Description
A 60-year old, healthy man presented with a 72 h history of an abdominal pain and nausea. Pain started initially in the epigastrium and migrated subsequently to the right iliac fossa (RIF). The patient denied any change in the bowel habit, rectal bleeding or weight loss. There was no history of previous abdominal pain or surgery. The provisional diagnosis of an acute appendicitis was made, but due to patient’s age a CT was performed in order to exclude colonic malignancy before any surgical intervention. Examination revealed normal observations and soft abdomen with percussion tenderness in the RIF. Digital rectal examination was normal. Laboratory tests were normal, including urea/electrolytes, liver function test, mean cell volume and amylase. The haemoglobin level was 11.9 g/dl. Urinary dip stick was negative. Abdominal radiograph showed a normal gas and bowel pattern. A CT showed 6.5 cm haematoma (figure 1) due to ruptured superior mesenteric artery (SMA) branch pseudoaneurysm (figure 2). The wait-and-see policy was implemented as the pseudoaneurysm was deemed to be not suitable for the embolisation due to difficult anatomy. Follow-up CT scans revealed disappearance of the pseudoaneurysm and resolving haematoma (figures 3 and 4). The patient remains asymptomatic. The incidence of the SMA aneurysms is around 5.5% among all visceral arteries aneurysms and less than 0.5% of all intra-abdominal aneurysms.1 Aetiology of the true SMA aneurysms includes vasculitis (polyarteritis nodosa), fibromuscular dysplasia and collagen vascular disorders (Marfan’s and Ehlers–Danlos syndromes).2 In contrast the SMA pseudoaneurysms are caused by infection, pancreatitis, and dissection.2 Although the vast majority remains asymptomatic, they can like any other aneurysm cause local pressure symptoms, ischaemia or rupture. Diagnosis is usually established by a combination of clinical and radiological findings. Radiological confirmation can be achieved by ultrasound of the abdomen, CT angiography or selective angiography of the SMA.1–3 Patients may present with vague abdominal symptoms or various degree of the haemorrhagic shock due to rupture, which is often fatal. Therefore, the vast majority of cases require an emergency treatment in the form of surgical ligation with or without excision, revascularisation with primary anastomosis or endovascular techniques (stent-graft, embolisation).3 This case showed that conservative approach can be successful. However, such treatment should be always very carefully balanced against the risk of a rupture on individual basis.
Figure 1.
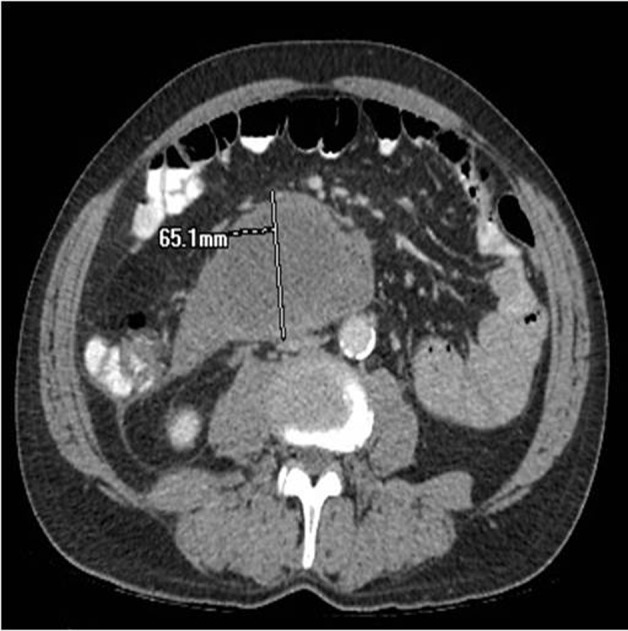
Venous phase CT showing a 6.5 cm collection representing haemorrhage tracking within the mesentery.
Figure 2.

CTA confirming the presence of a 6 mm SMA branch pseudoaneurysm.
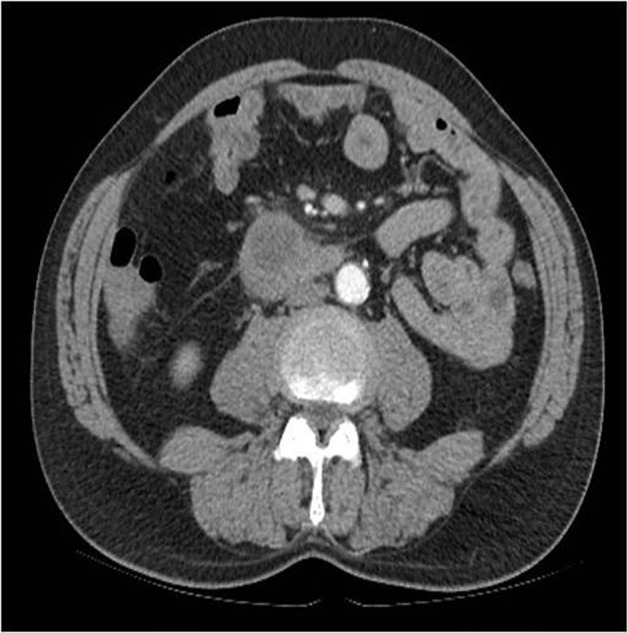
Figure 3.

No evidence of the pseudoaneurysm, which has thrombosed.
Figure 4.
Haematoma significantly reduced in size.
Learning points.
Visceral aneurysms are rare but potentially life threatening.
Prompt diagnosis and surgical or endovascular interventions are crucial in reducing the risk of intestinal infarction and death.
In older group of patients presenting with RIF pain, visceral aneurysms should be kept in mind as a differential diagnosis.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Stewart M, Roy R. An acute presentation of visceral artery aneurysm. BMJ Case Rep 2011; doi:10.1136/bcr.09.2011.4736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Armstrong PJ, Franklin DP. Superior mesenteric artery branch aneurysm with absence of the celiac trunk. Vascular 2006;14:109–12. [DOI] [PubMed] [Google Scholar]
- 3.Kopatsis A, D’Anna JA, Sithian N, et al. Superior mesenteric artery aneurysm: 45 years later. Am Surg 1998;64:263–6. [PubMed] [Google Scholar]


