Thy food is such As has been belch’d on by infected lungs. William Shakespeare, Pericles, IV, vi, 178.
The causal relationship between the conjugal pair of famine and pestilence has been known for millennia. It is recognized that malnutrition and infection are the two major obstacles for health, development, and survival worldwide, and poverty and ignorance are the most significant contributing factors (1, 2). Epidemiological observations have confirmed that infection and malnutrition aggravate each other. However, nutrition does not influence all infections equally (3, 4). For some infections (e.g., pneumonia, bacterial and viral diarrhea, measles, tuberculosis), there is overwhelming evidence that the clinical course and final outcome are affected adversely by nutritional deficiency. For others (e.g., viral encephalitis, tetanus), the effect of nutritional status is minimal. For still others (e.g., influenza virus, human immunodeficiency virus), nutrition exerts a moderate influence. It is now established that nutritional deficiency is commonly associated with impaired immune responses, particularly cell-mediated immunity, phagocyte function, cytokine production, secretory antibody response, antibody affinity, and the complement system (1, 5, 6). In fact, malnutrition is the commonest cause of immunodeficiency worldwide.
There was a three-pronged impetus for systematic studies of immune responses in undernourished individuals. First, there was a plethora of public health data indicating an interaction, usually synergistic but occasionally antagonistic, between malnutrition and infection (3). Second, new concepts and novel techniques in immunology emerged in the 1960s and 1970s. Third, dramatic human stories and demographic data stimulated individual scientists, as the following example shows (7). My interest in nutrition-immunity interactions was kindled by two cases: first, the story with an unhappy ending, of a child; second, the bleak scenario of the Third World. Eighteen-month-old Kamala was thin, her skin pale as wax, and her lungs screaming for air. She wore a spectral white death-mask in a frame of black hair. Her shrivelled body and swollen legs were typical of marasmic kwashiorkor, and she had an obvious fulminant infection. Lung aspirate revealed the opportunistic organism Pneumocystis carinii. Despite our best efforts, we lost the child. I speculated that malnutrition had robbed Kamala of her defenses against infection and led to premature demise. The tears shed on her death were not my first and would not be my last. There would be another Kamala, and another, and another. The second case was of the poor nations of the world, with high infant mortality, poor sanitation, contaminated food and water, a low literacy rate, and short life expectancy. Widespread malnutrition and infection were obvious shackles to development. Research into their interactions became a necessity.
Tuberculosis is a major cause of death in underprivileged populations. It has been estimated that 3 million to 4 million individuals die of the disease every year. In addition to environmental factors such as overcrowding, host immunity plays a crucial role in determining the final outcome. The delicate balance between the host’s ability to kill Mycobacterium tuberculosis and the microorganism’s efforts to evade the microbicidal armamentarium of the host makes fascinating study.
A number of innate and adaptive mechanisms are responsible for killing Mycobacteria (8, 9). The major role played by macrophages has been reviewed extensively (10). Infection occurs commonly through the respiratory tract. Bacteria that survive mucociliary escalator of the upper respiratory tract are ingested by alveolar macrophages that contain numerous acidic phagocytic vacuoles and hydrolytic enzymes. Macrophage activation results in a drastic reduction in the number of viable bacteria that may be completely eradicated. However, some mycobacteria may survive the powerful microbicidal onslaught and escape into the cytoplasm where they multiply unhindered, leading ultimately to cell death, and release into the tissues where they enter other cells including macrophages. Persistent organisms provide the antigenic stimulation and cell-mediated hypersensitivity reaction that leads to local accumulation of inflammatory cells and formation of granulomas. This process limits the spread of mycobacteria but is associated with tissue necrosis, fibrosis, and functional impairment. This stereotypic hide-and-seek game of evasion, activation, attack, and death is played out in response to many intracellular pathogens, e.g., Listeria monocytogenes (11).
Bloom and colleagues (12–16) have conducted a number of studies to elucidate the principal mechanisms by which murine mononuclear phagocytes kill M. tuberculosis. Now, Bloom and colleagues take us one major step forward by examining the effects of a low protein diet on anti-mycobacterial immunity (17). Young adult mice fed a diet containing 2% protein died rapidly following challenge with M. tuberculosis; their immune responses were compared with those of animals fed a diet containing 20% protein. Malnourished animals showed a reduced expression of interferon γ, tumor necrosis factor α, and inducible nitric oxide synthase in the first 2 weeks after infectious challenge. Interestingly, these changes were observed in the lungs but not in the liver, and the effects wore off after 2 weeks after challenge. There was no significant effect on total nitric acid production in vivo. Granulomatous inflammation was studied at the light, immunohistochemical, and electron microscopic levels, and was impaired in the low-protein group, confirming and extending earlier observations (18). The immunologic changes and risk of death could be reversed by reverting to a normal high-protein diet.
The seminal work of Bloom and colleagues raises many new questions. Are the findings nutrient-specific? Did body weight and lymphoid organ weight differ in the two animal groups? It is possible that at least some of the observed effects may be the result of concomitant deficiencies of micronutrients such as zinc. It is recognized that inadequate diets result in poor appetite, malabsorption, and decreased growth. Thus, the consumption and absorption of nutrients that are critical for optimum immune responses (e.g., zinc, selenium, vitamin A, pyridoxine, vitamin E) are compromised. This confounding variable can be sorted out by including a pair-fed comparison group. Would the quality of dietary protein make a difference? In general, animal proteins are superior to vegetable proteins in sustaining growth and maintaining immunity; there are subtle differences in immune responses of animals fed casein-based and whey-based diets. What is the threshold of nutritional deficiency that results in a significant impairment of anti-mycobacterial defenses? The 2% protein diet is a very drastic nutritional insult and quite unlike what happens in the majority of deprived human populations. What is the explanation for the marked heterogeneity of survival time in genetically similar mice challenged with the same mycobacterial burden? What is the basis of tissue specificity of macrophage handling of the microorganisms? It has been shown that CD8 T cells specific for listeriolysin O mediate significant immunity in the liver but not in the spleen (19). Is one cell type essential for antibacterial defense at one site but not at another location, as has been shown for neutrophils and Listeria (20). Would deficiencies of other nutrients result in impaired anti-mycobacterial immunity similar to that observed in mice on low-protein diet? For instance, deficiencies of vitamin A (1, 21, 22) and zinc (1, 23–25) alter a wide range of immune responses. Would the immunologic abnormalities be reversible in young animals whose mothers had been subjected to a chronic nutritional insult before and/or during gestation? Both in small-for-gestation low-birth-weight infants (26, 27) and in animal models of intrauterine undernutrition or zinc deficiency (28, 29), the immunologic impairment is profound and long lasting. What is the status of other immunologic mechanisms that play an important role in defense against intracellular pathogens, e.g., CD4+ and CD8+ T cells (19, 30, 31); αβ and γδ T cells (32, 33); interleukins 2, 4, 6, 8, and 12 (31, 33–38); natural killer cell activity (39); fibronectin (40); and heat-shock protein (41)? Neutralizing antibodies (42), gene knockout mice (43), and adoptive transfer assays (19) with bone marrow chimeric or transgenic rodent hosts can be deployed to study the specific role of individual immune processes. What is the impact of genetic host factors on antigen recognition and immunologic defense (44)? Finally, it would be useful to confirm the interesting observations reported in the study by Chan et al. (17) on a larger number of animals that would permit an adequate statistical analysis and to extend these investigations to newly diagnosed as well as chronically infected patients with pulmonary tuberculosis.
There is exciting new information on another face of host–parasite interaction. Viruses can mutate and show altered virulence because of nutritional deficiencies in the hosts they infect. Beck and coworkers (45) showed that selenium deficiency enhanced the heart-damaging potential of coxsackievirus. Virus strain recovered from selenium-deficient animals was capable of inducting damage in well-nourished animals. Most interestingly, there were six nucleotide changes between the avirulent input virus strain and the virulent virus recovered from selenium-deficient animals. This report of a specific nutritional deficiency associated with changes in a viral genome and virulence needs confirmation in other viruses and in other nutritional deficiency states. Moreover, the magnitude and duration of nutritional insult that has the potential to bring about these changes in the structure and virulence of pathogens needs to be defined. If confirmed, these exciting data will have far-reaching epidemiologic implications and may explain the emergence of novel infectious diseases in populations with endemic nutritional deficiencies.
Our knowledge in nutrition-immunity interactions has opened up exciting possibilities for nutritional intervention for both primary and secondary prevention of infection in high-risk groups. Nutritional deficiencies are seen often in hospitalized patients. These individuals are susceptible to develop life-threatening opportunistic infections. Recent animal work (46) has highlighted the value of nutrient-enriched diets in improving immune responses and survival following challenge with organisms such as Listeria (Figs. 1 and 2), and limited clinical studies have confirmed these observations. Similarly, a large proportion of the elderly have reduced dietary intakes and low blood levels of various nutrients (47). They are also prone to respiratory infection. Several investigations have shown a correlation between nutritional status and incidence of infection in old age. The results of a few recent intervention trials indicate that modest supplements of micronutrients improve immune responses and more significantly, reduce the incidence of respiratory infection and antibiotic usage (48). In addition, post-vaccination immune responses are higher in subjects given nutritional supplements than in untreated controls. These observations have profound clinical and public health implications.
Figure 1.
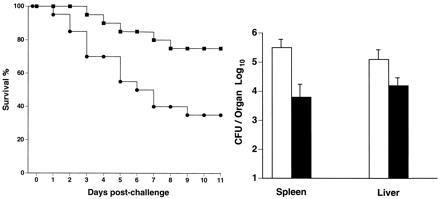
Malnutrition was induced in 8-week-old C57BL/6 × DBA/2 F1 hybrid male mice fed approximately 40% of nutrient requirement for 3 weeks, and the animals were divided into two groups. One group received a feeding formula that was enriched in those nutrients known to stimulate immune responses; the second group received a control formula. After 2 weeks of formula feeding, the mice were challenged with 4 × 104 L. monocytogenes intraperitoneally. Survival was observed, and the number of bacteria in the liver and the spleen were counted. (Left) More mice survived in the enriched formula group (▪) compared with the control (•) on days 3, 5 (P < 0.05), 7 (P < 0.02), and 10 (P < 0.02) postchallenge. (Right) The number of Listeria in both the spleen (P < 0.01) and the liver (P < 0.05) was lower in the enriched formula fed group (solid bars) compared with the control (open bars). CFU, colony-forming units.
Figure 2.
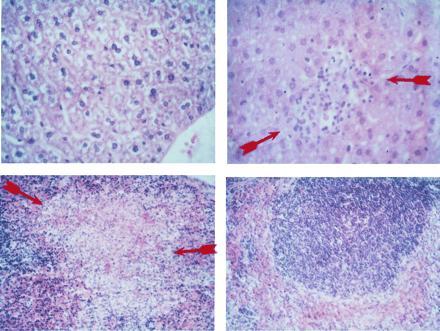
Histological examination of the liver showed focal areas of hepatocyte necrosis, mononuclear and neutrophilic infiltrate, and apoptotic liver cells in animals fed control formula (Upper Right); the necrotic liver cells appeared fuzzy. (Upper Left) In contrast, the normal lobular architecture and hepatocyte appearance was preserved in animals on enriched formula. (Hematoxylin/eosin ×20.) (Lower Left) The spleen of animals on the control formula showed subcapsular foci of granulomatous inflammation populated mainly by macrophages and paucity of lymphoid follicles. There was evidence of cellular necrosis. (Lower Right) In contrast, the spleen of animals fed the enriched formula showed dense mononuclear cell aggregates and absence of necrotic granuloma. (Hematoxylin/eosin ×10.)
The era of nutritional manipulation of the immune system has finally dawned and it brings with it the promise of using diet and nutrition as innovative powerful tools to reduce illness and death caused by infection.
References
- 1.Chandra R K. Am J Clin Nutr. 1991;53:1087–1101. doi: 10.1093/ajcn/53.5.1087. [DOI] [PubMed] [Google Scholar]
- 2.Chandra R K. Nutrition and Immunology. St. John’s, Newfoundland, Canada: ARTS Biomedical; 1992. pp. 9–43. [Google Scholar]
- 3.Scrimshaw N S, Taylor C E, Gordon J E. Interactions of Nutrition and Infection. Geneva: W.H.O.; 1968. [PubMed] [Google Scholar]
- 4.Chandra R K. Lancet. 1983;i:688–691. [Google Scholar]
- 5.Chandra R K, Newberne P M. Nutrition, immunity and infection: Mechanisms of interactions. New York: Plenum; 1977. [Google Scholar]
- 6.Gershwin M E, Beach R S, Hurley L S. Nutrition and Immunity. New York: Academic; 1985. [Google Scholar]
- 7.Anonymous Curr Contents. 1987;30:15. [Google Scholar]
- 8.Kaufmann S H E. Curr Topics Microbiol Immunol. 1988;138:141–176. [PubMed] [Google Scholar]
- 9.Bancroft G J, Schreiber R D, Unanue E R. Immunol Rev. 1991;124:5–24. doi: 10.1111/j.1600-065x.1991.tb00613.x. [DOI] [PubMed] [Google Scholar]
- 10.Fenton M J, Vermeulen M W. Infect Immun. 1996;64:683–690. doi: 10.1128/iai.64.3.683-690.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kaufmann S H E. Annu Rev Immunol. 1993;11:129–163. doi: 10.1146/annurev.iy.11.040193.001021. [DOI] [PubMed] [Google Scholar]
- 12.Chan J, Xing Y, Magliozzo R S, Bloom B R. J Exp Med. 1992;175:1111–1122. doi: 10.1084/jem.175.4.1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Flynn J L, Chan J, Triebold K J, Dalton D K, Stewart T A, Bloom B R. J Exp Med. 1993;178:2249–2253. doi: 10.1084/jem.178.6.2249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chan J, Tanaka K, Carroll D, Flynn J, Bloom B R. Infect Immun. 1995;63:736–740. doi: 10.1128/iai.63.2.736-740.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Flynn J L, Goldstein M M, Chan J, Triebold K J, Pfeffer K, Lowenstein C J, Schreiber R, Mak T W, Bloom B R. Immunity. 1995;2:561–572. doi: 10.1016/1074-7613(95)90001-2. [DOI] [PubMed] [Google Scholar]
- 16.Flynn J L, Goldstein M M, Triebold K J, Sypek J, Wolfe S, Bloom B R. J Immunol. 1995;155:2515–2524. [PubMed] [Google Scholar]
- 17.Chan J, Tian Y, Tanaka K E, Tsang M S, Yu K, Salgame P, Carroll D, Kress Y, Teitelbaum R, Bloom B R. Proc Natl Acad Sci USA. 1996;93:14857–14861. doi: 10.1073/pnas.93.25.14857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bhuyan U N, Ramalingaswami R. Am J Pathol. 1974;76:313–320. [PMC free article] [PubMed] [Google Scholar]
- 19.Harty J T, Bevan M L. Infect Immun. 1996;64:3632–3640. doi: 10.1128/iai.64.9.3632-3640.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Conlan J W, North R J. J Exp Med. 1994;179:259–268. doi: 10.1084/jem.179.1.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nauss K M, Phua C-C, Ambrogi L, Newberne P M. J Nutr. 1985;115:109–118. doi: 10.1093/jn/115.7.909. [DOI] [PubMed] [Google Scholar]
- 22.Weidermann U, Tarkowski A, Bremell T, Hanson L A, Kahu H, Dahlgren U I. Infect Immun. 1996;64:209–214. doi: 10.1128/iai.64.1.209-214.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fernandez G, Nair M, Onoe K, Tanaka T, Floyd R, Good R A. Proc Natl Acad Sci USA. 1979;76:457–461. doi: 10.1073/pnas.76.1.457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chandra R K. Pediatrics. 1980;66:789–791. [PubMed] [Google Scholar]
- 25.Prasad A S, Meftah S, Abdallah J, Dardenne M. J Clin Invest. 1988;82:1202–1210. doi: 10.1172/JCI113717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chandra R K. Am J Dis Child. 1975;129:450–455. doi: 10.1001/archpedi.1975.02120410038013. [DOI] [PubMed] [Google Scholar]
- 27.Moscatelli P, Bricarelli F G, Piccinini A, Tomatis S, Dufour M A. Helv Paediatr Acta. 1976;31:241–247. [PubMed] [Google Scholar]
- 28.Chandra R K. Science. 1975;190:289–290. doi: 10.1126/science.1179211. [DOI] [PubMed] [Google Scholar]
- 29.Beach R S, Gershwin M E, Hurley L S. Science. 1982;218:469–472. doi: 10.1126/science.7123244. [DOI] [PubMed] [Google Scholar]
- 30.Harty J T, Schreiber R D, Bevan M J. Proc Natl Acad Sci USA. 1992;89:11612–11616. doi: 10.1073/pnas.89.23.11612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cooper A M, Roberts A D, Rhoades E R, Callahan H E, Getzy D M, Orme I M. Immunology. 1995;84:423–432. [PMC free article] [PubMed] [Google Scholar]
- 32.Fu Y X, Roark C E, Kelly K, Drevets D, Campbell P, O’Brien R, Born W. J Immunol. 1994;153:3101–3115. [PubMed] [Google Scholar]
- 33.Munk, M. E. & Emoto, M. (1995) Eur. Resp. J. 8, Suppl. 20, S668–S675. [PubMed]
- 34.Appelberg R. Immunobiology. 1994;191:520–525. doi: 10.1016/S0171-2985(11)80458-4. [DOI] [PubMed] [Google Scholar]
- 35.Johnson B J, McMurray D N. Infect Immun. 1994;62:1444–1450. doi: 10.1128/iai.62.4.1444-1450.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Munk M E, Mayer P, Anding P, Feldmann K, Kaufmann S H E. Infect Immun. 1996;64:1078–1080. doi: 10.1128/iai.64.3.1078-1080.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hook S, Griffin F, Mackintosh C, Buchan G. Immunology. 1996;88:269–274. doi: 10.1111/j.1365-2567.1996.tb00014.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Friedland J S, Hartley J C, Hartley C G S, Shattock R J, Griffin G E. Trans R Soc Trop Med Hyg. 1996;90:119–203. doi: 10.1016/s0035-9203(96)90141-8. [DOI] [PubMed] [Google Scholar]
- 39.Ratcliffe L T, Lukey P T, MacKenzie C R, Ress S R. Clin Exp Immunol. 1994;97:373–379. doi: 10.1111/j.1365-2249.1994.tb06097.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Aung H, Toossi Z, Wisnieski J J, Wallis R S, Culp L A, Phillips N B, Phillips M, Averill L E, Daniel T M, Ellner J J. J Clin Invest. 1996;98:1261–1268. doi: 10.1172/JCI118910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Retzlaff C, Yamamoto Y, Hoffman P S, Friedman H, Klein T W. Infect Immun. 1994;62:5689–5693. doi: 10.1128/iai.62.12.5689-5693.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Buchmeier N A, Schreiber R D. Proc Natl Acad Sci USA. 1985;82:7404–7408. doi: 10.1073/pnas.82.21.7404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rothe J, Lesslauer W, Lotscher H, Lang Y, Koebel P, Kontgen F, Althage A, Zinkernagel R, Steinmetz M, Bluetthmann H. Nature (London) 1993;364:798–802. doi: 10.1038/364798a0. [DOI] [PubMed] [Google Scholar]
- 44.Daugelat S, Ladel C H, Kaufmann S H E. Infect Immun. 1995;63:2033–2040. doi: 10.1128/iai.63.5.2033-2040.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Beck M A, Shi Q, Morris V C, Levander O, A. Nat Med. 1995;1:433–436. doi: 10.1038/nm0595-433. [DOI] [PubMed] [Google Scholar]
- 46.Chandra R K, Baker M, Whang S, Au B. Immunol Lett. 1991;27:45–48. doi: 10.1016/0165-2478(91)90242-3. [DOI] [PubMed] [Google Scholar]
- 47.Munro H, Schlierf G, editors. Nutrition of the Elderly. New York: Raven; 1992. [Google Scholar]
- 48.Chandra R K. Lancet. 1992;34:1124–1127. doi: 10.1016/0140-6736(92)93151-c. [DOI] [PubMed] [Google Scholar]


