Abstract
Hidrocystoma and basal cell carcinoma (BCC) are common eyelid lesions. The former is benign while the latter is malignant and can cause significant destruction of the adnexal structures, orbital invasion and visual loss. The authors describe a case of a 76-year-old female with a slow growing right upper lid lesion which was diagnosed as a hidrocystoma but excision biopsy revealed a collision tumour comprised of a BCC abutting a hidrocystoma in the same lesion. Cystic BCC can masquerade as hidrocystoma but there are no previous case reports of BCC coexisting with hidrocystoma in the same lesion. This case highlights the fact that apparently benign lesions, such as hidrocystomas, may actually be malignant or coexist with malignant pathology. Clinicians should have a low threshold for appropriate excision biopsy and histological examination of such lesions, especially if there are sinister features, such as lash loss, induration, pigmentation or a pearly appearance.
Background
Eyelid hidrocystomas are relatively common lesions which are frequently encountered in ophthalmic practice.1 These slow-growing, painless tumours are generally regarded as an insignificant cosmetic blemish and may not be referred for treatment. We present the case of a 76-year-old patient with a transilluminable cystic lesion on the right upper lid. The lesion was initially diagnosed as a hidrocystoma on clinical grounds but histopathology revealed a collision tumour comprised of a basal cell carcinoma (BCC) abutting a hidrocystoma in the same lesion. This case highlights the fact that hidrocystoma may be difficult to differentiate from malignant pathology, especially cystic BCC, on clinical appearance alone. Such diagnostic confusion is not infrequently encountered in our clinical practice and has been previously reported in the medical literature.2 Another interesting aspect of this case is the coexistence of a hidrocystoma and BCC in the same eyelid. Collision tumours of the eyelid are very rare and, to the best of our knowledge, this is the first report of a hidrocystoma colliding with an eyelid BCC in the medical literature.
Case presentation
A 76-year-old female Caucasian patient presented to our unit with a 2 year history of a slow growing, painless lesion on her right upper eyelid margin which she noticed when blinking. The lesion was otherwise asymptomatic. Her previous ocular history and medical history were unremarkable and she was not on any medications.
On examination, there was a soft, dome-shaped, skin-coloured, translucent, cystic swelling which measured 3 mm in diameter, on the lateral aspect of the right upper lid margin (figure 1). The clinical appearance was thought to be consistent with that of a hidrocystoma by the examining ophthalmologist, and excision biopsy of the lesion was arranged.
Figure 1.

Clinical appearance of the cystic, transilluminable lesion on the right upper eyelid with lash loss and a pearly base which is more obvious on the lateral view.
On the day of surgery the lesion was assessed by a more senior surgeon who noted some nodularity, loss and displacement of lashes and a slightly pearly appearance at the base of the transilluminable cyst, raising suspicion of a BCC. The patient subsequently underwent excision biopsy of the lesion with conservative margins, but was warned that further surgery may be required to achieve margin control.
Investigations
Histological examination revealed a thin-walled cyst lined with a double layer of bland cells. The apical cells showed apocrine change focally, consistent with a hidrocystoma. Abutting the cyst was a nodular dermal lesion with connections to the overlying epidermis and peripheral pallisading arranged as slender cords. The cells were atypical and apoptotic bodies were present. There was no evidence of vascular or perineural invasion, and the tumour extended to one of the peripheral margins (figure 2). The histological diagnosis was of a collision tumour comprised of an incompletely excised nodular BCC and a hidrocystoma.
Figure 2.
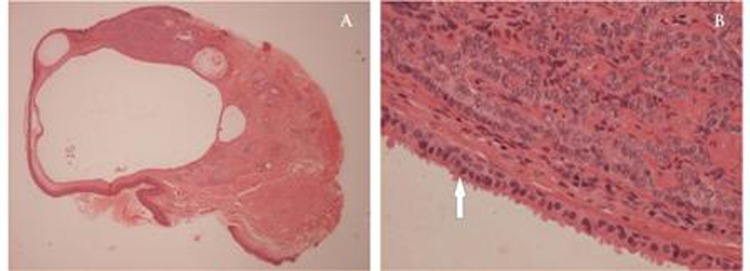
Low power light microscopy reveals an intradermal loculated cyst with an adjacent solid tumour towards the top of the section, extending to the excision margin (H&E x25). The cyst lining consists of a double layer of cells with ‘decapitation’ of the cytoplasm on the luminal border (arrow), characteristic of an apocrine hidrocystoma on high power. Adjacent cords of basaloid cells with peripheral pallisading, characteristic of a basal cell carcinoma, are seen in the upper part of the section (H&E x400).
Outcome and follow-up
After the initial excision biopsy, the patient subsequently underwent Mohs micrographic surgery for margin control and right upper lid reconstruction, achieving a good cosmetic result. There has been no recurrence at the latest review, 11 months postoperatively.
Discussion
The coexistence of two different tumours in the same lesion, known as a collision tumour, is an unusual entity which has been well documented for a variety of benign and malignant lesions. However, there have been few reports of collision tumours involving the eyelid.3–7 A large retrospective review of approximately 40 000 cutaneous biopsies found only 69 collision tumours, of which only four involved the eyelid.8 To the best of our knowledge there are no previous reports of hidrocystoma colliding with BCC in the literature.
Eyelid hidrocystomas are relatively common lesions which are among the top five benign eyelid lesions encountered in ophthalmic practice, accounting for 8% of benign eyelid lesions.1 These sweat gland tumours are either of eccrine or apocrine sweat gland origin and are usually easy to diagnose; presenting as solitary or multiple small, tense, dome-shaped, thin walled-cysts which are slow growing, but can reach a maximum diameter of 15 mm. They are usually translucent, skin-coloured lesions but are occasionally lightly or deeply pigmented.9 Because they are slow-growing and are usually asymptomatic, they are generally regarded as an insignificant cosmetic blemish and are unlikely to be referred for treatment, especially under new commissioning rules. However, not infrequently, malignant pathology may be misdiagnosed as a hidrocystoma; this is especially true of cystic BCC. Similarly, a cutaneous malignant melanoma may be mistakenly diagnosed as a pigmented hidrocystoma. Induration, loss of lashes, a pearly appearance or pigmentation should raise suspicion of malignancy and warrant histological examination. Dermoscopy may also help to differentiate between benign and malignant pathology but the clinical differentiation between the two can be difficult even after histopathological examination.2 A study of 5504 eyelid skin tumours revealed a poor correlation between clinical and histological diagnosis for several tumour subtypes.1 This concurs with our clinical experience and suggests that both general clinicians and ophthalmologists should exercise caution in using clinical diagnosis alone in making the diagnosis of eyelid lesions.
Various treatment options have been tried for hidrocystoma including simple needle puncture, surgical excision, electrodessication of the cyst wall, carbon dioxide vaporisation, pulsed-dye laser treatment and intralesional injection of trichloroacetic acid (TCA).9 10 Because lesions that appear to be hidrocystomas could be malignant or coexist with malignant pathology, we recommend very careful examination of these lesions to exclude signs of malignancy and a low threshold for complete surgical excision and histological examination where suspicion exists. Interestingly, the BCC component of this tumour could have been missed by a more superficial biopsy, such as, decapitation, or other treatment modalities such as needle puncture or intralesional TCA.
This case highlights the fact that hidrocystoma may be difficult to differentiate from malignant pathology on clinical appearance alone, and is a reminder that benign and malignant pathology can coexist within the same lesion, albeit rarely.
Learning points.
Hidrocystoma may be difficult to differentiate from malignant pathology, especially cystic BCC, on clinical examination only.
Benign and malignant pathology may co-exist within the same lesion.
Clinical features suggestive of eyelid malignancy include surface telangiectasia, a pearly edge, loss of lashes, pigmentation of recent onset or worsening, and irregularity of the eyelid margin.
The clinical implications and prognosis are vastly different for a benign hidrocystoma or malignant lesion, such as a BCC.
Acknowledgments
The authors would like to thank Dr Meryl Griffiths, Consultant Histopathologist, for her assistance in the histological evaluation of the specimens.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Deprez M, Uffer S. Clinicopathological features of eyelid skin tumors. A retrospective study of 5504 cases and review of literature. Am J Dermatopathol 2009;31:256–62. [DOI] [PubMed] [Google Scholar]
- 2.Buckel TB, Helm KF, Ioffreda MD. Cystic basal cell carcinoma or hidrocytoma? The use of an excisional biopsy in a histopathologically challenging case. Am J Dermatopathol 2004;26:67–9. [DOI] [PubMed] [Google Scholar]
- 3.Levy J, Cagnano E, Benharroch D, et al. Collision sebaceous and basal cell carcinomas of the eyelid. Ann Diagn Pathol 2006;10:157–9. [DOI] [PubMed] [Google Scholar]
- 4.Shams PN, Olver JM. A case of cutaneous collision tumour: the importance of photographic documentation and large incisional biopsy. Eye (Lond) 2006;20:1324–5. [DOI] [PubMed] [Google Scholar]
- 5.Proia AD, Selim MA, Reutter JC, et al. Basal cell-signet-ring squamous cell carcinoma of the eyelid. Arch Pathol Lab Med 2006;130:393–6. [DOI] [PubMed] [Google Scholar]
- 6.Tunc M, Simmons ML, Char DH, et al. Non-Hodgkin lymphoma and Kaposi sarcoma in an eyelid of a patient with acquired immunodeficiency syndrome. Multiple viruses in pathogenesis. Arch Ophthalmol 1997;115:1464–6. [DOI] [PubMed] [Google Scholar]
- 7.Jakobiec FA, Zakka FR, Hatton MP. Eyelid basal cell carcinoma developing in an epidermoid cyst: a previously unreported event. Ophthal Plast Reconstr Surg 2010;26:491–4. [DOI] [PubMed] [Google Scholar]
- 8.Boyd AS, Rapini RP. Cutaneous collision tumors. An analysis of 69 cases and review of the literature. Am J Dermatopathol 1994;16:253–7. [PubMed] [Google Scholar]
- 9.Sarabi K, Khachemoune A. Hidrocystomas–a brief review. MedGenMed 2006;8:57. [PMC free article] [PubMed] [Google Scholar]
- 10.Dailey RA, Saulny SM, Tower RN. Treatment of multiple apocrine hidrocystomas with trichloroacetic acid. Ophthal Plast Reconstr Surg 2005;21:148–50. [DOI] [PubMed] [Google Scholar]


