Abstract
Chronic heart failure is accompanied by anorexia and increased release of B-type natriuretic peptide (BNP) from ventricular cardiomyocytes. The pathophysiological mechanisms linking heart failure and appetite regulation remain unknown. In this study, we investigated the impact of intravenous BNP administration on appetite-regulating hormones and subjective ratings of hunger and satiety in 10 healthy volunteers. Participants received in a randomized, placebo-controlled, crossover, single-blinded study (subject) placebo once and 3.0 pmol/kg/min human BNP-32 once administered as a continuous infusion during 4 h. Circulating concentrations of appetite-regulating peptides were measured hourly. Subjective ratings of hunger and satiety were evaluated by visual analog scales. BNP inhibited the fasting-induced increase in total and acylated ghrelin concentrations over time (P = 0.043 and P = 0.038, respectively). In addition, BNP decreased the subjective rating of hunger (P = 0.009) and increased the feeling of satiety (P = 0.012) when compared with placebo. There were no significant changes in circulating peptide YY, glucagon-like peptide 1, oxyntomodulin, pancreatic polypeptide, leptin, and adiponectin concentrations. In summary, our results demonstrate that BNP exerts anorectic effects and reduces ghrelin concentrations in men. These data, taken together with the known cardiovascular properties of ghrelin, support the existence of a heart–gut–brain axis, which could be therapeutically targeted in patients with heart failure and obesity.
The control of appetite and energy balance is tightly regulated by a complex neuronal network in the brainstem and hypothalamus that receives information from the periphery via nutrients, hormones, and afferent nervous fibers (1). Important members of this network are the gut-derived hormones ghrelin and peptide YY (PYY), which modulate not only appetite in the short term, but also energy balance in the long term (2–4).
Appetite and BMI decrease progressively in patients with heart failure, and cachexia accompanies end-stage disease (5). The changes in body composition have prognostic importance, as lower waist circumference and BMI are associated with a worse outcome in patients with heart failure (6).
The biochemical diagnosis and prognosis of heart failure is strongly dependent on the circulating concentrations of B-type natriuretic peptide (BNP), which is secreted from ventricular myocytes in response to cell stretching and stress and reflects the degree of cardiac dysfunction (7–9). BNP has hormone properties, binds to transmembrane receptors, and induces natriuresis, diuresis, and vasodilatation, thereby reducing the preload (7). Recent studies corroborate an association between BNP concentrations and appetite regulation. BNP transgenic mice are protected against diet-induced obesity and insulin resistance (10). Cross-sectional studies reveal an inverse correlation between circulating BNP and BMI not only in patients with heart failure, but also in healthy people (11). Heart failure is associated with resistance to the orexigenic hormone ghrelin (12), and ghrelin administration improves both left ventricular function and muscle wasting (13,14).
In this study, we investigated the acute effect of intravenous BNP administration on appetite-regulating hormones and on subjective ratings of hunger and satiety in a placebo-controlled, crossover study conducted in healthy men.
RESEARCH DESIGN AND METHODS
Study subjects.
The protocol was approved by the institutional review board, registered at http://www.clinicaltrials.gov (NCT01375153), and performed according to the Declaration of Helsinki. Ten healthy male subjects were recruited in the study after prior oral and written informed consent. On the screening day, a careful medical history was taken. Inclusion criteria were normal BMI, no history of concomitant or chronic disease, no smoking, no drug and alcohol abuse, and no medication, including nonprescription drugs. A thorough medical examination and biochemical tests for glucose, HbA1c, BNP, electrolytes, C-reactive protein, lipid values, and renal, liver, and thyroid function were performed before enrollment in the study. Blood pressure was measured in supine and sitting positions. An electrocardiogram was recorded. Only subjects having all values within the normal range were included in the study. They were aged between 21 and 29 years and had BMIs ranging from 22–24.6 kg/m2.
Study protocol.
This was a randomized, placebo-controlled, single-blind (subject), crossover study. All subjects were examined in two sessions, scheduled at least 3 weeks apart, at which they received placebo once and BNP once. At both sessions, participants came to the clinical trials center at 8:00 a.m. after having fasted overnight and remained fasted till the end of the study. To avoid BNP effects on blood pressure, all participants were confined to bed rest and remained in a laying position throughout the study period (15).
Cannulas were placed in the antecubital veins of the right and left arm for infusions and blood sampling, respectively. After venous cannulation, the subjects relaxed for ∼20 min. Then, 3 pmol/kg/min active BNP (BNP-32, containing amino acids 77–108 of the preproBNP; obtained from American Peptide Company, Sunnyvale, CA) or placebo (0.9% NaCl) was administered as a continuous intravenous infusion during 4 h (time point 0–4 h). Blood samples were obtained at time points −5 min and 0, 1, 2, 3, and 4 h. The subjective ratings of hunger and satiety were marked on a 10-cm visual analog scale (VAS) half-hourly during the 4 study h.
Primary outcome measurements were circulating ghrelin, acylated ghrelin, PYY, and adiponectin concentrations. Secondary outcome measurements were the ratings of hunger and satiety in the VAS and plasma glucagon-like peptide 1 (GLP-1), oxyntomodulin, pancreatic polypeptide (PP), and leptin concentrations.
Blood sampling and assays.
Blood samples for the measurement of ghrelin, PYY, oxyntomodulin, PP, leptin, and adiponectin were obtained in collection tubes containing EDTA. Blood samples for the measurement of BNP were obtained in collection tubes containing heparin. Blood samples for the measurement of GLP-1 were obtained in collection tubes containing EDTA and immediately supplemented with DPP IV inhibitor (Millipore, Billerica, MA). All of these samples were immediately cooled on ice, centrifuged at 3,000 rpm for 10 min, and then frozen at −20°C. Samples for the measurement of acylated ghrelin were withdrawn in EDTA supplemented with the protease inhibitor Trasylol (Sigma-Aldrich), centrifuged at 3,000 rpm for 10 min, acidified with 1 N HCl (1/10), and frozen at −20°C. Assays were performed at the very end of the study in duplicates, with samples from both study days of each individual analyzed within one assay.
Total ghrelin concentrations were measured using a commercially available radioimmunoassay (RIA) kit with inter- and intra-assay coefficients of variation being 5 and 8%, respectively (Bachem-Peninsula Laboratories, San Carlos, CA). Acylated ghrelin was determined using a commercially available sandwich ELISA kit with no cross-reactivity with des-octanoyl-ghrelin (Millipore). The inter- and intra-assay coefficients were 7.5–12 and 0.9–7.5%, respectively. Plasma PYY3–36 concentrations were quantified using an RIA kit (Millipore) with inter- and intra-assay variations of 8.2 and 9%, respectively. Active GLP-1 was determined using an ELISA kit (Millipore) with inter- and intra-assay variations being 6–10%. Oxyntomodulin concentrations were quantified with an RIA kit (Phoenix Pharmaceuticals, Burlingame, CA). PP was quantified using a sandwich ELISA (Millipore) with intra-assay coefficients of variation being 3.3–5% and interassay coefficients of variation being 5–9.8%. Leptin and adiponectin were measured with RIA kits (Millipore), both having inter- and intra-assay variations of 5–8%. BNP concentrations were measured using the commercially available ARCHITECT BNP immunoassay on the ARCHITECT System (Abbott Laboratories, Vienna, Austria).
Statistical evaluation.
Data were analyzed using the statistical software SPSS release 12.0.1 (SPSS, Chicago, IL). Subjects’ characteristics are expressed as mean and range or mean ± SE. The values of primary and secondary outcome parameters are expressed as mean ± SE. The significance of differences between the 2 study days was assessed by repeated-measurements ANOVA (RM-ANOVA) with the interaction between time and treatment (time * treatment) being the term of interest. A P value <0.05 was considered statistically significant. Post hoc paired t tests for comparing the intervention-induced changes at each time point were performed only when RM-ANOVA revealed significant results.
RESULTS
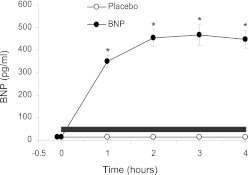
The intravenous infusion of 3 pmol/kg/min BNP significantly increased plasma BNP concentrations, which remained constant between 400 and 500 pg/mL during the last 2 h of the study (Fig. 1). In accordance with previous reports, BNP did not modulate blood pressure in the supine position (15).
FIG. 1.
Changes in circulating BNP concentrations. BNP administered as a continuous intravenous infusion of 3 pmol/kg/min. Horizontal black bar shows infusion duration. Data are presented as mean ± SEM. ●, 3 pmol/kg/min BNP; ○, placebo; *P < 0.05.
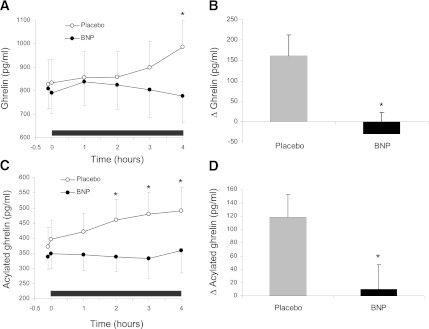
BNP infusion decreased total ghrelin concentrations (P = 0.043, RM-ANOVA), reaching 778 ± 113 pg/mL in BNP sessions as compared with 988 ± 122 pg/mL during placebo sessions at time point 4 h (P = 0.012, post hoc t tests) (Fig. 2A and B). In parallel, BNP reduced the increase in acylated ghrelin concentrations during fasting (P = 0.038, RM-ANOVA), with significant differences observed at time points 2, 3, and 4 h (P = 0.014, P = 0.002, and P = 0.029, respectively, post hoc t tests) (Fig. 2C and D). However, BNP did not significantly modify plasma PYY3–36 (P = 0.716), active GLP-1 (P = 0.265), oxyntomodulin (P = 0.419), pancreatic polypeptide (P = 0.577), leptin (P = 0.533), and adiponectin (P = 0.180) concentrations (Fig. 3A–F).
FIG. 2.
Effects of BNP on acylated and total ghrelin concentrations. A: Profile of changes in plasma ghrelin concentrations. B: Differences between ghrelin concentrations at baseline and time point 4 h. C: Profile of changes in acylated ghrelin concentrations. D: Differences between acylated ghrelin concentrations at baseline and at time point 4 h. Data are presented as mean ± SEM. Horizontal black bar shows infusion duration. ●, 3 pmol/kg/min BNP; ○, placebo; *P < 0.05.
FIG. 3.
Effects of BNP on gut peptides and adipokines. BNP-induced changes in circulating PYY3–36 (A), GLP-1 (B), oxyntomodulin (C), PP (D), leptin (E), and adiponectin concentrations (F). Data are presented as mean ± SEM. Horizontal black bar shows infusion duration. ●, 3 pmol/kg/min BNP; ○, placebo.
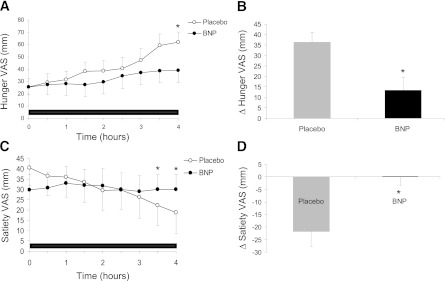
The increase in the subjective rating of hunger with time during fasting was reduced during the BNP infusion (P = 0.009 RM-ANOVA) (Fig. 4A). At time point 4 h, the changes in scores of hunger VAS versus baseline were 36.2 ± 4.9 mm in placebo sessions and 13.4 ± 6.1 mm in BNP sessions (P = 0.024) (Fig. 4B). In parallel, BNP infusion abolished the decrease in the subjective rating of satiety during fasting (P = 0.012 RM-ANOVA), achieving a decrease of 21.7 ± 5.9 mm in placebo sessions versus an increase of 0.3 ± 3.6 mm in BNP sessions (P = 0.018) (Fig. 4C and D).
FIG. 4.
Effects of BNP on subjective ratings of hunger and satiety, as measured by VAS. Scores are depicted as change from the 0 value (mm). A: Profile of hunger VAS values. B: Differences between hunger VAS values at baseline and time point 4 h. C: Profile of satiety VAS values. D: Differences between satiety VAS values at baseline and time point 4 h. Data are presented as mean ± SEM. Horizontal black bar shows infusion duration. ●, 3 pmol/kg/min BNP; ○, placebo; *P < 0.05.
DISCUSSION
In this study, we report that the cardiac hormone BNP modulates appetite via reducing the circulating concentrations of the appetite-stimulating hormone ghrelin, thereby decreasing hunger and inducing the feeling of satiety. These anorexigenic properties of BNP suggest the existence of a pathway originating from the heart, linking heart dysfunction and appetite regulation.
The gut–brain axis with its main hormone ghrelin is one of the key players controlling appetite regulation, as it not only transmits information on the feeding status but also coordinates information coming from other hormones and organs, adapting appetite in response to stressors (3,16,17). Ghrelin is a potent orexigenic peptide; therefore, the BNP-induced reduction in the ratings of hunger and increase in the feeling of satiety might be, at least in part, mediated by the decrease in circulating ghrelin concentrations (2). Nevertheless, BNP receptors are widely spread throughout the brain, and potential direct effects of BNP on appetite regulating centers cannot be excluded (18).
Interestingly, BNP administration did not change the concentrations of the anorexigenic gut hormone PYY. The secretion of ghrelin and PYY in response to food intake is mediated via the cholinergic system. Pharmacological modulation of the cholinergic system alters both ghrelin and PYY secretion during fasting (19). The fact that BNP administration affects only ghrelin and not PYY speaks against a possible mediation of BNP effects via the cholinergic system. This hypothesis is supported by a physiological study in eels revealing that BNP effects are dependent on β-adrenergic blockade but not on cholinergic blockade (20). The fact that BNP does not influence GLP-1, oxyntomodulin, and PP is somewhat expected in this fasting study, as all these peptides are mainly modulated in response to food intake.
It is important to emphasize that this trial investigated only the acute effects of BNP administration in healthy men. The continuous infusion of BNP led to plasma BNP concentrations between 400 and 500 pg/mL. These concentrations are in agreement with other studies using similar infusion protocols and similar to the values found in patients with heart failure (21). Patients with heart failure–associated anorexia have increased ghrelin concentrations compared with healthy people, as expected from the strong negative correlation between ghrelin and BMI in all studied populations (2,22). We suggest that the continuous BNP oversecretion in patients with heart failure could thus impede a further increase in ghrelin. This hypothesis is supported by the fact that patients with cardiac cachexia, despite having increased ghrelin concentrations, significantly benefit from the pharmacological administration of ghrelin (23). In addition to increasing appetite, ghrelin displays also positive cardiovascular properties, such as the stimulation of left ventricular function, vasodilatation, and anti-inflammatory effects (13,14,17).
Several studies have addressed the positive correlation between circulating concentrations of BNP and adiponectin not only in patients with heart failure but also in healthy people (24). BNP enhances adiponectin mRNA expression in human adipocytes in primary culture (25). In contrast to these in vitro effects, we show that systemic BNP administration does not significantly change adiponectin concentrations. Taken together, these results demonstrate that the relationship between BNP and adiponectin is not just a direct one.
Strength of the study is the use of an adequate randomized crossover protocol for investigating novel effects of BNP on appetite-regulating hormones, hunger, and satiety, independently from effects on blood pressure. Study weaknesses are the single-blind design and the lack of a meal intake, which was conditioned by the fact that subjects had to remain in supine position. Therefore, we cannot exclude BNP effects on the meal-induced changes in GLP-1, oxyntomodulin, and PP.
In summary, in this study, we demonstrate that intravenous administration of BNP reduces circulating ghrelin concentrations, decreases hunger, and increases the feeling of satiety in healthy people. These data, taken together with the known cardioprotective effects of ghrelin, support the existence of a bidirectional heart–gut crosstalk, which might play a central role in adapting appetite and energy homeostasis to the degree of heart dysfunction. Heart–gut signaling links two vital human functions and might be further investigated as a potential therapeutical target not only in heart failure, but also in obesity and eating disorders.
ACKNOWLEDGMENTS
This study was supported by Research Grant 13583 of the Austrian National Bank (to M.C.).
No potential conflicts of interest relevant to this article were reported.
G.V., B.H., A.L., and M.C. designed the study. G.V., G.G., M.R., E.E., H.E., B.D., and T.M. performed research. G.V., A.L., and M.C. analyzed the data. G.V. wrote the manuscript. G.V., G.G., M.R., B.H., E.E., H.E., B.D., T.M., A.L., and M.C. approved the final version of the manuscript. M.C. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Parts of this study were presented in abstract form at the 94th Annual Meeting of The Endocrine Society, Boston, Massachusetts, 4–7 June 2011.
The authors thank A. Hofer, L.-I. Ionasz, and E. Nowotny (Division of Endocrinology and Metabolism, Medical University of Vienna, Vienna, Austria) for excellent technical assistance.
Footnotes
Clinical trial reg. no. NCT01375153, clinicaltrials.gov.
See accompanying commentary, p. 2403.
REFERENCES
- 1.Coll AP, Farooqi IS, O’Rahilly S. The hormonal control of food intake. Cell 2007;129:251–262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Murphy KG, Dhillo WS, Bloom SR. Gut peptides in the regulation of food intake and energy homeostasis. Endocr Rev 2006;27:719–727 [DOI] [PubMed] [Google Scholar]
- 3.Castañeda TR, Tong J, Datta R, Culler M, Tschöp MH. Ghrelin in the regulation of body weight and metabolism. Front Neuroendocrinol 2010;31:44–60 [DOI] [PubMed] [Google Scholar]
- 4.Batterham RL, ffytche DH, Rosenthal JM, et al. PYY modulation of cortical and hypothalamic brain areas predicts feeding behaviour in humans. Nature 2007;450:106–109 [DOI] [PubMed] [Google Scholar]
- 5.von Haehling S, Lainscak M, Springer J, Anker SD. Cardiac cachexia: a systematic overview. Pharmacol Ther 2009;121:227–252 [DOI] [PubMed] [Google Scholar]
- 6.Curtis JP, Selter JG, Wang Y, et al. The obesity paradox: body mass index and outcomes in patients with heart failure. Arch Intern Med 2005;165:55–61 [DOI] [PubMed] [Google Scholar]
- 7.Clerico A, Giannoni A, Vittorini S, Passino C. Thirty years of the heart as an endocrine organ: physiological role and clinical utility of cardiac natriuretic hormones. Am J Physiol Heart Circ Physiol 2011;301:H12–H20 [DOI] [PubMed] [Google Scholar]
- 8.Braunwald E. Biomarkers in heart failure. N Engl J Med 2008;358:2148–2159 [DOI] [PubMed] [Google Scholar]
- 9.Vila G, Resl M, Stelzeneder D, et al. Plasma NT-proBNP increases in response to LPS administration in healthy men. J Appl Physiol 2008;105:1741–1745 [DOI] [PubMed] [Google Scholar]
- 10.Miyashita K, Itoh H, Tsujimoto H, et al. Natriuretic peptides/cGMP/cGMP-dependent protein kinase cascades promote muscle mitochondrial biogenesis and prevent obesity. Diabetes 2009;58:2880–2892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Das SR, Drazner MH, Dries DL, et al. Impact of body mass and body composition on circulating levels of natriuretic peptides: results from the Dallas Heart Study. Circulation 2005;112:2163–2168 [DOI] [PubMed] [Google Scholar]
- 12.Lund LH, Williams JJ, Freda P, LaManca JJ, LeJemtel TH, Mancini DM. Ghrelin resistance occurs in severe heart failure and resolves after heart transplantation. Eur J Heart Fail 2009;11:789–794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vestergaard ET, Andersen NH, Hansen TK, et al. Cardiovascular effects of intravenous ghrelin infusion in healthy young men. Am J Physiol Heart Circ Physiol 2007;293:H3020–H3026 [DOI] [PubMed] [Google Scholar]
- 14.Nagaya N, Moriya J, Yasumura Y, et al. Effects of ghrelin administration on left ventricular function, exercise capacity, and muscle wasting in patients with chronic heart failure. Circulation 2004;110:3674–3679 [DOI] [PubMed] [Google Scholar]
- 15.van der Zander K, Houben AJ, Hofstra L, Kroon AA, de Leeuw PW. Hemodynamic and renal effects of low-dose brain natriuretic peptide infusion in humans: a randomized, placebo-controlled crossover study. Am J Physiol Heart Circ Physiol 2003;285:H1206–H1212 [DOI] [PubMed] [Google Scholar]
- 16.Seoane LM, Al-Massadi O, Caminos JE, Tovar SA, Dieguez C, Casanueva FF. Sensory stimuli directly acting at the central nervous system regulate gastric ghrelin secretion. an ex vivo organ culture study. Endocrinology 2007;148:3998–4006 [DOI] [PubMed] [Google Scholar]
- 17.Vila G, Maier C, Riedl M, et al. Bacterial endotoxin induces biphasic changes in plasma ghrelin in healthy humans. J Clin Endocrinol Metab 2007;92:3930–3934 [DOI] [PubMed] [Google Scholar]
- 18.Cao LH, Yang XL. Natriuretic peptides and their receptors in the central nervous system. Prog Neurobiol 2008;84:234–248 [DOI] [PubMed] [Google Scholar]
- 19.Maier C, Riedl M, Vila G, et al. Cholinergic regulation of ghrelin and peptide YY release may be impaired in obesity. Diabetes 2008;57:2332–2340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nobata S, Ventura A, Kaiya H, Takei Y. Diversified cardiovascular actions of six homologous natriuretic peptides (ANP, BNP, VNP, CNP1, CNP3, and CNP4) in conscious eels. Am J Physiol Regul Integr Comp Physiol 2010;298:R1549–R1559 [DOI] [PubMed] [Google Scholar]
- 21.Lainchbury JG, Richards AM, Nicholls MG, Espiner EA, Yandle TG. Brain natriuretic peptide and neutral endopeptidase inhibition in left ventricular impairment. J Clin Endocrinol Metab 1999;84:723–729 [DOI] [PubMed] [Google Scholar]
- 22.Nagaya N, Uematsu M, Kojima M, et al. Elevated circulating level of ghrelin in cachexia associated with chronic heart failure: relationships between ghrelin and anabolic/catabolic factors. Circulation 2001;104:2034–2038 [DOI] [PubMed] [Google Scholar]
- 23.Akamizu T, Kangawa K. Therapeutical applications of ghrelin to cachexia utilizing its appetite-stimulating effect. Peptides 2011;11:2295–2300 [DOI] [PubMed] [Google Scholar]
- 24.Fujimatsu D, Kotooka N, Inoue T, Nishiyama M, Node K. Association between high molecular weight adiponectin levels and metabolic parameters. J Atheroscler Thromb 2009;16:553–559 [DOI] [PubMed] [Google Scholar]
- 25.Tsukamoto O, Fujita M, Kato M, et al. Natriuretic peptides enhance the production of adiponectin in human adipocytes and in patients with chronic heart failure. J Am Coll Cardiol 2009;53:2070–2077 [DOI] [PubMed] [Google Scholar]