Abstract
Objective. To develop, implement, and assess the effectiveness of an online medication therapy management (MTM) program to train pharmacists and pharmacy students in providing MTM services for patients with diabetes and to increase their intent to perform these services.
Design. An online program was created using an Internet-based learning platform to simulate 4 MTM meetings between a pharmacist and a virtual patient diagnosed with diabetes.
Assessment. Eighty students and 42 pharmacists completed the program. After completing the program, scores on post-intervention assessments showed significant improvement in 2 areas: control over performing MTM, and knowledge of how to perform MTM. Students had a significantly less-positive attitude about MTM and a decline in their perception of the social expectation that MTM is part of the practice of pharmacy, while pharmacists’ attitudes did not change significantly in these areas.
Conclusion. This online program using a virtual patient improved both participants’ belief that they have control over performing MTM, and their knowledge of how to perform MTM for diabetic patients, which may increase the likelihood that pharmacists and pharmacy students will perform MTM in the future.
Keywords: medication therapy management, diabetes, pharmacist, virtual patient, simulation, pharmacy student
INTRODUCTION
Medication therapy management (MTM) is the process of a pharmacist interviewing a patient and making therapy recommendations, with the goals of promoting safe and appropriate medication use, resolving or preventing drug-related problems, providing patient education, and promoting the use of evidence-based and cost-effective medications.1,2 Patients who have been diagnosed with type 1 or type 2 diabetes mellitus are particularly good candidates for pharmacist-performed MTM. Patients with this condition often take several medications concurrently, and because pharmacists are uniquely positioned to provide care and highly accessible to patients in the community, they can have a positive impact on the healthcare of these patients.3,4 Additionally, some MTM programs, including the Wisconsin Pharmacy Quality Collaborative (WPQC), pay pharmacists to provide MTM to patients with diabetes.2
With the emergence of MTM programs, there is a growing need to educate pharmacy students and practicing pharmacists on how to perform high-quality MTM. There is also a need to address the barriers preventing pharmacists from performing this service, such as knowledge of how to operate a particular MTM billing program, and access to educational materials focused on MTM and the disease states typically encountered.5 Pharmacists’ confidence in their ability to perform these reviews is a factor in whether they include MTM services in their practice. Therefore, advanced training focused on improving pharmacists’ comfort with performing MTM and responding to patients’ needs may result in increased performance of MTM by community pharmacists.6 Effective training programs for pharmacists should provide example patient cases, teach how to use treatment guidelines to recommend medication changes to patients’ providers, and demonstrate how to plan for an efficient MTM meeting with a patient.
MTM education can occur in several formats. Several colleges and schools of pharmacy have implemented elective and required courses in laboratory, lecture, and advanced experiential settings using active-learning techniques, such as role-playing and online learning, that include patient cases and an existing commercial MTM platform.7-9 Working these simulated patient cases allows participants to increase their confidence and ability to perform MTM in a safe but realistic active-learning environment.7-8 Online virtual-patient learning experiences increase the knowledge of health professionals, including pharmacists seeking professional development.10-14
The Theory of Planned Behavior states that a person’s actions may be predicted based on their beliefs about a subject. Assessment of these beliefs will predict whether an educational intervention will alter the participant’s future behavior in terms of intent to apply the new knowledge gained.15 The theory uses 3 realms for this measurement: the participants’ attitudes toward the subject (eg, whether they believe the topic is useful for their work setting), their perception of the subjective norm of the topic (social and professional pressure and expectations about the practice, or expectations regarding standards of care), and their perception of control over the topic (whether they feel they can personally perform the activity). For example, if a practitioner believes that a particular laboratory test is effective, accepted as the general practice in the management of a particular condition, and not prohibitively difficult to perform, that practitioner will probably use that test.
The hypothesis of this study was that pharmacists and pharmacy students who completed an online virtual patient MTM program would increase their intent to perform MTM, as measured by a change in their beliefs about MTM described by the Theory of Planned Behavior. If there is a change in whether pharmacists consider MTM to be an effective patient care tool (attitude), in their belief that they are expected to perform MTM (subjective norm), and their perceived ability to perform MTM (behavioral control), then their future behavior toward this activity would likely change. An improvement in these 3 areas would indicate that a participant was more likely to perform MTM reviews in the future. The secondary goals of the study were to determine whether this teaching method was effective for both practicing pharmacists and pharmacy students, and to detect whether there was a change in MTM and diabetes care skills.
DESIGN
The online program was created during the summer and fall of 2010 within Moodle, (Moodle Trust, Perth, Australia), an Internet-based software program that previously had been used successfully as a virtual learning platform for health professions students.16 The Moodle platform supplements classroom learning by allowing a course instructor to create tools that are accessible outside of the classroom through a secure Internet site, including practice activities and quizzes, patient case examples, discussion boards for communication between students and the instructor, and provision of resources by posting links or documents. Development and delivery of the MTM program required the coordinated efforts of several individuals at the UW School of Pharmacy: a pharmacy resident to create the program content and supervise the program, a certified diabetes educator to review program content, the informational technology department to assist with transfer of the program from a word processing document into the online Moodle platform, a laboratory faculty member willing to include the program as a required activity within her class, and a UW Extension Services in Pharmacy faculty member to provide access and Accreditation Council for Pharmacy Education (ACPE) accreditation for practicing pharmacists. Creation of the program required approximately 100 hours.
This study was submitted to and approved by the University of Wisconsin (UW) Educational Investigational Review Board prior to the initial recruitment of subjects. Approximately 140 third-year pharmacy students were invited to participate in the research portion of the project. All pharmacy students were required to complete the MTM program as part of their pharmacotherapy laboratory course, but only those who provided written consent were included in the study.
Pharmacist members of the Pharmacy Society of Wisconsin and those serving as clinical instructors for the UW School of Pharmacy were sent e-mail invitations to participate. Pharmacists were eligible to earn ACPE continuing education credit for completing the program. In the e-mail invitation to participate, the pharmacists were told that only the first 140 pharmacists to provide written consent for inclusion in the study would be allowed access to the program.
The MTM program included: (1) collection of demographic information, including personal experience with MTM; (2) multiple-choice and short-answer survey questions based on the Theory of Planned Behavior which participants answered before and after the intervention; (3) pre- and post-intervention quiz questions related to skills required for a diabetes-focused MTM, including knowledge of the goals of therapy and resolution of drug-related problems; (4) recorded PowerPoint tutorials describing how to use the educational program, find general diabetes care information, and perform an MTM meeting; (5) an electronic medical record for the female virtual patient, recently diagnosed with diabetes; (6) four interactive virtual MTM meetings between the participant (pharmacist or pharmacy student) and the virtual patient to allow for multiple opportunities to practice MTM skills and to monitor laboratory values and medications, which the investigators programmed to became more complicated over time; (7) an electronic “drop box” to collect participants’ documentation of patient meetings.
Participants accessed the program online through Moodle and were instructed to review the patient’s electronic chart before proceeding to the simulated meeting. The patient’s chart included demographics, relevant laboratory results, and the pharmacy’s refill history record. Over the course of the 4 meetings, the chart reflected changes in the patient’s laboratory results and pharmacy records to reflect the addition of new medications and response to therapy or the results of non-adherence to prescribed therapy.
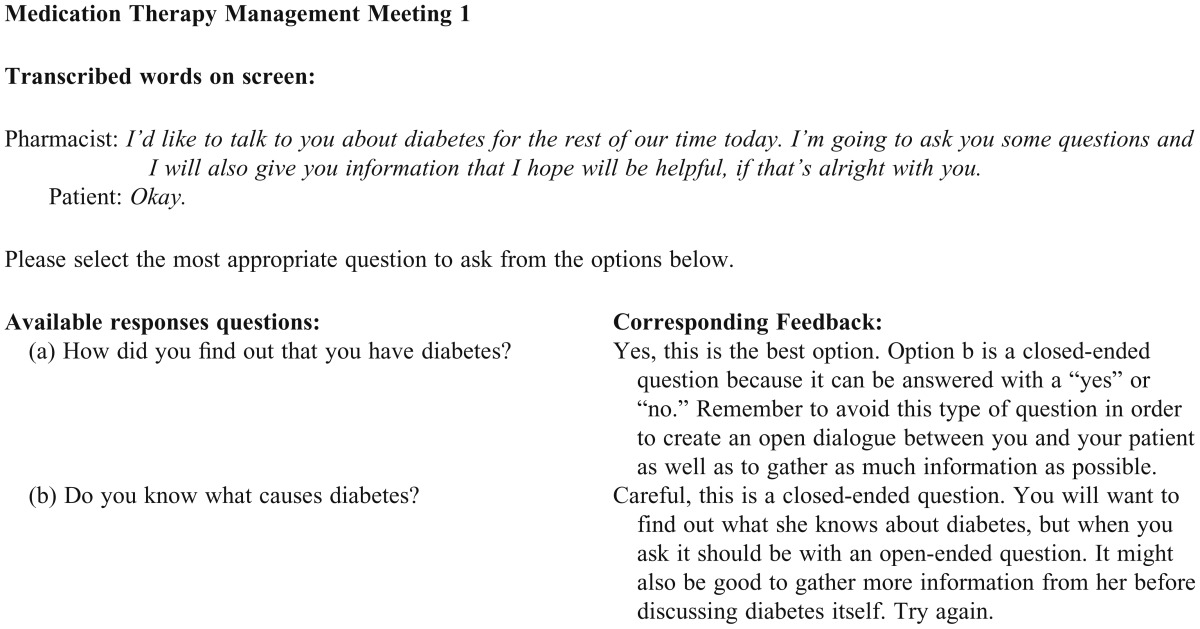
The 4 simulated MTM meetings were available on a text-only Web page as a transcribed conversation where the viewer could see a small portion of the conversation at a time. The first screen of the MTM meeting included the pharmacist’s welcoming remarks to the patient, with the patient’s response listed in a separate paragraph just below. Under this transcription was a list of phrases from which the participant selected what the pharmacist should say to the patient at that point in the conversation. The user was given immediate feedback about his/her selection in the form of a pop-up window describing why the selection was or was not the best of those listed, thus reinforcing the participant’s knowledge of the goals of MTM, good communication skills, and motivational interviewing techniques. From there the participant could either click on the link to continue to the next portion of the conversation, or return to the previous screen to select a more appropriate phrase. In this way, participants were guided in prioritizing problems identified and order of conversation topics, provided training through modeling appropriate behavior, and given immediate feedback for incorrect answers.
For example, during the first MTM meeting, the participant was given 2 options for how to ask the patient about the circumstances surrounding her diagnosis. One option used an open-ended question while the other used a closed-ended question (Appendix 1). If the best response was not chosen on the first try, the participant could select another option. Other questions asked participants to choose the best treatment option based on national guidelines, and how to phrase the importance of patient adherence to medication in lay terms.
During each virtual MTM meeting, participants were asked to complete the 5 core elements for MTM as defined by the American Pharmacists Association and the National Association of Chain Drug Stores (NACDS): medication therapy review, documentation and follow-up, a medication action plan, a personal medication record, and intervention or referral.1 The interventions and observations made during each of the 4 virtual MTM meetings were documented using a SOAP (subjective, objective, assessment, and plan) note format. The notes included any referrals, drug-therapy problems that were identified or resolved, and the participant’s follow-up plan. Each participant was provided with a SOAP note template and asked to complete the assessment and plan sections. There was also a section in the same template document to complete the patient’s medication action plan and personal medication record.
Requiring the participant to complete 4 MTM meetings with the patient ensured that the major categories of medical care for patients with diabetes listed in the 2009 American Diabetes Association Guidelines would be discussed, such as blood glucose management, smoking cessation, and immunizations. In this way, the program prepared participants to discuss relevant treatment topics with patients who have diabetes.
EVALUATION AND ASSESSMENT
The pre- and post-intervention assessment included 4 sections: demographic information, 12 questions assessing participants’ beliefs about MTM, a question regarding intent to use program materials, and 11 knowledge-based quiz questions. The section on beliefs about MTM asked participants to rate a list of 12 statements created to assess the 3 domains of the Theory of Planned Behavior (attitude, subjective norm, and behavioral control) on a 7-point Likert scale ranging from 1 = strongly agree to 7 = strongly disagree. Each statement assessed 1 of the 3 domains and all 12 statements were worded identically on the pre- and post-intervention survey instruments.
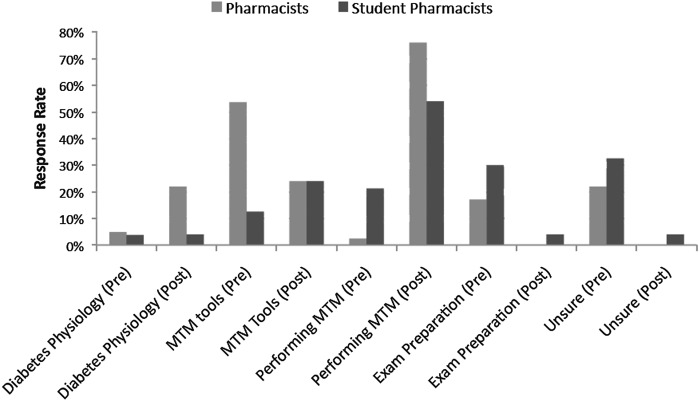
On the pre-intervention survey instrument, participants were also asked to select how they expected the program to be useful to them (Figure 1). On the post-intervention survey instrument, they were asked to share, in their own words, how they intended to use the skills and information gained through the program. Responses were individually assessed and grouped into topics, then compared with the original categories listed in the pre-intervention survey instrument.
Figure 1.
Learning goals and intended application.
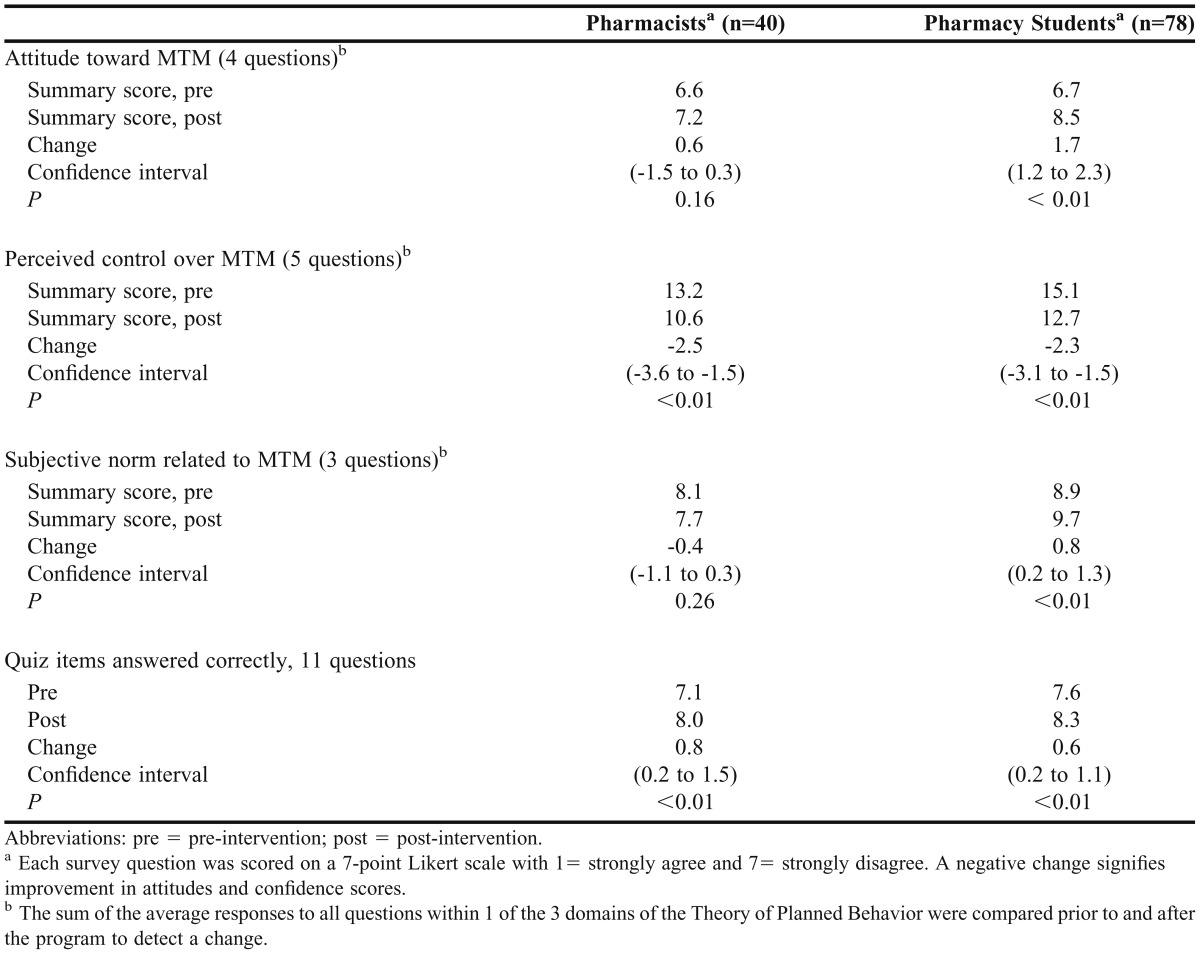
The average response to each individual pre-intervention survey question related to participants’ beliefs about MTM was compared to the average response to its identical post-intervention counterpart to detect a change. To determine whether change had occurred in each of the 3 domains of the Theory of Planned Behavior, average pre-intervention responses to all questions for a given domain were added to find the summary pre-intervention response score for that domain; that score was then compared to the summary post-intervention response score for that domain. For example, participants’ average responses to the 4 items from the pre-intervention survey instrument assessing participants’ attitudes toward MTM were added to form the pre-intervention attitude score, which was then compared to the average post-assessment MTM attitude score. Summations and comparisons of the behavioral control and subjective norm survey questions were calculated and compared in the same way.
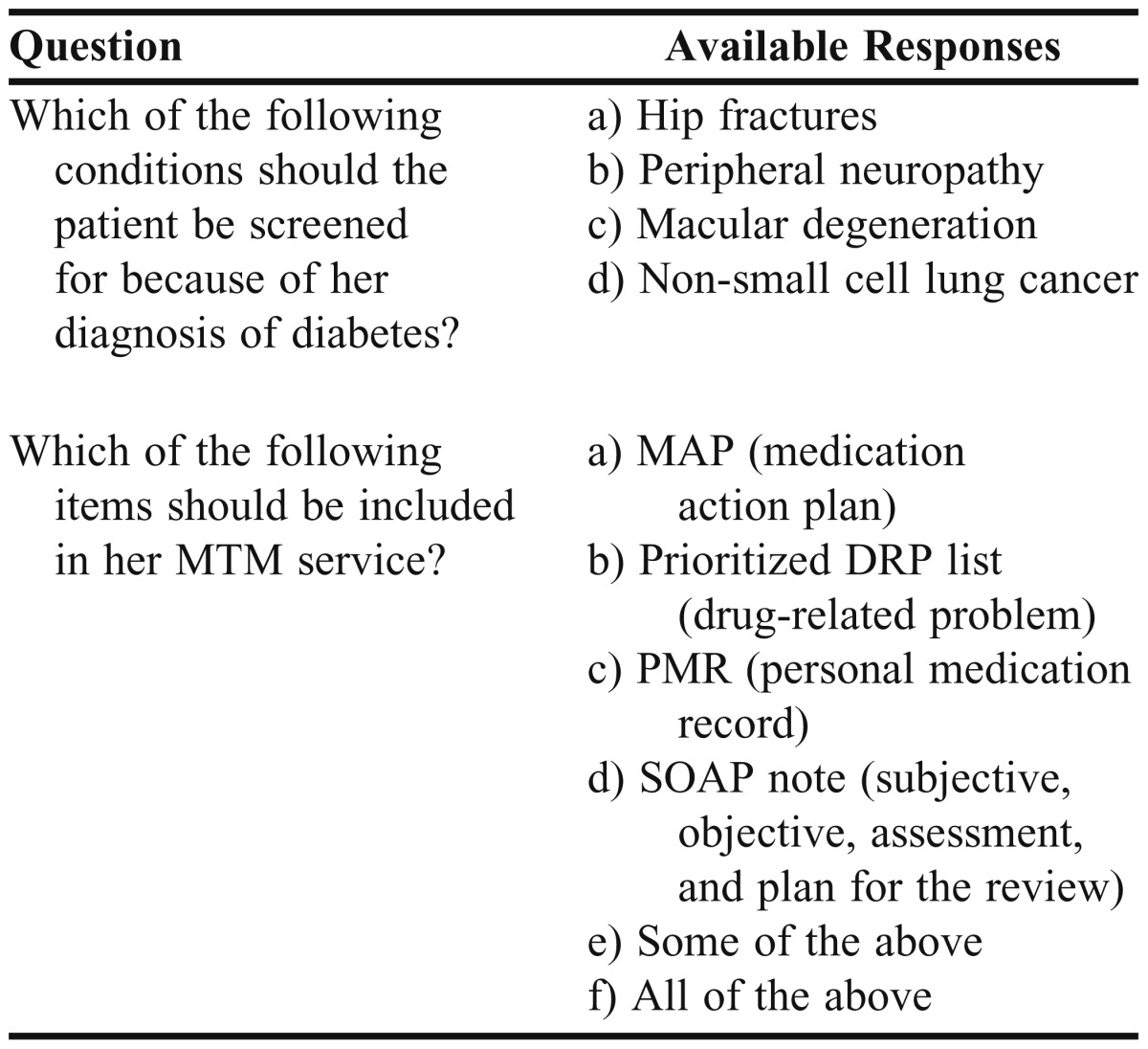
The 11 multiple-choice questions that tested participants’ knowledge of diabetes care were similar, though not identical, in the pre- and post-intervention quiz section (Table 1). Quiz scores were calculated based on the number of multiple-choice questions answered correctly in the pre- and post-intervention quiz. T tests were used for paired samples to compare changes in mean survey and quiz scores before and after participants completed the online program. Analyses were performed using Stata, version 11 (StataCorp LP, College Station, TX). Two-sided p values less than 0.05 were considered significant.
Table 1.
Examples of Questions From a Pre-intervention Quiz Administered to Pharmacy Students and Pharmacists Who Participated in an Online Training Program Medication Therapy Management for Diabetes
Only data from participants who completed the online program, the pre- and post-intervention survey instruments, and the pre- and post-intervention quizzes were analyzed. If participants did not complete all segments, their data were excluded entirely. If participants did not answer all individual questions in each analyzed section, their pre- and post-intervention responses for that particular section were eliminated from the analysis.
Eighty of approximately 140 third-year pharmacy students who completed the program as a required part of a laboratory course provided written consent for their data to be included in this study. Of the more than 2,000 pharmacists who were invited by e-mail to participate, 42 completed the program prior to the deadline for study completion, for a total of 122 participants.
Demographic data differed significantly between the 2 groups: on average, students were younger, had less experience performing MTM, had completed fewer formal MTM training programs, had higher baseline knowledge of the core elements of an MTM review, and had different educational goals than practicing pharmacists (Table 2). For example, whereas 54% (22 of 41) of pharmacists stated they wanted online tools to guide an MTM interview, only 13% (10 of 80) of pharmacy students listed learning how to use online tools as an educational goal (Figure 1).
Table 2.
Demographics of Participants in a Study of the Effectiveness of an Online Course Using a Virtual Patient to Teach Medication Therapy Management for Patients With Diabetes
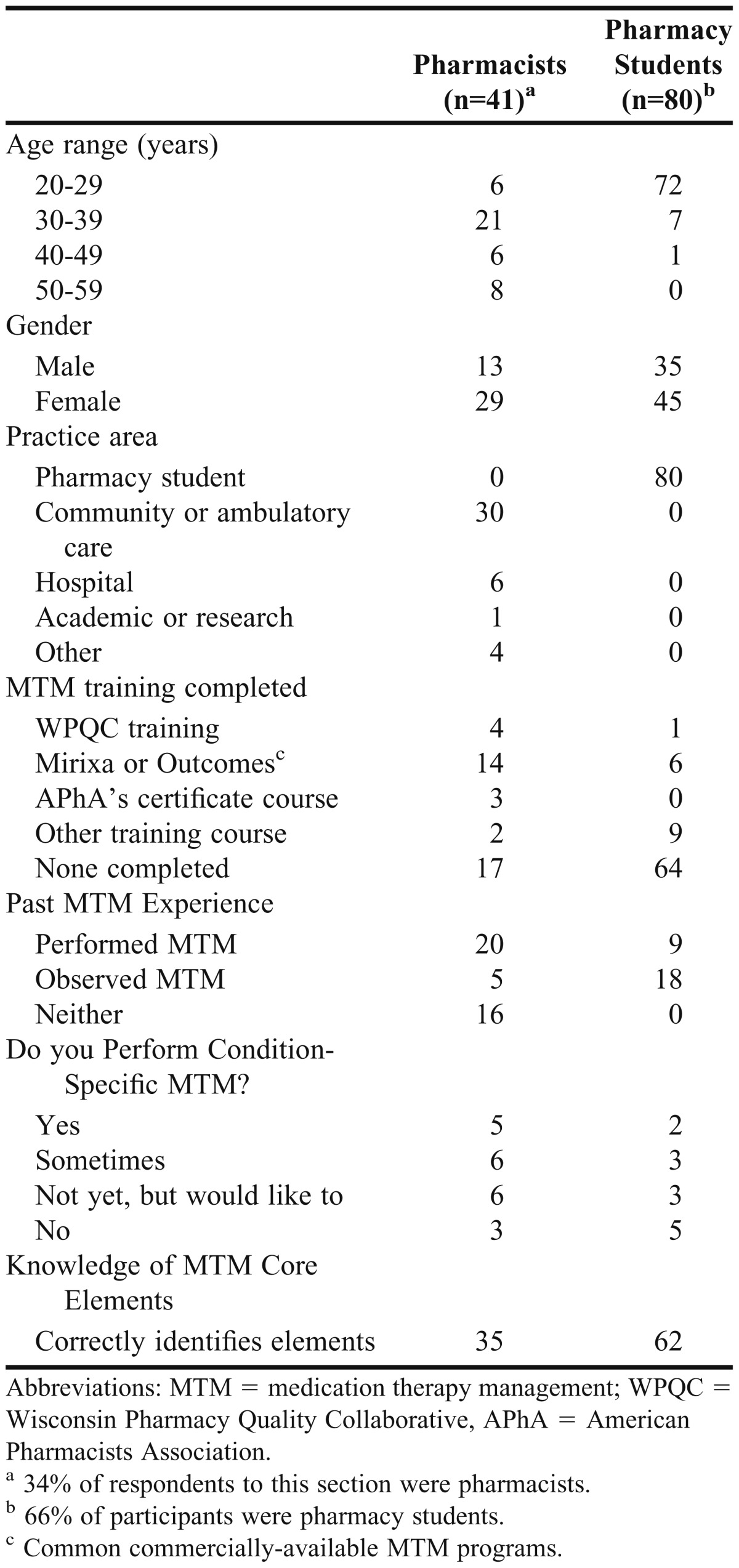
Table 3 lists the change in quiz and survey scores for pharmacists and students during the program. Both pharmacists’ and students’ agreement with survey items related to their perception of behavioral control related to MTM increased from pre-assessment to post-assessment, with an average increase of -2.5 (p < 0.01) for pharmacists and -2.3 (p < 0.01) for students. (A negative numerical change indicated increased agreement with the topic as lower scores correlated with greater agreement, ie, 1 = strongly agree, 2 = agree, etc.)
Table 3.
Change in Mean Scores of Pharmacy Students and Pharmacists Who Participated in an Online Training Program in Medication Therapy Management for Diabetes
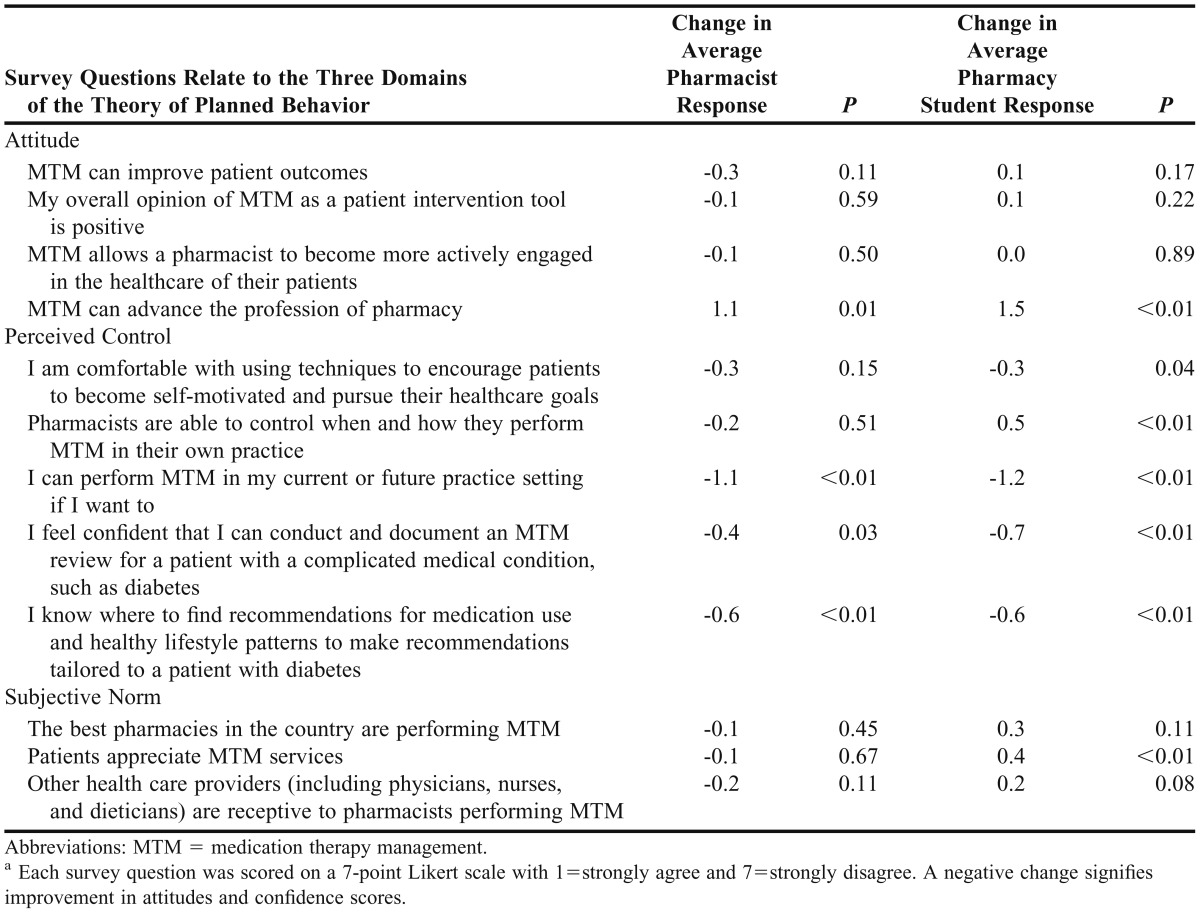
Pharmacists’ attitudes and perceptions regarding the behavioral norm did not change significantly. On average, students agreed less with these same measures after the program than before (Table 3). This change in summative data is partly due to the changes in responses to 2 questions: whether MTM advances the profession of pharmacy (1.6 pre-intervention score versus 3.0 post-intervention score) and perception of patients’ appreciation of MTM (2.7 vs. 3.0), as shown in Table 4. The average response to all statements remained at some level of agreement following the program, as neutral feelings were scored as 4.
Table 4.
Change in average response to individual survey questionsa
Quiz scores for pharmacists and pharmacy students significantly improved by 0.8 (p = 0.02) and 0.6 (p < 0.01), respectively. Pharmacists answered an average of 0.8 more questions correctly and students answered 0.6 more questions correctly after completion of the program.
Based on participants’ responses to the demographic questions in the survey instrument, the 2 groups had different educational goals for participating in the program. Pharmacists were looking for tools to perform MTM, whereas a large number of students did not have a particular goal in mind. After completing the program, both groups conveyed that they had gained beneficial knowledge. Several participants commented that they understood MTM better and over 50% of participants in both groups stated that they intend to use the skills gained during the program to conduct MTM sessions with patients (Figure 1). Participants’ other comments included that they better understood how to detect and solve drug-related problems, communicate with patients, and prioritize drug-related problems and patient educational needs given the time constraints of an MTM.
DISCUSSION
This study showed significant improvement in pharmacists’ and students’ perception of their ability to control performance of MTM, which suggests an increased likelihood for future performance of MTM. However, this form of education does not appear to be effective in improving participants’ attitudes about MTM or their perception of the subjective norm regarding pharmacist-provided MTM. Although the average response to certain statements showed a decline in agreement following completion of the program, none of the statements changed from agreement to disagreement. This may be partly due to the high level of agreement prior to the intervention and the possibility of self-selection to participate in the study of students and pharmacists who already valued the practice of MTM prior to the study.
These data are similar to those of Gallimore and colleagues who found that lecture and MTM activities in a pharmacotherapy laboratory class improved participants’ knowledge and perceived behavioral control, but found no improvement in attitudes about MTM or intent to perform MTM services.14 Increased confidence and knowledge following the use of an online case program and the MirixaPro platform was also found by Begley and colleagues.12 They found that students had a greater appreciation of MTM as a whole and felt they could use MTM in their future practice, which is congruent with the participant response in this study.
The 2 groups that participated in this study did not respond similarly to the educational method used. The program’s benefits were more clearly seen in the pharmacist group, whereas pharmacy students showed both improvement and regression in their perception of MTM. This may be due to several factors: students completed the program following completion of diabetes lectures and an examination in class, students had composed SOAP notes in previous classes, students completed this training program outside of designated class time, and as third-year students, they were unlikely to have the opportunity to apply these skills until the following year in their advanced pharmacy practice experiences.
Pharmacists may have been less experienced with documenting patient assessments using SOAP notes, so a greater amount of the program’s content was a training experience for them. Also, pharmacists probably saw greater immediate value in the educational program because of the relevance of MTM training to their daily practice.
Student participants commented that the program would have been more suitable if placed earlier in the semester as a learning tool for the examination on diabetes administered in their therapeutics course. Due to unforeseen technical challenges with Moodle, the MTM program was not available to students until after that examination. It would have been most helpful for students to complete each of the 4 MTM meetings online as they progressed through that portion of the diabetes module in class.
Many students struggled with understanding the purpose and content of a medication action plan and the personal medication record which was to be included at the end of their SOAP note. Many simply repeated the patient’s medication list as their action plan instead of listing other items for the patient to accomplish, such as using a medication box or home blood glucose meter. Because these 2 patient tools had not been included in the students’ previous training experiences, future programs for students in MTM should focus on these unique aspects of MTM so as not to duplicate material at the expense of learning new material.
The average time required to complete the entire MTM program was 4 to 5 hours for pharmacists and students, which was longer than the originally anticipated time of 2 to 3 hours. However, we cannot validate the accuracy of the participants’ perception of how long the program took, especially as most completed sections of the program on separate days. Several students commented that the program took too long to complete, considering their workload during the end of the semester and this may have affected how much effort they invested in completing the program. Additionally, several technical problems that occurred during the study may have confused participants and affected the time spent online using the program, as well as their overall perception of the program.
Limitations of this study include the small sample size that was composed of pharmacists from 1 state and students from 1 graduating class at 1 university. Thus, participants may not be representative of pharmacists or students as a whole. Also, different types of credit were offered to the 2 groups, and the program did not train participants to use a commercially available MTM program. Finally, addressing many of the barriers to performing MTM, such as access to patients’ medical records, compensation for MTM services, and changes in pharmacy workflow and staffing patterns necessary to allow pharmacists to sit down for a 30-minute interview with a patient, are beyond the scope of an educational program.5
CONCLUSION
An online training program that used a virtual learning platform to train pharmacists and students suggests that this and similar programs at other institutions may be used to increase the likelihood of high-quality MTM performance following pharmacy school graduation. More than half of each group of participants stated that they intended to use the knowledge and skills gained in this program in their future practice of MTM. The program improved participants’ perception of behavioral control over performance of MTM and knowledge of how to perform MTM, but no improvements were seen in participants’ attitude toward or perception of the subjective norm surrounding MTM performance. Pharmacists’ beliefs in MTM showed an increase in agreement with positive MTM statements more consistently than pharmacy students, who showed both an increase and decrease in agreement with survey statements. This suggests that an online virtual case training method is beneficial for pharmacists’ MTM training, and that a virtual program should be strategically incorporated into the pharmacy curriculum to support classroom learning for greatest results.
ACKNOWLEDGEMENTS
This research project was supported through a grant from the NACDS, though NACDS did not have any influence on the content of the research intervention or data reporting.
The researchers thank the University of Wisconsin (UW) Extension Services in Pharmacy for supporting the program on their Web site; Denise L. Walbrandt-Pigarelli and Casey Gallimore for their help in the creation of the content for the virtual patient educational program; Audrey Fish and Kari Trapskin for their help in sending e-mail invitations to pharmacists; Giselle Di’Piro for help in gathering informed consent forms from pharmacy students; Sharron Vetter for help in writing the research grant for this project; and Jeannette Roberts, Dean of the UW School of Pharmacy, for her role in creating the first UW PGY2 Ambulatory Care Residency Program.
Appendix 1. Excerpt from virtual patient encounter in an online medication therapy management teaching program.
REFERENCES
- 1.American Pharmacists Association, National Association of Chain Drug Stores Foundation. Medication therapy management core elements service model version 2.0. J Am Pharm Assoc. 2008;48(3):341–353. doi: 10.1331/JAPhA.2008.08514. [DOI] [PubMed] [Google Scholar]
- 2.Pharmacy Society of Wisconsin. The Wisconsin Pharmacy Quality Collaborative Web site. http://www.pswi.org. Accessed August 8, 2012.
- 3.American Diabetes Association. Standards of medical care in diabetes-2011. Diabetes Care. 2011;34(Suppl 1):S11–S61. doi: 10.2337/dc11-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kraemer DF, Kradjan WA, Blanco TM, Low JA. A randomized study to assess the impact of pharmacist counseling of employer-based health plan beneficiaries with diabetes: the EMPOWER study. J Pharm Pract. 2012;25(2):169–79. doi: 10.1177/0897190011418513. [DOI] [PubMed] [Google Scholar]
- 5.Lounsbery JL, Green CG, Bennett MS, Pedersen CA. Evaluation of pharmacists' barriers to the implementation of medication therapy management services. J Am Pharm Assoc (2003). 2009;49(1):51–58. doi: 10.1331/JAPhA.2009.017158. [DOI] [PubMed] [Google Scholar]
- 6.Blake KV, Madhavan SS. Perceived barriers to provision of medication therapy management services (MTMS) and the likelihood of a pharmacist to work in a pharmacy that provides MTMS. Ann Pharmacother. 2010;44(3):424–431. doi: 10.1345/aph.1M386. [DOI] [PubMed] [Google Scholar]
- 7.Kuhn C, Powell PH, Sterrett JJ. Elective course on medication therapy management services. Am J Pharm Educ. 2010;74(3):Article 40. doi: 10.5688/aj740340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Begley KJ, Coover KL, Tilleman JA, Haddad AM, Augustine SC. Medication therapy management training using case studies and the MirixaPro platform. Am J Pharm Educ. 2011;75(3):Article 49. doi: 10.5688/ajpe75349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gallimore CE, Thorpe JM, Trapskin K. Simulated medication therapy management activities in a pharmacotherapy laboratory course. Am J Pharm Educ. 2011;75(5):Article 95. doi: 10.5688/ajpe75595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cook DA, Triola MM. Virtual patients: a critical literature review and next steps. Med Educ. 2009;43(4):303–311. doi: 10.1111/j.1365-2923.2008.03286.x. [DOI] [PubMed] [Google Scholar]
- 11.Gesundheit N, Brutlag P, Youngblood P, Gunning WT, Zary N, Fors U. The use of virtual patients to assess the clinical skills and reasoning of medical students: initial insights on student acceptance. Med Teach. 2009;31(8):739–742. doi: 10.1080/01421590903126489. [DOI] [PubMed] [Google Scholar]
- 12.Villaume WA, Berger BA, Barker BN. Learning motivational interviewing: scripting a virtual patient. Am J Pharm Educ. 2006;70(2):Article 33. doi: 10.5688/aj700233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Orr KK. Integrating virtual patients into a self-care course. Am J Pharm Educ. 2007;71(2):Article 30. doi: 10.5688/aj710230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sweet BV, Welage LS, Johnston JP. Effect of a Web-based continuing-education program on pharmacist learning. Am J Health-Syst Pharm. 2009;66(21):1902–1903. doi: 10.2146/ajhp080658. [DOI] [PubMed] [Google Scholar]
- 15.Francis JJ, Eccles MP, Johnston M, et al. Constructing questionnaires based on the theory of planned behavior: a manual for health services researchers. http://www.rebeqi.org/ViewFile.aspx?itemID=212. Accessed June 6, 2012.
- 16.Muñoz DC, Ortiz A, González C, López DM, Blobel B. Effective e-learning for health professional and medical students: the experience with SIAS-intelligent tutoring system. Stud Health Technol Inform. 2010;156:89–102. [PubMed] [Google Scholar]