Abstract
Prior studies implicate facial emotion recognition (FER) difficulties among individuals with autism spectrum disorders (ASD); however, many investigations focus on FER accuracy alone and few examine ecological validity through links with everyday functioning. We compared FER accuracy and perceptual sensitivity (from neutral to full expression) between 42 adolescents with high functioning (IQ>80) ASD and 31 typically developing adolescents (matched on age, IQ, sex ratio) across six basic emotions and examined links between FER and symptomatology/adaptive functioning within the ASD group. Adolescents with ASD required more intense facial expressions for accurate emotion identification. Controlling for this overall group difference revealed particularly diminished sensitivity to sad facial expressions in ASD, which was uniquely correlated with ratings of autism-related behavior and adaptive functioning.
Keywords: autism, emotion, face, symptomatology, adaptive functioning
In his seminal report of 11 cases, Kanner (1944) described children with an ‘autistic disorder of affective contact’. Indeed, modern diagnostic criteria and the tools commonly used to make autism spectrum disorder (ASD) diagnoses include items related to difficulties identifying and processing emotional information (APA, 1994, Lord et al., 2000). In clinical and laboratory settings, perhaps the most common way to assess emotional identification and perception is through facial emotion recognition (FER) paradigms. Many studies have examined FER in ASD, with varying results (for review, see Harms, Martin, & Wallace, 2010). In the context of intellectual disability, children with ASD have shown deficits in FER (e.g., Celani, Battacchi, & Arcidiacono, 1999); however, low IQ impacts FER, complicating interpretation of findings and identification of ASD-specific deficits. More recent studies have included predominantly high functioning individuals on the autism spectrum in order to isolate ASD-specific deficits in FER. Several of these studies have shown general ASD-related difficulties with labeling full facial expressions (Bormann-Kischkel, Vilsmeier, & Baude, 1995; Buitelaar, Van der Wees, Swaab-Barneveld, & Van der Gaag, 1999; Hobson, 1986; Gross, 2004). However, some studies have found no deficits in identifying full emotional expressions (Adolphs, Sears, & Piven, 2001; Capps, Yirmiya, & Sigman, 1992; Castelli, 2005; Jones et al., 2010; Prior, Dahlstrom, & Squires, 1990; Robel et al., 2004), while others have found FER deficits restricted to particular emotions, most often emotions with a negative valence, such as fear (Howard et al., 2000; Pelphrey et al., 2002), disgust, sadness, and anger (Ashwin, Chapman, Colle, & Baron-Cohen, 2006). Mixed findings may occur in part because most images used in previous studies depict fully expressed emotions with diminished complexity and subtlety unlike the constantly changing expressions encountered in real-world interactions and because many interventions tailored to ASD currently incorporate training of facial emotion identification often using images of fully expressive faces. Therefore, the relative difficulty individuals with ASD may encounter, or different strategies they may use, with real-life FER could be masked in studies that use only these stereotyped images.
Indeed, faces change from neutral to expressive and from one expression to another in everyday contexts. Such movement has been shown to facilitate perception of faces and facial expressions in neurotypical adults (Berry, 1990) and individuals with intellectual impairments (Harwood, Hall, & Shinkfield, 1999). Gepner, Deruelle, and Grynfeltt (2001) found that dynamic (i.e., video and stroboscopic) presentations of facial emotion also facilitated emotional expression recognition among individuals with ASD. These clips, however, lasted only two seconds each. To examine fine grain perceptual sensitivity to facial emotional expression (i.e., the intensity of expression a previously neutral face needs to exhibit for successful recognition), greater exposure to the stimuli is needed.
Only a few studies to date have utilized “morphing faces” stimuli (in which intensity of emotional expressions is varied) to assess not only accurate identification of, but also perceptual sensitivity to, facial expressions of emotion among individuals with ASD. Of those that have, most used blends or morphs between emotions, rather than beginning with a neutral expression and progressing to full emotional expression. For example, in one study, Humphreys, Minshew, Leonard, and Behrmann (2007) found ASD-related difficulties with fear recognition from facial expression blends (e.g., fear-surprise). In another study using emotion blends, Teunisse and de Gelder (2001) found atypical responses to anger-sadness and anger-fear blends but intact responses to happy-sad blends among individuals with ASD. In contrast, Homer and Rutherford (2008) used numerous emotion blends and documented primarily intact performance among individuals with ASD. Only one study has examined FER perceptual sensitivity based on fine grain progressions from neutral to full expression (using the emotional multimorph task) among individuals with ASD. Participants were categorized into two groups of either high or low callous-unemotional trait ratings (associated with a form of antisocial behavior) (Rogers, Viding, Blair, Frith, & Happé, 2006). Using planned comparisons, only sadness required more intense facial expressions to be accurately recognized by individuals with both ASD and high callous-unemotional trait ratings than those with ASD and low ratings. However, a typically developing (TD) control group was not included in this study, which means that the ASD-related (a)typicality of performance on this task (whether responding to faces depicting sadness or any of the other five basic emotions) relative to TD peers of the same age and functioning level was not documented. Further work is needed to examine whether perceptual sensitivity to not only sad facial expressions, but also those depicting the other five basic emotions, is intact or impaired among individuals with ASD.
Identifying the functional impact of FER difficulties provides external validity for deficits documented in the laboratory setting; nevertheless, assessing correlations between everyday behavior and lab FER performance has only just begun to be explored in studies of ASD. For example, Humphreys et al. (2007) found that difficulties identifying fearful faces among individuals with ASD were associated with communication symptoms rated during a standardized interaction with a clinician (i.e., the Autism Diagnostic Observation Schedule [ADOS]). Similarly, Boraston, Blakemore, Chilvers, and Skuse (2007) found a significant correlation between sadness recognition (in the context of abstract Heider and Simmel-type animations (Heider & Simmel, 1944) designed to elicit emotion-laden descriptions, though without explicit social perceptual cues) and degree of impairment on the ADOS reciprocal social interaction score. Again, the ability to identify fear and sadness in particular, correlates with ASD symptomatology; however, these studies have been limited in utilizing only symptom counts from the standard diagnostic measures as real-life behavioral correlates. In addition to symptomatology, adaptive functioning, including social, communication, and daily living skills, provides a targeted correlate for validating the real-life impact of FER difficulties, particularly in ASD, in which adaptive behavior difficulties are common even in the highest functioning individuals (Liss et al., 2001; Kenworthy, Case, Harms, Martin, & Wallace, 2010).
The current study extends the investigation of perceptual sensitivity to facial expression in ASD by using the emotional multimorph task in which faces take 20 steps to morph from neutral to full expression to assess fine-tuned differences in perceptual sensitivity between high functioning adolescents with ASD (to avoid confounds associated with intellectual impairments) and TD adolescents. Moreover, correlational analyses with not only autism-related behavior ratings (including symptomatology) but also adaptive functioning will clarify relationships between FER in the laboratory and everyday behaviors observed by caregivers and clinicians. It is predicted that 1) TD adolescents will provide more accurate identification of and will be more perceptually sensitive to facial expressions of fear and sadness than will adolescents with ASD and 2) sensitivity to these two negative emotions will correlate with both autism-related behavior ratings and adaptive functioning as rated by clinicians and parents in the ASD group.
Method
Participants
Thirty-one TD adolescents (three female) and 42 high functioning adolescents (four female) with an ASD (11 with high functioning autism, 27 with Asperger’s syndrome, three with pervasive developmental disorder-not otherwise specified, and one with an ASD but exact diagnosis unknown because of sparse developmental data) completed the emotional multimorph task. ASD diagnoses were given by experienced clinicians according to DSM-IV criteria. Additionally, all participants met the Autism Diagnostic Interview-Revised (Lord, Rutter, & LeCouteur, 1994) cutoff for autism in the social domain and at least one other domain and/or met the ADOS-Generic (Lord et al., 2000) ASD cutoff for combined social and communication symptoms (Lainhart et al., 2006). Exclusion criteria for the ASD group included any known co-morbid medical conditions, genetic disorder (e.g., fragile X syndrome), or head injury/neurological insult which may affect cognitive functioning. TD participants were recruited from the community and parents of all TD participants underwent telephone screenings. TD participants were excluded from participation if they had ever received mental health treatment for anxiety, depression, or any other psychiatric condition, taken psychiatric medications, required special services in school, or had trauma/injury that could potentially affect cognitive functioning. Additionally, all participants scored 80 or higher on a Wechsler IQ test: all TD participants received the Wechsler Abbreviated Scale of Intelligence (WASI; Wechsler, 1999); ASD participants received the WASI [n=32], the Wechsler Intelligence Scale for Children (WISC)-III [n=2] (Wechsler, 1991) or WISC-IV [n=5] (Wechsler, 2003), or the Wechsler Adult Intelligence Scale-III [n=1] (Wechsler, 1997), and two ASD participants were missing IQ scores. The TD and ASD participants were group-matched on and therefore did not differ significantly in age, IQ, or sex ratio (see Table 1). Written consent from parents (and participants when they were 18 or older) and verbal and written assent from participants under age 18 were obtained.
Table 1.
Participant characteristics: Mean (SD).
| Autism Spectrum Disorder (N=42) |
Typically Developing (N=31) |
Statistic | p | |
|---|---|---|---|---|
| Age | 15.70 (2.79) Range: 12.00–23.67 |
16.35 (2.00) Range 12.67–19.67 |
t(1,71)=1.10 | .28 |
| Full Scale IQ | 113.80 (16.11) Range: 83–143 |
113.74 (10.94) Range 97–134 |
t(1,69)=−0.02 | .99 |
| Verbal IQ | 112.18 (16.36) Range: 77–140 |
111.16 (11.79) Range 92–132 |
t(1,69)= −0.29 | .77 |
| Performance IQ | 110.40 (14.93) Range: 74–136 |
112.74 (10.47) Range 93–142 |
t(1,69)=0.74 | .46 |
| Sex ratio (M:F) | 38:4 | 28:3 | Fisher’s Exact Test | .64 |
| ADI: Social Interaction | 19.00 (5.36) Range=8–29 |
|||
| ADI: verbal Communication | 14.98 (4.92) Range=6–26 |
|||
| ADI: Repetitive Behaviors | 5.78 (2.95) Range=0–12 |
|||
| ADOS: Social + Communication* | 12.00 (4.59) Range=3–20 |
|||
| ADOS Stereotyped Behavior* | 1.29 (1.45) Range=0–5 |
ADI-Autism Diagnostic Interview
ADOS-Autism Diagnostic Observation Schedule
n=41
Measures
Experimental Task
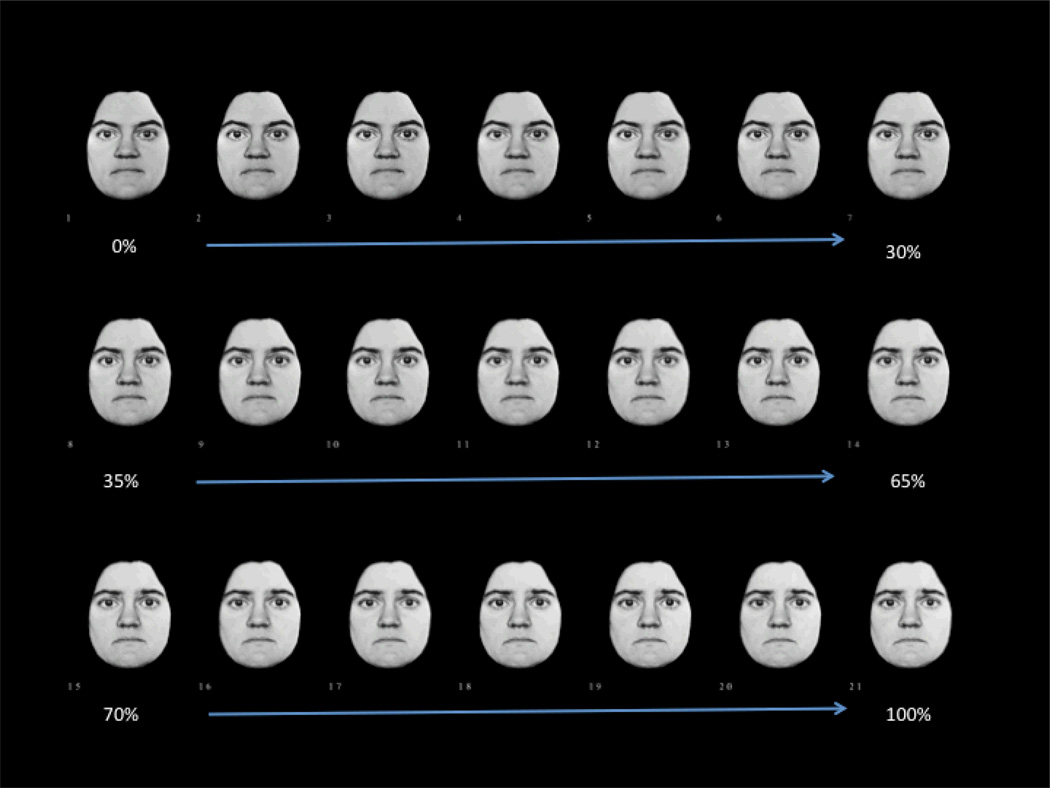
The Emotional MultiMorph Task: The stimuli in this task were taken from Ekman and Friesen’s Pictures of Facial Affect Series (Ekman & Friesen, 1976) and consisted of faces depicting six emotional expressions—happiness, sadness, fear, anger, surprise, and disgust. The task was administered previously by Blair, Colledge, Murray, and Mitchell (2001). Photo images were created for each emotion by morphing a full emotional expression with a neutral expression on the same face. Utilizing 179 key feature-points, the faces were manually delineated (Rowland & Perrett, 1995). For each emotionally expressive face, differences in spatial position were calculated for all pairs of corresponding feature-points on the neutral and fully expressive (i.e., end-point) faces. Algorithms were then used to produce equally distributed morphs between these end-points (Benson & Perrett, 1991). The result was 21 photo images or slides advancing in 5% increments from a 0% (neutral) emotional face to a 100% (fully expressive) emotional face (see Figure 1 for a depiction of a 5% graded morph from neutral to full expression of sadness). These images were presented in order, beginning with the most neutral. Each facial image (i.e., 5% increment) was shown for three seconds. Two different faces depicting each of the six emotions were shown resulting in a total of 12 trials. These 12 trials were presented in one of four pseudo-randomized orders that were counterbalanced across subjects.
Figure 1.
Morphing faces task: From neutral to full expression of sad in 5% increments.
Prior to beginning the task, participants were told that they would see facial expressions on the computer screen and that each face would start out neutral but would slowly change to show one of six emotions listed on their instruction sheet (placed in front of the participant for the duration of the experiment). Participants also were asked to describe each of the six emotions, prior to testing, to confirm their understanding of the emotion vocabulary. If participants had any confusion, the experimenter provided a definition of said emotion and confirmed that the participant understood before beginning the task. Participants were instructed to name verbally the emotion being shown as soon as they could confidently identify it (i.e., without making any random guesses). The experimenter warned participants that they would not be told whether their response was correct or not. Participants were also informed that they could change their response at any time during the presentation of the 21-slide sequence per face. Thus, during the study participants viewed and evaluated 252 faces (21 images for each of 12 trials).
Performance was assessed along two dimensions: (a) accuracy in identifying each emotion (0–100%) and (b) sensitivity to subtle expressions of emotion, as measured by the morph series/slide number at which correct emotional identification occurred (1–21). The slide score gauged a participant’s perceptual sensitivity and/or how quickly s/he correctly labeled each emotion. The final answer from each trial was used to evaluate accuracy. If a participant provided an incorrect final response—even if a previous response on that trial was correct—a slide score was not calculated so that including slide scores for emotions that were incorrectly identified would not skew the results. Participants may have provided considerably delayed or quick and impulsive incorrect responses. Either way, slide scores would be skewed if using inaccurate trials. The results of the two trials for each target emotion were collapsed into single average accuracy and average slide scores for each of the six emotions.
In order to maintain sample size for omnibus statistics, such as mixed-model analysis of variance, for individuals with no slide score (because they inaccurately labeled the emotion on both trials), the group (ASD vs. TD) mean was substituted (which did not change any results reported below). However, it is important to note that this group mean substitution was not completed for the correlational analyses.
Behavioral Correlates
Autism Diagnostic Observation Schedule (ADOS) – Generic (Lord et al., 2000): The ADOS is a semi-structured assessment used to evaluate individuals suspected of having ASD. It consists of various activities that allow one to observe social and communication behaviors related to ASD diagnoses. Either module 3 or 4, given the age and expressive language abilities of the participants here, was administered. Classification is determined by cutoffs for both the broader diagnosis of ASD, as well as a narrower conceptualization of autism. A trained researcher who had undergone reliability confirmation administered the ADOS.
Social Responsiveness Scale (SRS) (Constantino, 2002): The SRS is a 65-item informant-based rating scale utilized to assess (mostly social-communication) traits associated with ASD across the full range of severity. It distinguishes individuals with ASD from controls (Constantino, Przybeck, Friesen, & Todd, 2000) and is highly correlated with one of the most widely used diagnostic instruments in the field, the Autism Diagnostic Inventory (Constantino et al., 2003). The SRS provides an overall summary score that was used here as a correlate with FER.
Adaptive Behavior Assessment System-II (ABAS-II) (Harrison & Oakland, 2003): The ABAS-II is an informant-completed questionnaire designed to assess a participant’s adaptive skills. The parent-completed ABAS-II was used here to evaluate an individual’s strengths and weaknesses in the domains of communication, community use, functional academics, home living, health/safety, leisure, self-direction, social, and (for participants 17 and up) work and has proven effective in assessing adaptive difficulties among high functioning adolescents with ASD. Here, the Global Adaptive Composite was used as an overall measure of adaptive functioning and therefore as a correlate with FER.
Data Analysis
To establish that accuracy and sensitivity were indeed relatively independent metrics of FER, correlations between each of these metrics, collapsing across emotions, were run. Accuracy in identifying the six basic emotions was analyzed nonparametrically (using the Wilcoxon-Mann-Whitney test) because of the categorical nature of the data and ceiling effects in the TD group. Perceptual sensitivity was assessed with a mixed-model analysis of variance (ANOVA) with group (ASD vs. TD) as the between subjects factor and emotion (six basic emotions) as the within subjects factor. Follow-up one-way ANOVAs were used to examine group differences in sensitivity to each emotion. Analysis of covariance (ANCOVA) was used to test group differences in perceptual sensitivity for each emotion, taking into account the group difference in overall perceptual sensitivity (collapsed across the six emotions). Pearson correlations between both age and FSIQ, and FER perceptual sensitivity for each of the six emotions as well as overall FER accuracy (across all six emotions) were run in the ASD group only in order to insure that these potential nuisance variables were not affecting performance. Subsequently, Pearson and partial correlations (whenever age or IQ was related to perceptual sensitivity) were run to assess the relationship between sensitivity to emotional expressions or overall FER accuracy and both autism symptomatology and adaptive functioning.
Results
Intriguingly, overall FER accuracy and perceptual sensitivity were not significantly correlated with one another in either the TD (r=.19, p=.31) or ASD (r=−.06, p=.72) group, suggesting that these are independent measures of FER. Collapsing across all six emotions, TD adolescents were more accurate overall in emotion identification than ASD adolescents (Z=2.99, p=.003). Examining each emotion individually revealed that TD adolescents were more accurate in identifying only anger (Z=3.30, p=.001; see Table 2). This effect, however, should be interpreted with caution because of a ceiling effect in the TD group; only one TD participant failed a trial of an expression of anger.
Table 2.
Percent accuracy in emotion identification and percent intensity of facial expression needed to accurately identify each emotion by group: Mean (standard deviation).
| Emotion | Metric | Autism Spectrum Disorder |
Typically Developing |
Z/F | p |
|---|---|---|---|---|---|
| Happy | % accuracy | 100.00 (0.00) | 98.39 (8.98) | 1.16 | .24 |
| % intensity | 63.99 (15.41) | 49.92 (15.45) | 14.84 | <.001+ | |
| Anger | % accuracy | 80.95 (26.94) | 98.39 (8.98) | 3.30 | .001+ |
| % intensity | 73.05 (17.01) | 60.49 (16.80) | 9.73 | .003+ | |
| Sad | % accuracy | 73.81 (31.70) | 85.48 (23.07) | 1.60 | .12 |
| % intensity | 77.12 (16.75) | 54.76 (19.69) | 26.30 | <.001+* | |
| Fear | % accuracy | 77.38 (36.96) | 91.94 (18.69) | 1.65 | .10 |
| % intensity | 72.22 (14.89) | 65.16 (14.70) | 3.79 | .06 | |
| Disgust | % accuracy | 76.19 (31.70) | 85.48 (23.07) | 1.17 | .24 |
| % intensity | 71.06 (16.53) | 55.65 (17.00) | 14.82 | <.001+ | |
| Surprise | % accuracy | 85.71 (27.69) | 91.94 (22.72) | 1.14 | .25 |
| % intensity | 65.19 (19.43) | 53.92 (17.32) | 6.38 | .01 | |
| All | % accuracy | 82.39 (15.88) | 91.94 (9.33) | 2.99 | .003 |
| % intensity | 71.80 (11.31) | 58.70 (11.78) | 23.07 | <.001 |
After Bonferroni correction, group difference significant in ANOVA/ANCOVA controlling for IQ (for % intensity scores only) and in Wilcoxon-Mann-Whitney test (for % accuracy scores only).
Group difference significant in ANCOVA controlling for overall perceptual sensitivity (no longer significant after Bonferroni correction).
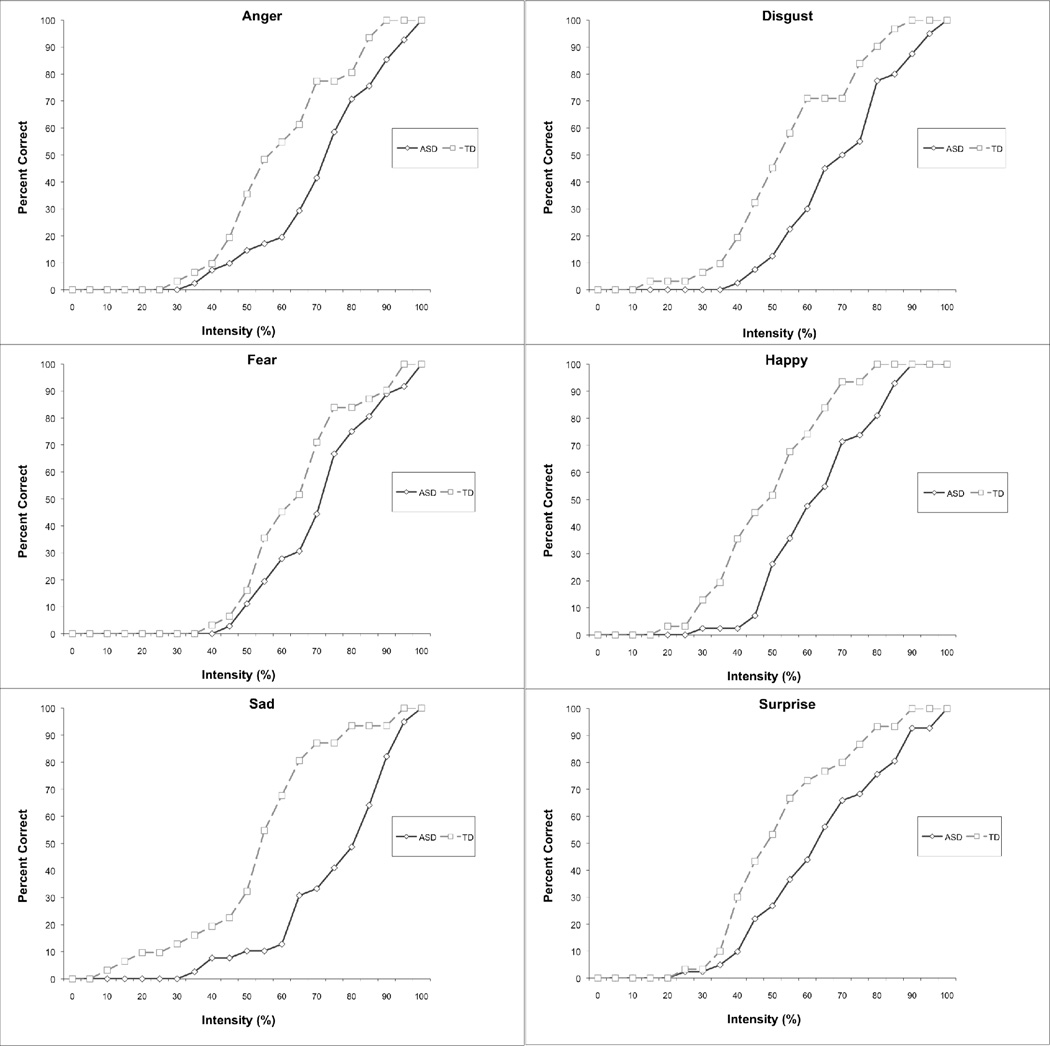
A mixed-model ANOVA revealed main effects of group (F(1,58)=14.08, p<.001), with the TD group showing greater perceptual sensitivity than the ASD group (see Table 2 and Figure 2), and emotion (F(5,54)=12.51, p<.001). There was also a significant interaction of group by emotion (F(5,54)=2.54, p=.03). Follow-up one-way ANOVAs revealed that the ASD group showed diminished perceptual sensitivity for each individual emotion (all Fs(1,68–1,71)>6.37, ps<.02), except for fear, which demonstrated a trend in this direction (F(1,65)=3.79, p=.06). If submitted to a Bonferroni correction, four (happiness, anger, sadness, disgust) of the six emotions remained significantly different between groups. After covarying for differences in overall perceptual sensitivity, only perceptual sensitivity to faces depicting sadness (of the six emotions) remained significantly different between the ASD and TD groups (F(1,70)=4.75, p=.03). Adding FSIQ as a covariate did not alter the pattern of findings.
Figure 2.
Cumulative percentage of adolescents with autism spectrum disorders (ASD) versus typically developing (TD) adolescents who accurately identified each of the six emotions at each intensity level.
Results showed that perceptual sensitivity scores for faces depicting happiness (r=−.48, p=.002) and surprise (r=−.35, p=.03) were significantly correlated with FSIQ in the ASD group, whereas age was not significantly correlated with any perceptual sensitivity scores. Therefore, subsequent correlational analyses for happiness and surprise include both standard Pearson and partial (covarying the effects of FSIQ) values.
Pearson correlations revealed a consistent pattern in which clinician or parent ratings of everyday functioning (i.e., autism social-communication symptomatology and adaptive functioning) were associated with perceptual sensitivity to facial depictions of sadness (see Table 3). More specifically, diminished sensitivity to sadness was associated with a higher number of social and communication symptoms from the ADOS, greater endorsement of ASD traits from the SRS, and lower adaptive functioning scores on the ABAS-II Global Adaptive Composite. For autism-related behavior ratings as measured by the ADOS (social-communication symptoms only) and the SRS, sensitivity to faces depicting happiness also showed a positive correlation; however, once IQ was partialled only the association with the ADOS social-communication symptoms remained significant. Complementing these correlations with perceptual sensitivity, greater overall FER accuracy (across all six emotions) was found to be associated with increased adaptive functioning.
Table 3.
Pearson (r) and partial (pr) correlations between behavior ratings and facial emotion recognition perceptual sensitivity and accuracy within the group of adolescents with autism spectrum disorders.
| Emotion | Type of Correlation |
ADOS: Social + Communication (n=41) |
ADOS: Stereotyped Behavior (n=41) |
SRS: Total Score (n=41) |
ABAS-II: Global Adaptive Composite (n=41) |
|---|---|---|---|---|---|
| Perceptual Sensitivity | |||||
| Happy | r | .36* | .20 | .24 | −.21 |
| pr (IQ) | .33* | .13 | .11 | −.02 | |
| Anger | r | −.02 | .15 | .05 | −.13 |
| Sad | r | .48** | .23 | .49** | −.43** |
| Fear | r | .23 | −.27 | .18 | −.25 |
| Disgust | r | .09 | .21 | .36* | −.23 |
| Surprise | r | .02 | .12 | .03 | .03 |
| pr (IQ) | −.02 | .06 | −.05 | .10 | |
| Accuracy | |||||
| All | r | −.15 | −.21 | −.14 | .42** |
ADOS-Autism Diagnostic Observation Schedule
SRS-Social Responsiveness Scale
ABAS-Adaptive Behavior Assessment System
p<.05,
p<.01
A confusion matrix was constructed to examine whether any particular emotions were systematically mislabeled as certain other emotions and whether systematic mislabeling varied by group (Table 4). In general, ASD participants made similar errors to those made by TD participants, but in larger numbers. Participants most commonly labeled sad as angry or fear and labeled disgust as angry.
Table 4.
Facial emotion recognition confusion matrix by group.
| Autism Spectrum Disorder |
Response Given (% of total responses) | |||||||
|---|---|---|---|---|---|---|---|---|
| Happy | Angry | Sad | Fear | Disgust | Surprise | No Response | ||
| Target Emotion | Happy | 100.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Angry | 0.00 | 80.95 | 0.00 | 1.20 | 11.90 | 3.57 | 2.38 | |
| Sad | 0.00 | 13.10 | 73.81 | 8.33 | 3.57 | 1.20 | 0.00 | |
| Fear | 4.76 | 0.00 | 4.76 | 77.38 | 0.00 | 13.10 | 0.00 | |
| Disgust | 1.20 | 22.62 | 0.00 | 0.00 | 76.19 | 0.00 | 0.00 | |
| Surprise | 3.57 | 2.38 | 0.00 | 8.33 | 0.00 | 85.71 | 0.00 | |
| Typically Developing | Response Given (% of total responses) | |||||||
|---|---|---|---|---|---|---|---|---|
| Happy | Angry | Sad | Fear | Disgust | Surprise | No Response | ||
| Target Emotion | Happy | 98.39 | 0.00 | 0.00 | 0.00 | 0.00 | 1.61 | 0.00 |
| Angry | 0.00 | 98.39 | 0.00 | 0.00 | 1.61 | 0.00 | 0.00 | |
| Sad | 0.00 | 6.45 | 85.48 | 4.84 | 3.22 | 0.00 | 0.00 | |
| Fear | 1.61 | 0.00 | 0.00 | 91.94 | 3.22 | 3.22 | 0.00 | |
| Disgust | 0.00 | 14.52 | 0.00 | 0.00 | 85.48 | 0.00 | 0.00 | |
| Surprise | 1.61 | 0.00 | 0.00 | 6.45 | 0.00 | 91.94 | 0.00 | |
Discussion
When asked to identify emotions using a morphing faces paradigm, adolescents with ASD showed overall diminished perceptual sensitivity to facial emotions relative to TD adolescents. More specifically, perceptual sensitivity to four of the six emotions was lower in ASD after correction for multiple comparisons. After accounting for the overall group differences in perceptual sensitivity to emotional faces, adolescents with ASD required higher intensity facial depictions of sadness, in particular, for accurate recognition. This finding is tempered in that it did not survive Bonferroni correction for multiple comparisons; nevertheless, it extends findings from a previous study showing ASD-related difficulty in accurately recognizing sadness both in faces and in animations without explicit social cues (Boraston et al., 2007). The significant correlation found here between diminished perceptual sensitivity to sad faces and the number of social-communication symptoms endorsed using the ADOS also expands findings from Boraston et al. (2007) and suggests the functional relevance of this deficit to symptomatology. Moreover, we extend these findings across raters and domains; not only clinician-rated social-communication symptoms (using the ADOS), but also parent-reported ASD traits (using the SRS) and adaptive functioning (using the ABAS-II) were associated with diminished perceptual sensitivity to sad faces. Though there was a main effect of group for FER accuracy (a measure largely independent of perceptual sensitivity based on correlational analyses), this finding was driven primarily by group differences in identifying faces depicting anger. The tentative finding of diminished accuracy (but not sensitivity) in identifying faces depicting anger has some precedence in the extant literature (Ashwin, Chapman, Colle, & Baron-Cohen, 2006; Wallace, Coleman, & Bailey, 2008). However, because there was a limited number of trials assessing FER accuracy for each emotion and there was a ceiling effect of accurately identifying angry faces among the group of TD adolescents, we remain cautious about this finding. Finally, overall FER accuracy (collapsing across all six emotions) was positively correlated with scores on a measure of adaptive skills, further linking FER with everyday functioning in ASD.
Difficulty processing sadness, a marker for emotional empathy, has been associated with a particular type of antisocial behavior, psychopathy (Woodworth & Waschbusch, 2008), though not as strongly as diminished recognition of fear (Marsh & Blair, 2008). Diminished perceptual sensitivity to sad faces in ASD also may relate to difficulties with empathy. Nonverbal processing of affect is a principal component of empathy (Elfenbein & Ambady, 2002) and ratings of the intensity of facial sadness based on pupil size have been linked to empathic abilities (Harrison, Wilson, & Critchley, 2007). Some studies have shown autism-related difficulties (even compared to clinical controls) in emotional empathy-related behaviors, such as responding to distress cues (Scambler, Hepburn, Rutherford, Wehner, & Rogers, 2007; Sigman, Kasari, Kwon, & Yirmiya, 1992). Even more directly related to the FER results documented here, Rogers et al. (2006) found diminished sensitivity in recognizing sadness in a subset of ASD boys with high callous-unemotional trait ratings versus those with low ratings; all of whom were selected from a special school for children with behavioral difficulties (unlike the participants here who did not have externalizing behavior problems based on parent report [unpublished data]).
Although the current findings do not directly address emotional empathy in ASD, they likely reflect the enormous variability in the autism spectrum, including associated behavioral and emotional difficulties, particularly among higher functioning individuals (Kenworthy et al., 2005; Siegel, Minshew, & Goldstein, 1996). A model (Blair, 2008) has been delineated in which those with psychopathy or high psychopathic traits demonstrate intact or better cognitive empathy (e.g., theory of mind) but low emotional empathy, as indicated by the processing of faces depicting sadness and fear. In contrast and perhaps inconsistent with our findings, according to this model, individuals with ASD provide a mirror image with intact emotional empathy and impaired cognitive empathy (Dziobek et al., 2008). Nevertheless, our findings add to a growing literature demonstrating emotional processing difficulties in ASD and suggest that emotional empathy (insofar as this is associated with perceptual sensitivity to sadness) is not intact in ASD.
Our results also indicate that FER deficits, particularly in sensitivity to perceiving sad facial expressions, are strongly linked to both symptomatology and real-world social functioning in this group. It is perhaps unsurprising to find these associations between FER and real-life behavior ratings made by clinicians and parents because everyday situations demand fast, efficient assessment of emotion during interactions. Failing to quickly and accurately perceive another’s emotional state can have dire consequences for an individual’s ability to communicate and interact with others. Furthermore, because people often do not encode a full, stereotypical emotional expression when communicating, sensitivity to subtle emotional expressions, even more than accuracy in identifying stereotypical expressions, may predict success in social interactions.
Alternatively, it could be that lower adaptive functioning and higher symptomatology ratings reflect the ASD group’s diminished experience engaging in social interactions (including identifying and processing emotions in others) which is in turn reflected in performance on the FER task, though this is unlikely to explain the specific findings regarding sadness. Regardless, the correlations between behavior ratings and the sensitivity score for sad facial expressions in the ASD group are not a function of overall poor performance across tasks; for example, IQ was not associated with sensitivity to faces depicting sadness. Similarly, the documented significant correlations were not due to capitalizing on greater variance in performance on this task, since slide scores to faces depicting surprise were associated with greater variability (i.e., a larger standard deviation) in performance than were slide scores to sad faces.
It could be that more subtle changes in facial movement associated with the neutral-sad morphs compared to the morphs of the other five emotions were more difficult to process for individuals with ASD and drove the correlations with everyday functioning. However, general perceptual discrimination (e.g., ‘spot the difference’) is usually viewed as a strength (or at least intact), not a weakness, in ASD (for review, see Happé & Frith, 2006; Mottron et al., 2006). Furthermore, even after Bonferroni correction, the impairments in perceptual sensitivity of FER in ASD were not limited to sadness, but included other emotions with more pronounced facial movements, such as anger. Though the subtlety of change associated with neutral-sad morphs could have played a role in the findings, it does not completely explain them.
Also relevant to our findings are previous neuroimaging studies. For example, when asked to view morphing expressions of fear and anger, individuals with ASD demonstrated hypoactivation of the amygdala and the fusiform gyrus, and when contrasting morphed versus stereotyped depictions of these emotions, adults with ASD (as compared to control participants) irregularly modulated the amygdala, posterior superior temporal sulcus, and the fusiform gyrus (Pelphrey, Morris, McCarthy, & Labar, 2007). Pelphrey et al.’s study is part of a larger literature implicating a crucial role for the amygdala in processing facial depictions of negative emotions in particular (Costafreda, Brammer, David, & Fu, 2008). In addition to its well-known role in fear perception (Adolphs, Tranel, Damasio, & Damasio, 1995), the amygdala appears to play a crucial role in perceiving sad facial expressions as well. Implicit processing of both masked (Killgore & Yurgelun-Todd, 2007) and unmasked sad faces varying in intensity (Blair, Morris, Frith, Perret, & Dolan, 1999) has been shown to activate the amygdala in neurotypical children and adults, in contrast to other emotions (happy and angry) which did not activate the amygdala in these studies. Furthermore, Adolphs and Tranel (2004) found that patients with bilateral amygdala lesions rated sad morphs with less specificity than individuals with unilateral amygdala damage, other brain damage, or no brain damage. Finally, a recent study (Monk et al., 2010) provides evidence of atypical amygdala activation and functional connectivity (with cortical structures) among adults with ASD when viewing sad facial expressions (while completing a probe detection task). In addition to functional neuroimaging studies suggesting abnormal amygdalar activation patterns to emotionally expressive faces in ASD (Ashwin, Baron-Cohen, Wheelright, O’Riordan, & Bullmore, 2007; Pelphrey et al., 2007; Wang, Dapretto, Hariri, Sigman, & Bookheimer, 2004), investigations employing structural neuroimaging techniques indicate an abnormal developmental growth trajectory of the amygdala in children and young adults with ASD (Schumann et al., 2004). Based on our findings here, future work should further explore the link between perceptual sensitivity to distinct facial emotion depictions and both brain structure and function among individuals with ASD.
In the current study, the similarity of error patterns to the various emotions in our ASD and TD groups suggests similar looking patterns. Although the ASD group was less accurate in recognizing angry faces, both groups most often mistook sad and disgusted faces for angry and confused fear and surprise. These results suggest that both ASD and TD individuals were led to misclassify emotions by looking at the same (misleading/difficult to process) parts of the faces. Future research could use eye-tracking technology to determine if aberrant scan paths might account for FER difficulties in the ASD group. Interestingly, in our own eye-tracking study (Snow et al., submitted) we found no differences in time spent focusing on the eye and mouth regions for ASD versus TD participants (a subset of whom participated in the present study) consistent with some recent reports (e.g., Anderson, Colombo, & Shaddy, 2006; Rutherford & Towns, 2008), but not others (e.g., Pelphrey, Sasson, Reznick, Paul, & Goldman, 2002; Rutherford, Clements, & Sekuler, 2007).
Though we document overall difficulties in FER perceptual sensitivity among adolescents with ASD relative to TD adolescents, it remains possible that response bias/caution could have been a contributory factor. In addition, it may be viewed as a weakness that we utilized a limited number of emotional face exemplars. Finally, using ANCOVA procedures in which the covariate (overall perceptual sensitivity in this case) contains variance contributed by the dependent variables of interest (perceptual sensitivity scores for each of the six emotions) is a potential weakness. This practice has been a point of considerable debate and discussion in neuroimaging work, where for example, regionally specific volumetric differences are presented uncorrected and after controlling for overall brain volume to account for effects of overall brain size differences. However, we remain confident in the validity and specificity of our finding of an ASD-related decrease in perceptual sensitivity to sad facial expressions, because, alone among the six emotions tested, the result for sadness (a) survived covariation accounting for overall differences in perceptual sensitivity across all six emotions (which could be considered an overly conservative correction) and (b) was the only index significantly associated with both autistic behavior ratings and adaptive skills. Moreover, using a limited number of emotional face exemplars allowed maximal perceptual sensitivity resolution (i.e., 5% increments) balanced against task length and demands on participants’ attentional resources. Finally, even when examining single trial data for each emotion (not presented here), the pattern of perceptual sensitivity results remained similar to those reported, suggesting a robust effect. Nevertheless, to address these concerns, future work should use a greater number of emotional face exemplars (most likely with greater incremental changes in emotional expressiveness) and utilize control (e.g., object) morphing tasks to account for potential response bias and to test general perceptual sensitivity to non-face and non-social stimuli.
Conclusion
The present study adds to a growing body of work showing that high functioning individuals with ASD have difficulty processing facial depictions of emotions, particularly in terms of perceptual sensitivity. Here we show that high functioning adolescents with ASD require greater intensity of sad facial expressions for accurate recognition than do TD adolescents. Furthermore, this diminished sensitivity to sad facial expressions was uniquely associated with not only autistic behavior ratings but also adaptive functioning. These findings may reflect purported empathy deficits associated with ASD.
Acknowledgments
This research was supported by the Intramural Research Program of the NIH, National Institute of Mental Health.
We would like to thank the children and families who so kindly gave their time and energy to assist in this research.
References
- Adolphs R, Sears L, Piven J. Abnormal processing of social information from faces in autism. Journal of Cognitive Neuroscience. 2001;13(2):232–240. doi: 10.1162/089892901564289. [DOI] [PubMed] [Google Scholar]
- Adolphs R, Tranel D. Impaired judgments of sadness but not happiness following bilateral amygdala damage. Journal of Cognitive Neuroscience. 2004;16(3):453–462. doi: 10.1162/089892904322926782. [DOI] [PubMed] [Google Scholar]
- Adolphs R, Tranel D, Damasio H, Damasio AR. Fear and the human amygdala. Journal of Neuroscience. 1995;15(9):5879–5891. doi: 10.1523/JNEUROSCI.15-09-05879.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. The Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV) Washington, DC: Authors; 1994. [Google Scholar]
- Anderson CJ, Colombo J, Shaddy JD. Visual scanning and pupillary responses in young children with autism spectrum disorder. Journal of Clinical and Experimental Neuropsychology. 2006;28(7):1238–1256. doi: 10.1080/13803390500376790. [DOI] [PubMed] [Google Scholar]
- Ashwin C, Baron-Cohen S, Wheelright S, O’Riordan M, Bullmore ET. Differential activation of the amygdala and the ‘social brain’ during fearful face-processing in Asperger syndrome. Neuropsychologia. 2007;45(1):2–14. doi: 10.1016/j.neuropsychologia.2006.04.014. [DOI] [PubMed] [Google Scholar]
- Ashwin C, Chapman E, Colle L, Baron-Cohen S. Impaired recognition of negative basic emotions in autism: A test of the amygdala theory. Social Neuroscience. 2006;1(3–4):349–363. doi: 10.1080/17470910601040772. [DOI] [PubMed] [Google Scholar]
- Benson PJ, Perrett DI. Synthesising continuous-tone caricatures. Image and Vision Computing. 1991;9(2):123–129. [Google Scholar]
- Berry DS. What can a moving face tell us? Journal of Personality and Social Psychology. 1990;58(6):1004–1014. doi: 10.1037//0022-3514.58.6.1004. [DOI] [PubMed] [Google Scholar]
- Blair RJR. Fine cuts of empathy and the amygdala: Dissociable deficits in psychopathy and autism. Quarterly Journal of Experimental Psychology. 2008;61(1):157–170. doi: 10.1080/17470210701508855. [DOI] [PubMed] [Google Scholar]
- Blair RJR, Morris JS, Frith CD, Perrett DI, Dolan RJ. Dissociable neural responses to facial expressions of sadness and anger. Brain. 1999;122(5):883–893. doi: 10.1093/brain/122.5.883. [DOI] [PubMed] [Google Scholar]
- Blair RJR, Colledge E, Murray L, Mitchell DGV. A selective impairment in the processing of sad and fearful expressions in children with psychopathic tendencies. Journal of Abnormal Child Psychology. 2001;29(6):491–498. doi: 10.1023/a:1012225108281. [DOI] [PubMed] [Google Scholar]
- Boraston Z, Blakemore SJ, Chilvers R, Skuse D. Impaired sadness recognition is linked to social interaction deficit in autism. Neuropsychologia. 2007;45(7):1501–1510. doi: 10.1016/j.neuropsychologia.2006.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bormann-Kischkel C, Vilsmeier M, Baude B. The development of emotional concepts in autism. Journal of Child Psychology and Psychiatry. 1995;36(7):1243–1259. doi: 10.1111/j.1469-7610.1995.tb01368.x. [DOI] [PubMed] [Google Scholar]
- Buitelaar JK, Van der Wees M, Swaab-Barneveld H, Van der Gaag RJ. Theory of mind and emotion-recognition functioning in autistic spectrum disorders and in psychiatric control and normal children. Development and Psychopathology. 1999;11(1):39–58. doi: 10.1017/s0954579499001947. [DOI] [PubMed] [Google Scholar]
- Capps L, Yirmiya N, Sigman M. Understanding of simple and complex emotions in nonretarted children with autism. Journal of Child Psychology and Psychiatry. 1992;33(7):1169–1182. doi: 10.1111/j.1469-7610.1992.tb00936.x. [DOI] [PubMed] [Google Scholar]
- Castelli F. Understanding emotions from standardized facial expressions in autism and normal development. Autism. 2005;9(4):428–449. doi: 10.1177/1362361305056082. [DOI] [PubMed] [Google Scholar]
- Celani G, Battacchi MW, Arcidiacono L. The understanding of the emotional meaning of facial expressions in people with autism. Journal of Autism and Developmental Disorders. 1999;29(1):57–66. doi: 10.1023/a:1025970600181. [DOI] [PubMed] [Google Scholar]
- Constantino JN. Social Responsiveness Scale. Los Angeles, CA: Western Psychological Association; 2002. [Google Scholar]
- Constantino JN, Davis SA, Todd RD, Schindler MK, Gross MM, Brophy SL, Metzger LM, Shoushtari CS, Splinter R, Reich W. Validation of a brief quantitative measure of autistic traits: Comparison of the Social Responsiveness Scale with the Autism Diagnostic Interview-Revised. Journal of Autism and Developmental Disorders. 2003;33(4):427–433. doi: 10.1023/a:1025014929212. [DOI] [PubMed] [Google Scholar]
- Constantino JN, Przybeck T, Friesen D, Todd RD. Reciprocal social behavior in children with and without pervasive developmental disorders. Journal of Developmental and Behavioral Pediatrics. 2000;21(1):2–11. doi: 10.1097/00004703-200002000-00002. [DOI] [PubMed] [Google Scholar]
- Costafreda SG, Brammer MJ, David AS, Fu CHY. Predictors of amygdala activation during the processing of emotional stimuli: A meta-analysis of 385 PET and fMRI studies. Brain Research Reviews. 2008;58(1):57–70. doi: 10.1016/j.brainresrev.2007.10.012. [DOI] [PubMed] [Google Scholar]
- Dziobek I, Rogers K, Fleck S, Bahnemann M, Heekeren HR, Wolf OT, Convit A. Dissociation of cognitive and emotional empathy in adults with Asperger syndrome using the multifaceted empathy test (MET). Journal of. Autism and Developmental Disorders. 2008;38(3):464–473. doi: 10.1007/s10803-007-0486-x. [DOI] [PubMed] [Google Scholar]
- Ekman P, Friesen WV. Measuring facial movement. Environmental Psychology and Nonverbal Behavior. 1976;1(1):56–75. [Google Scholar]
- Elfenbein HA, Ambady N. On the universality and cultural specificity of emotion recognition: A meta-analysis. Psychological Bulletin. 2002;128(2):203–235. doi: 10.1037/0033-2909.128.2.203. [DOI] [PubMed] [Google Scholar]
- Gepner B, Deruelle C, Grynfeltt S. Motion and emotion: A novel approach to the study of face processing by young autistic children. Journal of Autism and Developmental Disorders. 2001;31(1):37–45. doi: 10.1023/a:1005609629218. [DOI] [PubMed] [Google Scholar]
- Gross TF. The perception of four basic emotions in human and nonhuman faces by children with autism and other developmental disabilities. Journal of Abnormal Child Psychology. 2004;32(5):469–480. doi: 10.1023/b:jacp.0000037777.17698.01. [DOI] [PubMed] [Google Scholar]
- Happé F, Frith U. The weak coherence account: Detail-focused cognitive style in autism spectrum disorders. Journal of Autism and Developmental Disorders. 2006;36(1):5–25. doi: 10.1007/s10803-005-0039-0. [DOI] [PubMed] [Google Scholar]
- Harms MB, Martin A, Wallace GL. Facial emotion recognition in autism spectrum disorders: A review of behavioral and neuroimaging studies. Neuropsychology Review. 2010;20(3):290–322. doi: 10.1007/s11065-010-9138-6. [DOI] [PubMed] [Google Scholar]
- Harrison NA, Wilson CE, Critchley HD. Processing of observed pupil size modulates perception of sadness and predicts empathy. Emotion. 2007;7(4):724–729. doi: 10.1037/1528-3542.7.4.724. [DOI] [PubMed] [Google Scholar]
- Harrison PL, Oakland T. Adaptive Behavior Assessment System-II. San Antonio, TX: Harcourt Assessment, Inc; 2003. [Google Scholar]
- Harwood NK, Hall LJ, Shinkfield AJ. Recognition of facial emotional expressions from moving and static displays by individuals with mental retardation. American Journal of Mental Retardation. 1999;104(3):270–278. doi: 10.1352/0895-8017(1999)104<0270:ROFEEF>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Heider F, Simmel M. An experimental study of apparent behavior. American Journal of Psychology. 1944;57(2):243–259. [Google Scholar]
- Hobson RP. The autistic child's appraisal of expressions of emotion. Journal of Child Psychology and Psychiatry. 1986;27(3):321–342. doi: 10.1111/j.1469-7610.1986.tb01836.x. [DOI] [PubMed] [Google Scholar]
- Homer M, Rutherford MD. Individuals with autism can categorize facial expressions. Child Neuropsychology. 2008;14(5):419–437. doi: 10.1080/09297040802291715. [DOI] [PubMed] [Google Scholar]
- Howard MA, Cowell PE, Boucher J, Broks P, Mayes A, Farrant A, Roberts N. Convergent neuroanatomical and behavioural evidence of an amygdala hypothesis of autism. Neuroreport. 2000;11(13):2931–2935. doi: 10.1097/00001756-200009110-00020. [DOI] [PubMed] [Google Scholar]
- Humphreys K, Minshew N, Leonard GL, Behrmann M. A fine-grained analysis of facial expression processing in high-functioning adults with autism. Neuropsychologia. 2007;45(4):685–695. doi: 10.1016/j.neuropsychologia.2006.08.003. [DOI] [PubMed] [Google Scholar]
- Jones CR, Pickles A, Falcaro M, Marsden AJ, Happé F, Scott SK, Sauter D, Tregay J, Phillips RJ, Baird G, Simonoff E, Charman T. A multimodal approach to emotion recognition ability in autism spectrum disorders. Journal of Child Psychology and Psychiatry. 2010 doi: 10.1111/j.1469-7610.2010.02328.x. In press. [DOI] [PubMed] [Google Scholar]
- Kanner L. Autistic disturbances of affective contact. Nervous Child. 1943;2:217–250. [PubMed] [Google Scholar]
- Kenworthy LE, Black DO, Wallace GL, Ahluvalia T, Wagner AE, Sirian LM. Disorganization: The forgotten executive dysfunction in high functioning autism (HFA) spectrum disorders. Developmental Neuropsychology. 2005;28(3):809–827. doi: 10.1207/s15326942dn2803_4. [DOI] [PubMed] [Google Scholar]
- Kenworthy L, Case L, Harms MB, Martin A, Wallace GL. Adaptive behavior ratings correlate with symptomatology and IQ among individuals with high-functioning autism spectrum disorders. Journal of Autism and Developmental Disorders. 2010;40(4):416–423. doi: 10.1007/s10803-009-0911-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killgore WD, Yurgelun-Todd DA. Unconscious processing of facial affect in children and adolescents. Social Neuroscience. 2007;2(1):28–47. doi: 10.1080/17470910701214186. [DOI] [PubMed] [Google Scholar]
- Lainhart JE, Bigler ED, Bocian M, Coon H, Dinh E, Dawson G, Deutsch CK, Dunn M, Estes A, Tager-Flusberg H, Folstein S, Hepburn S, Hyman S, McMahon W, Minshew N, Munson J, Osann K, Ozonoff S, Rodier P, Rogers S, Sigman M, Spence MA, Stodgell CJ, Volkmar F. Head circumference and height in autism: a study by the Collaborative Program of Excellence in Autism. American Journal of Medical Genetics. 2006;140(21):2257–2274. doi: 10.1002/ajmg.a.31465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liss M, Harel B, Fein D, Allen D, Dunn M, Feinstein C, Morris R, Waterhouse L, Rapin I. Predictors and correlates of adaptive functioning in children with developmental disorders. Journal of Autism and Developmental Disorders. 2001;31(2):219–230. doi: 10.1023/a:1010707417274. [DOI] [PubMed] [Google Scholar]
- Lord C, Risi S, Lambrecht L, Cook EH, Jr, Leventhal BL, DiLavore PC, Pickles A, Rutter M. The Autism Diagnostic Observation Schedule-Generic: a standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders. 2000;30(3):205–223. [PubMed] [Google Scholar]
- Lord C, Rutter M, LeCouteur A. Autism diagnostic interview-revised – a revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders. 1994;24(5):659–685. doi: 10.1007/BF02172145. [DOI] [PubMed] [Google Scholar]
- Marsh AA, Blair RJR. Deficits in facial affect recognition among antisocial populations: A meta-analysis. Neuroscience and Biobehavioral Reviews. 2008;32(3):454–465. doi: 10.1016/j.neubiorev.2007.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monk CS, Weng SJ, Wiggins JL, Kurapati N, Louro HM, Carrasco M, Maslowsky J, Risi S, Lord C. Neural circuitry of emotional face processing in autism spectrum disorders. Journal of Psychiatry & Neuroscience. 2010;35(2):105–114. doi: 10.1503/jpn.090085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mottron L, Dawson M, Soulières I, Hubert B, Burack J. Enhanced perceptual functioning in autism: An update, and eight principles of autistic perception. Journal of Autism and Developmental Disorders. 2006;36(1):27–43. doi: 10.1007/s10803-005-0040-7. [DOI] [PubMed] [Google Scholar]
- Pelphrey KA, Morris JP, McCarthy G, Labar KS. Perception of dynamic changes in facial affect and identity in autism. Social Cognitive and Affective Neuroscience. 2007;2(2):140–149. doi: 10.1093/scan/nsm010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelphrey KA, Sasson RJ, Reznick JS, Paul G, Goldman BD, Piven J. Visual scanning of faces in autism. Journal of Autism and Developmental. Disorders. 2002;32(4):249–261. doi: 10.1023/a:1016374617369. [DOI] [PubMed] [Google Scholar]
- Prior M, Dahlstrom B, Squires TL. Autistic children's knowledge of thinking and feeling states in other people. Journal of Child Psychology and Psychiatry. 1990;31(4):587–601. doi: 10.1111/j.1469-7610.1990.tb00799.x. [DOI] [PubMed] [Google Scholar]
- Robel L, Ennouri K, Piana HN, Vaivre-Douret L, Perier A, Flament MF, Mouren-Simeoni MC. Discrimination of face identities and expressions in children with autism: Same or different? European Child and Adolescent Psychiatry. 2004;13(4):227–233. doi: 10.1007/s00787-004-0409-8. [DOI] [PubMed] [Google Scholar]
- Rogers J, Viding E, Blair RJ, Frith U, Happé F. Autism spectrum disorder and psychopathy: shared cognitive underpinnings or double hit? Psychological Medicine. 2006;36(12):1789–1798. doi: 10.1017/S0033291706008853. [DOI] [PubMed] [Google Scholar]
- Rowland DA, Perrett DI. Manipulating facial appearance through shape and color. IEEE Computer Graphics and Applications. 1995;15(5):70–76. [Google Scholar]
- Rutherford MD, Clements KA, Sekuler AB. Differences in discrimination of eye and mouth displacement in autism spectrum disorders. Vision Research. 2007;47(15):2099–2110. doi: 10.1016/j.visres.2007.01.029. [DOI] [PubMed] [Google Scholar]
- Rutherford MD, Towns AM. Scan path differences and similarities during emotion perception in those with and without autism spectrum disorders. Journal of Autism and Developmental Disorders. 2008;38(7):1371–1381. doi: 10.1007/s10803-007-0525-7. [DOI] [PubMed] [Google Scholar]
- Scambler DJ, Hepburn S, Rutherford MD, Wehner EA, Rogers SJ. Emotional responsivity in children with autism, children with other developmental disabilities, and children with typical development. Journal of Autism and Developmental Disorders. 2007;37(3):553–563. doi: 10.1007/s10803-006-0186-y. [DOI] [PubMed] [Google Scholar]
- Schumann CM, Hamstra J, Goodlin-Jones BL, Kwon H, Reiss AL, Amaral DG. The amygdala is enlarged in children but not adolescents with autism; The hippocampus is enlarged at all ages. Journal of Neuroscience. 2004;24(28):6392–6401. doi: 10.1523/JNEUROSCI.1297-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel DJ, Minshew NJ, Goldstein G. Wechsler IQ profiles in diagnosis of high-functioning autism. Journal of Autism and Developmental Disorders. 1996;26(4):389–406. doi: 10.1007/BF02172825. [DOI] [PubMed] [Google Scholar]
- Sigman MD, Kasari C, Kwon JH, Yirmiya N. Responses to the negative emotions of others by autistic, mentally-retarded, and normal children. Child Development. 1992;63(4):796–807. [PubMed] [Google Scholar]
- Teunisse JP, de Gelder B. Impaired categorical perception of facial expressions in high-functioning adolescents with autism. Child Neuropsychology. 2001;7(1):1–14. doi: 10.1076/chin.7.1.1.3150. [DOI] [PubMed] [Google Scholar]
- Wallace S, Coleman M, Bailey A. An investigation of basic facial expression recognition in autism spectrum disorders. Cognition & Emotion. 2008;22(7):1353–1380. [Google Scholar]
- Wang AT, Dapretto M, Hariri AR, Sigman M, Bookheimer SY. Neural correlates of facial affect processing in children and adolescents with autism spectrum disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43(4):481–490. doi: 10.1097/00004583-200404000-00015. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Wechsler Intelligence Scale for Children-Third Edition. San Antonio, TX: The Psychological Corporation; 1991. [Google Scholar]
- Wechsler D. Wechsler Adult Intelligence Scale-Third Edition. San Antonio, TX: The Psychological Corporation; 1997. [Google Scholar]
- Wechsler D. Wechsler Abbreviated Scale of Intelligence. San Antonio, TX: The Psychological Corporation; 1999. [Google Scholar]
- Wechsler D. Wechsler Intelligence Scale for Children-Fourth Edition. San Antonio, TX: The Psychological Corporation; 2003. [Google Scholar]
- Woodworth M, Waschbusch D. Emotional processing in children with conduct problems and callous/unemotional traits. Child Care Health and Development. 2008;34(2):234–244. doi: 10.1111/j.1365-2214.2007.00792.x. [DOI] [PubMed] [Google Scholar]