Abstract
Background: High doses of cisplatin and cranial radiotherapy (CRT) have been reported to cause irreversible hearing loss. The objective of this study was to examine the influence of cranial irradiation on cisplatin-associated ototoxicity in children with pediatric malignancies.
Methods: Serial audiograms were obtained for 33 children, age <16 years, treated with cisplatin-based chemotherapy (90-120 mg/m2 per cycle) with or without CRT. Eligible patients included those with normal baseline audiometric evaluations and without significant exposure to other ototoxic drugs. We defined significant hearing loss as a hearing threshold ≥30 dB at 2,000-8,000 Hz frequencies.
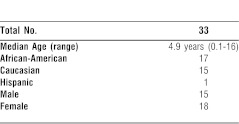
Results: The median age of our study population was 4.9 years (range 6 weeks to 16 years), and the male to female ratio was 0.8:1. The study population consisted of 15 Caucasians, 17 African-Americans, and 1 Hispanic. Fourteen patients had brain tumors, and 19 had other solid tumors. Thirteen patients were exposed to CRT, and 20 were not. Bilateral hearing loss was observed in 24/33 (73%) patients, with severe/profound (≥70 dB) impairment in 10/33 (30%) of all patients. Young age (<5 years), CRT, and brain tumors were independent prognostic factors predicting hearing loss.
Conclusion: The study demonstrated a high incidence of hearing loss in children treated with cisplatin and CRT. Consequently, we recommend monitoring these children for the early detection of hearing loss.
Keywords: Cisplatin, cranial irradiation, ototoxicity, pediatric brain tumor
INTRODUCTION
Discovered more than 30 years ago,1 cisplatin remains one of the most widely used anticancer agents in the world. Cisplatin is active against most pediatric solid tumors, including brain tumors, neuroblastomas, osteosarcomas, and germ-cell tumors.2,3 Combined sequentially with radiotherapy, the drug has successfully been used in multimodal regimes in children with brain tumors and other solid tumors.2,3 The combination of cisplatin with radiotherapy potentiates the antitumor effects of the agents without increasing toxicity.4 Improvement in therapeutic ratio may be limited in certain situations by overlapping toxicities that result in the enhancement of site-specific damage to normal tissues.4
High cumulative doses of cisplatin5,6 and cranial radiotherapy (CRT)7,8 have both been reported to be independently responsible for irreversible high-frequency sensorineural hearing loss that may ultimately involve the speech range frequencies. Reports conflict regarding the ototoxicity observed in brain tumor patients receiving cranial irradiation. Schell et al9 reported hearing loss with lower cumulative cisplatin doses at 270 mg/m2 in CRT patients, while Kretschmar et al10 reported acceptable ototoxicity with cisplatin doses at 300 mg/m2 in similarly irradiated patients.
The present study examined the effect of CRT and cisplatin on ototoxicity in children.
METHODS
We prospectively recorded serial audiometric evaluations in 33 children with cancer, age ≤16 years at Children's Hospital, New Orleans. Only children with normal audiograms and negative history of prior exposure to ototoxic drugs who received cisplatin-based chemotherapy with or without cranial radiation were eligible for the study. We recorded patient characteristics in detail: age at diagnosis, sex, race, type and extent of disease, and dosing of cisplatin and CRT.
Serial audiograms were obtained prior to each treatment with cisplatin as well as 3-4 weeks after the last dose of cisplatin. Auditory function was evaluated using the audiologic technique appropriate for the age and cognitive ability of each patient. Pure-tone threshold audiometry was used in most patients (n=27). Younger patients who were unable to cooperate for pure-tone testing were tested by soundfield behavioral testing (n=6). Nine auditory brainstem-evoked response (ABR) tests were performed. Six ABR tests confirmed the results of behavioral audiometric testing, and 3 provided a baseline in patients aged 3 months to 4 years. These measurements were not included in the analysis because ABR tests lack frequency specificity.
Hearing threshold was determined for each ear at stimulus frequencies of 500, 1,000, 2,000, 3,000, 4,000, 6,000, and 8,000 Hz in patients undergoing pure-tone threshold testing and at 500, 1,000, 2,000, 3,000, 4,000, and 6,000 Hz for patients needing soundfield behavioral audiometry. We analyzed data for the test frequencies of 2,000, 3,000, 4,000, 6,000, and 8,000 Hz only. A hearing threshold ≥30 dB hearing loss was considered significant for hearing impairment. We averaged minimum hearing levels for the right and left ears. Normal or acceptable variability in hearing threshold for any patient was 10 dB; hearing threshold 0-29 dB hearing loss was defined as normal. Mild, moderate, and severe/profound hearing loss were defined as hearing thresholds in the range of 30-49 dB, 50-69 dB, and ≥70 dB, respectively. Whenever possible, audiometric testing was performed in an IAC (Industrial Acoustics Co., Winchester, UK) double-walled audiometric sound booth using a Grason-Stadler (Eden Prairie, MN) GSI 10. When the clinical situation warranted (eg, the patient was started on chemotherapy on the same day), bedside pure-tone testing was performed with the portable Madsen Impedance Audiometer ZS76-IB (Otometrics, Taastrup, Denmark). All audiometric equipment was calibrated to American National Standards Institute S3.6-1969 (R 1973) S5.26-1981 standards on a quarterly basis.
Patients with brain tumors received cisplatin at 90 mg/m2 as a 6-hour infusion every 3-4 weeks along with vincristine and cyclophosphamide. Patients with other solid tumors received cisplatin in doses of 90-120 mg/m2 per course in combination with etoposide phosphate, adriamycin, and cyclophosphamide. All patients received adequate hydration and mannitol (to ensure good diuresis) with cisplatin therapy.
Statistical Analysis
Arithmetic mean and median were calculated by standard methods, and P values were considered significant below .05. Normally distributed continuous variables were analyzed using the analysis of variance (ANOVA) or the Student t test. Continuous variables that were not normally distributed were analyzed using the Mann-Whitney U test. Either the chi-square or Fisher exact test was used to analyze crosstabs, and appropriate multivariate analyses were carried out with logistic regression.
RESULTS
Table 1 presents the age, sex, and racial distribution of the 33 children evaluated. As shown in Table 2, brain tumors constituted 42% (14) of the tumors; the rest included neuroblastomas (9), osteosarcomas (5), rhabdomyosarcomas (4), and dysgerminoma (1).
Table 1.
Patient Characteristics
Table 2.
Median Cumulative Dose of Cisplatin and Cranial Irradiation by Tumor Type
A total of 174 audiometric evaluations were performed, including pure tone (n=122) and soundfield (n=52). All baseline measurements were within normal limits. Twenty-seven (82%) of the 33 children evaluated developed hearing loss as defined by hearing threshold ≥30 dB at 2,000-8,000 Hz stimulus frequency. Bilateral hearing loss was observed in 24/27 children and unilateral hearing loss in 3/27. Mild, moderate, severe, and profound hearing loss occurred in 5, 12, 5, and 5 patients, respectively.
Hearing loss was first detected at 8,000 Hz. A significant median threshold shift of 20 dB was noted at this frequency (P=.02) after the first treatment cycle with cisplatin (90-120 mg/m2). A greater shift (57.5 dB) at the same frequency became more significant (P<.0001) after the third cycle of cisplatin. With higher cumulative doses of cisplatin, lower frequencies were progressively involved. Hearing loss in the speech range occurred in 10/33 (30%) of the patients. Of the 6 children whose hearing was unimpaired after completing treatments, only 1 had a brain tumor and had not received cranial radiation because of age >1 year at diagnosis. The median cumulative dose of cisplatin administered was higher in patients developing hearing loss (400 mg/m2) than in patients with unimpaired hearing (360 mg/m2), but the difference was not statistically significant.
The median cumulative cisplatin dose at which hearing loss was first detected was 200 mg/m2. The dose was significantly lower in brain tumor patients (180 mg/m2) than in non–brain tumor patients (330 mg/m2) (P<.008 using the Mann-Whitney U test, non-parametric) (Table 3). Of the 14 patients with brain tumors, only 13 received CRT. All 13 brain tumor patients receiving CRT developed hearing loss, and 14 of the 19 non–brain tumor patients (74%) developed hearing loss (P<.005 using chi-square analysis). Logistic regression analysis showed CRT to be an independent and statistically significant factor in the incidence of hearing loss. The odds ratio for patients receiving CRT was 14.4, ie, these patients were 14.4 times more likely to demonstrate hearing loss compared to non-CRT patients. Patients receiving CRT had a 2.2 times greater likelihood of developing severe to profound hearing loss compared to the non-CRT group. Seven patients with CRT and 3 with no CRT had severe to profound hearing loss (≥70 dB). Severe to profound hearing loss occurred in 4 of 7 patients receiving postchemotherapy CRT and in 3 of 6 receiving CRT before cisplatin (P=.59, Fisher exact test).
Table 3.
Median Cumulative Cisplatin Dose at Which Hearing Loss Was First Detected
The median cumulative cisplatin dose administered to non–brain tumor patients was higher (480 mg/m2) than that given to brain tumor patients (270 mg/m2) and higher for the non-CRT patients (507 mg/m2) than for those receiving CRT (347 mg/m2). In the present study, although cumulative chemotherapy dose was not statistically significant in relation to hearing loss, we found a definite trend toward increased incidence of hearing loss with higher doses of cisplatin (P=.722, Student t test; multiple regression, P=.18). The median cumulative cisplatin dose was higher (400 mg/m2) in patients developing hearing loss than in those with unimpaired hearing (360 mg/m2, P=NS).
Age was the only significant factor other than CRT and brain tumor that influenced hearing loss in our study. Age was observed to be inversely related to the likelihood of developing hearing loss, with young children (≤5 years) demonstrating a higher incidence of hearing loss (Student t test assuming equal variances, P=.03). With each year of younger age, a patient was 1.24 times more likely to demonstrate hearing loss (odds ratio). The mean hearing threshold at the speech range was significantly higher: 32 dB in the ≤5 years group compared to 9.8 dB in children >5 years (P=.001, ANOVA).
Binaural amplification was recommended in 8 of 27 patients who developed hearing loss. One family refused, so 7 children were fitted with binaural hearing aids. Five of the 7 patients were alive at their most recent follow-up and are attending schools in regular classrooms. Two of the 5 are receiving speech therapy with an emphasis on articulation.
Hearing in 2 of 10 patients with speech range frequency deficits continued to deteriorate during off-therapy follow-up. One patient showed a 30-40 dB decrease bilaterally for the frequencies 2,000-6,000 Hz at 6 months with no additional change at 12, 18, and 24 months. The other patient had a 10-25 dB decrease at 3,000-6,000 Hz bilaterally, detected on an audiogram performed after more than 24 months off therapy.
DISCUSSION
In this study of 33 children with various solid tumors treated with cisplatin-based chemotherapy, hearing loss was compared in 2 basic groups: those with brain tumors versus those with other cancers. All patients with brain tumors except 1 and none of the non–brain tumor group received CRT. Comparative hearing loss was also analyzed with respect to CRT, age, and cisplatin dose. Most patients received 3 to 6 courses of cisplatin (range: 90-120 mg/m2).
The overall occurrence of bilateral, high-frequency (8,000 Hz) hearing loss in this heterogeneous group of solid tumor patients was 73% (24/33). Severe/profound hearing loss (≥70 dB) at 8,000 Hz was observed in 10/33, and clinically relevant speech range frequencies (<4,000 Hz) were impaired in 10/33 patients. McHaney et al5 reported a similarly high incidence of hearing loss (>4,000 Hz) in children treated with a ≥450 mg/m2 cumulative dose of cisplatin. Schell et al9 reported minimum hearing loss in 71% of patients exposed to the median cumulative cisplatin dose of 360 mg/m2, with substantial (≤50 dB) hearing loss and speech range involvement in 11% and 61% of the CRT group, respectively. While Cohen et al11 reported 97% (33/34) hearing loss (≥4,000 Hz) in patients treated with cisplatin and with CRT, Kretschmar et al10 reported a lower incidence of 47% with 300 mg/m2 of cisplatin and 27% occurring in the speech range frequencies.
The pattern of hearing loss observed in our patients was similar to that reported by others,5-15 with initial impairment occurring in the high-frequency range (8,000 Hz). If subsequent doses of cisplatin worsened hearing, the doses progressively affected lower frequencies, ultimately involving the speech range (4,000 Hz).
Hearing loss was usually bilateral (24/27) and permanent.5-11 Three patients had mild hearing loss involving only 1 ear. No long-term recovery was observed in any of the 7 patients fitted with binaural aids. Progression of hearing loss was seen in 2 patients with severe to profound hearing loss who had not received CRT. This pattern is better documented in studies demonstrating the late effects of radiotherapy to the cranium.8,16,17 We recommended, as have others who have reported progression after the cessation of therapy,16 long-term audiologic monitoring after completion of treatment.
In multivariate analysis, CRT and brain tumors were both independent prognostic variables predicting hearing loss. Schell et al9 reported a significantly higher probability of developing hearing loss, as well as 20-30 dB higher thresholds, in brain tumor patients receiving CRT than in brain tumor patients not irradiated, although the numbers in each group are small. Cohen et al11 observed high-frequency hearing loss in 33/34 children with brain tumors who were treated with surgical resection, irradiation, and cisplatin-based chemotherapy.
Kretschmar et al10 discussed the issue of timing cisplatin in relationship to CRT, which may affect the extent of observed ototoxicity. They reported a low (11%) incidence of speech range hearing loss in children receiving cisplatin before irradiation. Walker and colleagues7 reported severe hearing loss in all 4 patients who received cisplatin simultaneously within 3 to 10 months of CRT. Similarly McHaney et al5 reported an 82% probability of a hearing threshold ≥50 dB at ≥3,000 Hz after 360 mg/m2 of cisplatin after prior CRT and recommended amplification in 80% of these patients, compared to 33% of patients treated with similar doses of cisplatin alone.16,17
The enhanced ototoxicity of cisplatin when given after irradiation has also been documented in pediatric series by McHaney et al,5 Walker et al,7 Khan et al,12 Sexauer et al,13 Granowetter et al,15 and Mahoney et al.18 We did not note a difference between the pre- and postcisplatin irradiated groups, which may have been confounded by the high incidence of hearing loss in irradiated patients. Suggested mechanisms for enhanced ototoxicity with precisplatin CRT include enhanced penetration of the drug, hypoxic cell sensitization, and weakening of the differentiating aspects of the cochlear cytoarchitecture.10,19
We observed a definite trend toward increased incidence of hearing loss with higher doses of cisplatin. The lack of a statistically significant trend in our study, compared to others,5,9 may well be explained by the confounding effect of CRT that led to hearing loss in all exposed patients. Larger studies with patients receiving uniform doses of cisplatin are more likely to demonstrate this effect. The initial results of studies using carboplatin in pediatric medulloblastomas20 and other childhood malignancies21 suggest responses and survival similar to those of cisplatin-based and other drug combinations but with a lower incidence of ototoxicity.
Age was an independent prognostic factor determining hearing loss. Patients ≤5 years were more likely to develop hearing loss than children >5 years. This pattern, although reported by some investigators,5,6,8 was not observed by others.11,12,22 Researchers have suggested that this result may stem from the increased susceptibility of the younger patients' less mature cochlear and vascular systems to cisplatin ototoxicity.5 Hence, younger patients especially would benefit from serial audiometric testing. Children too young for pure-tone audiometry should have ABR testing and/or otoacoustic emission testing.
Some new reports discuss a potential novel treatment for cisplatin-induced ototoxicity. Animal experiments have suggested that hyperbaric oxygen therapy may reverse or prevent auditory loss secondary to cisplatin exposure.23 An animal experiment conducted in Brazil supported the use of amifostine as an otoprotector against cisplatin-induced ototoxicity.24 However, one American clinical trial on the role of amifostine in preventing ototoxicity induced by high-dose cisplatin combined with etoposide and bleomycin showed discouraging results.25
Hearing loss in younger children significantly affects the acquisition of speech and language skills. Close monitoring of speech and language development with aural rehabilitation and speech therapy interventions for affected children is essential. Knowledge of early brain development mandates optimal hearing in infancy to lay the groundwork for later language skills.
CONCLUSION
This study demonstrates a high incidence of hearing loss in children with brain tumors treated with cisplatin and CRT. Age, CRT, and tumor location were independent prognostic factors predicting hearing loss. We recommend serial monitoring of these patients for the early detection of hearing loss. Establishing the treatment sequence of cisplatin and CRT and developing equally effective and less ototoxic alternative drugs such as carboplatin appear to be other major areas of interest in this field.
Footnotes
The authors have no financial or proprietary interest in the subject matter of this article.
This article meets the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties Maintenance of Certification competencies for Patient Care and Medical Knowledge.
REFERENCES
- 1.Rosenberg B, Van Camp L, Krigas T. Inhibition of cell division in Escherichia coli by electrolysis products from a platinum electrode. Nature. 1965 Feb 13;205:698–699. doi: 10.1038/205698a0. [DOI] [PubMed] [Google Scholar]
- 2.Packer RJ, Sutton LN, Elterman R, et al. Outcome for children with medulloblastoma treated with radiation and cisplatin, CCNU, and vincristine chemotherapy. J Neurosurg. 1994 Nov;81(5):690–698. doi: 10.3171/jns.1994.81.5.0690. [DOI] [PubMed] [Google Scholar]
- 3.Rosen EM, Cassady JR, Frantz CN, Kretschmar C, Levey R, Sallan SE. Neuroblastoma: the Joint Center for Radiation Therapy/Dana-Farber Cancer Institute/Children's Hospital experience. J Clin Oncol. 1984 Jul;2(7):719–732. doi: 10.1200/JCO.1984.2.7.719. [DOI] [PubMed] [Google Scholar]
- 4.Steel GG, Peckham MJ. Exploitable mechanisms in combined radiotherapy-chemotherapy: the concept of additivity. Int J Radiat Oncol Biol Phys. 1979 Jan;5(1):85–91. doi: 10.1016/0360-3016(79)90044-0. [DOI] [PubMed] [Google Scholar]
- 5.McHaney VA, Thibadoux G, Hayes FA, Green AA. Hearing loss in children receiving cisplatin chemotherapy. J Pediatr. 1983 Feb;102(2):314–317. doi: 10.1016/s0022-3476(83)80551-4. [DOI] [PubMed] [Google Scholar]
- 6.Weatherly RA, Owens JJ, Catlin FI, Mahoney DH. Cis-platinum ototoxicity in children. Laryngoscope. 1991 Sep;101(9):917–924. doi: 10.1288/00005537-199109000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Walker DA, Pillow J, Waters KD, Keir E. Enhanced cis-platinum ototoxicity in children with brain tumours who have received simultaneous or prior cranial irradiation. Med Pediatr Oncol. 1989;17(1):48–52. doi: 10.1002/mpo.2950170110. [DOI] [PubMed] [Google Scholar]
- 8.Grau C, Møller K, Overgaard M, Overgaard J, Elbrønd O. Sensori-neural hearing loss in patients treated with irradiation for nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys. 1991 Aug;21(3):723–728. doi: 10.1016/0360-3016(91)90692-w. [DOI] [PubMed] [Google Scholar]
- 9.Schell MJ, McHaney VA, Green AA, et al. Hearing loss in children and young adults receiving cisplatin with or without prior cranial irradiation. J Clin Oncol. 1989 Jun;7(6):754–760. doi: 10.1200/JCO.1989.7.6.754. [DOI] [PubMed] [Google Scholar]
- 10.Kretschmar CS, Warren MP, Lavally BL, Dyer S, Tarbell NJ. Ototoxicity of preradiation cisplatin for children with central nervous system tumors. J Clin Oncol. 1990 Jul;8(7):1191–1198. doi: 10.1200/JCO.1990.8.7.1191. [DOI] [PubMed] [Google Scholar]
- 11.Cohen BH, Zweidler P, Goldwein JW, Molloy J, Packer RJ. Ototoxic effect of cisplatin in children with brain tumors. Pediatr Neurosurg. 1990-1991;16(6):292–296. doi: 10.1159/000120545. [DOI] [PubMed] [Google Scholar]
- 12.Khan AB, D'Souza BJ, Wharam MD, et al. Cisplatin therapy in recurrent childhood brain tumors. Cancer Treat Rep. 1982 Dec;66(12):2013–2020. [PubMed] [Google Scholar]
- 13.Sexauer CL, Khan A, Burger PC, et al. Cisplatin in recurrent pediatric brain tumors. A POG Phase II study. A Pediatric Oncology Group Study. Cancer. 1985 Oct 1;56(7):1497–1501. doi: 10.1002/1097-0142(19851001)56:7<1497::aid-cncr2820560703>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 14.Walker RW, Allen JC. Treatment of recurrent primary intracranial childhood tumors with cis-diamminedichloroplatinum. Ann Neurol. 1983 Sep;14(3):371–372. [Google Scholar]
- 15.Granowetter L, Rosenstock JG, Packer RJ. Enhanced cis-platinum neurotoxicity in pediatric patients with brain tumors. J Neurooncol. 1983;1(4):293–297. doi: 10.1007/BF00165711. [DOI] [PubMed] [Google Scholar]
- 16.Sweetow RW, Will TI. Progression of hearing loss following the completion of chemotherapy and radiation therapy: case report. J Am Acad Audiol. 1993 Nov;4(6):360–363. [PubMed] [Google Scholar]
- 17.Schot LJ, Hilgers FJ, Keus RB, Schouwenburg PF, Dreschler WA. Late effects of radiotherapy on hearing. Eur Arch Otorhinolaryngol. 1992;249(6):305–308. doi: 10.1007/BF00179377. [DOI] [PubMed] [Google Scholar]
- 18.Mahoney DH, Jr, Weaver T, Steuber CP, Starling KA. Ototoxicity with cisplatin therapy. J Pediatr. 1983 Dec;103(6):1006–1007. doi: 10.1016/s0022-3476(83)80747-1. [DOI] [PubMed] [Google Scholar]
- 19.Rubin P. The Franz Buschke lecture: late effects of chemotherapy and radiation therapy: a new hypothesis. Int J Radiat Oncol Biol Phys. 1984 Jan;10(1):5–34. doi: 10.1016/0360-3016(84)90408-5. [DOI] [PubMed] [Google Scholar]
- 20.Heideman RL, Kovnar EH, Kellie SJ, et al. Preirradiation chemotherapy with carboplatin and etoposide in newly diagnosed embryonal pediatric CNS tumors. J Clin Oncol. 1995 Sep;13(9):2247–2254. doi: 10.1200/JCO.1995.13.9.2247. [DOI] [PubMed] [Google Scholar]
- 21.Gaynon PS. Carboplatin in pediatric malignancies. Semin Oncol. 1994 Oct;21((5 Suppl 12)):65–76. [PubMed] [Google Scholar]
- 22.Davis H. Hearing handicap, standards for hearing and medicolegal rules. In: Davis H, Silverman SR, editors. Hearing and Deafness. 3rd ed. New York, NY: Holt, Rinehart, and Wilson;; 1970. [Google Scholar]
- 23.Yassuda CC, Righetti AE, Cury MC, Hyppolito MA, Oliveira JA, Féres O. The role of hyperbaric oxygen therapy (hot) as an otoprotection agent against cisplatin ototoxicity. Acta Cir Bras. 2008;23(Suppl 1):72–76. doi: 10.1590/s0102-86502008000700013. ; discussion 76. [DOI] [PubMed] [Google Scholar]
- 24.Hyppolito MA, de Oliveira AA, Lessa RM, Rossato M. Amifostine otoprotection to cisplatin ototoxicity: a guinea pig study using otoacoustic emission distortion products (DPOEA) and scanning electron microscopy [in Portuguese] Braz J Otorhinolaryngol. 2005 May-Jun;71(3):268–273. doi: 10.1016/S1808-8694(15)31322-7. Epub 2005 Dec 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Marina N, Chang KW, Malogolowkin M, et al. Children's Oncology Group. Amifostine does not protect against the ototoxicity of high-dose cisplatin combined with etoposide and bleomycin in pediatric germ-cell tumors: a Children's Oncology Group study. Cancer. 2005 Aug 15;104(4):841–847. doi: 10.1002/cncr.21218. [DOI] [PubMed] [Google Scholar]