Abstract
Background
Although dietary weight loss counseling usually employs a 500-1000 kcal/d energy deficit to induce weight loss of 0.5-1 kg/wk, this rate of weight loss is rarely achieved in research settings. Biological factors, such as changes in metabolic rate, are partly responsible but would account for a small deviation from expected weight loss. There must be other factors, behavioral or related to study design and implementation that affect the rate of weight loss observed.
Objective
To examine factors that influence the rate of weight loss obtained in clinical studies.
Design
Thirty-five weight loss studies published between 1995 and 2009 were identified that used dietary counseling to induce weight loss in healthy subjects. Studies were included if they had a duration of at least 6 wk, used a strategy to counsel subjects to reduce free-living energy intakes, and reported weight loss data based on a completers analysis. Variables that were associated with the rate of weight loss among age, gender (% female subjects), initial body weight, frequency of dietary counseling, placebo use, exercise level, study length, and prescribed energy deficit were examined using linear regression analysis.
Results
Study length was negatively related to the rate of weight loss (P<0.0001) whereas subject age (P<0.002), subject age squared (P=0.0073), initial body weight (P=0.0003), frequency of dietary counseling (P=0.0197), and prescribed energy deficit (P<0.0001) were positively related to the rate of weight loss observed in clinical studies.
Conclusions
These findings provide a tool for investigators and clinical dietitians to predict the rate of weight loss that can be expected within a population given the age, initial body weight, frequency of dietary counseling, and energy deficit prescription. These data, from clinical studies, suggest that the rate of weight loss is greater in older and heavier subjects and with higher contact frequency and caloric restriction.
Keywords: Obesity, duration, weight loss, caloric deficit, dietary counseling, diet
INTRODUCTION
The U.S. National Institutes of Health’s clinical guidelines on obesity recommend that a caloric deficit of 500-1,000 kcal/d be prescribed as an integral part of a weight loss program aimed at achieving a safe rate of weight loss of 0.5-1 kg/wk (1). This level of caloric deficit (3500-7000 kcal/wk) should result in the expected rate of weight loss of 0.5-1 kg/wk, assuming that 0.5 kg of fat mass is approximately equivalent to 3500 kcal. Another implicit assumption in this recommendation is that this rate of weight loss remains constant over a period of time. In actuality, during weight loss, the energy level required to maintain a stable body weight is reduced due to metabolic adaptations. One such adaptation is a reduced metabolic rate (2) which may be the result of decreases in metabolically active tissue or in hormone concentrations. Second, the energy costs of daily activities are lower at reduced body weight. Therefore, in order to continue losing weight at the same rate, an individual must also gradually reduce energy intake so as to maintain a constant negative energy balance. To do so, the prescribed caloric deficit should follow the reduction in caloric requirements at lower body weight. If these recommendations are followed, and assumptions hold true, then one should obtain a rate of weight loss of approximately 0.5 kg/wk with a constant caloric deficit of 3500 kcal/wk.
Weight loss studies, however, show a wide range of weight loss achievements within the same study group. For example, a 500 kcal/d deficit, which would be expected to lead to a rate of weight loss of 1 lb/wk, does not create this level of weight loss for all participants. There has been much interest in finding characteristics, either patient- or diet-related, that would predict weight loss success. Williamson et al. (3) have identified 2 components of adherence: behavioral and dietary. Behavioral adherence, including attendance to counseling sessions and self-monitoring, predicted reductions in body weight, waist circumference, and body fat (4) whereas dietary adherence, including adherence to calorie, macronutrient and food goals, was also predictive but to a smaller extent.
Other studies have aimed to determine predictors of weight loss success, defined as losing at least 5 % of initial body weight during the weight loss period. Fabricatore et al. (5) found that shorter duration of overweight and depression were associated with lower success rate whereas Greenberg et al. (6) observed that higher initial body weight, type of diet and physical activity were the most dominant factors contributing to weight loss success. Texeira et al. (7) also identified that fewer previous diets and weight outcome evaluations, and to a lesser degree self-motivation and body image, were associated with weight loss in Portuguese women. They noted that women reporting a larger discrepancy between self and ideal body figures were less likely to lose weight.
These previous studies have identified potential variables that may affect weight loss but tend to be specific to their study population and type of weight loss strategy employed. This study was conducted to determine the empirically observed relationship between caloric deficit prescription and amount of weight loss obtained in previously published weight loss studies. The objective was to evaluate the impact of various study design factors, such as duration of the intervention, caloric deficit and exercise prescription, among others, and subject characteristics, such as age, gender, and initial body weight, on the rate of weight loss. We hypothesized that rate of weight loss would be greater in those with higher initial body weight, more frequent counseling sessions, and greater caloric deficit and exercise prescription. We also hypothesized that the rate of weight loss would be lower in older age and women.
METHODS
A literature search of published studies in the English language was performed in PubMed (National Library of Medicine, National Center for Biotechnology Information, National Institutes of Health) to find weight loss studies. Search terms included weight loss and diet. Acceptable articles were published between January 1995 and December 2009, reported weight loss results from studies with an intervention period of at least 6 wk duration in healthy, adult subjects and used dietary counseling to induce a reduction in subject caloric intake by a fixed amount. Placebo arms of weight loss drug studies were eligible for inclusion if results from all recruited subjects who completed the study were provided. However, arms that involved active drug component were not included in the study. Studies that uniquely reported results of an intent-to-treat analysis were excluded from this analysis; only data from completers analyses were included in this study. Each group within studies consisting of more than one study treatment, such as studies comparing weight loss with diet alone and weight loss with diet and exercise, was included as a separate data point in the analyses. Only data from treatment arms that provided calorie restriction were included in the analysis such that the low carbohydrate arm of the study by Stern et al. (8) was omitted. Similarly, one study tested a low-sucrose diet (9); this diet arm was not included in the analysis. Informed consent was obtained in each of the studies reviewed by their institutional review board. However, this study was exempt.
A general linear model procedure was performed to determine which variables were associated with weekly change in weight. The dependent variable was change in body weight in kg/wk. Independent variables that were included in the general linear model analysis were study length, prescribed caloric deficit, frequency of dietary counseling, percentage of female subjects included in the study, age and initial body weight of the subjects, presence or absence of placebo, and exercise. Study length was the length of time between baseline and endpoint body weight measurements. This may be identical to the length of the intervention program or slightly longer if the intervention had a graded counseling program (ie. weekly for the first X weeks, then bi-weekly for Y weeks, and every 4 weeks for the last Z weeks). Furthermore, in the case of a graded counseling program, frequency of dietary counseling was calculated as the total number of counseling sessions during the study period divided by the total duration (in weeks) of the study. This produced an average frequency of dietary counseling over the entire measurement period which would reflect even rate of counseling throughout the study. However, not all studies actually had a constant counseling schedule. Counseling rate was counted as weekly for one study which used exclusively daily food records (10). Food records were not factored in the model for other studies. However, repeating the analyses including food records as a component of the counseling did not change the overall conclusions of our analysis. Presence and absence of placebo were coded as 1 and 0, respectively, since placebo consumption may remind individuals that they are in a weight loss program and improve compliance. Exercise prescription was graded on a 4-point ordinal scale where 0 corresponded to no exercise recommendation, or recommendation not to alter basal physical activity level; 1 corresponded to physical activity that was encouraged but not structured or controlled within the context of the study; 2 corresponded to prescribed resistance training or aerobic exercise at low intensity or frequency (≤3 times/week); and 3 corresponded to aerobic exercise at high intensity or frequency (most or every day of the week) that was prescribed as part of the study. All study-related variables were converted to weekly values for the purpose of our analyses. Interactions were examined between gender and exercise, energy deficit and exercise, and frequency of counseling and energy deficit. A quadratic effect of energy deficit and age were also tested. Terms that were not statistically significant were removed from the model by stepwise backward elimination. Of the interactions and quadratic effects tested, only a quadratic effect of age was statistically significant. We therefore included both a linear and a quadratic component of age in our model. All statistical analyses were performed using the SAS system for Windows (version 9.2, 2008, SAS Institute Cary, NC). Data are reported as means ± S.E.M and P<0.05 was used to determine statistical significance.
RESULTS
A total of 35 studies published between January 1995 and December 2009 were identified and included in the present analyses (8-42). These studies provided a total of 64 data points. The majority of the studies included dietary counseling without drug treatment; only 7 data points provided placebo pills in addition to the dietary counseling. Twenty-four data points included some recommendation for physical activity; the other advised participants not to alter their physical activity level or provided no information to their participants on physical activity. The age and initial body weight of the subjects in the included studies ranged from 29-71 y (average 45.6 y) and 81.7-129.0 kg (average 95.7 kg). Studies included in the present analysis prescribed energy deficits of 1670-7000 kcal/wk and were of 8-52 wk in duration. The rate of weight loss observed in the studies included here ranged between 0.002-1.13 kg/wk. The average number of subjects represented by each data point was 19.9 ± 3.1 (mode 12, median 13.5). Approximately 25 % of data points represented study arms with 10 subjects or less; 40.6% represented study arms with 11-15 subjects; 23.4% with 16-30 subjects; 6.3% with 31-50 subjects; and 4.7% represented study arms with more than 50 subjects. One study had 188 participants in the treatment arm (28).
Percentage of female subjects, presence or absence of placebo, and exercise were not significant factors in the model to predict rate of weight loss and were not included in the final analyses. Similarly, interactions between gender and exercise, energy deficit and exercise, and frequency of counseling and energy deficit, did not reach statistical significance and were therefore removed from the model. In the final model, only study length, age, initial body weight, prescribed energy deficit, frequency of dietary counseling and a quadratic effect of age were retained (Table 1). The predictive equation for the rate of weight loss (kg/wk) was therefore,
where l is study length in wk, a is age in y, w is initial body weight in kg, c is counseling sessions per week, and Edf is prescribed energy deficit in kcal/wk.
Table 1.
Results of the linear regression model of the predictive variables for rate of weight loss.
| Parameter | Estimate | Standard Error | P-value |
|---|---|---|---|
| Intercept | 2.0738 | 0.4540 | <0.0001 |
| Length, wk | 0.01775 | 0.002547 | <0.0001 |
| Counseling sessions/wk | -0.08964 | 0.03735 | 0.0197 |
| Deficit, kcal/wk | -0.00005719 | 0.00001297 | <0.0001 |
| Age, y | -0.06398 | 0.01979 | 0.0020 |
| Age x age, y2 | 0.0005568 | 0.0002002 | 0.0073 |
| Initial body weight, kg | -0.008814 | 0.002293 | 0.0003 |
The results of the regression analysis show that, as study length (l) increases, the rate of weight loss decreases whereas higher age (a), initial body weight (w), frequency of dietary counseling (c), and prescribed energy deficit (Edf) predict greater rate of weight loss. For example, increasing study length by 1 week would reduce the rate of weight change by 0.01775 kg/wk.
Figures 1 and 2 show the rate of weight loss expected by individuals, differing in age (Figure 1) or initial body weight (Figure 2), counseled to reduce their caloric intakes by 3500 kcal/wk for a period of 16 wk. We chose to present this study length since this was the mode and median of the data points used to generate the data and average study length was 17.7 ± 1.0 weeks. Dietary counseling was set at weekly sessions. The slopes show the rate of weight loss with each treatment length for the various ages and body weights, using our predictive equation, above. The rate of weight loss increases in a linear fashion with increasing age and initial body weight.
Figure 1. Rate of weight loss can be predicted by patient characteristics and intervention strategies.
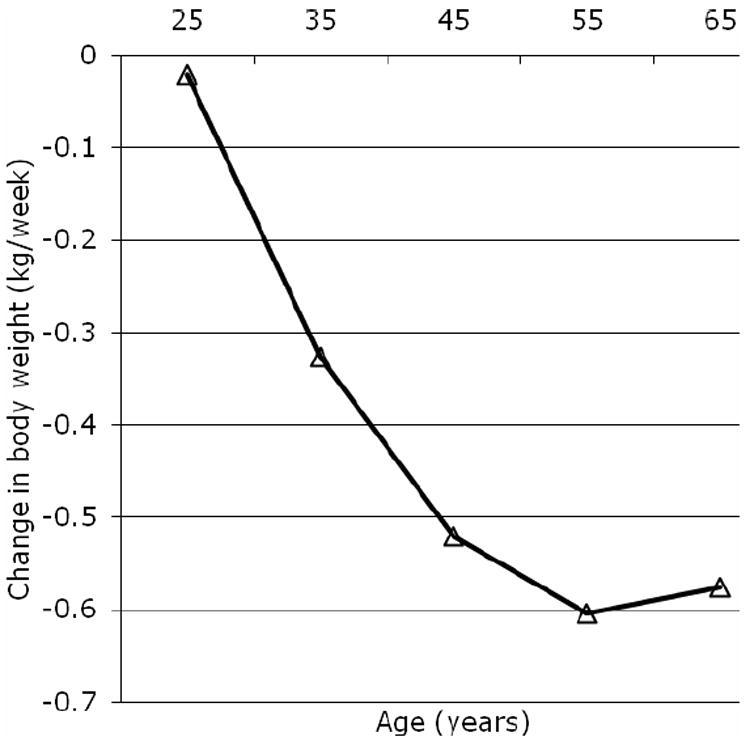
Effect of age on the rate of body weight loss. This figure depicts a hypothetical 95-kg individual undergoing weekly dietary counseling to reduce intakes by 3,500 kcal/wk for a period of 16 weeks.
Figure 2.
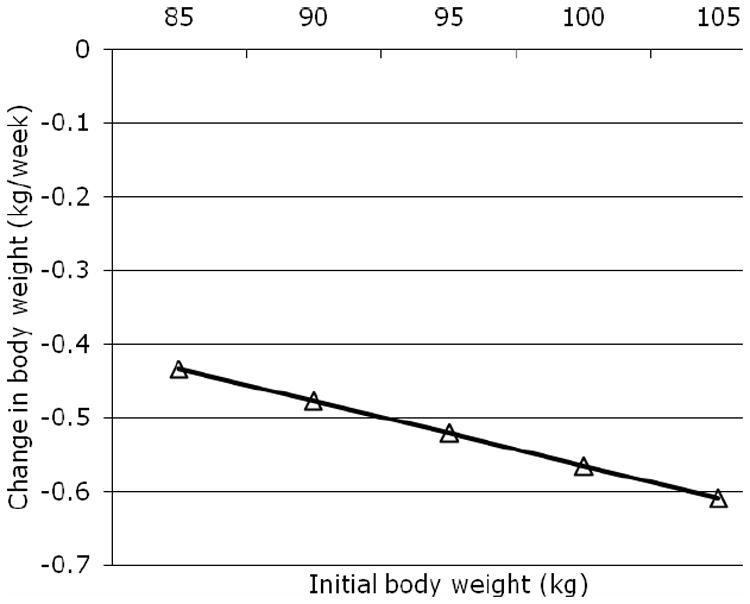
Effect of initial body weight on the rate of body weight loss. This figure depicts a hypothetical 45-y old individual undergoing weekly dietary counseling to reduce intakes by 3,500 kcal/wk deficit for a period of 16 weeks.
A similar strategy was employed for Figure 3, showing the effect of energy deficit (Figure 3) on the rate of weight loss in hypothetical 45-y old, 95-kg individuals. Dietary counseling was set at weekly sessions. The rate of weight loss increased with increasing caloric deficit but the relationship was not proportional.
Figure 3.
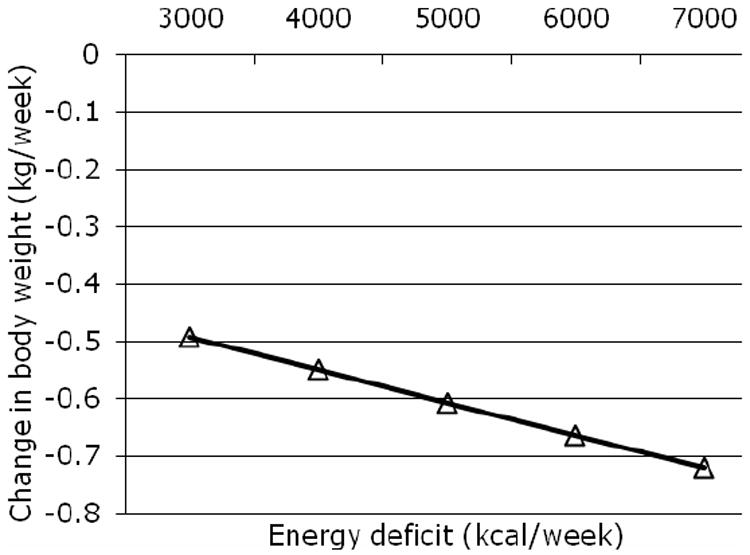
Effect of prescribed caloric deficit on the rate of body weight loss. This figure depicts a hypothetical 45-y old individual, weighing 95 kg, undergoing weekly dietary counseling for a period of 16 weeks.
DISCUSSION
This study shows that several factors must be taken into consideration when projecting a rate of weight loss with dietary restriction. Our prediction equation shows that a prescribed 3500 kcal/wk does not necessarily result in a weight loss of 0.5 kg/wk. Factors such as the individual’s initial body weight and age, the frequency of dietary counseling, prescribed energy deficit, and study length all impact on the actual rate of weight loss that one can predict. Our findings, based on previously published weight loss studies, show that the predicted rate of body weight loss that can be expected increases with increasing initial body weight, subject age, and prescribed energy deficit as well as frequency of dietary counseling. Furthermore, the predicted rate of weight loss decreases with increasing study length.
Our findings that initial body weight positively impacts the rate of weight loss is in agreement with previous studies that found a positive association between weight loss and baseline body weight (6, 43). These observations suggest that heavier individuals may reduce their energy intakes by levels that are closer to those prescribed resulting in improved adherence to the energy deficit prescribed, or reduce their intakes to a greater extent than expected or advised. Energy reductions may be easier to implement when starting intakes are higher and therefore the quantity of food may not be perceived to be very small.
Age was also a significant variable in predicting the rate of weight loss with diet. It was previously observed that older individuals tend to lose more weight on a weight loss diet compared to younger individuals (S. Heshka, personal communication) and this may be due to greater compliance by more mature adults. This is supported by data by Fabricatore et al. who reported that older age was predictive of lower attrition in a weight loss study (5). Although we hypothesize that compliance may be improved in older adults compared to younger adults, compliance is difficult to assess in dietary weight loss counseling and is typically assumed by the weight loss achieved. Greater weight loss during dietary counseling is typically taken to reflect a greater adherence to dietary guidelines set forth by the dietitian.
Of potential relevance is also the observation that older individuals tend to have less food cravings and report craving fewer foods than younger individuals (44). This may improve their compliance with dietary restrictions. In addition, age-related weight loss may partially account for the observed association noted in this study. Das et al. examined the influence of age on regulation of resting energy expenditure (REE) at weight maintenance and after weight loss (45). Changes in REE following underfeeding were compared between young normal weight men and women, young overweight men and women, and older men and women. The REE response to weight change was significantly attenuated in the older subjects as compared to the others groups. Specifically, the decrease in REE during underfeeding was smaller in older subjects as compared to young subjects and the absolute decrease in REE was reduced in older subjects relative to body weight loss. These results support our finding that the rate of weight loss is greater in older relative to younger individuals.
A linear correlation between prescribed energy deficit and weight was loss was demonstrated and exemplified in Figure 4. As long as energy expenditure exceeds energy intake weight loss will result. By prescribing larger energy deficits, the likelihood of reaching the point where energy expenditure surpasses energy intake is increased and, thus, a greater rate of weight loss will be more likely. Additionally, prescribing larger energy deficits allows for subjects to be slightly noncompliant and still achieve sufficient calorie reduction to produce weight loss. In a meta-analysis of very-low calorie diets (<800kcal/d), Tsai et al. (46) reported that very low calorie diets induced significantly greater short term weight loss when compared to conventional low calorie diets. However, this is in contrast to data by Del Corral et al. who reported that greater severity of caloric restriction was related to lower dietary adherence, suggesting that moderate calorie restriction relative to energy needs would be preferable for dietary adherence (47).
Frequency of counseling was also positively predictive of the rate of weight loss. One possible explanation for this finding may be the accountability that is expected from the subjects when they discuss their progress with a dietitian. In addition, contact with a dietician frequently could help to discern subjects who are not complying with the diet sooner and correct their energy intakes to achieve the expected rate of weight loss. This phenomenon of intervention associated with successful weight loss has been previously described by Raatz et al. (48) who reported that weight loss was significantly correlated with attendance to registered dietitian-instructed classes but not with attendance at weigh-in visits without a registered-dietician present.
Our observation that the rate of weight loss decreases as the study length increases may be due to a reduction in compliance with the caloric restriction and dietary modifications imposed by the weight loss program as the study extends in length. This was observed by Brinkworth et al. (49) who found that neither a low-fat nor a low-carbohydrate dietary pattern for weight loss was maintained at 1 y of the research study. Furthermore, this may be by compounded by a lack of adjustment to the lower energy requirements associated with a reduced body weight, which may become increasingly apparent as the study increases in length and subjects lose more weight. Metabolic adaptations have been observed previously in weight loss studies which show that these adaptations act to oppose the weight change obtained (2). For example, using the Harris-Benedict equation with an activity factor of 1.35, an 80-kg, 165-cm, 55-yr old women would require 1980 kcal/d to sustain her body weight. As this person loses weight, her energy requirements decrease such that, at 75 kg, she should consume 1915 kcal/d, a difference of 65 kcal/d. Although seemingly negligible, over time, this reduction in energy requirement can affect the rate of weight loss if caloric intake is not reduced accordingly. Furthermore, our observation that weight loss decreases as study length increases is supported by Sacks et al., who randomly assigned 811 overweight adults to one of four diets with different compositions of fat, protein, and carbohydrates: 20,15, and 65%; 20, 25, and 55%; 40, 15, and 45%; and 40, 25, 35% (50). At 6 mo, participants in each group had lost an average of 6 kg. However, all groups began to gain weight after 12 mo and continued to do so. At 2 y, weight loss in the 15% protein group was 3.0 kg, 25% protein group 3.6 kg, and both the 65% and 35% carbohydrate groups lost 3.3 kg.
Nevertheless, the longer weight loss duration compensates for the lower rate of weight loss such that there is still greater weight loss over a longer weight loss program compared to a shorter weight loss program. Using our predictive equation, we calculated the rate of weight loss with an 8-week weight loss period in a 45-y old prescribed a 3500 kcal/wk deficit to be -0.66 kg/wk. The rate of weight loss for a 16-week study is -0.52 kg/wk. However, total weight loss during the 8-week study would be 5.3 kg compared to 8.3 kg for the 16 week study.
A strength of our analysis was that we found many published studies with a wide range of baseline BMI, age, and length to examine the impact of these factors on rate of weight loss. However, we are limited in the number of men included in these studies and the factors on which studies reported. Other factors that impact the rate of weight loss, such as state of change or motivation to lose weight, were not considered in our analyses. The degree to which the rate of weight loss is affected by the inclusion of these other factors in a model estimate is uncertain. Moreover, the impact of exercise on rate of weight loss was difficult to assess because of the limited details provided in most studies. Therefore, our predictive equation may not be so applicable to men and may underestimate the rate of the weight loss that can be achieved with dietary weight loss counseling. However, Williamson et al. reported that dietary adherence had a lesser predictive value on weight loss than behavioral adherence (4) and the factors included here tended to reflect behavioral rather than dietary adherence. In addition, our study included only published observations, which could have introduction some publication bias.
CONCLUSIONS
Finally, our data provide important information concerning participant and intervention characteristics that are associated with rate of weight loss. Specifically, one must take a person’s age, initial body weight, and study length into account when prescribing a caloric deficit for weight loss. Older adults with a greater body weight can be predicted to lose weight at a faster rate than younger, lower-weight adults, and this rate is diminished as the length of the study increases. Although we realize that each situation is unique in clinical practice, our results provide clinicians, dietary counselors, and weight loss researchers an empirical tool with which to estimate the rate of weight loss that can be expected given a fixed prescribed caloric deficit, study length, frequency of dietary counseling, and individual characteristics. In addition, agencies and groups developing guidelines may need to take several factors, such as population age and starting body weight, into consideration when formulating a suggested caloric deficit. This would lead to more realistic expectations regarding the obtained rate of weight loss.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Elissa Finkler, Masters’ Student, Institute of Human Nutrition, Columbia University, 636 W168th Street, PH1512, New York, NY 10032, Phone 212-305-4808
Steven B. Heymsfield, Executive Director, Clinical Research and Metabolism, Merck Research Laboratories, 126 East Lincoln Ave, Rahway, NJ 07065.
Marie-Pierre St-Onge, College of Physicians & Surgeons, Columbia University, Research Associate, St. Luke’s/Roosevelt Hospital Center, 1090 Amsterdam Avenue, suite 14D, New York, NY 10025, Phone 212-523-3564 Fax 212-523-3571, ms2554@columbia.edu.
References
- 1.Services U.S. Department of Health and Human Services. NIH Publication No 98-4083. Washington: 1998. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report. [Google Scholar]
- 2.Leibel RL, Rosenbaum M, Hirsch J. Changes in energy expenditure resulting from altered body weight. New Engl J Med. 1995;332:621–628. doi: 10.1056/NEJM199503093321001. [DOI] [PubMed] [Google Scholar]
- 3.Williamson DA, Anton SD, Han H, Champagne CM, Allen R, LeBlanc E, Ryan DH, McManus K, Laranjo N, Carey VJ, Loria CM, Bray GA, Sacks FM. Adherence is a multi-dimensional construct in the POUNDS LOST trial. J Behav Med. 2010;33:35–46. doi: 10.1007/s10865-009-9230-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Williamson DA, Anton SD, Han H, Champagne CM, Allen R, LeBlanc E, Ryan DH, Rood J, McManus K, Laranjo N, Carey VJ, Loria CM, Bray GA, Sacks FM. Early behavioral adherence predicts short and long-term weight loss in the POUNDS LOST study. J Behav Med. 2010;33:305–314. doi: 10.1007/s10865-010-9253-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fabricatore AN, Wadden TA, Moore RH, Butryn ML, Heymsfield SB, Nguyen AM. Predictors of attrition and weight loss success: Results from a randomized controlled trial. Behav Res Ther. 2009;47:685–691. doi: 10.1016/j.brat.2009.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Greenberg I, Stampfer MJ, Schwarzfuchs D, Shai I. Adherence and success in long-term weight loss diets: the dietary intervention randomized controlled trial (DIRECT) J Am Coll Nutr. 2009;28:159–168. doi: 10.1080/07315724.2009.10719767. [DOI] [PubMed] [Google Scholar]
- 7.Texeira PJ, Palmeira AL, Branco TL, Martins SS, Minderico CS, Barata JT, Silva AM, Sardinha LB. Who will lose weight? A reexamination of predictors of weight loss in women. Int J Behav Nutr Phys Act. 2004;1:12. doi: 10.1186/1479-5868-1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stern L, Iqbal N, Seshadri P, Chicano KL, Daily DA, McGrory J, Williams M, Gracely EJ, Samaha FF. The effects of low-carbohydrate versus conventional weight loss diets in severely obese adults: one-year follow-up of a randomized trial. Ann Intern Med. 2004;140:778–785. doi: 10.7326/0003-4819-140-10-200405180-00007. [DOI] [PubMed] [Google Scholar]
- 9.West JA, de Looy AE. Weight loss in overweight subjects following low-sucrose or sucrose-containing diets. Int J Obes Relat Metab Disord. 2001;25:1122–1128. doi: 10.1038/sj.ijo.0801652. [DOI] [PubMed] [Google Scholar]
- 10.Rice B, Janssen I, Hudson R, Ross R. Effects of aerobic or resistance exercise and/or diet on glucose tolerance and plasma insulin levels in obese men. Diabetes Care. 1999;22:684–691. doi: 10.2337/diacare.22.5.684. [DOI] [PubMed] [Google Scholar]
- 11.Albert SG, Mooradian AD. Low-dose recombinant human growth hormone as adjuvant therapy to lifestyle modifications in the management of obesity. J Clin Endocrinol Metab. 2004;89:695–701. doi: 10.1210/jc.2003-031264. [DOI] [PubMed] [Google Scholar]
- 12.Aude YW, Agatson A, Lopez-Jimenez F, Lieberman EH, Almon M, Hansen M, Rojas G, Lamas GA, Hennekens CH. The national cholesterol education program diet vs a diet lower in carbohydrates and higher in protein and monounsaturated fat. Arch Intern Med. 2004;164:2141–2146. doi: 10.1001/archinte.164.19.2141. [DOI] [PubMed] [Google Scholar]
- 13.Bowen J, Noakes M, Clifton P. Effect of calcium and diary foods in high protein, energy-restricted diets on weight loss and metabolic parameters in overweight adults. Int J Obes. 2005;29:957–965. doi: 10.1038/sj.ijo.0802895. [DOI] [PubMed] [Google Scholar]
- 14.Brehm BJ, Spang SE, Lattin BL, Seeley RJ, Daniels SR, D’Alessio DA. The role of energy expenditure in the differential weight loss in obese women on low-fat and low-carbohydrate diets. J Endocrinol Metab. 2005;90:1475–1482. doi: 10.1210/jc.2004-1540. [DOI] [PubMed] [Google Scholar]
- 15.Brook R, Bard R, Glazewski L, Kehrer C, Bodary PF, Eitzman DL, Rajagopalan S. Effect of short-term weight loss on the metabolic syndrome and conduit vascular endothelial function in overweight adults. Am J Cardiol. 2004;93:1012–1016. doi: 10.1016/j.amjcard.2004.01.009. [DOI] [PubMed] [Google Scholar]
- 16.Dengel DR, Pratley RE, Hagberg JM, Rogus EM, Goldberg AP. Distinct effects of aerobic exercise training and weight loss on glucose homeostasis in obese sedentary men. J Appl Physiol. 1996;81:318–325. doi: 10.1152/jappl.1996.81.1.318. [DOI] [PubMed] [Google Scholar]
- 17.Di Buono M, Hannah JS, Katzel LI, Jones PJ. Weight loss due to energy restriction suppresses cholesterol biosynthesis in overweight, mildly hypercholesterolemic men. J Nutr. 1999;129:1545–1548. doi: 10.1093/jn/129.8.1545. [DOI] [PubMed] [Google Scholar]
- 18.Drummond S, Dixon K, Griffin J, de Looy A. Weight loss on an energy-restricted, low fat, sugar-containing diet in overweight sedentary men. Int J Food Sci Nutr. 2004;55:279–290. doi: 10.1080/09637480412331290495. [DOI] [PubMed] [Google Scholar]
- 19.Evans EM, Saunders MJ, Spano MA, Arngrimsson SA, Lewis RD, Cureton KJ. Effects of diet and exercise on the density and composition of the fat-free mass in obese women. Med Sci Sports Exerc. 1999;31:1778–1787. doi: 10.1097/00005768-199912000-00013. [DOI] [PubMed] [Google Scholar]
- 20.Fogteloo AJ, Pijl H, Frolich M, McCamish M, Meinders AE. Effects of recombinant human leptin treatment as an adjunct of moderate energy restriction on body weight, resting energy expenditure and energy intake in obese humans. Diabetes Nutr Metab. 2003;16:109–114. [PubMed] [Google Scholar]
- 21.Fox AA, Thompson JL, Butterfield GE, Gylfadottir U, Moynihan S, Spiller G. Effects of diet and exercise on common cardiovascular disease risk factors in moderately obese older women. Am J Clin Nutr. 1996;63:225–233. doi: 10.1093/ajcn/63.2.225. [DOI] [PubMed] [Google Scholar]
- 22.Gadde KM, Franciscy DM, Wagner HR, 2nd, Krishnan KR. Zonisamide for weight loss in obese adults: a randomized controlled trial. JAMA. 2003;289:1820–1825. doi: 10.1001/jama.289.14.1820. [DOI] [PubMed] [Google Scholar]
- 23.Himeno E, Nishino K, Nakashima Y, Kuroiwa A, Ikeda M. Weight reduction regresses left ventricular mass regardless of blood pressure level in obese subjects. Am Heart J. 1996;131:313–319. doi: 10.1016/s0002-8703(96)90360-9. [DOI] [PubMed] [Google Scholar]
- 24.Janssen I, Ross R. Effects of sex on the change in visceral, subcutaneous adipose tissue and skeletal muscle in response to weight loss. Int J Obes Relat Metab Disord. 1999;23:1035–1046. doi: 10.1038/sj.ijo.0801038. [DOI] [PubMed] [Google Scholar]
- 25.Janssen I, Fortier A, Hudson R, Ross R. Effects of an energy-restrictive diet with or without exercise on abdominal fat, intermuscular fat, and metabolic risk factors in obese women. Diabetes Care. 2002;25:431–438. doi: 10.2337/diacare.25.3.431. [DOI] [PubMed] [Google Scholar]
- 26.Layman DK, Evans E, Baum J, Seyler JI, Erickson DJ, Boileau RA. Dietary protein and exercise have additive effects on body composition during weight loss in adult women. J Nutr. 2005;135:1903–1910. doi: 10.1093/jn/135.8.1903. [DOI] [PubMed] [Google Scholar]
- 27.Leslie WS, Lean ME, Baillie HM, Hankey CR. Weight management: a comparison of existing dietary approaches in a work-site setting. Int J Obes Relat Metab Disord. 2002;26:1469–1475. doi: 10.1038/sj.ijo.0802153. [DOI] [PubMed] [Google Scholar]
- 28.Lucas CP, Boldrin MN, Reaven GM. Effect of orlistat added to diet (30% of calories from fat) on plasma lipids, glucose, and insulin in obese patients with hypercholesterolemia. Am J Cardiol. 2003;91:961–964. doi: 10.1016/s0002-9149(03)00112-7. [DOI] [PubMed] [Google Scholar]
- 29.Luscombe-Marsh ND, Noakes M, Wittert GA, Keogh JB, Foster P, Clifton PM. Carbohydrate-restricted diets high in either monounsaturated fat or protein are equally effective at promoting fat loss and improving blood lipids. Am J Clin Nutr. 2005;81:762–772. doi: 10.1093/ajcn/81.4.762. [DOI] [PubMed] [Google Scholar]
- 30.Melanson KJ, Dell’Olio J, Carpenter MR, Angelopoulos TJ. Changes in multiple health outcomes at 12 and 24 weeks resulting from 12 weeks of exercise counseling with or without dietary counseling in obese adults. Nutrition. 2004;20:849–856. doi: 10.1016/j.nut.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 31.Mori TA, Bao DQ, Burke V, Puddey IB, Watts GF, Beilin LJ. Dietary fish as a major component of a weight-loss diet: effect on serum lipids, glucose, and insulin metabolism in overweight hypertensive subjects. Am J Clin Nutr. 1999;70:817–825. doi: 10.1093/ajcn/70.5.817. [DOI] [PubMed] [Google Scholar]
- 32.Nicklas BJ, Rogus EM, Goldberg AP. Exercise blunts declines in lipolysis and fat oxidation after dietary-induced weight loss in obese older women. Am J Physiol. 1997;273:E149–155. doi: 10.1152/ajpendo.1997.273.1.E149. [DOI] [PubMed] [Google Scholar]
- 33.Ross R, Pedwell H, Rissanen J. Effects of energy restriction and exercise on skeletal muscle and adipose tissue in women as measured by magnetic resonance imaging. Am J Clin Nutr. 1995;61:1179–1185. doi: 10.1093/ajcn/61.6.1179. [DOI] [PubMed] [Google Scholar]
- 34.Ross R, Dagnone D, Jones PJ, Smith H, Paddags A, Hudson R, Janssen I. Reduction in obesity and related comorbid conditions after diet-induced weight loss or exercise-induced weight loss in men. A randomized, controlled trial. Ann Intern Med. 2000;133:92–103. doi: 10.7326/0003-4819-133-2-200007180-00008. [DOI] [PubMed] [Google Scholar]
- 35.Ross R, Jassen I, Dawson J, Kungl AM, Kuk SL, Nguyen-Duy TB, Lee S, Kilpatrick K, Hudson R. Exercise-induced reduction in obesity and insulin resistance in women: a randomized controlled trial. Obes Res. 2004;12:789–798. doi: 10.1038/oby.2004.95. [DOI] [PubMed] [Google Scholar]
- 36.Shadid S, Jensen MD. Effects of pioglitazone versus diet and exercise on metabolic health and fat distribution in upper body obesity. Diabetes Care. 2003;26:3148–3152. doi: 10.2337/diacare.26.11.3148. [DOI] [PubMed] [Google Scholar]
- 37.Shapses SA, Heshka S, Heymsfield SB. Effect of calcium supplementation on weight and fat loss in women. J Clin Endocrinol Metab. 2004;89:632–637. doi: 10.1210/jc.2002-021136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stich V, Marion-Latard F, Hejnova J, viguerie N, Lefort C, Suljkovicova H, Langin D, Lafontan M, Berian M. Hypocaloric diet reduces exercise-induced alpha 2-adrenergic antilipolytic effect and alpha 2-adrenergic receptor mRNA levels in adipose tissue of obese women. J Clin Endocrinol Metab. 2002;87:1274–1281. doi: 10.1210/jcem.87.3.8349. [DOI] [PubMed] [Google Scholar]
- 39.St-Onge MP, Bosarge A. Weight-loss diet that includes consumption of medium-chain triacylglycerol oil leads to greater rate of weight and fat mass loss than does olive oil. Am J Clin Nutr. 2008;87:621–626. doi: 10.1093/ajcn/87.3.621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Thong FSL, Hudson R, Ross R, Janssen I, Graham TE. Plasma leptin in moderately obese men: independent effects of weight loss and aerobic exercise. Am J Physiol Endocrinol Metab. 2000;279:E307–E313. doi: 10.1152/ajpendo.2000.279.2.E307. [DOI] [PubMed] [Google Scholar]
- 41.Tiikkainen M, Bergholm R, Rissanen A, Aro A, Salminen I, Tamminen M, Teramo K, Yki-Jarvinen H. Effects of equal weight loss with orlistat and placebo on body fat and serum fatty acid composition and insulin resistance in obese women. Am J Clin Nutr. 2004;79:22–30. doi: 10.1093/ajcn/79.1.22. [DOI] [PubMed] [Google Scholar]
- 42.You T, Berman DM, Ryan AS, Nicklas BJ. Effects of hypocaloric diet and exercise training on inflammation and adipocyte lipolysis in obese postmenopausal women. J Clin Endocrinol Metab. 2004;89:1739–1746. doi: 10.1210/jc.2003-031310. [DOI] [PubMed] [Google Scholar]
- 43.Hansen D, Astrup A, Toubro S, Finer N, Kopelman P, Hilsted J, Rossner S, Saris W, Van Gaal L, James W, Goulder M STORM Study Group. Predictors of weight loss and maintenance during 2 years of treatment by sibutramine in obesity. Results from the European multi-centre STORM trial. Sibutramine Trial of Obesity Reduction and Maintenance. Int J Obes Relat Metab Disord. 2001;25:496–501. doi: 10.1038/sj.ijo.0801481. [DOI] [PubMed] [Google Scholar]
- 44.Pelchat ML. Food cravings in young and elderly adults. Appetite. 1997;28:103–113. doi: 10.1006/appe.1996.0063. [DOI] [PubMed] [Google Scholar]
- 45.Del Corral P, Chandler-Laney PC, Casazza K, Gower BA, Hunter GR. Effect of dietary adherence with or without exercise on weight loss: a mechanistic approach to a global problem. J Clin Endocrinol Metab. 2009;94:1602–1607. doi: 10.1210/jc.2008-1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Das SK, Moriguti JC, McCrory MA, Saltzman E, Mosunic C, Roberts SB. An underfeeding study in healthy men and women provides further evidence of impaired regulation of energy expenditure in old age. J Nutr. 2001;131:1833–1838. doi: 10.1093/jn/131.6.1833. [DOI] [PubMed] [Google Scholar]
- 47.Tsai A, Wadden T. The evolution of very-low-calorie diets: An update and meta-analysis. Obesity. 2006;14:1283–1293. doi: 10.1038/oby.2006.146. [DOI] [PubMed] [Google Scholar]
- 48.Raatz SK, Wimmer JK, Kwong CA, Sibley SD. Intensive diet instruction by registered dietitians improves weight-loss success. J Am Diet Assoc. 2008;108:110–113. doi: 10.1016/j.jada.2007.10.010. [DOI] [PubMed] [Google Scholar]
- 49.Brinkworth GD, Noakes M, Keogh JB, Luscombe ND, Wittert GA, Clifton P. Long-term effects of a high-protein, low-carbohydrate diet on weight control and cardiovascular risk markers in obese hyperinsulinemic subjects. Int J Obes. 2004;28:661–670. doi: 10.1038/sj.ijo.0802617. [DOI] [PubMed] [Google Scholar]
- 50.Sacks FM, Bray GA, Carey VJ, Smith SR, Ryan DH, Anton SD, McManus K, Champagne SM, Bishop LM, Laranjo N, Leboff MS, Rood JC, de Jonge L, Greenway FL, Loria CM, Obarzanek E, Williamson DA. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. N Engl J Med. 2009;360:859–873. doi: 10.1056/NEJMoa0804748. [DOI] [PMC free article] [PubMed] [Google Scholar]


