Diabetologists have been well aware since the seminal work of Himsworth (1) in the 1930s that type 2 (insulin resistant) and type 1 (insulin deficient) diabetes were distinct entities with different pathophysiological bases. They have been aware for some time that type 2 diabetes is associated with resistance of tissues such as muscle and liver to the biological effects of insulin. Furthermore, they knew that type 2 diabetes per se and insulin resistance could both predispose to an increased risk of premature coronary artery disease and particularly the premature occurrence of myocardial infarction (MI). By contrast, cardiologists came to embrace these concepts only slowly. It was not until approximately 1999 (2) that the major organizations that represented them consistently designated type 2 diabetes as a risk factor for coronary artery disease. It was against this backdrop that we and others sought to identify pathophysiological determinants that were both manifestations of type 2 diabetes and determinants of acceleration of coronary artery disease and precipitation of MI. Because type 2 diabetes is the predominant form, comprising more than 90% of patients with diabetes, and because its association with premature coronary artery disease is particularly well established, type 2 diabetes is the focus of this article and was the focus of the journey from the bench to the bedside that it addresses. Because we were graciously invited to describe our particular journey, we have emphasized references to our own work.
Potential impact of the fibrinolytic system on coronary artery disease
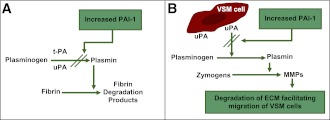
We and others have been interested in the fibrinolytic system in relation to the pathogenesis of coronary artery disease and precipitation of MI (3–5). Fibrinolysis in blood is mediated by activation of plasminogen activators, particularly tissue-type plasminogen activator (t-PA), that can be elaborated from endothelial cells in association with intravascular thrombosis (Fig. 1). t-PA is a serine protease. When it is elaborated into the blood it converts circulating plasminogen (present in high concentrations but biologically inert) to plasmin, a relatively nonspecific protease. Because both plasminogen and t-PA bind specifically to fibrin associated with nascent thrombi, the action of t-PA in blood is largely confined to clots, giving rise to what has been called clot-specific fibrinolysis (6). The fibrin-associated plasmin results in lysis of clots and preclusion of generation of otherwise induced macroscopic thrombi that can precipitate MI. A circulating protein called plasminogen activator inhibitor 1 (PAI-1) inhibits serine proteases such as t-PA, thereby attenuating the activity of the fibrinolytic system in blood. Thus, it inhibits t-PA associated with clots. Proteolysis that can be mediated by the relatively nonspecific proteinase, plasmin (Fig. 1) in other loci, can be inhibited by PAI-1 as well. One important such system operates in tissue. We have referred to it as the proteofibrinolytic system. It entails the conversion of plasminogen, present in high concentrations in the matrix, to plasmin when a plasminogen activator is elaborated. In tissues, the predominant plasminogen activator is urokinase. When it is expressed on cell surfaces such as those of vascular smooth muscle (VSM) cells, it converts matrix-associated plasminogen to plasmin. The result is activation of matrix metalloproteinases by cleavage of zymogens to form active moieties such as collagenase and stromolysin. A consequence is increased porosity of the matrix and facilitation of migration of diverse cell types through the matrix (5). Migration of VSM cells from the tunica media into the neointima is a hallmark of atherogenesis. The impact of increased expression of PAI-1 in tissue would therefore be expected to attenuate activation of matrix metalloproteinases, augmented porosity of the matrix, and migration of VSM cells from the tunica media into the tunica intima of evolving atheroma. Consequently, coronary atherosclerotic plaques that form under such circumstances are likely to be relatively devoid of VSM, lipid laden, and prone to rupture, thereby precipitating acute coronary syndromes. Plaques rich in VSM, though potentially obstructive, are known to be biologically quite stable, often over decades. By contrast, plaques relatively devoid of VSM, lipid laden, with thin fibrous caps are prone to rupture. Hence they are called vulnerable (to rupture) plaques. When they do rupture they can and often do precipitate acute coronary syndromes including MI and sudden cardiac death. Accordingly, overexpression of PAI-1 in the vessel that predisposes to development of vulnerable plaques predisposes also to acute coronary syndromes.
Figure 1.
Effects of increased concentrations of PAI-1. In blood (A) PAI-1 inhibits the action of t-PA, largely associated with clots, and thus attenuates the activity of the fibrinolytic system. In tissue (B), PAI-1attenuates activation of matrix metalloproteinases (MMPs) by plasmin generated from plasminogen by urokinase; plaques formed when PAI-1 is increased are likely to be prone to rupture. ECM, extracellular matrix; uPA, urokinase plasminogen activator.
Potential impact of increased concentrations of PAI-1 in blood associated with diabetes on coronary artery disease
It has been known for several decades that increased concentrations of PAI-1 in blood are associated with a predilection toward venous thrombosis and pulmonary embolism. Such an association is to be anticipated on the basis of inhibition by PAI-1 of lysis of nascent thrombi within the venous system. In addition it has been known for many years that increased concentrations of PAI-1 in blood (referred to in early work as simply activity of inhibitor of plasminogen activators) is a concomitant of the so-called metabolic syndrome and obesity as well as type 2 diabetes (7). A seminal article reporting results obtained in studies of a small number of patients was published by Hamsten et al. (3) in the late 1980s. They showed that young male survivors of MI when characterized 1 year later after the index infarction, at a time when the hemodynamic status of the patient was not overtly compromised, exhibited increased concentrations of an inhibitor of plasminogen activators (now known to be PAI-1) in blood compared with those in age-matched normal subjects. They speculated that the subjects with these increased concentrations of PAI-1 in blood had manifested elevated concentrations of PAI-1 in blood before the occurrence of MI. They concluded that the patients who sustained MI had been at increased risk of MI because of the presence of the increased concentrations of PAI-1 in blood. It was against this backdrop that we asked the question of whether patients with type 2 diabetes or obesity and presumed insulin resistance would exhibit increased concentrations of PAI-1 in blood (4). The results were compelling; in fact, the patients with type 2 diabetes or obesity compared with lean, otherwise normal subjects were characterized by markedly increased concentrations of PAI-1 in blood and the arterial wall. This led us to speculate that the increased expression of PAI-1 typical of type 2 diabetes and insulin resistance was a factor contributing to the increased incidence of MI and to premature coronary artery disease so typical of the condition.
Results of studies in vitro demonstrating direct effects of hormonal and metabolic factors on expression of PAI-1
An association between obesity, particularly in patients with type 2 diabetes, and elevated concentrations of PAI-1, led to studies in vitro evaluating the effects of insulin and precursors of insulin on expression of PAI-1. Insulin was shown to directly augment the expression of PAI-1 in a hepatocyte cell line, HepG2 (8). The effects of insulin were increased synergistically by the combination of insulin plus insulin-like growth factor 1 (9). In addition, precursors of insulin, both proinsulin and split products of proinsulin, concentrations of which are known to be elevated in blood from patients with type 2 diabetes, augment the expression of PAI-1 (10). Accordingly, insulin resistance increases the expression of PAI-1 by promoting compensatory hyperinsulinemia secondary to greater pancreatic β-cell release of insulin and its precursors, proinsulin and split proinsulin.
Results in mechanistic studies that we performed demonstrated that insulin reduced the rate of degradation of PAI-1 mRNA (11). Exertion of its effects through post translational modification sets the stage for interaction between agonists. Greater-than-additive effects are often seen when a process is stimulated by two agonists that have different mechanisms of action. Agents that increase transcription of PAI-1 mRNA can therefore amplify expression of PAI-1 protein to a greater extent in the presence of elevated concentrations of insulin.
In addition to the effects we and others observed in hepatocytes, pathophysiological concentrations of insulin increased the expression of PAI-1 by human arterial segments in vitro (12), an effect seen in segments that appeared to be grossly normal and those that exhibited atherosclerotic changes. The increased expression of PAI-1 was seen in segments harvested from subjects with or without preceding insulin-resistant states.
Augmented expression of PAI-1 was seen also in VSM cells in culture (13) in response to insulin and with cocultured endothelial cells and smooth muscle cells (12). Accordingly, studies in vitro with hepatocytes and with constituents of the vascular wall have demonstrated direct effects of insulin and its precursors on the expression of PAI-1.
Metabolic derangements including hyperglycemia and hypertriglyceridemia are a consequence of the relative or absolute deficiency of insulin. These metabolic abnormalities contribute to the elevated concentration of PAI-1 observed in vivo. Elevated concentrations of glucose increase expression of PAI-1 by both endothelial cells and VSM cells in vitro (14). Triglycerides and their constituents (fatty acids) increase the expression of PAI-1 in HepG2 cells (15). Moreover, the combination of elevated concentrations of both insulin and triglycerides exerts a synergistic increase in accumulation of PAI-1 in conditioned media of such cells (16).
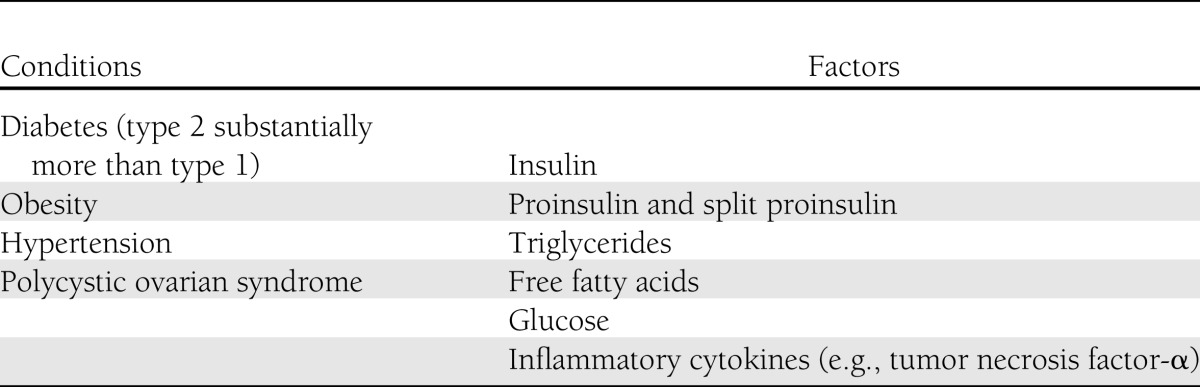
In aggregate, results of studies in vitro have demonstrated that the combination of hormonal abnormalities and metabolic derangements associated with insulin resistance and type 2 diabetes have direct effects on the expression of PAI-1 (Table 1). Synergism has been demonstrated and is consistent with the diverse mechanisms by which each of the agents augments the expression of PAI-1.
Table 1.
Conditions associated with and factors implicated in elevated expression of PAI-1
Results of studies in vivo linking diabetes and insulin resistance to increased expression of PAI-1
Elevated concentrations of PAI-1 have been observed consistently in blood from patients with diabetes, particularly those with type 2 diabetes (17). In addition, concentrations of PAI-1 are increased in blood from obese subjects, many of whom exhibit insulin resistance (7). Other conditions associated with insulin resistance such as hypertension (18) and polycystic ovarian syndrome (19) are associated with increased concentrations of PAI-1 in blood as well (Table 1). Consistent with direct effects observed in vitro, increased concentration and activity of PAI-1 correlate with elevated concentrations in blood of triglycerides and hyperinsulinemia (20). We found that increased concentrations in blood of PAI-1 impaired endogenous fibrinolytic system activity not only under basal conditions but also in response to a physiological challenge, i.e., transitory venous occlusion induced by inflation of an arm blood pressure cuff (4). Furthermore, we found that obese subjects with diabetes exhibited a threefold elevation of PAI-1 in blood compared with values in subjects without diabetes despite values of t-PA in blood that were virtually the same. These observations are consistent with constrained activity of the fibrinolytic system in the patients with diabetes. The observation of an impairment of fibrinolysis not only under basal conditions but also in response to physiologic stress indicates that the impairment is likely to shift the balance between fibrinolysis and thrombosis in vivo favoring thrombosis (4). It has been well established that impaired fibrinolysis predisposes to exaggerated and persistent thrombosis.
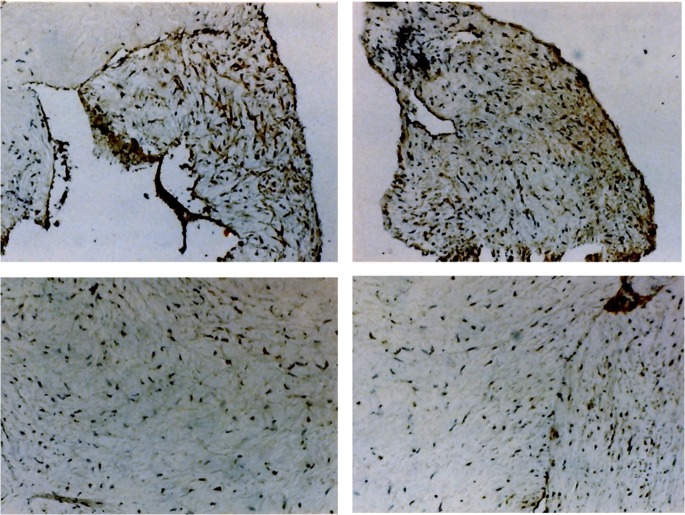
Expression of PAI-1 has been shown to be increased in tissues from patients with type 2 diabetes. Atherectomy specimens (excised segments of diseased coronary arteries) from patients with type 2 diabetes were shown to exhibit increased PAI-1 compared with that in comparably obstructive atheroma from patients without diabetes (Fig. 2) (21). Similarly, Pandolfi et al. (22) examined the internal mammary arteries from patients with type 2 diabetes and found a marked increase in active PAI-1. Adipose tissue expresses PAI-1 (23) and may be a particularly important source of PAI-1 in blood in obese subjects. Immunohistochemical examinations of retinas demonstrated that endothelial cells from patients with type 2 diabetes express significantly greater amounts of PAI-1 (24). Accordingly, greater concentrations in blood of PAI-1 reflect increased tissue expression of PAI-1 in patients with type 2 diabetes.
Figure 2.
Increased PAI-1 concentration is demonstrated by the intensity of brown immunohistochemical staining of specimens of diseased coronary arteries from representative patients with type 2 diabetes (top row) when compared with similar specimens from representative patients without diabetes (bottom row). Negative controls, obtained with the use of normal murine IgG instead of primary antibody against PAI-1, showed no detectable staining (data not shown). Magnification ×100. The figure is adapted with permission from Sobel et al. (21). (A high-quality digital representation of this figure is available in the online issue.)
The infusion of insulin and proinsulin in rabbits increased expression of PAI-1 (25). Similarly, acute hyperglycemia and hyperinsulinemia increased the concentration and activity of PAI-1 in blood from rats (26). The effect of insulin on metabolic derangements, particularly triglycerides and free fatty acids, could confound assessment of expression of PAI-1 in humans. However, localized intra-arterial infusion of insulin led to a marked increase in the concentration of PAI-1 in blood and induced impaired fibrinolysis (27). Furthermore, systemic infusion of a combination of insulin, glucose, and α-liposyn to simulate hypertriglyceridemia and insulin resistance was sufficient to increase expression of PAI-1 in healthy, normal human subjects (28). Results from these studies demonstrate that the combination of hormonal (hyperinsulinemia) and metabolic (hyperglycemia and hypertriglyceridemia) derangements typical of type 2 diabetes elevates the concentration of PAI-1 in blood.
Mechanisms by which increased expression of PAI-1 may influence outcomes in patients with coronary artery disease
As noted above, increased concentrations of PAI-1 in blood can lead to inhibition of fibrinolysis, facilitation of evolution of nascent thrombi to macroscopic thrombosis, and precipitation of MI. In addition, increased expression of PAI-1 within vessel walls can limit the migration of VSM cells. In general, migration of cells entails surface expression of urokinase and hence activation of the proteofibrinolytic system. Degradation of matrix follows facilitating migration. We speculated that increased PAI-1 in vessel walls would predispose to acceleration of atherosclerosis and development of plaques with specific characteristics rendering them vulnerable to rupture (29). Such plaques are characterized by a paucity of VSM (presumably resulting from inhibition of migration of VSM cells from the tunica media into the neointima). We hypothesized that as a result they would manifest increased deposition of lipid-laden cells and be relatively devoid of VSM. Plaques with these features are known to be prone to rupture in contrast to obstructive but biologically stable plaques populated heavily with VSM cells. Our hypothesis was spawned in part by observations made in the Bypass Angioplasty Revascularization Investigation 1 (BARI 1) trial. This trial was an investigation of patients with type 2 diabetes and clinically unstable coronary artery disease. The comparator groups were patients subjected to coronary artery bypass grafting (CABG) as opposed to the then-available percutaneous transluminal coronary angioplasty (PTCA). Observations in the BARI 1 trial showed that mortality over 5 years in the group subjected to CABG surgery was 9%. However, it was markedly augmented (fourfold greater) in those who had been treated initially with PTCA, despite successful initial restoration of coronary artery vascular patency with both interventions. The observations led to an issuance of a clinical alert by the National Institutes of Health pointing out that PTCA may be deleterious in patients with type 2 diabetes (30). We interpreted these results to indicate that iatrogenic trauma to the vasculature in patients with type 2 diabetes and insulin resistance would lead to accelerated evolution of plaques vulnerable to rupture and hence subsequently increased mortality consistent with the biological behavior of vasculature in which expression of PAI-1 was increased.
An additional factor requiring consideration with respect to the pathogenesis of coronary vascular disease per se in association with type 2 diabetes and insulin resistance is the impact on vessels subjected to injury, including the potent mitogenic iatrogenic injury induced by percutaneous coronary intervention (PCI). Such interventions are often followed by restenosis, a phenomenon more frequent and more pronounced in patients with diabetes, especially when drug eluting stents are not used. It is known that cellular proliferation and apoptosis are flip sides of the same coin. To determine whether PAI-1 could alter their balance and induce proliferation, we studied the effects of PAI-1 on the caspase system, known to be instrumental in a final common pathway leading to apoptosis (31). We found that PAI-1 inhibits this pathway. Accordingly, the increased expression of PAI-1 associated with diabetes can lead to augmented proliferation, diminished apoptosis, and hence accumulation of cells consistent with restenosis after PCI. In fact, by overexpressing PAI-1 in VSM cells and characterizing their response to chemotactic factors, we showed that proliferation (32) was, in fact, a consequence of the increased expression of PAI-1. This phenomenon may explain in part the well-recognized increased propensity of patients with type 2 diabetes who are subjected to PCI to develop restenosis in an accelerated fashion compared with that seen in patients without diabetes (33).
Agents that alter expression of PAI-1 in vivo
Therapeutic interventions that ameliorate metabolic derangements typical of diabetes, particularly those that do so without augmenting the concentration in blood of insulin, decrease expression of PAI-1. In patients with poorly controlled type 2 diabetes (HbA1c ∼10%), the elevation of PAI-1 in blood driven by hyperglycemia per se, hypertriglyceridemia, increased concentrations of free fatty acids, and increased compensatory hyperinsulinemia was profound (5- to 10-fold greater than normal). The elevation of PAI-1 was decreased comparably in response to administration of an insulin secretagogue, glipizide and with the insulin-sparing agent metformin (34). Metformin reduces hyperglycemia without stimulating pancreatic β-cell production or release of insulin. Results of other studies in patients with diabetes and other insulin-resistant states have demonstrated that metformin decreases the concentration of PAI-1 in blood (35). Nagi et al. (36) showed that metformin not only attenuates release of insulin but also attenuates release of precursors of insulin, namely proinsulin and proinsulin split products, each of which can stimulate expression of PAI-1.
Caloric restriction and exercise diminish insulin resistance, decrease hyperinsulinemia, improve glycemic control, and decrease concentrations of PAI-1 in blood (37). Thiazolidinediones such as troglitazone normalize metabolism and decrease the concentration in blood of insulin. These agents decrease PAI-1 in patients with type 2 diabetes (38) and subjects with insulin-resistant states (38,39) to the extent that they improve glycemic control and reduce hyperinsulinemia.
Agonists of glucagon-like peptide-1, such as liraglutide, inhibit induction of PAI-1 mediated by tumor necrosis factor-α or hyperglycemia (40). Agents that decrease concentrations of triglycerides in blood such as atorvastatin and gemfibrozil reduce concentrations of PAI-1 in blood from patients with insulin-resistant states (41).
Results in the BARI 2D trial
The Bypass Angioplasty Revascularization Investigation 2 Diabetes (BARI 2D) trial was undertaken to test two null hypotheses in patients with type 2 diabetes (42). The first was that the treatment of documented coronary stenosis in patients with clinically stable coronary artery disease would yield comparable results whether it entailed PCI or CABG coupled with optimal medical management compared with optimal medical management alone. The second was that treatment with pharmacological agents that were sensitizers to insulin (i.e., that diminished insulin resistance) would yield similar clinical outcomes (the incidence of fatal MI, stroke, and all-cause mortality) with respect to strategies predicated on augmentation of elaboration of insulin or administration of insulin itself. The overall results of the trial indicated that the incidences of the protocol delineated clinical outcomes were comparable in patients treated with coronary interventions or surgery coupled with optimal medical management compared with those in whom medical management alone was implemented and interventions initiated predicated on clinical manifestations of progression of the coronary artery disease (43). In addition, incidences of the same clinical outcomes were comparable in the trial as a whole (though not in several subsets) in patients treated with agents that increased sensitivity to insulin compared with those that increased availability of insulin. Our interest in participating in the BARI 2D trial was fanned by the likelihood that the results to be obtained could determine whether the insulin-sensitizing strategy compared with the insulin-providing strategy would result in differential effects on the proteofibrinolytic system.
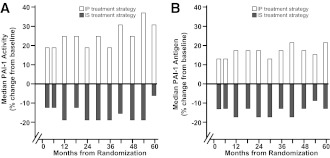
A total of 2,368 patients with type 2 diabetes and clinically stable angiographically documented coronary artery disease were randomized to treatment with one of the two strategies, insulin sensitization or insulin provision. They were followed for 5 years. Concentrations of PAI-1 in blood (antigen), PAI-1 activity, and concentrations of diverse other analytes were assayed in duplicate sequentially over the entire follow-up interval in 13 sets of blood samples over time. The results were rather startling (44). In contrast to the insulin-providing strategy, the insulin-sensitizing strategy led to the following (Fig. 3):
Lower concentrations of insulin in plasma despite wide, anticipated variance
Lower concentrations of PAI-1 antigen and
Lower concentrations of PAI-1 activity
Figure 3.
Comparison of insulin-sensitizing (IS) with insulin-providing (IP) treatment strategies in 2,368 patients with type 2 diabetes and clinically stable coronary artery disease for an overall treatment interval of 5 years in the BARI 2D trial (44). The insulin-sensitizing strategy led to lower concentrations of both PAI-1 activity (A) and antigen (B). Baseline values for PAI-1 activity and PAI-1 antigen (16 AU/mL and 23 ng/mL, respectively) were the same for both the insulin-sensitizing and insulin-providing treatment groups.
In addition, the results showed that the concentrations of C-reactive protein and of fibrinogen at all intervals after baseline were significantly lower in the patients treated with the insulin-sensitizing compared with the insulin-providing strategy.
These results indicated that insulin sensitization led to changes in biomarker profiles indicative of decreased insulin resistance and, as a consequence, a decrease in compensatory hyperinsulinemia. This decrease was associated with induction of an altered balance between thrombosis and fibrinolysis dependent on diminished expression of PAI-1 in patients treated with insulin sensitizers. The altered balance favored fibrinolysis. In addition, the biomarker profiles were consistent with a diminished intensity of a systemic inflammatory state in association with the use of insulin sensitizers. Both increased PAI-1 and an increased intensity of the systemic inflammatory state have been associated with acceleration of coronary atherosclerosis and an increased risk of MI. Accordingly, the results of the BARI 2D trial were consistent with results of preclinical observations showing that hyperinsulinemia associated with insulin resistance led to increased expression of PAI-1. Furthermore, they were consistent with the likelihood that insulin sensitization will protect patients with diabetes from acceleration of coronary atherosclerosis and precipitation of acute coronary syndromes including MI.
The lack of a difference in the incidence of the combined primary end point of overall mortality, fatal MI, and stroke in the BARI 2D trial in patients treated with an insulin-sensitizing compared with an insulin-providing strategy is not necessarily surprising. Factors responsible may include the fact that the overall event rate was quite low, as is common in many clinical trials in part because of patient selection and the intensity of monitoring and care. In addition, many factors other than the balance between fibrinolysis and thrombosis will affect outcomes in patients with diabetes. These include the severity of vascular disease at the time of entrance into a trial and the severity of metabolic derangements despite treatment. However, in the BARI 2D trial, there were strong trends consistent with favorable effects of insulin sensitization on outcomes with reduction of hazard ratios by 16% and with an improved prognosis in patients who underwent protocol-mandated investigator preselected CABG in those randomized to an intervention compared with optimal medical therapy alone. In this substratum, those patients who were treated with insulin sensitizing agents compared with those correspondingly randomized patients who underwent CABG but were treated with an insulin-provision strategy had a much more favorable outcome. In addition, the insulin-sensitizing strategy reduced the incidence of nonfatal, nonprocedurally related MI in the BARI 2D population as a whole (45).
Other considerations militate against a highly significant difference in clinical outcomes in a trial such as BARI 2D. Early studies of interventions such as diminution of hypertension showed favorable effects on clinical outcomes only when continued for many years in view of the lifelong nature of the evolution of atherosclerotic vascular disease. Thus, it is clear that delineation of statistically favorable effects on clinically significant outcomes per se may require a more prolonged interval of follow up in patients with type 2 diabetes treated with insulin-sensitizing compared with insulin-providing regimens than the 5-year interval of follow-up in BARI 2D.
Despite these caveats regarding clinical outcomes, the results in the BARI 2D trial with respect to the biomarker profiles are striking. Insulin sensitization favorably altered the balance between thrombosis and fibrinolysis reflected by concentrations of biomarkers such as fibrinopeptide A as a result of decreased constraints of fibrinolysis by PAI-1. Such a change in the balance between thrombosis and fibrinolysis is highly likely, in our view, when persistent for prolonged intervals, to translate into favorable effects on the progression of atherosclerosis, the incidence of MI, and hence clinical outcomes including mortality. Thus, the results in the BARI 2D trial constitute a key juncture in the journey from the bench to the bedside. They validate in patients with type 2 diabetes the existence of an intimate connection between insulin resistance and constrained fibrinolysis. They show that amelioration of insulin resistance favorably alters the balance between fibrinolysis and thrombosis favoring fibrinolysis over a 5-year interval in a large population of rigorously monitored patients with type 2 diabetes. They imply that significant clinical benefit may be achievable with treatment strategies in patients with type 2 diabetes over prolonged intervals that induce rigorous glycemic control with the lowest possible prevailing concentrations of insulin and its precursors.
Acknowledgments
No potential conflicts of interest relevant to this article were reported.
References
- 1.Himsworth HP. Management of Diabetes Mellitus. BMJ 1936;2:137–141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Greenland P, Alpert JS, Beller GA, et al. American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2010;122:e584–e636 [DOI] [PubMed] [Google Scholar]
- 3.Hamsten A, Wiman B, de Faire U, Blombäck M. Increased plasma levels of a rapid inhibitor of tissue plasminogen activator in young survivors of myocardial infarction. N Engl J Med 1985;313:1557–1563 [DOI] [PubMed] [Google Scholar]
- 4.McGill JB, Schneider DJ, Arfken CL, Lucore CL, Sobel BE. Factors responsible for impaired fibrinolysis in obese subjects and NIDDM patients. Diabetes 1994;43:104–109 [DOI] [PubMed] [Google Scholar]
- 5.Sobel BE. Increased plasminogen activator inhibitor-1 and vasculopathy. A reconcilable paradox. Circulation 1999;99:2496–2498 [DOI] [PubMed] [Google Scholar]
- 6.Van de Werf F, Ludbrook PA, Bergmann SR, et al. Coronary thrombolysis with tissue-type plasminogen activator in patients with evolving myocardial infarction. N Engl J Med 1984;310:609–613 [DOI] [PubMed] [Google Scholar]
- 7.Vague P, Juhan-Vague I, Aillaud MF, et al. Correlation between blood fibrinolytic activity, plasminogen activator inhibitor level, plasma insulin level, and relative body weight in normal and obese subjects. Metabolism 1986;35:250–253 [DOI] [PubMed] [Google Scholar]
- 8.Alessi MC, Juhan-Vague I, Kooistra T, Declerck PJ, Collen D. Insulin stimulates the synthesis of plasminogen activator inhibitor 1 by the human hepatocellular cell line Hep G2. Thromb Haemost 1988;60:491–494 [PubMed] [Google Scholar]
- 9.Schneider DJ, Sobel BE. Augmentation of synthesis of plasminogen activator inhibitor type 1 by insulin and insulin-like growth factor type I: implications for vascular disease in hyperinsulinemic states. Proc Natl Acad Sci USA 1991;88:9959–9963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nordt TK, Schneider DJ, Sobel BE. Augmentation of the synthesis of plasminogen activator inhibitor type-1 by precursors of insulin. A potential risk factor for vascular disease. Circulation 1994;89:321–330 [DOI] [PubMed] [Google Scholar]
- 11.Fattal PG, Schneider DJ, Sobel BE, Billadello JJ. Post-transcriptional regulation of expression of plasminogen activator inhibitor type 1 mRNA by insulin and insulin-like growth factor 1. J Biol Chem 1992;267:12412–12415 [PubMed] [Google Scholar]
- 12.Schneider DJ, Absher PM, Ricci MA. Dependence of augmentation of arterial endothelial cell expression of plasminogen activator inhibitor type 1 by insulin on soluble factors released from vascular smooth muscle cells. Circulation 1997;96:2868–2876 [DOI] [PubMed] [Google Scholar]
- 13.Pandolfi A, Iacoviello L, Capani F, Vitacolonna E, Donati MB, Consoli A. Glucose and insulin independently reduce the fibrinolytic potential of human vascular smooth muscle cells in culture. Diabetologia 1996;39:1425–1431 [DOI] [PubMed] [Google Scholar]
- 14.Chen YQ, Su M, Walia RR, Hao Q, Covington JW, Vaughan DE. Sp1 sites mediate activation of the plasminogen activator inhibitor-1 promoter by glucose in vascular smooth muscle cells. J Biol Chem 1998;273:8225–8231 [DOI] [PubMed] [Google Scholar]
- 15.Chen Y, Billadello JJ, Schneider DJ. Identification and localization of a fatty acid response region in the human plasminogen activator inhibitor-1 gene. Arterioscler Thromb Vasc Biol 2000;20:2696–2701 [DOI] [PubMed] [Google Scholar]
- 16.Schneider DJ, Sobel BE. Synergistic augmentation of expression of plasminogen activator inhibitor type-1 induced by insulin, very-low-density lipoproteins, and fatty acids. Coron Artery Dis 1996;7:813–817 [DOI] [PubMed] [Google Scholar]
- 17.Auwerx J, Bouillon R, Collen D, Geboers J. Tissue-type plasminogen activator antigen and plasminogen activator inhibitor in diabetes mellitus. Arteriosclerosis 1988;8:68–72 [DOI] [PubMed] [Google Scholar]
- 18.Jansson JH, Johansson B, Boman K, Nilsson TK. Hypo-fibrinolysis in patients with hypertension and elevated cholesterol. J Intern Med 1991;229:309–316 [DOI] [PubMed] [Google Scholar]
- 19.Sampson M, Kong C, Patel A, Unwin R, Jacobs HS. Ambulatory blood pressure profiles and plasminogen activator inhibitor (PAI-1) activity in lean women with and without the polycystic ovary syndrome. Clin Endocrinol (Oxf) 1996;45:623–629 [DOI] [PubMed] [Google Scholar]
- 20.Juhan-Vague I, Vague P, Alessi MC, et al. Relationships between plasma insulin triglyceride, body mass index, and plasminogen activator inhibitor 1. Diabete Metab 1987;13:331–336 [PubMed] [Google Scholar]
- 21.Sobel BE, Woodcock-Mitchell J, Schneider DJ, Holt RE, Marutsuka K, Gold H. Increased plasminogen activator inhibitor type 1 in coronary artery atherectomy specimens from type 2 diabetic compared with nondiabetic patients: a potential factor predisposing to thrombosis and its persistence. Circulation 1998;97:2213–2221 [DOI] [PubMed] [Google Scholar]
- 22.Pandolfi A, Cetrullo D, Polishuck R, et al. Plasminogen activator inhibitor type 1 is increased in the arterial wall of type II diabetic subjects. Arterioscler Thromb Vasc Biol 2001;21:1378–1382 [DOI] [PubMed] [Google Scholar]
- 23.Alessi MC, Peiretti F, Morange P, Henry M, Nalbone G, Juhan-Vague I. Production of plasminogen activator inhibitor 1 by human adipose tissue: possible link between visceral fat accumulation and vascular disease. Diabetes 1997;46:860–867 [DOI] [PubMed] [Google Scholar]
- 24.Grant MB, Ellis EA, Caballero S, Mames RN. Plasminogen activator inhibitor-1 overexpression in nonproliferative diabetic retinopathy. Exp Eye Res 1996;63:233–244 [DOI] [PubMed] [Google Scholar]
- 25.Nordt TK, Sawa H, Fujii S, Sobel BE. Induction of plasminogen activator inhibitor type-1 (PAI-1) by proinsulin and insulin in vivo. Circulation 1995;91:764–770 [DOI] [PubMed] [Google Scholar]
- 26.Pandolfi A, Giaccari A, Cilli C, et al. Acute hyperglycemia and acute hyperinsulinemia decrease plasma fibrinolytic activity and increase plasminogen activator inhibitor type 1 in the rat. Acta Diabetol 2001;38:71–76 [DOI] [PubMed] [Google Scholar]
- 27.Carmassi F, Morale M, Ferrini L, et al. Local insulin infusion stimulates expression of plasminogen activator inhibitor-1 and tissue-type plasminogen activator in normal subjects. Am J Med 1999;107:344–350 [DOI] [PubMed] [Google Scholar]
- 28.Calles-Escandon J, Mirza SA, Sobel BE, Schneider DJ. Induction of hyperinsulinemia combined with hyperglycemia and hypertriglyceridemia increases plasminogen activator inhibitor 1 in blood in normal human subjects. Diabetes 1998;47:290–293 [DOI] [PubMed] [Google Scholar]
- 29.Schneider DJ, Hayes M, Wadsworth M, et al. Attenuation of neointimal vascular smooth muscle cellularity in atheroma by plasminogen activator inhibitor type 1 (PAI-1). J Histochem Cytochem 2004;52:1091–1099 [DOI] [PubMed] [Google Scholar]
- 30.Sobel BE. Potentiation of vasculopathy by insulin: implications from an NHLBI clinical alert. Circulation 1996;93:1613–1615 [DOI] [PubMed] [Google Scholar]
- 31.Schneider DJ, Chen Y, Sobel BE. The effect of plasminogen activator inhibitor type 1 on apoptosis. Thromb Haemost 2008;100:1037–1040 [PubMed] [Google Scholar]
- 32.Chen Y, Budd RC, Kelm RJ, Jr, Sobel BE, Schneider DJ. Augmentation of proliferation of vascular smooth muscle cells by plasminogen activator inhibitor type 1. Arterioscler Thromb Vasc Biol 2006;26:1777–1783 [DOI] [PubMed] [Google Scholar]
- 33.Van Belle E, Ketelers R, Bauters C, et al. Patency of percutaneous transluminal coronary angioplasty sites at 6-month angiographic follow-up: A key determinant of survival in diabetics after coronary balloon angioplasty. Circulation 2001;103:1218–1224 [DOI] [PubMed] [Google Scholar]
- 34.Cefalu WT, Schneider DJ, Carlson HE, et al. Effect of combination glipizide GITS/metformin on fibrinolytic and metabolic parameters in poorly controlled type 2 diabetic subjects. Diabetes Care 2002;25:2123–2128 [DOI] [PubMed] [Google Scholar]
- 35.Grant PJ. The effects of metformin on the fibrinolytic system in diabetic and non-diabetic subjects. Diabete Metab 1991;17:168–173 [PubMed] [Google Scholar]
- 36.Nagi DK, Ali VM, Yudkin JS. Effect of metformin on intact proinsulin and des 31,32 proinsulin concentrations in subjects with non-insulin-dependent (type 2) diabetes mellitus. Diabet Med 1996;13:753–757 [DOI] [PubMed] [Google Scholar]
- 37.Belalcazar LM, Ballantyne CM, Lang W, et al. Look Action for Health in Diabetes Research Group Metabolic factors, adipose tissue, and plasminogen activator inhibitor-1 levels in type 2 diabetes: findings from the look AHEAD study. Arterioscler Thromb Vasc Biol 2011;31:1689–1695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kruszynska YT, Yu JG, Olefsky JM, Sobel BE. Effects of troglitazone on blood concentrations of plasminogen activator inhibitor 1 in patients with type 2 diabetes and in lean and obese normal subjects. Diabetes 2000;49:633–639 [DOI] [PubMed] [Google Scholar]
- 39.Ehrmann DA, Schneider DJ, Sobel BE, et al. Troglitazone improves defects in insulin action, insulin secretion, ovarian steroidogenesis, and fibrinolysis in women with polycystic ovary syndrome. J Clin Endocrinol Metab 1997;82:2108–2116 [DOI] [PubMed] [Google Scholar]
- 40.Liu H, Dear AE, Knudsen LB, Simpson RW. A long-acting glucagon-like peptide-1 analogue attenuates induction of plasminogen activator inhibitor type-1 and vascular adhesion molecules. J Endocrinol 2009;201:59–66 [DOI] [PubMed] [Google Scholar]
- 41.Krysiak R, Gdula-Dymek A, Bachowski R, Okopien B. Pleiotropic effects of atorvastatin and fenofibrate in metabolic syndrome and different types of pre-diabetes. Diabetes Care 2010;33:2266–2270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Brooks MM, Frye RL, Genuth S, et al. Bypass Angioplasty Revascularization Investigation 2 Diabetes (BARI 2D) Trial Investigators Hypotheses, design, and methods for the Bypass Angioplasty Revascularization Investigation 2 Diabetes (BARI 2D) Trial. Am J Cardiol 2006;97(12A):9G–19G [DOI] [PubMed] [Google Scholar]
- 43.Frye RL, August P, Brooks MM, et al. BARI 2D Study Group A randomized trial of therapies for type 2 diabetes and coronary artery disease. N Engl J Med 2009;360:2503–2515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sobel BE, Hardison RM, Genuth S, et al. BARI 2D Investigators Profibrinolytic, antithrombotic, and antiinflammatory effects of an insulin-sensitizing strategy in patients in the Bypass Angioplasty Revascularization Investigation 2 Diabetes (BARI 2D) trial. Circulation 2011;124:695–703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chaitman BR, Hardison RM, Adler D, et al. Bypass Angioplasty Revascularization Investigation 2 Diabetes (BARI 2D) Study Group The Bypass Angioplasty Revascularization Investigation 2 Diabetes randomized trial of different treatment strategies in type 2 diabetes mellitus with stable ischemic heart disease: impact of treatment strategy on cardiac mortality and myocardial infarction. Circulation 2009;120:2529–2540 [DOI] [PMC free article] [PubMed] [Google Scholar]