties or microarchitecture that may not be reflected in a single DXA-based measure of BMD.(33) Alternatively, men with accelerated loss may differ from those who maintained BMD in a number of ways, such as acute illness, change in fall risk or other factors that we did not or could not measure; thus, our results might be explained by such unmeasured factors.
The association between change in BMD and hip fracture was particularly strong. The multivariate-adjusted HR for hip fracture, per each SD loss of femoral neck BMD, was 1.44 (95% CI: 1.2, 1.7). In comparison, from the same multivariate model, the HR for hip fracture for each 5 years of additional age was 1.46 (95% CI: 1.2, 1.8). Thus, each additional standard deviation loss of femoral neck BMD increases hip fracture risk in a similar magnitude to 5 years of additional age. The associations were similar for subtypes of hip fracture (femoral neck and intertrochanteric).
Our results suggest that certain factors might be helpful in identifying subsets of men for whom routine bone densitometry screening followed by bisphosphonate treatment may be clinically appropriate, such as screening and treating men with relatively lower weight. However, further research would need to be completed before we could conclude that repeat BMD testing and subsequent treatment in such a population would be cost effective. Additionally, while the results from these analyses also suggest that a single measure of BMD may not be sufficient to estimate all men’s fracture risk over time, these analyses were not designed to determine the frequency or time intervals for BMD screening for older men. Our results suggest that other analyses, such as those recently employed for women(34) should be applied to the MrOS data to determine optimal screening intervals for older men.
These analyses have a number of strengths. First, change in BMD was assessed before the assessment of fracture risk, ensuring that fractures analyzed as outcomes did not influence the rate of change in BMD. The use of mixed effects models to estimate change reduced the intra-individual variation in estimates of change in BMD. However, a number of possible limitations must be noted. First, there may be remaining factors that we did not or could not measure that might confound the relation between change in BMD and risk of fracture. Although the use of mixed models is a sound statistical approach, the use of such models may limit the direct clinical utility of these results (as a simple linear change was not analyzed). Additionally, the generalizability of our results may be limited; for example, it is unclear whether these conclusions would apply to women or younger men.
In summary, change in BMD at the femoral neck or total hip is a strong risk factor for hip and other non-spine fractures in older men, and this relation is not explained by covariates or initial BMD, but is somewhat attenuated by the final BMD measurement. The highest absolute rate of fracture was seen in men who started with low BMD and lost the most BMD over time. Future research should aim to identify BMD screening intervals for older men and to understand the biological underpinnings for the association between change in BMD and fracture risk.
Acknowledgements
The Osteoporotic Fractures in Men (MrOS) Study is supported by National Institutes of Health funding. The following institutes provide support: the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), the National Institute on Aging (NIA), the National Center for Research Resources (NCRR), and NIH Roadmap for Medical Research under the following grant numbers: U01 AR45580, U01 AR45614, U01 AR45632, U01 AR45647, U01 AR45654, U01 AR45583, U01 AG18197, U01-AG027810, and UL1 RR024140
Footnotes
Author contributions: Peggy Cawthon: Lead analysis design, drafted manuscript, interpreted data; Susan Ewing: completed statistical analyses; Dawn Mackey, Howard Fink, Doug Bauer: critically reviewed manuscript; assisted with analysis design; Steven R Cummings, Kristine Ensrud, Marcia Stefanick, Jane Cauley, Eric Orwoll: acquisition of data; critically reviewed manuscript; assisted with analysis design.
References
- 1.Ensrud KE, Palermo L, Black DM, Cauley J, Jergas M, Orwoll ES, Nevitt MC, Fox KM, Cummings SR. Hip and calcaneal bone loss increase with advancing age: longitudinal results from the study of osteoporotic fractures. J Bone Miner Res. 1995;10(11):1778–1787. doi: 10.1002/jbmr.5650101122. [DOI] [PubMed] [Google Scholar]
- 2.Dennison E, Eastell R, Fall CH, Kellingray S, Wood PJ, Cooper C. Determinants of bone loss in elderly men and women: a prospective population-based study. Osteoporos Int. 1999;10(5):384–391. doi: 10.1007/s001980050244. [DOI] [PubMed] [Google Scholar]
- 3.Hannan MT, Felson DT, Dawson-Hughes B, Tucker KL, Cupples LA, Wilson PW, Kiel DP. Risk factors for longitudinal bone loss in elderly men and women: the Framingham Osteoporosis Study. J Bone Miner Res. 2000;15(4):710–720. doi: 10.1359/jbmr.2000.15.4.710. [DOI] [PubMed] [Google Scholar]
- 4.Melton LJ, 3rd, Khosla S, Atkinson EJ, Oconnor MK, Ofallon WM, Riggs BL. Cross-sectional versus longitudinal evaluation of bone loss in men and women. Osteoporos Int. 2000;11(7):592–599. doi: 10.1007/s001980070080. [DOI] [PubMed] [Google Scholar]
- 5.Slemenda CW, Christian JC, Reed T, Reister TK, Williams CJ, Johnston CC., Jr Long-term bone loss in men: effects of genetic and environmental factors. Ann Intern Med. 1992;117(4):286–291. doi: 10.7326/0003-4819-117-4-286. [DOI] [PubMed] [Google Scholar]
- 6.Tracy JK, Meyer WA, Flores RH, Wilson PD, Hochberg MC. Racial differences in rate of decline in bone mass in older men: the Baltimore men's osteoporosis study. J Bone Miner Res. 2005;20(7):1228–1234. doi: 10.1359/JBMR.050310. [DOI] [PubMed] [Google Scholar]
- 7.Warming L, Hassager C, Christiansen C. Changes in bone mineral density with age in men and women: a longitudinal study. Osteoporos Int. 2002;13(2):105–112. doi: 10.1007/s001980200001. [DOI] [PubMed] [Google Scholar]
- 8.Burger H, de Laet CE, van Daele PL, Weel AE, Witteman JC, Hofman A, Pols HA. Risk factors for increased bone loss in an elderly population: the Rotterdam Study. Am J Epidemiol. 1998;147(9):871–879. doi: 10.1093/oxfordjournals.aje.a009541. [DOI] [PubMed] [Google Scholar]
- 9.Szulc P, Delmas PD. Bone loss in elderly men: increased endosteal bone loss and stable periosteal apposition. The prospective MINOS study. Osteoporos Int. 2007;18(4):495–503. doi: 10.1007/s00198-006-0254-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cummings SR, Cawthon PM, Ensrud KE, Cauley JA, Fink HA, Orwoll ES. BMD and risk of hip and nonvertebral fractures in older men: a prospective study and comparison with older women. J Bone Miner Res. 2006;21(10):1550–1556. doi: 10.1359/jbmr.060708. [DOI] [PubMed] [Google Scholar]
- 11.Nguyen TV, Eisman JA, Kelly PJ, Sambrook PN. Risk factors for osteoporotic fractures in elderly men. Am J Epidemiol. 1996;144(3):255–263. doi: 10.1093/oxfordjournals.aje.a008920. [DOI] [PubMed] [Google Scholar]
- 12.Riis BJ, Hansen MA, Jensen AM, Overgaard K, Christiansen C. Low bone mass and fast rate of bone loss at menopause: equal risk factors for future fracture: a 15-year follow-up study. Bone. 1996;19(1):9–12. doi: 10.1016/8756-3282(96)00102-0. [DOI] [PubMed] [Google Scholar]
- 13.Gnudi S, Malavolta N, Lisi L, Ripamonti C. Bone mineral density and bone loss measured at the radius to predict the risk of nonspinal osteoporotic fracture. J Bone Miner Res. 2001;16(6):1130–1135. doi: 10.1359/jbmr.2001.16.6.1130. [DOI] [PubMed] [Google Scholar]
- 14.Nguyen TV, Center JR, Eisman JA. Femoral neck bone loss predicts fracture risk independent of baseline BMD. J Bone Miner Res. 2005;20(7):1195–1201. doi: 10.1359/JBMR.050215. [DOI] [PubMed] [Google Scholar]
- 15.Sornay-Rendu E, Munoz F, Duboeuf F, Delmas PD. Rate of forearm bone loss is associated with an increased risk of fracture independently of bone mass in postmenopausal women: the OFELY study. J Bone Miner Res. 2005;20(11):1929–1935. doi: 10.1359/JBMR.050704. [DOI] [PubMed] [Google Scholar]
- 16.Hillier TA, Stone KL, Bauer DC, Rizzo JH, Pedula KL, Cauley JA, Ensrud KE, Hochberg MC, Cummings SR. Evaluating the value of repeat bone mineral density measurement and prediction of fractures in older women: the study of osteoporotic fractures. Arch Intern Med. 2007;167(2):155–160. doi: 10.1001/archinte.167.2.155. [DOI] [PubMed] [Google Scholar]
- 17.Bruyere O, Varela AR, Adami S, Detilleux J, Rabenda V, Hiligsmann M, Reginster JY. Loss of hip bone mineral density over time is associated with spine and hip fracture incidence in osteoporotic postmenopausal women. Eur J Epidemiol. 2009;24(11):707–712. doi: 10.1007/s10654-009-9381-4. [DOI] [PubMed] [Google Scholar]
- 18.Leslie W, Morin SN, Lix L. Rate of Bone Density Change Does Not Enhance Fracture Prediction in Routine Clinical Practice. J Clin Endocrinol Metab. 2012 doi: 10.1210/jc.2011-2871. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 19.Berger C, Langsetmo L, Joseph L, Hanley DA, Davison KS, Josse RG, Prior JC, Kreiger N, Tenenhouse A, Goltzman D. Association between change in BMD and fragility fracture in women and men. J Bone Miner Res. 2009;24(2):361–370. doi: 10.1359/jbmr.081004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cawthon PM, Ewing SK, McCulloch CE, Ensrud KE, Cauley JA, Cummings SR, Orwoll ES. Loss of hip BMD in older men: the osteoporotic fractures in men (MrOS) study. J Bone Miner Res. 2009;24(10):1728–1735. doi: 10.1359/JBMR.090419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jones G, Nguyen T, Sambrook P, Kelly PJ, Eisman JA. Progressive loss of bone in the femoral neck in elderly people: longitudinal findings from the Dubbo osteoporosis epidemiology study. Br Med J. 1994;309:691–695. [PMC free article] [PubMed] [Google Scholar]
- 22.Burger H, de Laet CE, van Daele PL, Weel AE, Witteman JC, Hofman A, Pols HA. Risk factors for increased bone loss in an elderly population: the Rotterdam Study. Am J Epidemiol. 1998;147:871–879. doi: 10.1093/oxfordjournals.aje.a009541. [DOI] [PubMed] [Google Scholar]
- 23.Hannan MT, Felson DT, Dawson-Hughes B, Tucker KL, Cupples LA, Wilson PW, Kiel DP. Risk factors for longitudinal bone loss in elderly men and women: the Framingham Osteoporosis Study. J Bone Miner Res. 2000;15:710–720. doi: 10.1359/jbmr.2000.15.4.710. [DOI] [PubMed] [Google Scholar]
- 24.Blank JB, Cawthon PM, Carrion-Petersen ML, Harper L, Johnson JP, Mitson E, Delay RR. Overview of recruitment for the osteoporotic fractures in men study (MrOS) Contemp Clin Trials. 2005;26(5):557–568. doi: 10.1016/j.cct.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 25.Orwoll E, Blank JB, Barrett-Connor E, Cauley J, Cummings S, Ensrud K, Lewis C, Cawthon PM, Marcus R, Marshall LM, McGowan J, Phipps K, Sherman S, Stefanick ML, Stone K. Design and baseline characteristics of the osteoporotic fractures in men (MrOS) study--a large observational study of the determinants of fracture in older men. Contemp Clin Trials. 2005;26(5):569–585. doi: 10.1016/j.cct.2005.05.006. [DOI] [PubMed] [Google Scholar]
- 26.Cummings SR, Bates D, Black DM. Clinical use of bone densitometry: scientific review. JAMA. 2002;288(15):1889–1897. doi: 10.1001/jama.288.15.1889. [DOI] [PubMed] [Google Scholar]
- 27.Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC, Jr, Lindsay R. Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int. 1998;8(5):468–489. doi: 10.1007/s001980050093. [DOI] [PubMed] [Google Scholar]
- 28.Mackey DC, Lui LY, Cawthon PM, Bauer DC, Nevitt MC, Cauley JA, Hillier TA, Lewis CE, Barrett-Connor E, Cummings SR. High-trauma fractures and low bone mineral density in older women and men. Jama. 2007;298(20):2381–2388. doi: 10.1001/jama.298.20.2381. [DOI] [PubMed] [Google Scholar]
- 29.Washburn RA, Smith KW, Jette AM, Janney CA. The Physical Activity Scale for the Elderly (PASE): development and evaluation. J ClinEpidemiol. 1993;46:153–162. doi: 10.1016/0895-4356(93)90053-4. [DOI] [PubMed] [Google Scholar]
- 30.Cawthon PM, Fink HA, Barrett-Connor E, Cauley JA, Dam TT, Lewis CE, Marshall LM, Orwoll ES, Cummings SR. Alcohol use, physical performance, and functional limitations in older men. J Am Geriatr Soc. 2007;55(2):212–220. doi: 10.1111/j.1532-5415.2007.01062.x. [DOI] [PubMed] [Google Scholar]
- 31.Cawthon PM, Marshall LM, Michael Y, Dam TT, Ensrud KE, Barrett-Connor E, Orwoll ES. Frailty in older men: prevalence, progression, and relationship with mortality. J Am Geriatr Soc. 2007;55(8):1216–1223. doi: 10.1111/j.1532-5415.2007.01259.x. [DOI] [PubMed] [Google Scholar]
- 32.Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie MA. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–M156. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 33.Liu XS, Cohen A, Shane E, Yin PT, Stein EM, Rogers H, Kokolus SL, McMahon DJ, Lappe JM, Recker RR, Lang T, Guo XE. Bone density, geometry, microstructure, and stiffness: Relationships between peripheral and central skeletal sites assessed by DXA, HR-pQCT, and cQCT in premenopausal women. J Bone Miner Res. 2010;25(10):2229–2238. doi: 10.1002/jbmr.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gourlay ML, Fine JP, Preisser JS, May RC, Li C, Lui LY, Ransohoff DF, Cauley JA, Ensrud KE. Bone-density testing interval and transition to osteoporosis in older women. N Engl J Med. 2012;366(3):225–233. doi: 10.1056/NEJMoa1107142. [DOI] [PMC free article] [PubMed] [Google Scholar]