Abstract
Objective
To develop a simple clinical scoring system for severity of illness to help prioritize care and predict outcome in emergency department.
Methods
Prospective hospital based observational study. Out of a total of 874 children who attended emergency department in one year, 777 were included in the study. Data was collected at the time of admission in emergency department. The baseline information like age, gender, etc and variables of ‘toprs’ score viz temperature, oxygen saturation, pulse rate, respiratory rate, sensorium and seizures were recorded. Variables were categorized as normal (score zero) or abnormal (score 1) based on systemic inflammatory response syndrome (SIRS) criteria and criteria mentioned in advanced pediatric life support (APLS) and the total scores were computed for each child. The outcome (death/discharge) was correlated with the study variables and total score. The predictive ability of score was calculated using receiver operating characteristic (ROC) curve analysis.
Findings
Of the six variables, temperature, oxygen saturation and respiratory rate were found to be significantly associated with mortality. Mortality increased with the increase in the number of abnormal variables. Based on the regression coefficients, maximum possible score was 6.68. The predictive ability of score was 81.7 calculated using ROC curve. Maximum discrimination was observed at a score of 2.5.
Conclusion
For triage in emergency, any patient with 2 or more abnormal variables should be closely monitored and evaluated. These patients require admission as they have a potential risk of death.
Keywords: Outcome Assessment, Triage, Emergency Room, Pediatrics
Introduction
Identification and triage of seriously ill patients visiting emergency department is very important for prioritization of care and answering parent's queries about outcome, hospital stay and cost of treatment especially in developing countries like India where medical insurance of public is not developed yet. Early recognition of serious illness might reduce the morbidity and mortality in sick patients. Most of the existing scoring systems developed for intensive care unit (ICU) patients and neonates, are not executed at admission, hence these are not useful for triage [1–5]. Furthermore these are exhaustive and include multiple physical and laboratory variables making them cost and labor intensive and are thus difficult to implement in the emergency department. Simplified guidelines for the emergency care of sick children developed by Sandy G et al aimed at improving the triage and initiation of appropriate emergency treatment did not assess the outcome [6]. Measurement of vital signs is routine practice for children attending emergency department [7]. In the present study, a simple scoring system ‘TOPRS’ has been evolved using only physical variables to predict severity of illness and outcome in emergency department.
Subjects and Methods
The present study is a prospective teaching hospital based observational study. A sample of 874 consecutive children attending the emergency department over a period of one year (Jan – Dec 2009) were included, out of which 97 patients who left against medical advice or admitted only for one day were excluded. The remaining 777 patients finally formed the sample for study. Six clinical variables were noted at the time of admission of patients to emergency department. These included Temperature, Oxygen saturation, Pulse rate, Respiratory rate, Sensorium and Seizures. Axillary temperature was measured using a mercury thermometer. Oxygen saturation was measured using a pulse oximeter. These variables were divided into normal and abnormal using the standard SIRS criteria and criteria outlined in pediatric advanced life support (Table 1) [8, 9].
Table 1.
Scoring of abnormal clinical variables
| Variable | Abnormal range |
|---|---|
| Temperature | >38°C, <36°C |
| Oxygen saturation | < 90% |
| Heart rate | Infant >160/min |
| Child >150/min | |
| Respiratory rate | Infant >60/min |
| Child >50/min | |
| Sensorium | Loss of sensorium |
| Seizures | Present |
Normal Score – 0, Abnormal score – 1
Normal variable was given a score of zero and abnormal variable a score of one. Total score was computed for each child. The data obtained at this juncture was kept in a sealed envelope and numbered. The patients were sent and managed in the respective areas like intensive care unit and ward by the doctors and nursing staff as per standard protocols. The initial data were kept confidential and were not informed to the attending doctors. The final outcome was recorded at the time of discharge/death. The primary outcome variable included the final outcome (death/discharge). The ethical clearance and permission from the Institutional Review Board was obtained prior to initiation of the study.
The data was analyzed using SPSS-16 software. Odds ratio with 95% confidence intervals were calculated for each variable. Chi square test was used when more than two ordered groupings were present. A multiple logistic regression analysis was done to assess the magnitude of association. A receiver operating characteristic (ROC) curve analysis was done to find out predictive ability of score.
Findings
Of the 777 children studied, 157 were neonates, 28.5% were females while 71.5% were males. 127 children died in the hospital. The association of each of variables studied with the outcome (discharge/death) is shown in Table 2. Temperature, oxygen saturation and respiratory rate were found to have significant effect on the outcome while pulse rate, sensorium and seizures did not affect the mortality significantly. A multiple logistic regression analysis was done to determine the magnitude of association of each variable with mortality (Table 3).
Table 2.
Association of study variables with mortality
| Variable | Survived | Died | Odds Ratio | P value | |||
|---|---|---|---|---|---|---|---|
| No. | %age | No. | %age | ||||
| Temperature | Normal | 600 | 86.21 | 96 | 13.79 | 3.88 | 0.04 |
| Abnormal | 50 | 61.73 | 31 | 38.27 | 1.10–4.06 | ||
| O2 Saturation | Normal | 644 | 88.83 | 81 | 11.17 | 60.95 | <0.01 |
| Abnormal | 6 | 11.54 | 46 | 88.46 | 14.17–93.61 | ||
| Pulse Rate | Normal | 568 | 87.25 | 83 | 12.75 | 3.67 | 0.2 |
| Abnormal | 82 | 65.08 | 44 | 34.92 | 0.85–2.67 | ||
| Respiratory Rate | Normal | 539 | 92.77 | 42 | 7.23 | 9.83 | <0.01 |
| Abnormal | 111 | 56.63 | 85 | 43.37 | 3.74–10.52 | ||
| Sensorium | Normal | 592 | 85.67 | 99 | 14.33 | 2.89 | 0.06 |
| Abnormal | 58 | 67.44 | 28 | 32.56 | 0.93–10.80 | ||
| Seizures | Normal | 589 | 84.99 | 104 | 15.01 | 2.14 | 0.9 |
| Abnormal | 61 | 72.62 | 23 | 27.38 | 0.26–3.35 | ||
Table 3.
Weight (regression coefficient) for each variable: Logistic regression analysis
| Variable | Weight |
|---|---|
| Temperature | 0.75 |
| Oxygen Saturation | 2.60 |
| Pulse Rate | 0.41 |
| Respiratory Rate | 1.84 |
| Sensorium | 1.16 |
| Seizures | −0.08 |
| Maximum Possible Score | 6.68 |
| Maximum Observed Score | 6 |
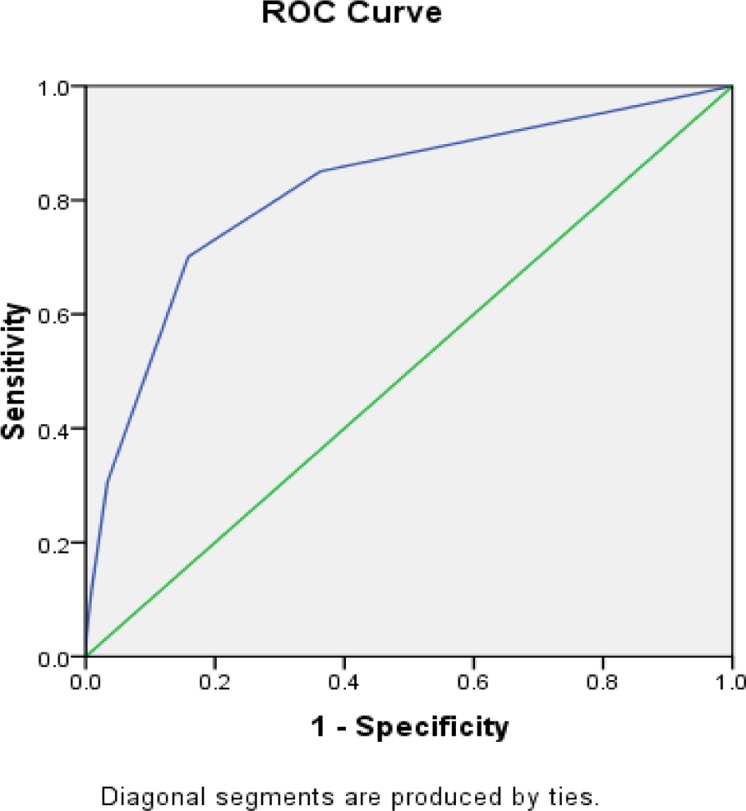
The maximum possible score for any child was found to be 6.68. However, in this study the maximum observed score was 6. It was observed in this study that increase in the number of abnormal variables of TOPRS score caused a statistically significant increase in the mortality. A mortality of 4.4% was observed in children with zero score while 80% of children having a score of 5 at admission died. A child with score of 6 had an odds ratio of 615 of dying in the hospital as compared to a child with a score of less than 1 (Table 4). ROC analysis shows the predictive ability of score as 81.7% (Fig. 1). Maximum discrimination was observed for a score of 2.5 (sensitivity-79.6, specificity-74.43).
Table 4.
Outcome at different scores
| Score | Survived | Died | Odds Ratio | 95% CI | Total | ||
|---|---|---|---|---|---|---|---|
| No. | % age | No. | % age | ||||
| 0 | 414 | 95.61 | 19 | 4.39 | 433 | ||
| 1 | 133 | 87.50 | 19 | 12.50 | 1 | 152 | |
| 2 | 81 | 61.83 | 50 | 38.17 | 3.26 | 2.51-3.74 | 131 |
| 3 | 16 | 40.00 | 24 | 60.00 | 9.98 | 3.68–28.74 | 40 |
| 4 | 5 | 33.33 | 10 | 66.67 | 40.11 | 9.15–147.12 | 15 |
| 5 | 1 | 20.00 | 4 | 80.00 | 200.73 | 29.51–874.21 | 5 |
| 6 | 0 | 0.00 | 1 | 100.00 | 615.32 | 47.68–8853.41 | 1 |
CI: Confidence Interval
Fig. 1.
Receiver Operating Characteristic (ROC) curve
Discussion
Triage is very important in the emergency department. It helps to ensure that patients are treated in order of their severity of illness and the treatment is appropriate and timely. For this a simple scoring system is required to predict outcome. It should also be easy to use so that it can be applied at first contact with patient. One of the earliest physiological scoring systems for children was physiology stability index (PSI) in which score was calculated from the worst of 34 values from routinely measured variables over first day of PICU stay[10].
To make it less tedious, PRISM scoring system was evolved from it with 14 variables [11]. It used both physical and laboratory variables so was not useful for triage. Pediatric index of mortality, on the other hand was assessed directly on admission to PICU [12]. All these scoring systems are either for ICU patients or requiring extensive laboratory variables and observation. Thus, these systems can't be used in emergency department and precious time is lost as laboratory investigations take time. These drawbacks make them unsuitable for use in developing country like India. Emergency triage, assessment and treatment (ETAT) guidelines have been formulated by WHO for use in developing countries. The drawback with this system is that it requires specialized training program for doctors and other health care staff for implementation. In a study conducted by M. Thompson et al, it was concluded that a combination of vital signs can be used to differentiate children with serious infections from those with less serious infections in a pediatric assessment unit [13].
In the present study, we hypothesized that physical variables alone can be helpful in predicting outcome. So the biochemical and other variables were excluded and the physical variables were taken based on the SIRS criteria and its continuum. No special training is required for implementation and can be applied immediately when the patient comes in emergency. A total of six physical variables were studied, out of which 3 variables viz temperature, oxygen saturation and respiratory rate were having a significant effect on outcome on univariate analysis. It was observed that as the number of abnormal variables increased, the mortality also increased progressively. The predictive ability of the score was found to be 81.7% on ROC curve analysis.
In a study conducted by Manoj Gupta et al simultaneously in India and England, severity of illness was assessed using SICK score, the predictive ability of the score was found to be 84.1% [14]. Maximum discrimination was seen at a score of 2.5 with sensitivity of 79.6 and specificity of 74.4. Thus, any patient presenting in emergency department with 2 or more abnormal variables at admission should be treated as serious requiring admission as there is a potential risk of death. Cut off scores were not proposed in study conducted by Manoj Gupta et al as it required larger sample size[14]. Morley CJ et al developed a baby check scoring system on the basis of 28 predefined symptoms and 47 physical signs and found it to be useful to help quantify the severity of baby's systemic illness. However, they did not study the outcome[2].
Limitation of the study: However in the current study interpersonal variability among attending doctors may exist which is not accounted for.
Conclusion
A simple clinically developed scoring system 'TOPRS' will be useful in predicting severity of illness and also outcome at admission itself in emergency department.
Acknowledgment
Authors thank Dr Rupinder Singh for his help during the study.
Conflict of Interest
None
References
- 1.Shann E, Pearson G, Slater A, Wilkinson K. Pediatric index of mortality (PIM): A mortality prediction model for children in intensive care. Intensive Care Med. 1997;23(2):201–7. doi: 10.1007/s001340050317. [DOI] [PubMed] [Google Scholar]
- 2.Morley CJ, Thornton AJ, Cole T J, et al. Baby check: a scoring system to grade the severity of acute systemic illness in babies under 6 months old. Arch Dis Child. 1991;66(1):100–5. doi: 10.1136/adc.66.1.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mc Weeny PM, Emery JL. Unexpected post neonatal deaths (cot deaths) due to recognizable disease. Arch Dis Child. 1975;50(3):191–6. doi: 10.1136/adc.50.3.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.de Courcy-Wheeler R, Wolfe CDA, Fitzgerald A, et al. Use of the CRIB (clinical risk index for babies) Arch Dis Child. 1995;73(1):F32–F36. doi: 10.1136/fn.73.1.f32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kadivar M, Sagheb S, Bavafa F, et al. Neonatal mortality risk assessment in a neonatal intensive care unit (NICU) Iran J Pediatr. 2007;17(4):325–31. [Google Scholar]
- 6.Mathur P, Dawar S. Morbidity Index; An objective scoring system for predicting neonatal outcome. J Clin Diagn Res. 2007;1(1):10–16. [Google Scholar]
- 7.Grove S, Tamburlini G, Molyneux E, et al. Development and simplified basis of simplified guidelines for emergency triage assessment and treatment in developing countries. Arch Dis Child. 1991;81(6):473–7. doi: 10.1136/adc.81.6.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sun D, Aikawa N. The natural history of the systemic inflammatory response syndrome and the evaluation of SIRS criteria as a predictor of severity in patients hospitalized through emergency services. Keio J Med. 1999;48(1):28–37. doi: 10.2302/kjm.48.28. [DOI] [PubMed] [Google Scholar]
- 9.Mackway-Jones K, Molyneux E, Phillips B, Weeteska S. The Practical Approach. BMJ books. 3rd ed. London: Panther publishers; 2001. Advanced Pediatrics Life support; pp. 71–8. [Google Scholar]
- 10.Yeh TS, Pollack MM, Ruttimann UE, et al. Validation of a Physiologic Stability Index for use in critically iII infants and children. Pediatric Res. 1984;18(5):445–51. doi: 10.1203/00006450-198405000-00011. [DOI] [PubMed] [Google Scholar]
- 11.Pollack MM, Ruttimann UE, Getson PR. The pediatric risk of mortality (PRISM) scores. Crit Care Med. 1988;16(11):1110–6. doi: 10.1097/00003246-198811000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Slater A, Shann F, Pearson G. Pediatric Index of Mortality (PIM) Study Group: PIM 2: a revised version of the Pediatric Index of Mortality. Intensive Care Med. 2003;29(2):278–85. doi: 10.1007/s00134-002-1601-2. [DOI] [PubMed] [Google Scholar]
- 13.Thompson MJ, Coad N, Harnden A, et al. How well do vital signs identify children with serious infections in paediatric emergency care? Arch Dis Child. 2009;94(11):888–93. doi: 10.1136/adc.2009.159095. [DOI] [PubMed] [Google Scholar]
- 14.Gupta MA, Chakrabarty A, Halstead R, et al. Validation of “Signs of inflammation in children that kill” (SICK) score for immediate non invasive assessment of severity of illness. Italian J Pediatr. 2010;36:35. doi: 10.1186/1824-7288-36-35. [DOI] [PMC free article] [PubMed] [Google Scholar]