Abstract
Background
Despite the Centers for Disease Control and Prevention recommendations for annual HIV testing of at-risk populations, including those with substance use disorders, there are no data on the HIV testing practices of buprenorphine-prescribing physicians.
Objective
To describe HIV testing practices among buprenorphine-prescribing physicians.
Methods
We conducted a cross-sectional survey of physicians enrolled in a national system to support buprenorphine prescribing between July and August 2008. The electronic survey included questions on demographics; clinical training and experience; clinical practice; patient characteristics; and physician screening practices, including HIV testing.
Results
Only 46% of 382 respondent physicians conducted HIV testing. On univariate analysis, physicians who conducted HIV testing were more likely to report addiction specialty training (33% vs. 19%, p=.001), practicing in addiction settings (28% vs. 16%, p=.006), and having treated more than 50 patients with buprenorphine (50% vs. 31%, p<.0001) compared to those who did not. Compared to physicians who did not conduct HIV testing, physicians who conducted HIV testing had a lower proportion of buprenorphine patients who were White (75% vs. 82%, p=.01) or dependent upon prescription opioids (57% vs. 70%, p<.0001). In multivariate analysis, physicians who conducted HIV testing were more likely to have treated more than 50 patients with buprenorphine (OR 1.777, 95%CI 1.011 – 3.124) and had fewer patients dependent upon prescription opioids (OR 0.986 95% CI 0.975 – 0.998) than physicians who did not.
Conclusion
Interventions to increase HIV testing among physicians prescribing buprenorphine are needed.
Introduction
Opioid dependence, defined as tolerance, withdrawal and compulsive use of prescription opioids and heroin(American Psychiatric Association, 2000), is increasing(Substance Abuse & Mental Health Services Administration, 2010). Opioid agonist therapy, traditionally with methadone, is accepted as a central component of treatment for this disorder(Maremmani et al., 2010). Approved by the U.S. Food and Drug Administration in 2002, buprenorphine, a partial opioid agonist at the μ opioid receptor, is an effective(Sullivan et al., 2008; Walley et al., 2008) and increasingly available option in combination with naloxone (buprenorphine/naloxone) or alone(Sullivan et al., 2005). Physicians who have obtained a special registration from the Drug Enforcement Agency (DEA); and have established linkages to appropriate clinical services may prescribe buprenorphine through office-based practices(Sullivan et al., 2008). More than 16,000 United States physicians have been appropriately trained(Egan et al., 2010), including generalists, psychiatrists, and addiction specialists(Sullivan et al., 2008; Walley et al., 2008). As part of their practice, many office-based buprenorphine providers are well positioned to provide routine primary care to their patients. Recent data indicates that approximately 46% of office-based prescribers are generalists(Greene, 2010). Patients are typically young(Moore et al., 2007; Cunningham et al., 2008), lack routine medical care through other settings, and are seen at least monthly(Sullivan et al., 2008) by their buprenorphine-prescribing physician.
Current recommendations by the Centers for Disease Control and Prevention (CDC) advocate for routine HIV testing in general medical settings with annual testing of individuals at high risk(Branson et al., 2006). Given the prevalent needle-sharing and sexual risk behaviors among opioid dependent patients(Neaigus et al., 2001; Gyarmathy et al., 2002; Strathdee et al., 2003; Strathdee et al., 2010), annual HIV testing is recommended(Branson et al., 2006). Previous data have demonstrated slow implementation of routine HIV testing in addiction specialty treatment settings (e.g. opioid treatment programs)(Brown et al., 2007; Dookeran et al., 2009; Abraham et al., 2010; Pollack et al., 2010), but there are no data on the HIV testing practices of physicians who provide office-based buprenorphine.
Therefore, the purpose of the current study was to determine the rates of HIV testing among physicians prescribing buprenorphine. We compared the rate of HIV testing to evaluation of comorbid diseases; determined the characteristics of physicians and their associated practices among those conducting HIV testing and those not conducting HIV testing; and evaluated factors independently associated with conducting HIV testing.
Methods
Population
From July to August 2008, we conducted a national survey of physicians. A convenience sample of physicians (n=3,412) involved in the Substance Abuse and Mental Health Services Administration (SAMHSA)-funded Physician Clinical Support System for buprenorphine (PCSS-B)(Egan et al., 2010) were invited to complete our survey through an email. The PCCS-B includes a network of physician mentors and mentees to provide a structure for educational support for physicians interested in prescribing buprenorphine for opioid dependence (Egan et al., 2010). The survey was conducted as an electronic Web-based survey through SurveyMonkey©, with two email reminders. We present the findings of the 455 physicians who responded. All answers were kept anonymous and there were no identifiers linking the physicians to their responses. The study was reviewed and approved by the Yale Humans Investigation Committee. Participants were not reimbursed.
Data Collection: Survey Instrument
The online survey included 33 items. We collected data about physician demographics, clinical training, and experience with buprenorphine, including number of patients treated with buprenorphine and years prescribing buprenorphine, and addiction specialty certification. We inquired about the physicians’ practice, including practice type, size, and setting; and proportion of time spent on different activities, including patient care, research and administration. In addition, physicians were asked to estimate the percentage of patients in their practice with particular characteristics, including gender; age; race/ethnicity; insurance status and opioid of choice (e.g. heroin vs. prescription opioids).
Physicians were asked how frequently they addressed the following risk behaviors and comorbid diseases: tobacco, alcohol, substances other than opioids; depression; hepatitis screening and vaccination; HIV screening and queries about their patients’ sexual risk behaviors (see Appendix Table 1). Response options assessed frequency and included: never, once, every visit, every 3 months, every 6 months, once a year, don’t know, and decline to answer. For purposes of this analysis, we grouped the responses into the following three categories: 1) never/don’t know/decline to answer; 2) once; 3) more than once. Response options were grouped into these three categories to help identify the proportion of practices that were not reliably conducting such screening and based on distribution of the responses. The survey was piloted for usability before dissemination with members of the Connecticut Society of Addiction Medicine and PCSS mentors who were buprenorphine prescribers (total n=85). It was subsequently sent out unchanged in its final form.
Statistical Analysis
The primary analyses were a descriptive evaluation of survey responses, particularly those of physician reports of screening practices. Percentages were computed for categorical variables and means and standard deviations for continuous measures. To explore the characteristics of physicians who conducted HIV testing compared to those who did not, we first categorized responses by those who reported testing once or more frequently to those who did not. We then evaluated differences between HIV testers and non-testers for physician and patient characteristics, using t-tests and chi-square tests (Fisher’s exact tests were used for estimated cell sizes less than five) in univariate analysis and logistic regression in multivariate analysis. The multivariate logistic model included variables that were significant at p < 0.05 in univariate analyses. All analyses were conducted using SPSS/PASW 17.0 software (IBM Corporation, Somers, NY).
Results
Of the 3,412 providers who were invited to participate in the survey, 455 initiated the survey, representing a 13% response rate. We restricted our analysis to the 382 physicians that completed at least half of the survey, representing 84% of those that initiated the survey. The characteristics of the physicians and their patients are summarized in Table 1. The majority of physicians were White (76%), males (74%) and generalists (53%); physicians spent a mean of 81% of their time on patient care duties. The majority of their patients receiving buprenorphine were White (mean percent=79%, SD=27%), males (mean percent=61%, SD=25%), between the ages of 18–40 years old (mean percent=62%, SD=28%) and dependent upon prescription opioids (mean percent=64%, SD=30%). The minority were uninsured (mean percent=18%, SD=27%).
Table 1.
Physicians and their Practice and Patient Characteristics, n=382
| Characteristic | TOTAL (N=382) |
|---|---|
| Physician Race, %(n) | |
| American Indian or Alaska Native | 1% (5) |
| Asian | 9% (35) |
| African American | 5% (19) |
| Pacific Islander | < 1% (1) |
| White | 76% (291) |
| Others | 6% (21) |
| Physician Hispanic ethnicity, %(n) | 4% (15) |
| Physician male gender, %(n) | 74% (283) |
| Physician certified addiction training, %(n) | 28% (104) |
| Specialty (not mutually exclusive) | |
| Internal Medicine, %(n) | 19% (74) |
| Family practice, %(n) | 34% (131) |
| HIV/ID, % (n) | 4% (15) |
| Addiction medicine, %(n) | 25% (97) |
| Psychiatry, %(n) | 32% (123) |
| Percent of time on patient treatment, mean (SD) | 81%(22.5) |
| Years since graduation, mean (SD) | 24.3 (11.1) |
| Years prescribing buprenorphine, %(n) | |
| ≤ 3 Years | 72% (273) |
| > 3 Years | 28% (106) |
| Urban setting, %(n) | 56% (216) |
| Addiction setting, %(n) | 22% (83) |
| Treated >50 buprenorphine patients, %(n) | 40% (149) |
| Percent of patients male, mean (SD) | 61% (25) |
| Percent of patients white, mean (SD) | 79% (27) |
| Percent of patients Hispanic, mean (SD) | 8% (16) |
| Percent of patients age 18–40 years, mean (SD) | 62% (28) |
| Percent uninsured, mean (SD) | 18% (27) |
| Percent using prescription opioids, mean (SD) | 64% (30) |
| Percent using intravenous heroin, mean (SD) | 21% (26) |
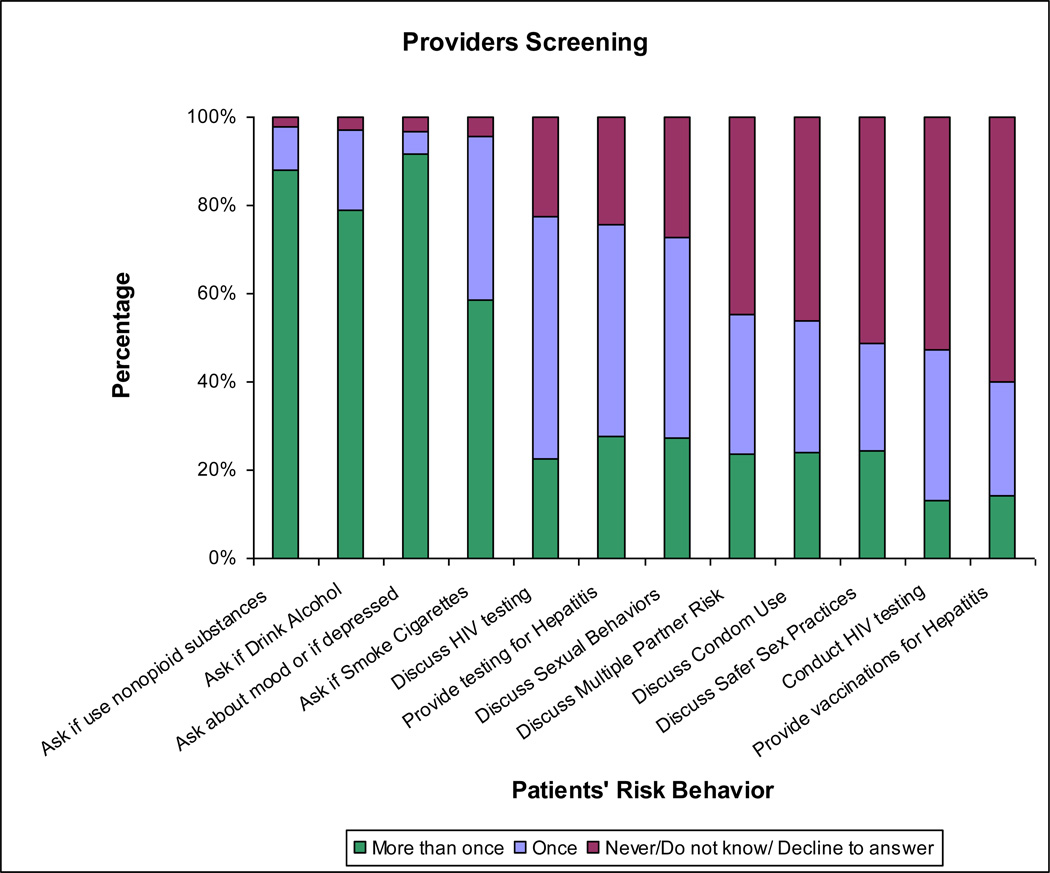
Assessments for Risk Behaviors and Comorbid Diseases
Most physicians reported assessing for alcohol use and other substances at every visit (65% and 84%, respectively) (Figure 1). Screening for depression was also common, with over 90% reporting routine screening (81% at every visit, 10% every 3 months) (data not otherwise shown). Less than 40% of physicians screened for cigarette smoking at every visit. A lower proportion of physicians reported frequent assessment of sexual risk behaviors and infectious diseases, including HIV and hepatitis C (HCV): fewer than 25% of physicians reported asking about condom use more than once; 26% reported discussing sexual behaviors more than once; fewer than 25% of physicians reported discussing HIV testing more than once and 14% reported screening at least annually (34% reported screening only once); and less than one third of physicians reported testing for HCV at least annually (27%).
Figure 1.
Physician Screening Practices for Risk Behaviors and Comorbid Diseases
Physician Characteristics by HIV Testing
Comparisons between physicians who conducted HIV testing at least once (175/382, 46%) and physicians who did not conduct HIV testing (207/382, 54%) are shown in Table 2. In comparison to respondents who did not conduct HIV testing, respondents who conducted HIV testing were more likely to report their specialty as addiction medicine (33% vs. 19%, p= .001). Similarly, physicians who conducted HIV testing were more likely to practice in an addiction setting (28% vs. 16%, p= .006) or have certification in addiction medicine or addiction psychiatry (36% vs. 22%, p= .004). Physicians who spent less time on patient treatment were more likely to conduct HIV testing than those with more patient treatment (78% vs. 82%, p= .03). Similarly, those with more than 3 years of experience prescribing buprenorphine were more likely to conduct HIV testing than those with less experience (p= .02). HIV testing practices did not vary by the physician’s race/ethnicity or gender.
Table 2.
Physician Characteristics by HIV Testing, n=382
| Characteristic | Conducted HIV Testing 46% (N=175) |
Did Not Conduct HIV Testing 54% (N=207) |
p-value |
|---|---|---|---|
| Physician Race, %(n) | .73 | ||
| American Indian or Alaska Native | 1% (2) | 2% (3) | |
| Asian | 12% (20) | 8% (15) | |
| African American | 5% (9) | 5% (10) | |
| Pacific Islander | 0% (0) | 0.5% (1) | |
| White | 77% (132) | 80% (159) | |
| Others | 5% (9) | 6% (12) | |
| Physician Hispanic ethnicity, %(n) | 3% (5) | 5% (10) | .31 |
| Physician male gender, %(n) | 71% (124) | 77% (159) | .19 |
| Physician certified addiction training, %(n) | 36% (61) | 22% (43) | .004 |
| Specialty (not mutually exclusive) | |||
| Internal Medicine, %(n) | 23% (40) | 16% (34) | .12 |
| Family practice, %(n) | 35% (62) | 33% (69) | .67 |
| HIV/ID | 6% (10) | 2% (5) | .11 |
| Addiction medicine, %(n) | 33% (58) | 19% (39) | .001 |
| Psychiatry, %(n) | 29% (51) | 35% (72) | .24 |
| Percent of time on patient treatment, mean (SD) | 78% (23%) | 82% (22%) | .03 |
| Years since graduation, mean (SD) | 23.98 (10.6) | 24.52 (11.5) | .64 |
| Years prescribing buprenorphine, %(n) | .02 | ||
| ≤3 Years | 66% (114) | 77%% (159) | |
| >3 Years | 34% (59) | 23% (47) |
Bold text indicates statistical significance at the p<0.05 level.
Practice and Patient Characteristics by HIV Testing
Patient and practice characteristics, based on physician-report, by physician HIV testing practices are shown in Table 3. Physicians who reported conducting HIV testing were more likely to have treated at least 50 patients with buprenorphine (50% vs. 31%, p< .0001). Compared to physicians who did not conduct HIV testing, physicians who conducted HIV testing had a lower proportion of buprenorphine patients who were White (75% vs. 82%, p= .01) or dependent upon prescription opioids (57% vs. 70%, p<.0001).
Table 3.
Practice and Patient Characteristics by HIV Testing, n=382
| Characteristic | Conducted HIV Testing 46% (N=175) |
Did Not Conduct HIV Testing 54% (N=207) |
p-value |
|---|---|---|---|
| Urban setting, %(n) | 61% (107) | 53% (109) | .10 |
| Addiction setting, %(n) | 28% (49) | 16% (34) | .006 |
| Treated >50 buprenorphine patients, %(n) | 50% (86) | 31% (63) | <0.0001 |
| Percent of patients male, mean (SD) | 60% (24) | 62% (25) | .48 |
| Percent of patients White, mean (SD) | 75% (29) | 82% (25) | .01 |
| Percent of patients Hispanic, mean (SD) | 10% (18) | 7% (15) | .04 |
| Percent of patients age 18–40 years, mean (SD) | 61% (27) | 62% (28) | .64 |
| Percent uninsured, mean (SD) | 19% (29) | 17% (25) | .33 |
| Percent using prescription opioids, mean (SD) | 57% (29) | 70% (30) | <.0001 |
| Percent using intravenous heroin, mean (SD) | 25% (25) | 18% (28) | .005 |
Bold text indicates statistical significance at the p<0.05 level.
Factors Independently Associated with HIV Testing
In multivariate analysis, we found that only two factors were significantly associated with conducting HIV testing (Table 4). Physicians who reported conducting HIV testing were more likely to have treated more than 50 patients with buprenorphine (OR 1.77, 95%CI 1.01, 3.12) and had fewer patients dependent upon prescription opioids (OR 0.99 95% CI 0.98, 1.0).
Table 4.
Factors Associated with HIV Testing, using Multivariate Logistic Regression, n=382
| Characteristic | OR | 95% CI | p value |
|---|---|---|---|
| Physician certified addiction training, | 0.683 | 0.371–1.259 | .222 |
| Specialty Addiction medicine | 1.271 | 0.675–2.394 | .458 |
| Percent of time on patient treatment | 0.997 | 0.986–1.008 | .605 |
| ≤ 3 years prescribing buprenorphine | 0.876 | 0.59–1.299 | .510 |
| Addiction setting | 1.127 | 0.600–2.114 | .711 |
| Treated >50 buprenorphine patients, %(n) | 1.777 | 1.011–3.124 | .046 |
| Percent of patients White | 0.995 | 0.983–1.007 | .401 |
| Percent of patients Hispanic | 1.004 | 0.985–1.024 | .671 |
| Percent using prescription opioids, mean (SD) | 0.986 | 0.975–0.998 | .020 |
| Percent using intravenous heroin, mean (SD) | 0.998 | 0.986–1.010 | .698 |
Bold text indicates statistical significance at the p<0.05 level.
Discussion
To our knowledge, this is the first survey specifically evaluating the medical screening practices of buprenorphine providers, the majority of whom were internists and family physicians who were not addiction specialists. Our results demonstrate several key findings. First, although physicians routinely assess substance use and mental health issues, including tobacco, alcohol, and depression, they did not report routinely inquiring about sexual risk behaviors or comorbid diseases, including HIV and HCV. Only about 25% of physicians discussed sexual risk factors more than once with their patients, and only 46% of physicians reported ever conducting HIV testing. Physicians who had addiction specialty training and who practiced in addiction settings, as well as those with more patients receiving buprenorphine, were more likely to conduct HIV testing. Patient characteristics were also associated with HIV testing practices, as physicians were more likely to conduct HIV testing if they had had a smaller proportion of patients that were White or dependent upon prescription opioids. Factors independently associated with conducting HIV testing in logistic regression analyses were having treated more than 50 patients with buprenorphine and having fewer patients dependent upon prescription opioids.
Our findings that buprenorphine prescribing physicians reported low rates of screening for sexual risk behaviors and HIV are consistent with the existing literature. Physicians often underestimate HIV risk behaviors (Ward et al., 1995), which may explain their inconsistent sexual history taking practices (Schwartz et al., 1991; Gongidi et al., 2010). A survey of osteopathic primary care physicians found that among the physicians that reported taking sexual histories from their patients, there was variation in the topics covered by the surveyed physicians. While 76% asked about contraceptive practices, only 53% asked about number of sex partners (Gongidi et al., 2010). These practices may, in part, explain the low rates of screening for sexually transmitted infections, including syphilis, gonorrhea and Chlamydia found in a national survey of U.S. physicians (St Lawrence et al., 2002). Among patients who are injection drug users and non-injection drug users (Strathdee et al., 2003; Des Jarlais et al., 2007), including those in treatment (Sullivan et al., 2008), sexual risk behaviors are prevalent and major drivers of the HIV epidemic. Although buprenorphine decreases HIV risk through decreasing drug-related HIV risk behaviors, it does not appear to decrease sexually-related HIV risk behaviors (Sullivan et al., 2008), underscoring the importance of continued assessment and education in this population.
In addition to targeting HIV risk behaviors, the importance of routine HIV testing, treatment and retention in care for patients who use substances is well recognized (Institute of Medicine, 2000; Branson et al., 2006; Volkow et al., 2010). Of the estimated 21% or 232,700 undiagnosed HIV-infected individuals in the U.S., 14.5% are male injection drug users and 13.7% are female injection drug users (Campsmith et al., 2010). High-risk heterosexual sex, including having sex with a partner that uses injection drugs, accounts for an additional 47% of those who are undiagnosed(Campsmith et al., 2010). HIV testing and diagnosis is essential for facilitating appropriate care and treatment for the individual, as earlier treatment is recognized to improve patient outcomes (Palella et al., 2003) and public health, since knowledge of one’s HIV status reduces risk behaviors (Marks et al., 2006).
Our findings of low HIV testing are consistent with the existing literature documenting there has been slow implementation of HIV screening to reach patients with substance use disorders (Dookeran et al., 2009) or in substance abuse treatment settings (Abraham et al., 2010; Pollack et al., 2010; Substance Abuse and Mental Health Services Administration, 2010). One study found that only 20% of all patients with a substance use disorder history had any evidence of HIV screening in their medical records; patients with both illicit drug and alcohol use disorders were screened the most (32%), with even lower screening rates among those with illicit drug use disorders alone (25%) and those with alcohol use disorders alone (11%) (Dookeran et al., 2009). Data from the National Survey of Substance Abuse Treatment Services (N-SSATS), which annually surveys all known public and private facilities in the United States offering substance abuse treatment, found that only 30% of surveyed facilities offered on-site HIV screening in 2007. Among those programs offering opioid agonist treatment (e.g. methadone), this number increased to 70% (Substance Abuse and Mental Health Services Administration, 2010). Available services, however, do not necessarily translate into patient care. The National Drug Abuse Treatment System Survey (NDATSS), which tracks services in outpatient substance abuse treatment facilities, found that although 82% of surveyed programs provide HIV counseling and testing services, only 29% of patients had actually received such services (Pollack et al., 2010). When the analysis was restricted to treatment facilities that had counseling and testing services, still only 35% patients received these services. These findings are consistent with other studies (Abraham et al., 2010). While one would anticipate that office-based physicians with a more medical focus than typically encountered in specialty treatment settings would be more likely to conduct HIV testing, our current study does not confirm that finding.
In our sample, physicians were less likely to conduct HIV testing if they had more White patients who were dependent upon prescription opioids. This pattern is concerning as it may reflect clinicians reserving testing for those patients with characteristics that they perceive at highest risk. Risk-based HIV testing, however, has not been shown to be more effective than universal screening (Jenkins et al., 2006). Moreover, this type of testing fails to recognize that individuals who use but do not inject drugs, including heroin and prescription opioids, are a high risk group for HIV, with HIV rates paralleling those of individuals who inject drugs (Strathdee et al., 2003; Des Jarlais et al., 2007; Strathdee et al., 2010). In fact, studies have demonstrated that non-injection drug using populations may have HIV risk that is as great or greater than their injecting counterparts (Strathdee et al., 2010). HIV transmission may occur through sexual activity with injection drug users; possibly through high risk drug use activity, including sharing of non-injection drug paraphernalia; and high levels of unprotected sex (Strathdee et al., 2010). Importantly, despite its impact on needle-sharing practices, buprenorphine does not necessarily decrease sexual risk behaviors (Sullivan et al., 2008).
A comprehensive review of published and unpublished literature identified multiple patient, provider and system level factors that hindered HIV testing (Burke et al., 2007). Patient-level factors include lack of patient acceptance and patient confidentiality concerns. Provider concerns are also important to consider, including lack of knowledge/training; competing priorities; perception of a low-risk patient population; and fear/concern of offending the patient. Inadequate reimbursement; lack of institutional policies that encourage HIV testing; lack of HIV-related referral networks are system-level factors that have been implicated as causes of low universal testing (Burke et al., 2007). Even since the recommendation of opt-out HIV testing, barriers persist. A qualitative study of patient and provider beliefs about HIV testing found that stigma and communication about HIV testing served as barriers (Bokhour et al., 2009). Among physicians in our survey, those that have treated more than 50 patients with buprenorphine or treat fewer patients dependent upon prescription opioids were more likely to conduct HIV testing. This may be related to increased physician comfort in providing buprenorphine and other addiction treatment, allowing for more time to provide comprehensive care to their patients. In addition, these physicians may have greater knowledge and comfort with sensitive issues, including discussing topics typically associated with stigma, such as HIV testing. Similar to our findings, the National Drug Abuse Treatment System Survey (NDATSS) (Pollack et al., 2010) found that programs serving a greater proportion of clients who inject drugs, African Americans, and Hispanic/Latinos were more likely to provide counseling and testing services. Although we did not specifically assess these variables, other factors that have been associated with HIV testing of a higher proportion of clients in outpatient substance abuse treatment centers include: higher staff-client ratios; public ownership; nonprofit status; programs that provide methadone; programs with the Joint Commission and city agency accreditation; and the implementation of comprehensive intake assessments and formal protocols and guidelines. Outpatient substance abuse treatment programs that had implemented formal protocols and guidelines tested twice the proportion of clients as other programs (30.7% vs. 15.3%). Beyond providers, program and patient-level factors are clearly associated with HIV testing availability (Brown et al., 2007; Brown et al., 2009; Tracy et al., 2009; Abraham et al., 2010).
Our study has several limitations. First, as we collected a convenience sample of buprenorphine-prescribing physicians registered into the PCCS-B, our findings may not be generalized to all physicians involved in the PCCS-B(Egan et al., 2010) or all buprenorphine-prescribing physicians in general though our response rate is consistent with other internet-based surveys of physicians (Katz et al., 2009; Shirts et al., 2009; Chun et al., 2011). Regardless, our findings likely represent a conservative estimate of screening practices as physicians failing to perform routine screening may have been less likely to respond. In addition, according to physicians in our sample, the majority of their patients were dependent upon prescription opioids. This contrasts to previous reports of patients engaged in office-based opioid treatment, which have found that the majority of patients prefer heroin thus our sample may not be representative of all clinical settings(Stein et al., 2005; Soeffing et al., 2009; Parran et al., 2010; Alford et al., 2011). Despite these limitations, this survey represents the first evaluation of screening practices specifically among buprenorphine-prescribing providers and is consistent with existing data from other settings providing care to patients who use substances(Brown et al., 2007; Abraham et al., 2010; Pollack et al., 2010). Second, our assessment relied on self-report, which may introduce reporting bias. Our results, therefore, likely represent a conservative estimate of actual practices and may overestimate current HIV testing. Third, we did not assess for reasons that physicians did not conduct HIV testing. We, therefore, cannot draw firm conclusions about why physicians did not conduct testing; for example, we do not know the proportion of patients that were previously known to be HIV-infected or were receiving care in other settings or recently tested. Physicians, however, also reported low rates of discussing HIV testing, in addition to low rates of actual testing. Finally, we relied on physician reports of patient behavior for this analysis, which likely underestimates the actual rates of patient HIV risk behaviors.
Conclusions
Rates of screening for sexual risk behaviors and HIV testing among buprenorphine physicians are not consistent with current guidelines, even among this high risk population. Future efforts need to focus on identifying and addressing barriers to meeting these recommendations. Informed by the literature from substance abuse treatment settings, office-based buprenorphine practices may benefit from implementing standardized assessments and protocols (Pollack et al., 2010) to routinize HIV testing.
Acknowledgements
Role of the Funding Source
This work was generously supported by Robert Wood Johnson Physician Faculty Scholars Award; NIDA grants (DA022398, DA000445, DA009803, DA019511-01, DA025991, DA020576-01A1); Robert Wood Johnson Foundation Clinical Scholars Program and the United States Department of Veterans Affairs Administration. These funding sources had no further role in the study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
Conflicts of Interest
The authors have no conflicts of interest.
Disclosures
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs.
This work was presented in earlier version at the College on Problems of Drug Dependence Annual Meeting, June 24th, 2009, Reno, Nevada.
References
- Abraham AJ, O'Brien LA, Bride BE, et al. HIV/AIDS services in private substance abuse treatment programs. Drug Alcohol Depend. 2010 doi: 10.1016/j.drugalcdep.2010.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alford DP, LaBelle CT, Kretsch N, et al. Collaborative care of opioid-addicted patients in primary care using buprenorphine: five-year experience. Arch Intern Med. 2011;171(5):425–431. doi: 10.1001/archinternmed.2010.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 2000 [Google Scholar]
- Bokhour BG, Solomon JL, Knapp H, et al. Barriers and facilitators to routine HIV testing in VA primary care. J Gen Intern Med. 2009;24(10):1109–1114. doi: 10.1007/s11606-009-1078-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Branson BM, Handsfield HH, Lampe MA, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep. 2006;55(RR-14):1–17. quiz CE11-14. [PubMed] [Google Scholar]
- Brown LS, Jr, Kritz S, Goldsmith RJ, et al. Health services for HIV/AIDS, HCV, and sexually transmitted infections in substance abuse treatment programs. Public Health Rep. 2007;122(4):441–451. doi: 10.1177/003335490712200404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown LS, Kritz S, Muhammad A, et al. Disparities in Health Services for HIV/AIDS, Hepatitis C Virus, and Sexually Transmitted Infections: Role of Substance Abuse Treatment Programs. J Addict Med. 2009;3(2):95–102. doi: 10.1097/ADM.0b013e318190f0e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke RC, Sepkowitz KA, Bernstein KT, et al. Why don't physicians test for HIV? A review of the US literature. AIDS. 2007;21(12):1617–1624. doi: 10.1097/QAD.0b013e32823f91ff. [DOI] [PubMed] [Google Scholar]
- Campsmith ML, Rhodes PH, Hall HI, et al. Undiagnosed HIV prevalence among adults and adolescents in the United States at the end of 2006. J Acquir Immune Defic Syndr. 2010;53(5):619–624. doi: 10.1097/QAI.0b013e3181bf1c45. [DOI] [PubMed] [Google Scholar]
- Chun TH, Spirito A, Rakowski W, et al. Beliefs and practices of pediatric emergency physicians and nurses regarding counseling alcohol-using adolescents: can counseling practice be predicted? Pediatr Emerg Care. 2011;27(9):812–825. doi: 10.1097/PEC.0b013e31822c1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham C, Giovanniello A, Sacajiu G, et al. Buprenorphine treatment in an urban community health center: what to expect. Fam Med. 2008;40(7):500–506. [PMC free article] [PubMed] [Google Scholar]
- Des Jarlais DC, Arasteh K, Perlis T, et al. Convergence of HIV seroprevalence among injecting and non-injecting drug users in New York City. AIDS. 2007;21(2):231–235. doi: 10.1097/QAD.0b013e3280114a15. [DOI] [PubMed] [Google Scholar]
- Dookeran NM, Burgess JF, Jr, Bowman CC, et al. HIV screening among substance-abusing veterans in care. J Subst Abuse Treat. 2009;37(3):286–291. doi: 10.1016/j.jsat.2009.03.003. [DOI] [PubMed] [Google Scholar]
- Egan JE, Casadonte P, Gartenmann T, et al. The Physician Clinical Support System-Buprenorphine (PCSS-B): a novel project to expand/improve buprenorphine treatment. J Gen Intern Med. 2010;25(9):936–941. doi: 10.1007/s11606-010-1377-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gongidi P, Sierakowski JJ, Bowen GS, et al. Survey of Attitudes and Practices of Osteopathic Primary Care Physicians Regarding Taking of Sexual Histories and HIV Screening. J Am Osteopath Assoc. 2010;110(12):712–720. [PubMed] [Google Scholar]
- Greene P. Outpatient Drug Utilization Trends for Buprenorphine Years 2002–2009. 2010 [Google Scholar]
- Gyarmathy VA, Neaigus A, Miller M, et al. Risk correlates of prevalent HIV, hepatitis B virus, and hepatitis C virus infections among noninjecting heroin users. J Acquir Immune Defic Syndr. 2002;30(4):448–456. doi: 10.1097/00042560-200208010-00011. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine, I. No Time to Lose: Making the Most of HIV Prevention. Washington, D.C.: 2000. [Google Scholar]
- Jenkins TC, Gardner EM, Thrun MW, et al. Risk-based human immunodeficiency virus (HIV) testing fails to detect the majority of HIV-infected persons in medical care Settings. Sex Transm Dis. 2006;33(5):329–333. doi: 10.1097/01.olq.0000194617.91454.3f. [DOI] [PubMed] [Google Scholar]
- Katz MA, Lamias MJ, Shay DK, et al. Use of rapid tests and antiviral medications for influenza among primary care providers in the United States. Influenza Other Respi Viruses. 2009;3(1):29–35. doi: 10.1111/j.1750-2659.2009.00070.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maremmani I, Gerra G. Buprenorphine-based regimens and methadone for the medical management of opioid dependence: selecting the appropriate drug for treatment. Am J Addict. 2010;19(6):557–568. doi: 10.1111/j.1521-0391.2010.00086.x. [DOI] [PubMed] [Google Scholar]
- Marks G, Crepaz N, Janssen RS. Estimating sexual transmission of HIV from persons aware and unaware that they are infected with the virus in the USA. AIDS. 2006;20(10):1447–1450. doi: 10.1097/01.aids.0000233579.79714.8d. [DOI] [PubMed] [Google Scholar]
- Moore BA, Fiellin DA, Barry DT, et al. Primary care office-based buprenorphine treatment: comparison of heroin and prescription opioid dependent patients. J Gen Intern Med. 2007;22(4):527–530. doi: 10.1007/s11606-007-0129-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neaigus A, Miller M, Friedman SR, et al. Sexual transmission risk among noninjecting heroin users infected with human immunodeficiency virus or hepatitis C virus. J Infect Dis. 2001;184(3):359–363. doi: 10.1086/322020. [DOI] [PubMed] [Google Scholar]
- Palella FJ, Jr, Deloria-Knoll M, Chmiel JS, et al. Survival benefit of initiating antiretroviral therapy in HIV-infected persons in different CD4+ cell strata. Ann Intern Med. 2003;138(8):620–626. doi: 10.7326/0003-4819-138-8-200304150-00007. [DOI] [PubMed] [Google Scholar]
- Parran TV, Adelman CA, Merkin B, et al. Long-term outcomes of office-based buprenorphine/naloxone maintenance therapy. Drug Alcohol Depend. 2010;106(1):56–60. doi: 10.1016/j.drugalcdep.2009.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollack HA, D'Aunno T. HIV testing and counseling in the nation's outpatient substance abuse treatment system, 1995–2005. J Subst Abuse Treat. 2010;38(4):307–316. doi: 10.1016/j.jsat.2009.12.004. [DOI] [PubMed] [Google Scholar]
- Schwartz JS, Lewis CE, Clancy C, et al. Internists' practices in health promotion and disease prevention. A survey. Ann Intern Med. 1991;114(1):46–53. doi: 10.7326/0003-4819-114-1-46. [DOI] [PubMed] [Google Scholar]
- Shirts BH, Perera S, Hanlon JT, et al. Provider management of and satisfaction with laboratory testing in the nursing home setting: results of a national internet-based survey. J Am Med Dir Assoc. 2009;10(3):161–166. doi: 10.1016/j.jamda.2008.08.018. e163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soeffing JM, Martin LD, Fingerhood MI, et al. Buprenorphine maintenance treatment in a primary care setting: outcomes at 1 year. J Subst Abuse Treat. 2009;37(4):426–430. doi: 10.1016/j.jsat.2009.05.003. [DOI] [PubMed] [Google Scholar]
- St Lawrence JS, Montano DE, Kasprzyk D, et al. STD screening, testing, case reporting, and clinical and partner notification practices: a national survey of US physicians. Am J Public Health. 2002;92(11):1784–1788. doi: 10.2105/ajph.92.11.1784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein MD, Cioe P, Friedmann PD. Buprenorphine retention in primary care. J Gen Intern Med. 2005;20(11):1038–1041. doi: 10.1111/j.1525-1497.2005.0228.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strathdee SA, Sherman SG. The role of sexual transmission of HIV infection among injection and non-injection drug users. J Urban Health. 2003;80(4 Suppl 3):iii7–iii14. doi: 10.1093/jurban/jtg078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strathdee SA, Stockman JK. Epidemiology of HIV among injecting and non-injecting drug users: current trends and implications for interventions. Curr HIV/AIDS Rep. 2010;7(2):99–106. doi: 10.1007/s11904-010-0043-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse & Mental Health Services Administration, O. o. A. S. Rockville, MD: 2010. Results from the 2009 National Survey on Drug Use and Health: Volume I. Summary of National Findings. (Office of Applied Studies, NSDUH Series H-38A, HHS Publication No. SMA 10-4586 Findings). [Google Scholar]
- Substance Abuse and Mental Health Services Administration, O. o. A. S. The N-SSATS Report: Infectious Disease Screening. Rockville, MD: 2010. [Google Scholar]
- Sullivan LE, Chawarski M, O'Connor PG, et al. The practice of office-based buprenorphine treatment of opioid dependence: is it associated with new patients entering into treatment? Drug Alcohol Depend. 2005;79(1):113–116. doi: 10.1016/j.drugalcdep.2004.12.008. [DOI] [PubMed] [Google Scholar]
- Sullivan LE, Fiellin DA. Narrative review: buprenorphine for opioid-dependent patients in office practice. Ann Intern Med. 2008;148(9):662–670. doi: 10.7326/0003-4819-148-9-200805060-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan LE, Moore BA, Chawarski MC, et al. Buprenorphine/naloxone treatment in primary care is associated with decreased human immunodeficiency virus risk behaviors. J Subst Abuse Treat. 2008;35(1):87–92. doi: 10.1016/j.jsat.2007.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tracy K, Brown LS, Kritz S, et al. Substance abuse treatment clinician opinions and infectious disease service delivery. J Addict Dis. 2009;28(1):8–12. doi: 10.1080/10550880802544625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow ND, Montaner J. Enhanced HIV testing, treatment, and support for HIV-infected substance users. JAMA. 2010;303(14):1423–1424. doi: 10.1001/jama.2010.421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walley AY, Alperen JK, Cheng DM, et al. Office-based management of opioid dependence with buprenorphine: clinical practices and barriers. J Gen Intern Med. 2008;23(9):1393–1398. doi: 10.1007/s11606-008-0686-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward J, Sanson-Fisher R. Prevalence and detection of HIV risk behavior in primary care: implications for clinical preventive services. Am J Prev Med. 1995;11(4):224–230. [PubMed] [Google Scholar]