Abstract
Type 2 diabetes mellitus is characterized by insulin resistance and progressive β cell failure; therefore, β cell secretagogues are useful for achieving sufficient glycemic control. Glimepiride is a second-generation sulfonylurea that stimulates pancreatic β cells to release insulin. Additionally, is has been shown to work via several extra pancreatic mechanisms. It is administered as monotherapy in patients with type 2 diabetes mellitus in whom glycemic control is not achieved by dietary and lifestyle modifications. It can also be combined with other antihyperglycemic agents, including metformin and insulin, in patients who are not adequately controlled by sulfonylureas alone. The effective dosage range is 1 to 8 mg/day; however, there is no significant difference between 4 and 8 mg/day, but it should be used with caution in the elderly and in patients with renal or hepatic disease. In clinical studies, glimepiride was generally associated with lower risk of hypoglycemia and less weight gain compared to other sulfonylureas. Glimepiride use may be safer in patients with cardiovascular disease because of its lack of detrimental effects on ischemic preconditioning. It is effective in reducing fasting plasma glucose, post-prandial glucose, and glycosylated hemoglobin levels and is a useful, cost-effective treatment option for managing type 2 diabetes mellitus.
Keywords: antihyperglycemic agents, diabetes, glimepiride, sulfonylurea
Introduction
Diabetes is a major public health problem affecting 285 million people worldwide.1 The prevalence of diabetes is projected to double globally by 2030.2 Complications of diabetes include renal failure, neuropathy and peripheral vascular disease with potential for loss of limbs, retinopathy with increased risk of blindness, and an increased risk of cardiovascular disease and stroke, which are related to poorly controlled diabetes.3 Good glycemic control can prevent or delay chronic disease-related microvascular complications as shown by the United Kingdom Prospective Diabetes Study (UKPDS) and the landmark Diabetes Control and Complications Trial.4,5
The pathophysiology of type 2 diabetes mellitus (T2DM) is characterized by relative decrease in insulin secretion and/or insulin resistance. Insulin resistance is a complex phenomenon exacerbated by obesity, particularly central obesity, and is believed to start at a young age because hyperinsulinemia is observed in preteens when both parents have diabetes.6
T2DM results in progressive loss of insulin secretion and the UKPDS showed that ≥50% loss of β cells had occurred by the time of diagnosis; therefore, β cell secretagogues are useful for achieving sufficient glycemic control.7,8
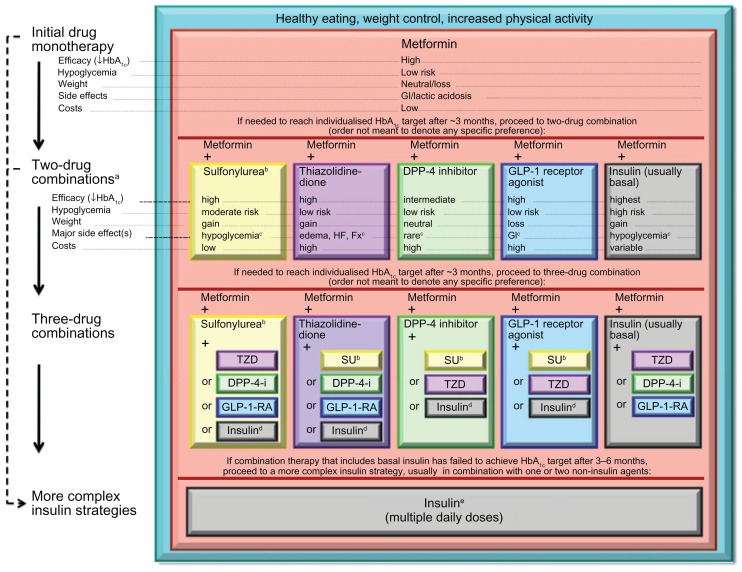
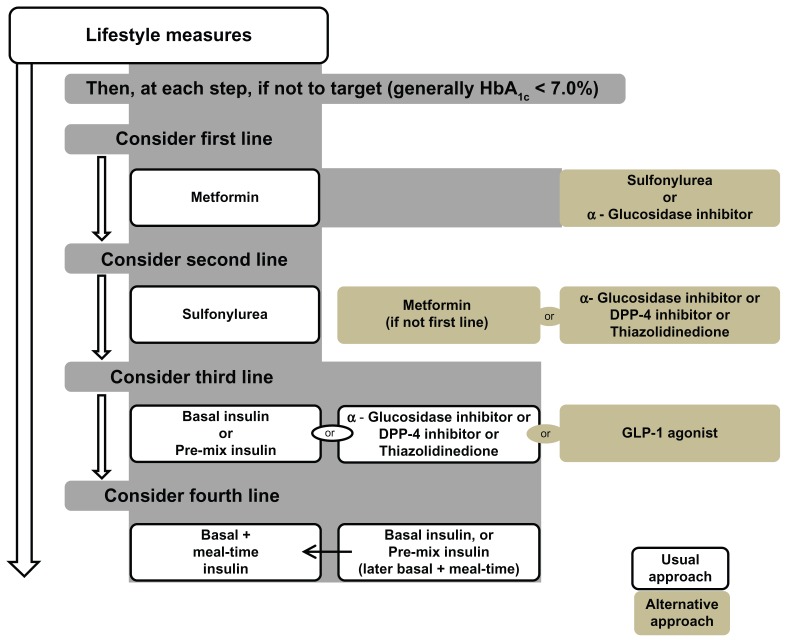
The American Diabetes Association/European Association for the study of Diabetes presented a consensus algorithm for managing T2DM (Figure 1) based on expected glycosylated hemoglobin (HbA1c) levels.9 International Diabetes Federation guidelines for the management of T2DM also recommend lifestyle modifications in the initial stages, and addition of metformin or sulfonylurea is then recommended if additional therapy is required (Figure 2).10
Figure 1.
Management of hyperglycemia in type 2 diabetes: a patient-centered approach. Position statement of the American Diabetes Association and the European Association for the Study of Diabetes. © 2012, Springer Science and Business Media. Reproduced with kind permission from Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycaemia in type 2 diabetes: a patient-centered approach. Position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia. 2012;55(6):1577–1596.9
Abbreviations: DPP-4, dipeptidyl peptidase IV; GIP, glucose-dependent insulinotropic peptide; GLP-1, glucagon-like peptide 1; NPH, neutral protamine Hagedorn; TZD, thiazolidinedione.
Figure 2.
International Diabetes Federation treatment algorithm for people with type 2 diabetes.
© 2005, International Diabetes Federation. Reproduced with kind permission from International Diabetes Federation Clinical Guidelines Task Force. Global guidelines for type 2 diabetes. 2005. Available from: http://www.idf.org/Global_guideline. Accessed on March 29, 2012.10
The goals of pharmacologic therapy in diabetes are to achieve good glycemic control while avoiding hypoglycemia and weight gain so as to decrease the risk of future micro- and macrovascular complications.
Clinicians have a choice of a number of available glucose-lowering agents for managing T2DM which have been shown to be effective and well-tolerated in clinical practice (Table 1).
Table 1.
Comparison of oral hypoglycemic agents used in the management of type 2 diabetes mellitus
| Class of hypoglycemic agents | Duration of action | Reduction in HbA1c (%) | Reduction in FPG (mg/dL) | Dosage |
|---|---|---|---|---|
| Sulfonylureas | 12–24 hours | 0.8–2.0 | 60–70 | |
| Glyburide | Up to 24 hours | 1.25–20 mg as single dose or in two divided doses | ||
| Glipizide | 6–12 hours | 2.5–20 mg twice a day | ||
| Gliclazide | 12 hours | 40–80 mg single dose 160–320 | ||
| Glimepiride | Up to 24 hours | 1–4 mg once 8 mg max | ||
| Meglitinides analogues | 3 hours | 0.5–2.0 | 65–75 | 0.5–4 mg TDS |
| Biguanides | 7–12 hours | 1.5–2.0 | 50–70 | 1–2.5 g/day |
| Thiazolidinediones | Up to 24 hours | 0.5–1.5 | 25–50 | 15–45 mg/day |
| α-Glucosidase inhibitor | 4 hours | 0.7–1.0 | 35–40 | 25–100 mg TDS |
| DDP-4 inhibitors | 24 hours | 0.5–1.4 | – | |
| Sitagliptin | 100 mg once daily | |||
| Sexagliptin | 2.5 mg/5 g once daily | |||
| Vildagliptin | 50 mg once or twice daily | |||
| Linagliptin | 05 mg once daily |
Abbreviations: FPG, fasting plasma glucose; HbA1c, glycosylated hemoglobin; TDS, three times daily.
Methodology
The primary objective of this review is to assess the efficacy and safety of glimepiride, primarily from a clinical viewpoint, while considering clinically relevant end points.
A MEDLINE database search (January 1994 to December 2011) was performed to identify relevant published articles, including reviews and abstracts evaluating glimepiride for treating patients with T2DM (Table 2). Data from animal studies were also included if human data were not available. Reference lists of identified articles were also consulted. An occasional systematic review article and/or meta-analysis summarizing numerous clinical trials were selected for summarizing key data. Pharmacology information was taken from representative original articles.
Table 2.
Pharmacokinetic properties of glimepiride
| Absorption | Completely absorbed after oral administration within 1 hour of administration; significant absorption occurs: plasma protein binding is 99.4% and volume of distribution is 8.8 L. Accumulation does not occur after multiple doses. |
| Metabolism | The drug is primarily metabolized in the liver by CYP2C9 to the active M1 (hydroxyl) metabolite and then to inactive M2 (carboxy) metabolite. |
| Excretion | The main route of excretion is through kidneys. A total of 60% of the metabolites are excreted in urine (predominantly M1) and remainder in feces (predominantly M2). |
Initially, all articles mentioning the drug glimepiride were considered for review. Forty-five clinical trials were used to describe the clinical efficacy and safety of glimepiride. Clinical studies were selected for analysis based on methodological quality, appropriate study design, and publication of results.
Introduction of compounds
Sulfonylureas (SUs) are widely used in the management of T2DM as insulin secretagogues and are named for their common core configuration. They are classified as first- and secondgeneration SUs. First-generation SUs include long-acting chlorpropamide, tolbutamide, tolazamide, and acetohexamide. Substitutions at either end of the compound result in pharmacologic and pharmacokinetic differences among SUs.11
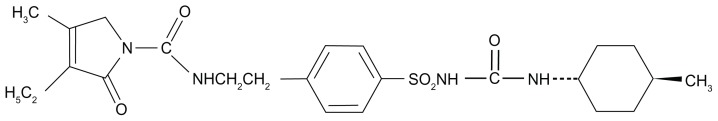
Second-generation SUs include glyburide ( glibenclamide), glipizide, gliquidone, and glimepiride, which vary in duration of action. Glimepiride and glyburide are longer-acting agents than glipizide. Glimepiride is the newest second-generation SU and is sometimes classified as a third-generation SU because it has larger substitutions than other second-generation SUs (Figure 3). It was first introduced into clinical practice in Sweden. The United States Food and Drug Administration (FDA) approved glimepiride in 1995 for the treatment of T2DM as monotherapy as well as in combination with metformin or insulin.
Figure 3.
Chemical structure of glimepiride.
Although other SUs are used with insulin, glimepiride is the only SU approved by FDA for use in combination with insulin. It is used in more than 60 countries worldwide. Treatment with glimepiride as monotherapy results in a 1.5%–2.0% reduction in HbA1c.11,12 Pharmacokinetic properties of glimepiride are shown in Table 2.
Pharmacodynamics
Pancreatic effects
Glimepiride acts at ATPase-dependent potassium channels in β cells of the pancreas to stimulate insulin release.14 using euglycemic and hyperglycemic clamp studies it has been shown to improve both first- and second-phase insulin secretion.15
Glimepiride binds to 65-kD proteins on β cells. In healthy volunteers, a linear relationship was shown between serum glimepiride concentrations and insulin release during euglycemia and a nearly linear relationship under hyperglycemic conditions.16,17
Maximal glucose-lowering activity and insulin level in T2DM patients is achieved within 2–3 hours of taking glimepiride and can last for 24 hours.16 In a 14-week clinical study, peak concentrations 2 hours after administration of 1, 4, and 8 mg doses of glimepiride were associated with decreases in median fasting plasma glucose (FPG) of 43, 70.5, and 74 mg/dL, respectively.12
Glimepiride reduces blood glucose levels and increases insulin levels in blood. A 3-day study of 14 T2DM patients found greater reductions in blood glucose (4.1 vs 1.9 mmol/L) and increase in C-peptide (1.8 vs 1.4 mg/L) and plasma insulin (41 vs 25 mu/L) with 2 mg/day glimepiride compared to placebo (P < 0.05).18
Hypoglycemia after exercise while taking glimepiride was observed in 167 patients with T2DM.19 This was associated with a greater reduction in insulinemia than glibenclamide during exercise, despite similar reductions in blood glucose.
Glimepiride may be taken before or after breakfast with similar results. The efficacy of 2 mg/day glimepiride for 2 weeks on blood glucose levels was not significantly different over a period of 0–4 hours when the drug was given either immediately before breakfast or 30 minutes after breakfast.20
Extrapancreatic effects
The extrapancreatic effects of glimepiride are similar to those of other sulfonylureas. Although peripheral tissue response to insulin is potentiated like other SUs, the clinical relevance of this is not yet clear.21,22 In in vitro studies, glimepiride was found to be two times as potent as glibenclamide in stimulating lipogenesis and glycogenesis.23 Studies in cultured skeletal muscle also suggest a sensitizing effect of glimepiride.24 Possible mechanisms include promotion of GLUT4 transport protein activation and/or translocation in fat and muscle.16,22 Glimepiride reduced insulin resistance and increased hepatic glucose disposal in animal models, but showed no effect in glucose utilization in patients with type 1 diabetes.25
Cardiovascular effects
Glimepiride appears to cause fewer cardiovascular effects than other SUs.16 It was found to be associated with few cardiac changes, fewer ventricular arrhythmias, and little or no effect on blood pressure compared to glyburide and glipizide in animal studies.23 The exact mechanism of this difference in cardiovascular activity is not clear; however, involvement of adenosine triphosphate-sensitive potassium (KATP) channels are thought to play an important role.24,25
Unlike other SUs, glimepiride does not impair ischemic preconditioning of cardiac myocytes. Ischemic preconditioning is an adaptive phenomenon which occurs in response to an ischemic event and delays infarct development during subsequent ischemic episodes, which may help limit tissue damage.26 The postulated mechanism involves selective interaction of glimepiride with sacrolemmal ATP dependent potassium channels in cardiac myocytes rather than mitochondrial channels.27 Evidence suggests that glimepiride preserves myocardial preconditioning, a protective mechanism that limits damage in the event of an ischemic event.14
Data from animal studies suggests that the effects of glimepiride on KATP channels, cardiac vessels, or blood vessels were insignificant compared to that caused by the same dosage of glyburide.28 Similarly, glimepiride has less of an effect in promoting ST segment elevation, enhancing coronary resistance and reducing coronary blood flow compared to glyburide or gliclazide.29
Thus, using glimepiride may be safer than other SUs in cardiac patients due to its lack of detrimental effects on cardiac preconditioning.26
Clinical efficacy
The drug has been assessed in placebo-controlled studies as monotherapy and compared with other SUs and insulin in T2DM patients. Most studies examined FPG, post-prandial glucose (PPG), and HbA1c. Some studies included plasma lipids, serum insulin, or fasting C-peptide levels.
Glimepiride as monotherapy
To assess the efficacy of glimepiride in T2DM, Goldberg et al randomized 304 patients to receive either placebo or one of the three doses (1, 4, or 8 mg) of glimepiride during a 14-week study period.29 All glimepiride regimens significantly reduced FPG, PPG, and HbA1c values (P < 0.001) compared to placebo by the end of the study period. Median changes in FPG levels were 43, 70, and 74 mg/dL at glimepiride doses of 1, 4, and 8 mg, respectively. HbA1c levels were lowered by 1.2%, 1.8%, and 1.9%, and the corresponding decreases in PPG were 63, 92, and 94 mg/dL, respectively. The 4- and 8-mg doses of glimepiride were more effective than the 1-mg dose; however, the 4-mg dose provided a nearly maximal antihyperglycemic effect.
Another study showed equal effects on FPG, PPG, HbA1c, C-peptide, and insulin levels in a cross-over study of 98 patients treated with glimepiride.31 The only significant difference was observed in glucose levels throughout the day, which were lower with a once daily dose compared to a twice daily dosage. The opposite results were observed by Rosenstock et al31 who found a significant decrease in FPG by 0.6 mmol/L with glimepiride when it was given twice daily compared to once daily dosage.
Another multicenter, randomized, placebo-controlled clinical trial by Schade et al studied glimepiride (1–8 mg) titrated over 10 weeks compared with placebo in T2DM subjects who were not controlled by diet alone.32 In this study, glimepiride lowered FPG by 46 mg/dL, PPG by 72 mg/dL, and HbA1c by 1.4% more than the placebo (P < 0.001). Good glycemic control (HbA1c < 7.2%) was achieved in 69% of glimepiride subjects compared to 32% of controls. C-peptide levels and non-fasting insulin levels were also increased in the study subjects.
Glimepiride monotherapy reduced both FPG and PPG levels more than placebo and once daily administration is equivalent to twice daily dosing. Studies also suggest that glimepiride controls blood glucose level throughout the day through its effect on stimulating insulin release, which appears to be greater 2 h after meals than under fasting conditions. These findings suggest that glimepiride enhances insulin and C-peptide secretion under physiologic conditions.
Combination therapy for treating T2DM is now a recommended practice as the disease progresses.10,33 Several studies have examined the combination of glimepiride with other oral hypoglycemic agents with different mechanisms of action for good glycemic control when monotherapy fails.33–35
In a study involving 372 patients with poorly controlled T2DM, glimepiride was added to metformin monotherapy. Study subjects were divided into three groups: metformin group, glimepiride group, metformin plus glimepiride group. In this study, a combination of glimepiride and metformin was shown to be more effective for controlling blood glucose levels compared to the use of either drug alone.33
Combination treatment was significantly more effective in controlling HbA1c (% change +0.07 ± 1.20 for metformin, +0.27 ± 1.10 for glimepiride, −0.74 ± 0.96 for combination treatment, P < 0.001). No significant difference was observed between metformin or glimepiride monotherapy with respect to change in HbA1c or fasting blood glucose; however, glimepiride was significantly more effective than metformin in reducing postprandial blood glucose. Episodes of symptomatic hypoglycemia was also higher in the combination group than in either monotherapy group (P = 0.039).
Comparison with thiazolidinediones
Combination therapy with rosiglitazone plus glimepiride versus rosiglitazone plus placebo was evaluated in a multicenter, double-blind, placebo-controlled study.34 A target HbA1c of <7% was achieved in the glimepiride group and no significant difference was observed in adverse events between the two groups. Metformin plus glimepiride versus metformin plus pioglitazone was studied in another study by Umpierrez.35 In both treatment groups, a similar decrease in mean HbA1c (P = 0.000) and FPG (P < 0.05) compared to baseline was observed; however, a more rapid decline in HbA1c levels (P < 0.05) was achieved with glimepiride (80–90 days) compared to pioglitazone (140–150 days). The study concluded that in poorly controlled T2DM patients on metformin monotherapy, addition of glimepiride was associated with faster glycemic control, lower total cholesterol, and low-density lipoprotein (LDL) as well as reduced short-term health care costs compared to the addition of pioglitazone, which was associated with a higher rate of peripheral edema (4% vs 1% with glimepiride).
Comparison with other sulfonylureas
Glimepiride has been compared to other SUs, including glibenclamide, glipizide, and gliclazide in several clinical trials.
Glimepiride 1–8 mg/day was found to be as effective as glibenclamide 1.26–20 mg/day in lowering FPG, PPG, and HbA1c. Dills et al evaluated the efficacy of glimepiride (≤16 mg) and glyburide (≤20 mg) as monotherapy in 577 patients with T2DM.36 There was no significant glycemic difference between FPG, PPG, or HbA1c in both study groups after the 1-year treatment period. However, the incidence of hypoglycemia was lower with glimepiride (1.7%) than with glibenclamide (5.0%) (P < 0.015).
Another multicenter, prospective, double-blind study comparing glimepiride (1 mg daily, n = 524) and glibenclamide (2.5 mg daily, n = 520) by Draeger et al showed similar results.37 Glimepiride provided equal glycemic control compared to glyburide, with mean FPG and HbA1c of 174 mg/dL and 8.4% for glimepiride and 168 mg/dL and 8.3% for glibenclamide. Additionally, in this study, glimepiride caused fewer hypoglycemic symptoms compared to glibenclamide. Glimepiride was associated with significantly smaller increases in fasting insulin (P = 0.04) and C-peptide (P = 0.03) concentrations than glyburide. In this trial, 11% of glimepiride-treated patients experienced 105 hypoglycemic episodes, and 14% of the glibenclamide treated patients experienced 150 such episodes.16
Schernthaner et al compared once daily gliclazide MR and glimepiride in patients with T2DM.38 In this double-blind, 27-week parallel group study, 845 subjects were randomized to either gliclazide modified release (MR) 30–120 mg daily or glimepiride 1–16 mg daily as monotherapy or in combination with their current treatment (metformin or α glucosidase inhibitor). Efficacy was evaluated based on HbA1c and safety by hypoglycemic episodes using the European Agency definition. HbA1c decreased similarly in both groups from 8.4% to 7.2% in patients on gliclazide MR and from 8.2% to 7.2% in patients receiving glimepiride. The study concluded that glimepiride is as effective as gliclazide MR either as monotherapy or in combination therapy; however, the safety of gliclazide MR was significantly better in terms of hypoglycemic episodes compared with glimepiride.38 Another study using glimepiride or metformin as monotherapy observed changes in serum sialic acid in patients with T2DM over a period of 12 months. The study concluded that there were no statistically significant differences between groups.39
Glimepiride in combination with insulin
Patients who fail to achieve good glycemic control on combination therapy may require insulin.40 Glimepiride is the only SU currently approved by the FDA for combination therapy with insulin. Several studies have demonstrated that a combination of insulin and glimepiride results in a decreased requirement of insulin and good glycemic control.38–42
In a 24-week study of obese patients not adequately controlled by maximum doses of SUs, addition of insulin was compared to insulin + placebo.41 Subjects were randomized to receive insulin and either glimepiride 16 mg/day or placebo, and the insulin dosage was titrated to achieve FPG of 100–120 mg/dL. The two groups showed similar HbA1c and FPG at the end of the study period. However, the group receiving insulin + glimepiride required less insulin (48 vs 78 U/day) and FPG was lowered more rapidly after 2 and 4 weeks of treatment than in the insulin/placebo group.41 Thus, insulin sparing properties are greater with glimepiride than with other SUs.
Another study conducted in 695 poorly controlled patients with T2DM assessed the safety and efficacy of glimepiride with NPH or glargine. Patients were divided into three groups to receive bedtime NPH, bedtime glargine, or morning glargine for 24 weeks in addition to 3 mg of glimepiride. HbA1c improvement was observed more with morning insulin glargine than with NPH insulin (P = 0.001) or bedtime insulin glargine (P = 0.008). The study concluded that the risk for nocturnal hypoglycemia was lower with glimepiride in combination with morning and bedtime insulin glargine than with glimepiride in combination with bedtime NPH insulin.43
Combination of glimepiride with dipeptidyl peptidase-4 inhibitors
Recently, several new classes of hypoglycemic agents have been introduced, including glucagon like peptide-1 and dipeptidyl peptidase-4 (DDP-4) inhibitors. These agents improved glycemic control in T2DM patients either as monotherapy or in combination with SU, metformin, thiazolidinedione, or insulin.44–46 Glimepiride can be used in combination with metformin and DDP-4 inhibitors if glycemic control is not achieved with a single or with two agents (Figure 1). Studies have reported an equal efficacy for glimepiride plus metformin vs vildagliptin/sitagliptin plus metformin in terms of HbA1c reduction.47–49
Although DDP-4 induces less weight gain and hypoglycemia compared to glimepiride, further long-term follow-up studies are needed to determine their safety and efficacy.
Advantages of glimepiride compared to other SUs
Hypoglycemia and weight gain are two important disadvantages of SU therapy; however, the unique properties of glimepiride may provide advantages over other currently available insulin secretagogues.
Glimepiride is generally well-tolerated, and its safety has been reviewed in various randomized clinical studies involving more than 5000 patients. Data from these clinical trials indicate that the overall incidences of adverse events associated with glimepiride are generally lower compared with other SUs.15,16,36,37,50
Hypoglycemia
Severe hypoglycemia is a potentially life-threatening condition and is typically associated with SUs; however, glimepiride differs from older agents in this class, as it is associated with equivalent metabolic control and lower stimulation of insulin secretion.
In a prospective analysis, frequency of severe hypoglycemia with glimepiride was compared with glibenclamide in T2DM patients.51 In this 4-year population-based study, blood glucose levels of all 30,768 patients who attended the emergency department of the region’s central hospital were determined to identify severe hypoglycemia, which was defined as blood glucose level of <2.8 mmol/L or a requirement for intravenous glucose or glucagon injection.
The results showed that although glimepiride was prescribed more frequently than glibenclamide (6976 vs 6789 persons-years), glimepiride induced fewer episodes of hypoglycemia compared to glibenclamide (6 vs 38 episodes). The study concluded that in routine clinical practice, glimepiride is associated with fewer episodes of severe hypoglycemia; the risk can be minimized if individual targets are determined before prescribing this medicine. Glimepiride has been shown to induce a statistically significant decrease in C-peptide and insulin levels compared with glibenclamide, which may explain the reduction of hypoglycemia during and after physical exercise;52 however, the risk of hypoglycemia is increased with concomitant use of other antihyperglycemic agents. Similarly, advanced age, renal, hepatic, and/or cardiovascular comorbidities may increase hypoglycemia risk; this drug should be used with caution in these patients.53
Weight gain
Most patients with T2DM are overweight.54 In these patients, weight reduction results in considerable improvements in their clinical and metabolic profiles, including HbA1c. Weight gain is considered a disadvantage of SUs, thiazolidinediones, and insulin; however, studies suggest that glimepiride has a weight-neutral effect on patients with T2DM.55,56
Several observational cohort studies have shown considerable weight loss with glimepiride. In one study, an average weight loss of 3 kg was reported after 1–5 years of glimepiride,56 while in another study, treatment with glimepiride resulted in weight loss of up to 2.2 kg within 8 weeks.55
The effects of glimepiride or glibencalmide treatment on body weight in patients with T2DM were observed over a 12-month period in a retrospective observational cohort study.57 In this study, mean weight loss and reduction in body mass index from baseline to the end of the study period were greater with glimepiride compared to glibenclamide ([−2.01 ± 4.01 kg/−0.7 ± 1.4 kg/m2] vs [−0.58 ± 3.7 kg/−0.2 ± 1.3 kg/m2]; P < 0.001). The study concluded that initial treatment of T2DM with glimepiride was associated with a significantly greater decrease in body weight and body mass index than treatment with glibenclamide, while providing equivalent glycemic control.57
Weight gain associated with therapies for managing T2DM is an important consideration in clinical practice and a major limitation in achieving good glycemic control. Glimepiride differs from other agents in this class in that it is associated with equivalent metabolic control with weight-neutral effects on patients with T2DM.
The exact mechanism of the weight-neutral effects of glimepiride has not been established; however, lower stimulation of insulin secretion in response to glimepiride compared to other SUs have been implicated.52,58,59 Additionally, glimepiride has many extra-pancreatic glucose-lowering effects,52,59,60 including decreased endogenous glucose production as well as improved peripheral glucose uptake.21 These effects may explain the weight loss or weight neutrality associated with glimepiride use.
Dosage and administration
The starting dose of glimepiride is 1–2 mg typically taken before breakfast. The dose is adjusted according to self-monitoring of blood glucose levels and is gradually increased until glycemic control is achieved. The maximum recommended dosage is 8 mg/day,61 although doses up to 32 mg/day have been used in clinical trials. Typical maintenance dosages are 1–4 mg/day. However, higher dosages (6–8 mg/day) have been found to be associated with reduced mean HbA1c before and after treatment.62 It may also be combined with other treatment modalities for T2DM, including insulin in patients who are not controlled with SUs. However, the combination of insulin and glimepiride requires a lower initial dose of insulin.63
Glimepiride in special situations
Glimepiride appears to be well-tolerated in patients with T2DM, including the elderly. However, it should be used cautiously in elderly, debilitated or malnourished patients. Although it can be used in renal insufficiency, patients should be monitored for signs and symptoms of hypoglycemia and lower doses of glimepiride should be used in these situations.
Conclusion
Glimepiride is a second-generation sulfonylurea which can be used as monotherapy or in combination with other antihyperglycemic agents, including insulin. It is the only SU currently recommended for use with insulin. The safety and efficacy of glimepiride has been confirmed in various controlled studies and it is associated with a lower risk of hypoglycemia and weight gain compared to other SUs.
Glimepiride is effective in reducing FPG, PPG, and HbA1c levels and is a useful, cost-effective treatment option for managing T2DM.
Table 3.
Comparative efficacy of glimepiride in patients with type 2 diabetes
| Reference | Study design | Drug regimen (mg) | Results |
|---|---|---|---|
| Goldberg et al29 | DB, R, PC 14-weeks |
G 0, 1, 4 or 8 qd | Median FPG, PPG and HbA1c at all G does significantly lower than P (P < 0.05) |
| Sonnenberg et al30 | DB, R, CO 8-weeks |
G 3 bid or 6 qd | Glycemic control equivalent between qd and bid regimens |
| Rosenstock et al31 | DB, R, PC 14-weeks |
G 0 qd, 4 bid, 8 qd, 8 bid or 16 qd | Median FPG and HbA1c at all G does significantly lower than P (P < 0.001) |
| Draeger et al37 | DB, R 52-weeks |
G 1–8 qd or glyburide 2.5 to 20 qd or bid | Similar (significant) reductions in FPG and HbA1c in both groups |
| Dills et al36 | DB, R 52-weeks |
G 1–16 qd or glyburide 1.25–20 qd | Similar (significant) reduction in FPG and HbA1c in both groups; significantly lower C peptide and fasting insulin concentrations with G than with glyburide |
| Riddle41 | DB, R, PC 24-weeks |
Insulin ± G 8 bid | Significantly reduced exogenous insulin requirement with G compared with P |
| Schernthaner et al38 | DB, R 27-weeks |
G 1–6 mg or Gliclazide modified release (MR) 30–120 mg | Similar reduction in FPG and HbA1c in both groups Safety of glimepiride was better |
| Charpentier et al33 | DB, R 20-weeks |
G 1–6 mg OD M 850 tid |
No difference in HbA1c or FBG with either agent as monotherapy glimepiride more effective in reducing PPBG |
| Jeon and Oh63 | OL, R 32-weeks |
V50 mg bid plus M500 mg bid or V 50 mg bid plus G 2 mg bid | Comparable efficacy of both groups in reducing HbA1c Less risk of hypoglycemia with V group |
Abbreviations: bid, twice daily; DB, double-blind; FPG, fasting plasma glucose; G, glimepiride; HbA1c, glycosylated hemoglobin; M, metformin; OL, open-label; PC, placebo-controlled; PPG, postprandial glucose; R, randomized; tid, three times daily; qd, once daily; V, vildagliptin.
Acknowledgments
We acknowledge the support of Getz Pharma (Pvt) Ltd, for providing educational support to the research department of Baqai Institute of Diabetology and Endocrinology (BIDE).
Footnotes
Disclosure
The authors have no conflicts of interest to declare.
References
- 1.Schwatz P, editor. Diabetes Prevention in Practice. Dresden, Germany: WCPD; 2010. [Google Scholar]
- 2.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27(5):1047–1053. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Fact sheet number 312: Diabetes. Media centre fact sheet. 2008. [Accessed on March 29, 2012]. Available from: http://www.who.int/mediacentre/factsheets/fs312/en/
- 4.Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998;352(9131):837–853. [PubMed] [Google Scholar]
- 5.The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. The Diabetes Control and Complications Trial Research Group. N Engl J Med. 1993;329(14):977–986. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 6.Fujimoto WY, Bergstrom RW, Leonetti DL, Newell-Morris LL, Shuman WP, Wahl PW. Metabolic and adipose risk factors for NIDDM and coronary disease in third-generation Japanese-American men and women with impaired glucose tolerance. Diabetologia. 1994;37(5):524–532. doi: 10.1007/s001250050142. [DOI] [PubMed] [Google Scholar]
- 7.Robertson RP, Porte D., Jr The glucose receptor a defective mechanism in diabetes mellitus distinct from the beta adrenergic receptor. Clin Invest. 1973;52(4):870–876. doi: 10.1172/JCI107251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reaven GM. Banting lecture 1988. Role of insulin resistance in human disease. Diabetes. 1988;37(12):1595–1607. doi: 10.2337/diab.37.12.1595. [DOI] [PubMed] [Google Scholar]
- 9.Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycaemia in type 2 diabetes: a patient-centered approach. Position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) Diabetologia. 2012;55(6):1577–1596. doi: 10.1007/s00125-012-2534-0. [DOI] [PubMed] [Google Scholar]
- 10.International Diabetes Federation Clinical Guidelines Task Force. Global guidelines for type 2 diabetes. 2005. [Accessed on March 29, 2012]. Available from: http://www.idf.org/Global_guideline.
- 11.Shukla UA, Chi EM, Lehr KH. Glimepiride pharmacokinetics in obese versus non-obese diabetic patients. Ann Pharmacother. 2004;38(1):30–35. doi: 10.1345/aph.1C397. [DOI] [PubMed] [Google Scholar]
- 12.Massi-Benedetti M. Glimepiride in type 2 diabetes mellitus: a review of the worldwide therapeutic experience. Clin Ther. 2003;25(3):799–816. doi: 10.1016/s0149-2918(03)80109-1. [DOI] [PubMed] [Google Scholar]
- 13.Korytkowski M, Thomas A, Reid L, Tedesco MB, Gooding WE, Gerich J. Glimepiride improves both first and second phases of insulin secretion in type 2 diabetes. Diabetes Care. 2002;25(9):1607–1611. doi: 10.2337/diacare.25.9.1607. [DOI] [PubMed] [Google Scholar]
- 14.Campbell RK. Glimepiride: role of a new sulfonylurea in the treatment of type 2 diabetes mellitus. Ann Pharmacother. 1998;32(10):1044–1052. doi: 10.1345/aph.17360. [DOI] [PubMed] [Google Scholar]
- 15.Rosenkranz B. Pharmacokinetic basis for the safety of glimepiride in risk groups of NIDDM patients. Horm Metab Res. 1996;28(9):434–439. doi: 10.1055/s-2007-979833. [DOI] [PubMed] [Google Scholar]
- 16.Goldberg RB, Holvey SM, Schneider J. The Glimepiride Protocol #201 Study Group. A dose response study of glimepiride in patients with NIDDM who have previously received sulfonylurea agents. Diabetes Care. 1996;19:847–856. doi: 10.2337/diacare.19.8.849. [DOI] [PubMed] [Google Scholar]
- 17.Wernicke-Panten K, Haupt E, Pfeiffer C, et al. Early onset of pharmacodynamic effects of glimepiride in type II diabetic patients [abstract] Diabetologia. 1994;37(Suppl 1):A163. [Google Scholar]
- 18.Massi-Benedetti M, Herz M, Pfeiffer C. The effects of acute exercise on metabolic control in type II diabetic patients treated with glimepiride or glibenclamide. Horm Metab Res. 1996;28:451–455. doi: 10.1055/s-2007-979836. [DOI] [PubMed] [Google Scholar]
- 19.Rosskamp R, Herz M. Effect of the time of ingestion of the sulfonylurea glimepiride on the daily blood glucose profile in NIDDM patients [abstract] 15th Int Diab Fed Congr. 1994:416. [Google Scholar]
- 20.Overkamp D, Volk A, Maerker E, et al. Acute effect of glimepiride on insulin-stimulated glucose metabolism in glucose-tolerant insulin-resistant offspring of patients with type 2 diabetes. Diabetes Care. 2002;25(11):2065–2073. doi: 10.2337/diacare.25.11.2065. [DOI] [PubMed] [Google Scholar]
- 21.Müller G. The molecular mechanism of the insulin-mimetic/sensitizing activity of the antidiabetic sulfonylurea drug Amaryl. Mol Med. 2000;6(11):907–933. [PMC free article] [PubMed] [Google Scholar]
- 22.Müller G, Wied S, Wetekam EM, Crecelius A, Unkelbach A, Pünter J. Stimulation of glucose utilization in 3T3 adipocytes and rat diaphragm in vitro by the sulphonylureas, glimepiride and glibenclamide, is correlated with modulations of the cAMP regulatory cascade. Biochem Pharmacol. 1994;30(48):985–996. doi: 10.1016/0006-2952(94)90369-7. [DOI] [PubMed] [Google Scholar]
- 23.Végh A, Papp JG. Haemodynamic and other effects of sulphonylurea drugs on the heart. Diabetes Res Clin Pract. 1996;(Suppl 31):S43–53. doi: 10.1016/0168-8227(96)01229-6. [DOI] [PubMed] [Google Scholar]
- 24.Müller G, Wied S, Straub J, Jung C. Coordinated regulation of esterification and lipolysis by palmitate, H2O2 and the anti-diabetic sulfonylurea drug, glimepiride, in rat adipocytes. Eur J Pharmacol. 2008;597(1–3):6–18. doi: 10.1016/j.ejphar.2008.08.034. [DOI] [PubMed] [Google Scholar]
- 25.Briscoe VJ, Griffith ML, Davis SN. The role of glimepiride in the treatment of type 2 diabetes mellitus. Expert Opin Drug Metab Toxicol. 2010;6(2):225–235. doi: 10.1517/17425250903512955. [DOI] [PubMed] [Google Scholar]
- 26.Mocanu MM, Maddock HL, Baxter GF, Lawrence CL, Standen NB, Yellon DM. Glimepiride, a novel sulfonylurea, does not abolish myocardial protection afforded by either ischemic preconditioning or diazoxide. Circulation. 2001;103(25):3111–3116. doi: 10.1161/01.cir.103.25.3111. [DOI] [PubMed] [Google Scholar]
- 27.Langtry HD, Balfour JA. Glimepiride: a review of its use in the management of type 2 diabetes mellitus. Drugs. 1998;55(4):563–584. doi: 10.2165/00003495-199855040-00007. [DOI] [PubMed] [Google Scholar]
- 28.Geisen K, Vegh A, Krause E, Papp JG. Cardiovascular effects of conventional sulfonylureas and glimepiride. Horm Metab Res. 1996;28:496–507. doi: 10.1055/s-2007-979841. [DOI] [PubMed] [Google Scholar]
- 29.Goldberg RB, Holvey SM, Schneider J. A dose-response study of glimepiride in patients with NIDDM who have previously received sulfonylurea agents. The Glimepiride Protocol #201 Study Group. Diabetes Care. 1996;19(8):849–856. doi: 10.2337/diacare.19.8.849. [DOI] [PubMed] [Google Scholar]
- 30.Sonnenberg GE, Garg DC, Weidler DJ, et al. Short-term comparison of once - versus twice-daily administration of glimepiride in patients with non-insulin-dependent diabetes mellitus. Ann Pharmacother. 1997;31:671–676. doi: 10.1177/106002809703100601. [DOI] [PubMed] [Google Scholar]
- 31.Rosenstock J, Samols E, Muchmore DB, Schneider J. Glimepiride, a new once-daily sulphonylurea. a double-blind placebo-controlled study of NIDDM patients. Glimepiride Study Group. Diabetes Care. 1996;19:1194–1199. doi: 10.2337/diacare.19.11.1194. [DOI] [PubMed] [Google Scholar]
- 32.Schade DS, Jovanovic L, Schneider J. A placebo-controlled, randomized study of glimepiride in patients with type 2 diabetes mellitus for whom diet therapy is unsuccessful. J Clin Pharmacol. 1998;38(7):636–641. doi: 10.1002/j.1552-4604.1998.tb04471.x. [DOI] [PubMed] [Google Scholar]
- 33.Charpentier G, Fleury F, Kabir M, Vaur L, Halimi S. Improved glycaemic control by addition of glimepiride to metformin monotherapy in type 2 diabetic patients. Diabet Med. 2001;18(10):828–834. doi: 10.1046/j.1464-5491.2001.00582.x. [DOI] [PubMed] [Google Scholar]
- 34.McCluskey D, Touger MS, Melis R, Schleusener DS. Results of a randomized, double-blind, placebo-controlled study administering glimepiride to patients with type 2 diabetes mellitus inadequately controlled with rosiglitazone monotherapy. Clin Ther. 2004;26(11):1783–1790. doi: 10.1016/j.clinthera.2004.11018. [DOI] [PubMed] [Google Scholar]
- 35.Umpierrez G, Issa M, Vlajnic A. Glimepiride versus pioglitazone combination therapy in subjects with type 2 diabetes inadequately controlled on metformin monotherapy: results of a randomized clinical trial. Curr Med Res Opin. 2006;22(4):751–759. doi: 10.1185/030079906X104786. [DOI] [PubMed] [Google Scholar]
- 36.Dills DG, Schneider J. Clinical evaluation of glimepiride versus glyburide in NIDDM in a double-blind comparative study. Glimepiride/Glyburide Research Group. Horm Metab Res. 1996;28(9):426–429. doi: 10.1055/s-2007-979831. [DOI] [PubMed] [Google Scholar]
- 37.Draeger KE, Wernicke-Panten K, Lomp HJ, Schuler E, Rosskamp R. Long-term treatment of type 2 diabetic patients with the new oral antidiabetic agent glimepiride (Amaryl): a double-blind comparison with glibenclamide. Horm Metab Res. 1996;28(9):419–425. doi: 10.1055/s-2007-979830. [DOI] [PubMed] [Google Scholar]
- 38.Schernthaner G, Grimaldi A, Di-Mario U, et al. GUIDE study: double-blind comparison of once-daily gliclazide MR and glimepiride in type 2 diabetic patients. Eur J Clin Invest. 2004;34:535–542. doi: 10.1111/j.1365-2362.2004.01381.x. [DOI] [PubMed] [Google Scholar]
- 39.Rahman IU, Malik SA, Bashir M, Khan RU, Idrees M. Monotherapy with metformin or glimepiride and changes in serum sialic acid in type 2 diabetes mellitus. Brit J Diab Vas Dis. 2011;11(3):137–140. [Google Scholar]
- 40.Garber AJ. Benefits of combination therapy of insulin and oral hypoglycemic agents. Arch Intern Med. 2003;163(15):1781–1782. doi: 10.1001/archinte.163.15.1781. [DOI] [PubMed] [Google Scholar]
- 41.Riddle MC. Combined therapy with a sulfonylurea plus evening insulin: safe, reliable, and becoming routine. Horm Metab Res. 1996;28:430–433. doi: 10.1055/s-2007-979832. [DOI] [PubMed] [Google Scholar]
- 42.Riddle MC, Schneider J. Beginning insulin treatment of obese patients with evening 70/30 insulin plus glimepiride versus insulin alone. Glimepiride Combination Group. Diabetes Care. 1998;21(7):1052–1057. doi: 10.2337/diacare.21.7.1052. [DOI] [PubMed] [Google Scholar]
- 43.Fritsche A, Schweitzer MA, Häring HU. Glimepiride combined with morning insulin glargine, bedtime neutral protamine Hagedorn insulin, or bedtime insulin glargine in patients with type 2 diabetes. A randomized, controlled trial. Ann Intern Med. 2003;138(12):952–959. doi: 10.7326/0003-4819-138-12-200306170-00006. [DOI] [PubMed] [Google Scholar]
- 44.Schneider J. An overview of the safety and tolerance of glimepiride. Horm Metab Res. 1996;28:413–418. doi: 10.1055/s-2007-979829. [DOI] [PubMed] [Google Scholar]
- 45.Holstein A, Plaschke A, Egberts EH. Lower incidence of severe hypoglycaemia in patients with type 2 diabetes treated with glimepiride versus glibenclamide. Diabetes Metab Res Rev. 2001;17(6):467–473. doi: 10.1002/dmrr.235. [DOI] [PubMed] [Google Scholar]
- 46.Müller G. The molecular mechanism of the insulin-mimetic/sensitizing activity of the antidiabetic sulfonylurea drug Amaryl. Mol Med. 2000;6(11):907–933. [PMC free article] [PubMed] [Google Scholar]
- 47.Heine RJ. Role of sulfonylureas in non-insulin-dependent diabetes mellitus: part II – ‘the cons’. Horm Metab Res. 1996;28:522–526. doi: 10.1055/s-2007-979845. [DOI] [PubMed] [Google Scholar]
- 48.Tremble JM, Donaldson D. Is continued weight gain inevitable in type 2 diabetes mellitus? J R Soc Promot Health. 1999;119:235–239. doi: 10.1177/146642409911900406. [DOI] [PubMed] [Google Scholar]
- 49.Scholz G, Schneider K, Knirsch W, Becker G. Efficacy and tolerability of glimepiride in daily practice: a non-interventional observational cohort study. Clin Drug Invest. 2001;21(9):597–604. [Google Scholar]
- 50.Weitgasser R, Lechleitner M, Luger A, Klingler A. Effects of glimepiride on HbA1c and body weight in type 2 diabetes: results of a 1.5-year follow-up study. Diabetes Res Clin Pract. 2003;61:13–19. doi: 10.1016/s0168-8227(02)00254-1. [DOI] [PubMed] [Google Scholar]
- 51.Martin S, Kolb H, Beuth J, van Leendert R, Schneider B, Scherbaum WA. Change in patients’ body weight after 12 months of treatment with glimepiride or glibenclamide in type 2 diabetes: a multicentre retrospective cohort study. Diabetologia. 2003;46(12):1611–1617. doi: 10.1007/s00125-003-1238-x. [DOI] [PubMed] [Google Scholar]
- 52.Draeger K, Wernicke-Panten K, Lomp HJ, Schuler E, Rosskamp R. Long-term treatment of type 2 diabetic patients with the new oral antidiabetic agent glimepiride (Amaryl): a double-blind comparison with glibenclamide. Horm Metab Res. 1996;28:419–425. doi: 10.1055/s-2007-979830. [DOI] [PubMed] [Google Scholar]
- 53.Müller G, Hartz D, Pünter J, Okonomopulos R, Kramer W. Differential interaction of glimepiride and glibenclamide with the beta-cell sulfonylurea receptor. I. Binding characteristics. Biochim Biophys Acta. 1994;1191:267–277. doi: 10.1016/0005-2736(94)90177-5. [DOI] [PubMed] [Google Scholar]
- 54.Müller G, Satoh Y, Geisen K. Extrapancreatic effects of sulfonylureas – a comparison between glimepiride and conventional sulfonylureas. Diabetes Res Clin Pract. 1995;(Suppl 28):S115–137. doi: 10.1016/0168-8227(95)01089-v. [DOI] [PubMed] [Google Scholar]
- 55.Hoechst-Roussel Pharmaceuticals, Inc Amaryl (glimepiride) prescribing information. Somerville, NJ: Hoechst-Roussel Pharmaceuticals, Inc; 1995. [Google Scholar]
- 56.Hydrie MZI, Gul A, Hakeem R, Ahmadani MY, Basit A. Glimepiride study on type-2 diabetic subjects. Pak J Med Sci. 2006;22:132–135. [Google Scholar]
- 57.Bugos C, Austin M, Atherton T, Viereck C. Long-term treatment of type 2 diabetes mellitus with glimepiride is weight neutral: a meta-analysis. Diabetes Res Clin Pract. 2000;50(Suppl 1):S47. [Google Scholar]
- 58.Rosenstock J, Fitchet M. Vildagliptin: clinical trials programme in monotherapy and combination therapy for type 2 diabetes. Int J Clin Pract Suppl. 2008;159:15–23. doi: 10.1111/j.1742-1241.2007.01692.x. [DOI] [PubMed] [Google Scholar]
- 59.Garber AJ, Foley JE, Banerji MA, et al. Effects of vildagliptin on glucose control in patients with type 2 diabetes inadequately controlled with a sulphonylurea. Diabetes Obes Metab. 2008;10(11):1047–1056. doi: 10.1111/j.1463-1326.2008.00859.x. [DOI] [PubMed] [Google Scholar]
- 60.Fonseca V, Baron M, Shao Q, Dejager S. Sustained efficacy and reduced hypoglycemia during one year of treatment with vildagliptin added to insulin in patients with type 2 diabetes mellitus. Horm Metab Res. 2008;40:427–430. doi: 10.1055/s-2008-1058090. [DOI] [PubMed] [Google Scholar]
- 61.Matthews DR, Dejager S, Ahren B, et al. Vildagliptin add-on to metformin produces similar efficacy and reduced hypoglycaemic risk compared with glimepiride, with no weight gain: results from a 2-year study. Diabetes Obes Metab. 2010;12:780–789. doi: 10.1111/j.1463-1326.2010.01233.x. [DOI] [PubMed] [Google Scholar]
- 62.Dejager S, Razac S, Foley JE, Schweizer A. Vildagliptin in drug-naive patients with type 2 diabetes: a 24-week, double-blind, randomized, placebo-controlled, multiple-dose study. Horm Metab Res. 2007;39:218–223. doi: 10.1055/s-2007-970422. [DOI] [PubMed] [Google Scholar]
- 63.Jeon HJ, Oh TK. Comparison of Vildagliptin-metformin and glimepiridemetformin treatments in type 2 diabetic patients. Diabetes Metab J. 2011;35:529–535. doi: 10.4093/dmj.2011.35.5.529. [DOI] [PMC free article] [PubMed] [Google Scholar]