Abstract
Purpose
To report the clinical findings of 2 patients with focal choroidal excavation in the macula detected by spectral-domain optical coherence tomography (SD-OCT).
Methods
Three eyes of 2 patients with a focal macular choroidal excavation detected by SD-OCT were studied. The eyes were examined by fundus autofluorescence (FAF), fluorescein angiography, fundus-related microperimetry, and multifocal electroretinography (mfERG).
Results
In spite of a complaint of metamorphopsia, the visual acuity was normal in 2 eyes. SD-OCT demonstrated a choroidal excavation in the macula but the foveal contour was normal in 3 eyes. The excavation involved the outer retinal layers up to the external limiting membrane in all eyes, and a type 2 secondary choroidal neovascularization (CNV) developed in 1 of the 3 eyes. There were areas of hypoautofluorescence in the FAF images, and areas of decreased retinal sensitivity determined by microperimetry. These areas corresponded to the choroidal excavation in all eyes. The P1 amplitudes of the mfERGs were decreased in the fovea of 1 eye without a CNV.
Conclusions
The choroidal excavation remained stable for 3 years in 2 eyes, a secondary CNV developed in 1 eye during the course of the disease. More cases and longer follow-up periods will be necessary to determine the etiology, clinical course, and visual prognosis of eyes with a choroidal excavation.
Key Words: Choroidal excavation, Choroidal neovascularization, Optical coherence tomography
Introduction
An anomalous excavation of the choroid is detected by time-domain optical coherence tomography (OCT) in an eye with good visual acuity and normal appearance of the overlying retina [1]. The analysis of the OCT images is however limited by the inability of the time-domain OCT instrument to obtain images deeper than the choroid. Thus, it is not possible to determine whether the defect involves just the choroid. Due to the recent introduction of the spectral-domain OCT (SD-OCT) more detailed morphological images of the deeper layers of the eye can be obtained. Three patients with similar excavations detected by SD-OCT were described by Wakabayashi et al. [2]. They described 2 patterns of choroidal excavations; excavations that involved the outer retinal layers up to the external limiting membrane (ELM), and excavations that involved only the retinal pigment epithelium (RPE). In both patterns, the sclera was not altered.
Margolis et al. [3] defined a focal choroidal excavation as an area of choroidal excavation in the macular area detected on an SD-OCT scan without evidence of a posterior staphyloma or scleral ectasia. In addition, patients with a choroidal excavation did not have a history of trauma, posterior uveitis, retinal or choroidal vascular disease, or prior retinal or choroidal infections. In their 12 cases, the presence of a choroidal excavation could not be determined on clinical examination or by color photography, and the use of SD-OCT in all patients was necessary to detect the focal choroidal excavation.
We present our findings in 3 eyes of 2 cases of focal macular choroidal excavation which involved the outer retinal layers and were detected by SD-OCT (Spectralis; Heidelberg Engineering, Heidelberg, Germany).
Case Reports
Case 1
A 58-year-old man complained of metamorphopsia in both eyes which he had noticed 2 months earlier. His family and disease histories were unremarkable. His BCVA was 1.2 OD and 1.0 OS, and his refractive errors (spherical equivalent) were −4.5 diopters (D) OD and −3.5 D OS. Slit-lamp examination showed no abnormalities. Fundus examination showed mottling of the RPE beneath and adjacent to the fovea (fig. 1a, b). Enhanced depth imaging OCT (EDI-OCT) demonstrated 2 focal choroidal excavations in the macula of both eyes in spite of a normal fovea contour (fig. 1e, f). The excavations involved the outer retinal layers up to the ELM, i.e. the RPE and photoreceptors. The retinal layers from the outer plexiform layer to the retinal nerve fiber layer were essentially normal. The outer nuclear layer appeared significantly thickened compared to that in the areas not affected by excavation. The ELM band and the photoreceptor inner segment/outer segment junction were preserved at the area of the excavation. The choroidal thickness in the areas not affected by the excavation was measured from the outer border of the RPE to the inner scleral border using EDI-OCT as described [3, 4]. The mean thickness of the uninvolved choroid adjacent to the areas of focal choroidal excavation was 314 μm in the right eye and 360 μm in the left eye.
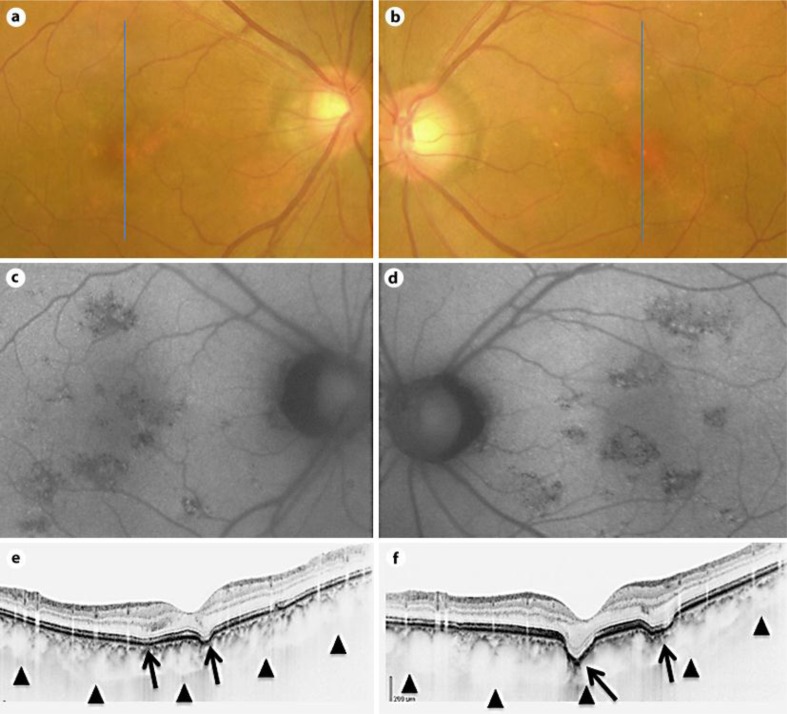
Fig. 1.
Findings in a 58-year-old man with bilateral focal choroidal excavation. a, c, e Images of the right eye. b, d, f Images of the left eye. a, b Fundus photographs on the initial presentation show RPE alterations beneath and adjacent to the fovea. c, d FAF image shows a focal area of hypoautofluorescence. e, f SD-OCT image with enhanced depth imaging through the fovea shows two concave-shaped conforming focal choroidal excavation (arrows) in both eyes. The excavations involved the outer retinal layers up to the ELM. The ELM band and the photoreceptor inner segment/outer segment junction can be seen at the excavation.
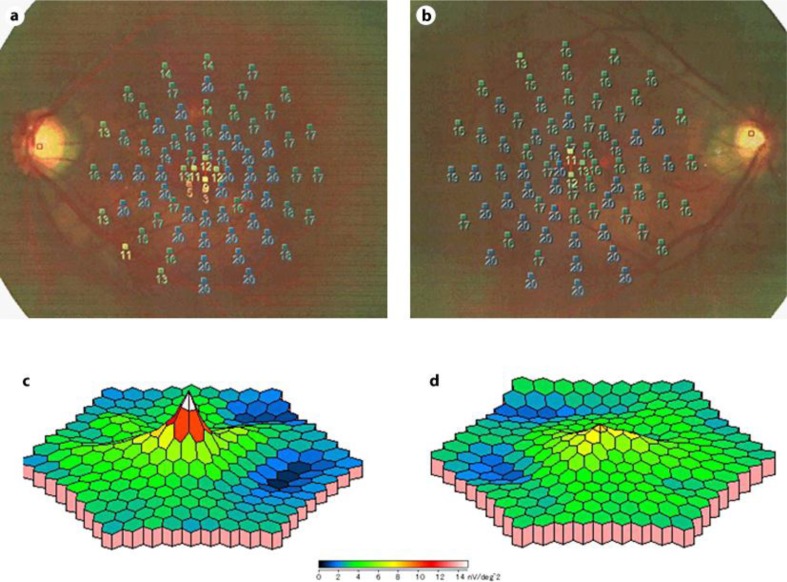
The area of the excavation in the fundus autofluorescent (FAF) images was hypofluorescent (fig. 1c, d). Fluorescein angiography showed hyperfluorescence over the macular lesions consistent with a window defect. Indocyanine green angiography did not show any abnormal findings corresponding to the two lesions. Microperimetry with the MP-1 (Nidek, Gamagori, Japan) showed a decrease in retinal sensitivity in the foveal region of both eyes (fig. 2a, b). The P1 amplitudes of the multifocal electroretinograms (mfERGs) were decreased in the foveal region of the left eye (fig. 2d). The visual acuity, degree of choroidal excavation, and symptoms in both eyes remained unchanged for 3 years.
Fig. 2.
Case 1. a, c Images of the right eye. b, d Images of the left eye. a, b Microperimetry using MP-1 (Nidek, Japan) shows a decrease of retinal sensitivity in the foveal region in both eyes. c, d Results of mfERG using an LE-4100 (Tomey, Japan). Three-dimensional topographic map of the mfERG responses showing a decrease in the P1 response amplitude in the foveal region of the left eye.
Case 2
A 34-year-old woman complained of metamorphopsia in her left eye which she had noticed 1 month prior to our examination. Her family and disease history was unremarkable. Her BCVA was 1.5 OD and 0.9 OS, and refractive error was −4.0 D OD and −6.0 D OS. Slit-lamp examination showed no abnormalities. Fundus examination showed RPE mottling superior to the fovea (fig. 3a).
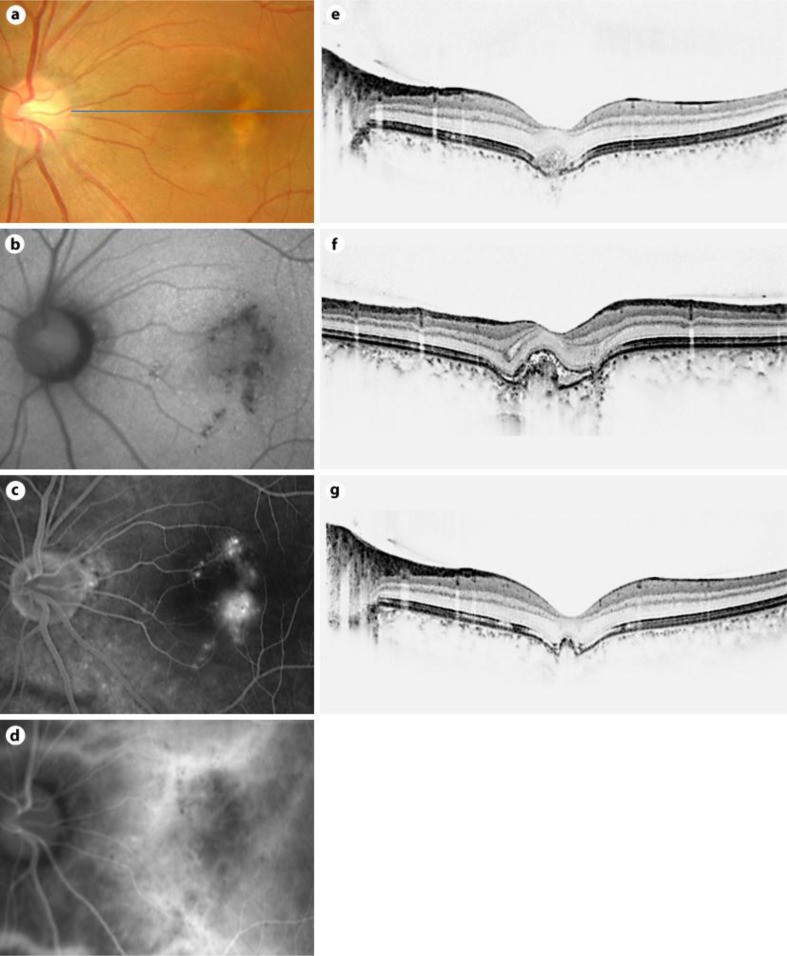
Fig. 3.
Findings in a 34-year-old woman with a focal choroidal excavation accompanied with type 2 CNV in the left eye. a Color photograph shows RPE alterations superior to the fovea. b FAF image shows an irregular area of hypofluorescence. c Fluorescein angiography in the late phase shows a classic CNV in the fovea. d Indocyanine green angiography in the late phase shows a classic CNV in the fovea. e SD-OCT at the initial examination shows a focal choroidal excavation with a type 2 CNV. The ELM band and the photoreceptor inner segment/outer segment junction are indistinct at the excavation. f SD-OCT scan taken 1 month after the initial presentation shows a type 2 CNV with subretinal fluid. g SD-OCT scan taken 5 months later shows a regression of the type 2 CNV after treatment with intravitreal bevacizumab injection.
SD-OCT demonstrated a concave-shaped choroidal excavation associated with type 2 choroidal neovascularization (CNV) in the macula of the left eye (fig. 3e). The ELM band and the inner segment/outer segment junction were indistinct in the area of the excavation. The mean thickness of the uninvolved choroid adjacent to the areas of focal choroidal excavation was 325 μm. FAF showed that the lesion was irregularly hypoautofluorescent (fig. 3b). The fluorescein angiography images showed a type 2 CNV in the fovea with irregular hyperfluorescence superior to the fovea corresponding to the RPE mottling (fig. 3c). Indocyanine green angiography showed hypofluorescence in the central macular lesions, which suggested the presence of impaired choroidal circulation in the lesion. The mfERGs were normal. One month after the initial examination, her BCVA decreased to 0.4 OS accompanied by the presence of subretinal fluid and hemorrhage (fig. 3f). After three monthly intravitreal bevacizumab injections, the BCVA improved to 1.5, and SD-OCT scan showed a regression of the type 2 CNV (fig. 3g). However, the focal choroidal excavation remained unchanged.
Discussion
Focal choroidal excavations have been analyzed using SD-OCT, however, no histopathologic confirmation has been published [2, 3, 5]. Margolis et al. [3] studied 13 eyes of 12 patients with focal choroidal excavations with 1 bilateral case. In 7 of the 13 eyes, SD-OCT showed the outer retinal layers conforming to the RPE alterations within the excavation, i.e. a conforming focal choroidal excavation. There was no separation between the photoreceptor tips and the RPE, and the outer nuclear layer appeared thicker than it did in areas not affected by the excavation. In the other 6 eyes, SD-OCT revealed a separation between the outer retina and the RPE within the excavation, i.e. a nonconforming focal choroidal excavation. In these cases, the photoreceptor tips appeared to be detached from the underlying RPE with the intervening hyporeflective space presumably filled with subretinal fluid.
EDI-OCT showed that the choroidal thickness was significantly thinner within the focal excavation than outside the excavations [2, 3]. EDI-OCT showed that the mean choroidal thickness of the uninvolved choroid was thicker than normal at 319 μm with a range of 244 to 439 μm [3]. This is consistent with our findings. Margolis et al. [3] reported that 10 of the 13 eyes were myopic, and the mean refractive error was −3.54 D with a range of −6.00 to −8.00 D. In our cases, all eyes had moderate to high myopia. In addition, Margolis et al. [3] reported that all 13 eyes with focal choroidal excavation had varying degrees of foveal pigmentary changes that were usually hypoautofluorescent on FAF. Our FAF findings were consistent with the report of Margolis et al. [3].
Abe et al. [5] reported smaller mfERG amplitudes for the two eccentric rings in eyes with nonconforming focal choroidal excavation. Wakabayashi et al. [2] reported that the mfERGs were normal in 2 eyes with conforming focal choroidal excavation. Margolis et al. [3] reported that the retinal sensitivity within the excavation measured by microperimetry was normal in one eye and decreased in one eye. On the other hand, the central visual field measured using Humphry Field Analyzer was reported to be normal in 3 eyes [2]. Our Case 1 had bilaterally decreased P1 amplitude of the mfERGs and decreased foveal sensitivity by microperimetry indicating that the macular function was slightly depressed.
Margolis et al. [3] reported that most focal choroidal excavation remained stable but a secondary CNV developed in one eye of their patients. Consistent with their report, our Case 2 developed type 2 CNV which regressed after intravitreous bevacizumab. Even after CNV regression, the focal choroidal excavation remained unchanged in this case.
In conclusion, we presented 3 eyes of 2 patients with focal choroidal excavation. Case 1 is the second reported case with bilateral focal choroidal excavation, and Case 2 is the second reported case with focal choroidal excavation and secondary type 2 CNV. Further prospective studies with more cases of eyes with focal choroidal excavation are necessary to determine the etiology, clinical course, and visual prognosis.
Disclosure Statement
The authors have no conflicts of interest to disclose.
References
- 1.Jampol LM, et al. Diagnostic and therapeutic challenges. Retina. 2006;26:1072–1076. doi: 10.1097/01.iae.0000248819.86737.a5. [DOI] [PubMed] [Google Scholar]
- 2.Wakabayashi Y, et al. Unilateral choroidal excavation in the macula detected by spectral-domain optical coherence tomography. Acta Ophthalmol. 2010;88:e87–e91. doi: 10.1111/j.1755-3768.2010.01895.x. [DOI] [PubMed] [Google Scholar]
- 3.Margolis R, et al. The expanded spectrum of focal choroidal excavation. Arch Ophthalmol. 2011;129:1320–1325. doi: 10.1001/archophthalmol.2011.148. [DOI] [PubMed] [Google Scholar]
- 4.Spaide RF. Enhanced depth imaging optical coherence tomography of retinal pigment epithelial detachment in age-related macular degeneration. Am J Ophthalmol. 2009;147:644–652. doi: 10.1016/j.ajo.2008.10.005. [DOI] [PubMed] [Google Scholar]
- 5.Abe S, Yamamoto T, Kirii E, Yamashita H. Cup-shaped choroidal excavation detected by optical coherence tomography: a case report. Retinal Cases Brief Rep. 2010;4:373–376. doi: 10.1097/ICB.0b013e3181babe7e. [DOI] [PubMed] [Google Scholar]